Abstract
Objective To develop expeditiously a pragmatic, modular, and extensible software framework for understanding and improving healthcare value (costs relative to outcomes).
Materials and methods In 2012, a multidisciplinary team was assembled by the leadership of the University of Utah Health Sciences Center and charged with rapidly developing a pragmatic and actionable analytics framework for understanding and enhancing healthcare value. Based on an analysis of relevant prior work, a value analytics framework known as Value Driven Outcomes (VDO) was developed using an agile methodology. Evaluation consisted of measurement against project objectives, including implementation timeliness, system performance, completeness, accuracy, extensibility, adoption, satisfaction, and the ability to support value improvement.
Results A modular, extensible framework was developed to allocate clinical care costs to individual patient encounters. For example, labor costs in a hospital unit are allocated to patients based on the hours they spent in the unit; actual medication acquisition costs are allocated to patients based on utilization; and radiology costs are allocated based on the minutes required for study performance. Relevant process and outcome measures are also available. A visualization layer facilitates the identification of value improvement opportunities, such as high-volume, high-cost case types with high variability in costs across providers. Initial implementation was completed within 6 months, and all project objectives were fulfilled. The framework has been improved iteratively and is now a foundational tool for delivering high-value care.
Conclusions The framework described can be expeditiously implemented to provide a pragmatic, modular, and extensible approach to understanding and improving healthcare value.
Keywords: care value, care quality, care outcomes, care costs, activity-based cost accounting
Background and significance
Improving healthcare value—defined as the health outcomes achieved per dollar spent—is a central challenge for the US healthcare system.1 The USA spends approximately $9000 per capita on health care annually, accounting for approximately 18% of the gross domestic product.2 This per capita expenditure is the highest in the world and roughly 2.5 times the average expenditure among industrialized nations.3 Despite these expenditures, health outcomes are relatively poor. An estimated 440 000 Americans die prematurely each year due to preventable medical harm.4 Moreover, US adults receive only about half of recommended care,5 and life expectancy in the US is below most developed nations and some developing nations.6 The lack of correlation between spending and outcomes is fueling a national focus on value.
Under traditional fee-for-service payment models, US healthcare systems have had little financial incentive to improve value.7 Increasingly, however, healthcare payors are adopting payment models that provide strong financial incentives for the delivery of high-value care.7 Payment models may offer a fixed fee for managing a population or episode of care rather than a variable fee that increases as more services are provided. Employers are also driving change. Large corporations such as Walmart have begun to steer high-cost, high-margin care such as cardiac and spine surgery to a small number of hospitals with demonstrated high value.8 Consequently, healthcare systems are faced with major financial and existential imperatives to understand and improve care value.
In seeking to improve care value, a central challenge most healthcare delivery organizations face is their limited capacity to measure and analyze healthcare value, particularly around costs.1 Understanding care costs is challenging due to the highly complex, fragmented, and variable nature of healthcare delivery.9 As noted by Porter and Lee, while measuring medical outcomes has become a national priority, there is a “near complete absence of data on the true costs of care for a patient with a particular condition over the full care cycle, crippling efforts to improve value.”10 Billing charges are often confused with the costs of delivering care. However, charges are an inaccurate estimate of the actual costs incurred.10 True costing numbers are critical to developing and monitoring strategies to reduce costs, supporting the adoption of value-based reimbursement systems, and encouraging innovation.9 Cost accounting has high relevance for informatics as well. According to Ohno-Machado, “an important but often underpublished area of biomedical informatics (is) the cost-effectiveness of informatics interventions in healthcare,”11 which requires accurate healthcare cost data for proper evaluation.
The prior literature on healthcare cost accounting includes analyses of the relative strengths and weaknesses of different approaches,12–15 as well as high-level descriptions of specific cost accounting systems.16–22 Several commercial entities also provide software and consulting services in this area. Important barriers to the adoption of these approaches include the lack of detailed technical implementation guidance in the literature, especially within the USA; the sole focus in many of the approaches on activity-based costing (costing based on detailed tracking of all activities involved in a patient's care), which can be accurate but too resource-intensive for implementation across a healthcare system; the use of inflexible system architectures that are difficult to customize; frequent reliance on manual data capture, which is resource-intensive and difficult to maintain; and insufficient evidence that a meaningful cost-accounting system can be implemented rapidly to provide institutional benefit. When the University of Utah Health Sciences Center (UUHSC) decided to address this problem in 2012 as an institutional priority, these barriers were of significant concern.
Here, we provide technical details on how a multidisciplinary team overcame these barriers to implement a value improvement framework known as Value Driven Outcomes (VDO) that can be rapidly implemented and iteratively enhanced to support value improvement. By sharing our methodology, outcomes, and lessons learned, we seek to facilitate value improvement on a wider scale.
Objective and scope
The objective of the VDO initiative was to develop expeditiously a software framework for understanding and improving healthcare value that is focused on delivering practical utility (pragmatic), implemented using components that can be independently enhanced (modular), and capable of being improved over time (extensible).
The VDO framework can support both direct care costs (ie, costs directly associated with patient care) and indirect costs (ie, other costs, such as for operating the finance department). The VDO project scope described herein is limited to direct costs, as indirect costs are managed and evaluated using other procedures. The scope encompasses both facility costs (ie, costs incurred by the healthcare system) and professional costs (ie, costs incurred by the physicians). These and other cost accounting terms are defined in online supplementary appendix A, which provides a primer on cost accounting. The initiative scope also includes the analysis of quality and outcomes in relation to costs.
VDO was launched in May 2012, with initial deliverables expected within 6 months. This manuscript focuses on these initial deliverables, including the core technical framework, robust facility costing, initial professional costing, and reports and dashboards. We expect future manuscripts will focus on subsequent VDO deliverables such as outcomes analytics, enhanced professional costing, and analyses of indirect costs.
Materials and methods
Setting, governance, and human resources
VDO is an initiative of UUHSC, which includes University of Utah Health Care, the University of Utah School of Medicine, and the University of Utah Medical Group. UUHSC serves as the Intermountain West's only academic healthcare system and includes four hospitals, 10 community clinics, over 10 000 employees, and over 1200 physicians.
VDO is governed by a steering committee consisting of senior executive leadership. Under the direct engagement and direction of this steering committee, a multidisciplinary project team was assembled from Biomedical Informatics, Information Technology (IT), the Enterprise Data Warehouse, Finance, the Medical Group, and clinical departments.
Staffing was almost exclusively through existing resources. A dedicated project space was used to maximize collaboration. Staffing during the first 6 months consisted of approximately 8–16 core team members providing 0.6–1.0 full time equivalent (FTE) effort each. Subsequent staffing has been approximately 20 core team members providing 0.2–0.6 FTE effort each.
Systems and technology
UUHSC uses commercial electronic health record (EHR) systems from Epic, Cerner, and GE Healthcare. Human resources are managed through PeopleSoft, the supply chain is managed with Lawson, and an Enterprise Data Warehouse consolidates institutional data using Oracle for database management and Informatica for data integration. SAP Business Objects is used for enterprise reporting. Before VDO, an initial cost accounting system had been implemented at UUHSC that assigned actual supply costs to individual encounters. However, this system was not as modular and extensible as the implemented system, and approximately 50% of direct costs were simply distributed equally across relevant encounters.
Agile development
As may be expected for a project in which the end-product was not fully specified beforehand, we used an agile development methodology that emphasizes the iterative enhancement of working software, adaptation to changing requirements, and constant communication with customers and other team members.
Design principles
A central design principle was modularity. A second principle was pragmatism, wherein more robust costing was implemented only if the expected benefits outweighed the anticipated resources required. Consequently, we sought to minimize the manual collection of data not already captured as a part of usual clinical and business processes.
Evaluation criteria and methodology
Success criteria and evaluation methods were established as a part of the project. Criteria included:
Implementation timeliness, with a functioning, extensible prototype desired in 3 months, and a system capable of supporting institutional decision making desired in 6 months.
System performance, with a goal that most report requests complete within 5 s. To simulate typical usage, the VDO reports described in figures 2–6 were opened for a representative department (Orthopedic Surgery), and filter values were changed five times to update the reports. The times required for opening and updating the reports were measured using a stopwatch and summarized descriptively.
Completeness, with a goal of total direct costs accounted in VDO being within 2% of total direct costs in the general ledger, which accounts for all institutional expenses.
Accuracy. Because we consider cost accounting based on actual cost or time to be most accurate, we compared the proportion of total direct facility costs accounted using actual cost or time before and after the introduction of VDO. We did not conduct such a comparison for professional costs because the pre-VDO costing system did not support professional costs.
Extensibility, with a goal of allowing system capabilities, particularly cost methodologies, to be incrementally enhanced.
End-user adoption. We identified the number of users and usage of the reporting system. We also assessed adoption by key institutional leaders.
Ability to support value improvement. We determined the number of value improvement initiatives supported by VDO.
End-user satisfaction. We evaluated end-user satisfaction through an online survey based on a validated survey instrument for measuring end-user computing satisfaction.23 The full survey details are provided in online supplementary appendix B.
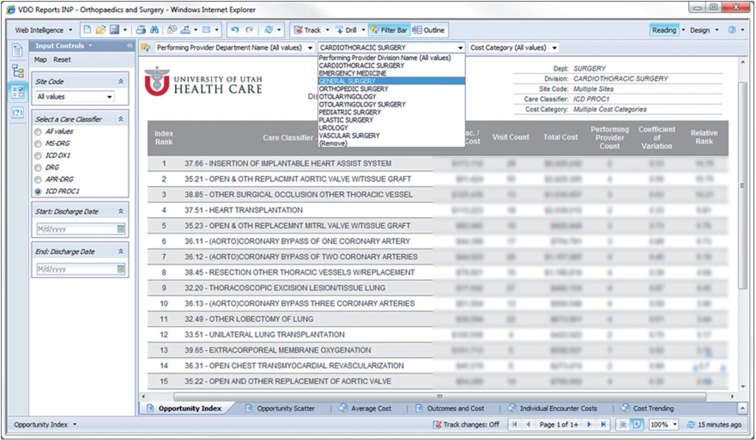
Figure 2:
Opportunity identification report.
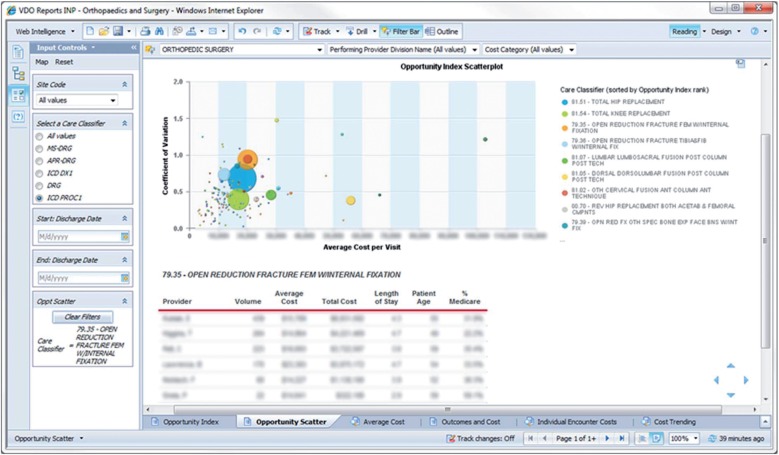
Figure 3:
Opportunity visualization report.
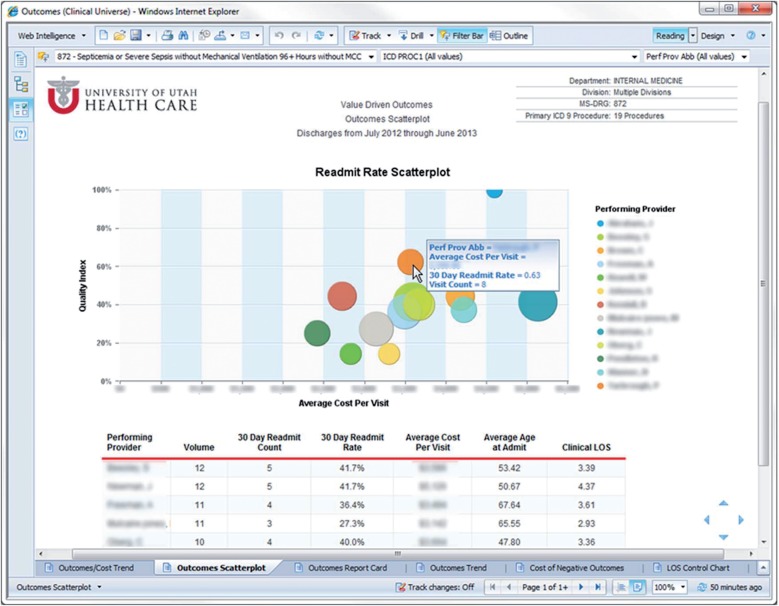
Figure 4:
Value dashboard.
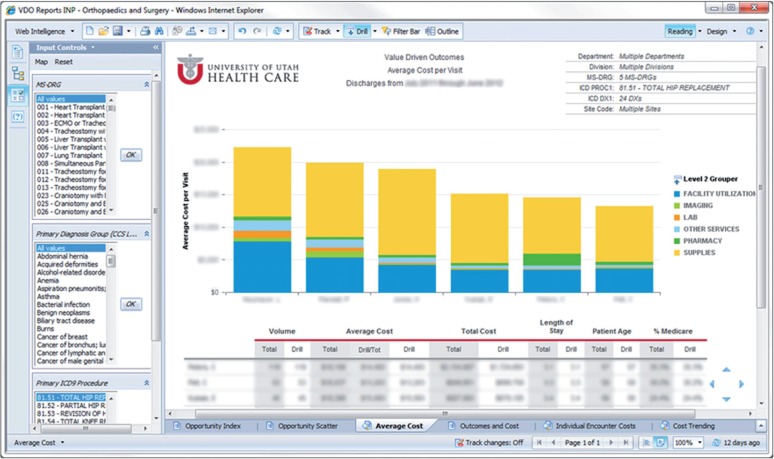
Figure 5:
Physician care cost dashboard.
Figure 6:
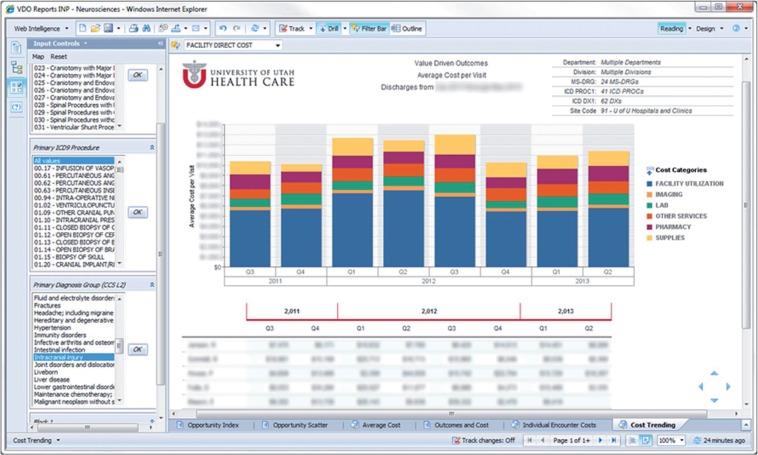
Cost trending report.
Challenges and solutions
We describe key challenges encountered and the solutions we implemented or are considering for future implementation.
Results
Overall cost accounting approach
VDO takes all costs recorded in the general ledgers of the healthcare system and the School of Medicine and identifies costs attributable to direct patient care. These direct care costs are then allocated to individual patient encounters. This cost allocation is determined by customizable cost methods that are applied to designated costs in the general ledger. These cost methods may include the allocation of large groups of costs (eg, a hospital unit's personnel costs) based on a patient's estimated usage of that resource, as well as the assignment of actual costs (eg, medication acquisition costs) based on a patient's actual usage of that resource. Virtually all costs are accounted for, and updates can be made both to cost methods and to the specification of which methods should be applied to which general ledger costs.
System architecture and primary system components
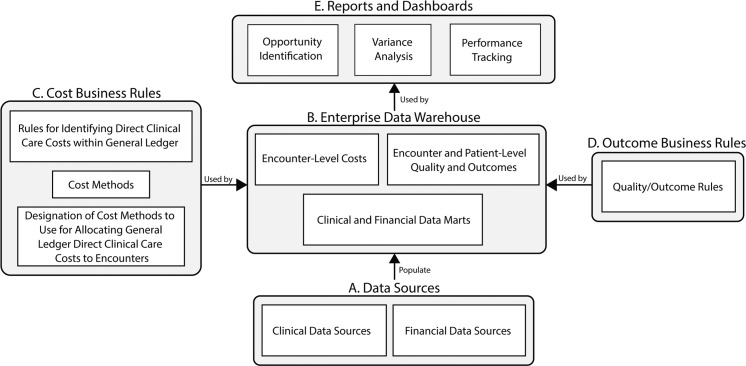
Figure 1 provides a high-level architectural overview. As is typical for an analytical tool leveraging a data warehouse,24 the VDO architecture includes layers for data sources, data marts, data analysis, and reporting. The various data sources (component A in figure 1) populate the Enterprise Data Warehouse (component B), where they are organized into clinical and financial data marts. Business rules are then applied to identify the general ledger costs attributable to direct patient care (component C). These direct clinical care costs are then allocated to individual encounters based on modular costing business rules (component C). Similarly, business rules for quality and outcome (component D) are used to define encounter and patient-level quality and outcome metrics. These cost and outcome data are then used within the reporting layer (component E) to provide actionable information to end users.
Figure 1:
Overview of system architecture. Letters refer to system components. Opportunity Identification = reports to identify potential opportunities for improving value. Variance Analysis = reports to analyze variance in care costs among care providers. Performance Tracking = reports to track performance over time with regard to both costs and outcomes.
Identification of direct clinical care costs
For facility costs, the identification of direct clinical costs is generally straightforward, as a healthcare facility has one primary mission—clinical care. For professional costs in the context of an academic healthcare system, the identification of direct clinical costs can be more challenging because physicians and their support staff may also engage in research and education. In the initial phase of VDO, direct professional clinical costs were identified by leveraging an existing annual faculty survey on effort allocation and an additional survey of clinical department administrators to identify expenses in the general ledger attributable to direct patient care. Business rules were then applied to identify direct professional costs (eg, direct clinical cost of physician = (salary + benefits) × (estimated % effort dedicated to clinical care)).
Costing methods for allocating costs to encounters
Table 1 provides an overview of the categories of costing methods that have been implemented for allocating identified direct care costs to encounters. Each method category can have multiple associated methods. For example, within the ‘actual cost’ method category, the pharmacy and supply costing methods are implemented as separate methods, as they use different algorithms to identify acquisition costs and encounter-level resource utilization.
Table 1:
Categories of costing methods and use before and after VDO implementation
| Costing method category | Example | Current use | % of total facility direct costs using costing method |
|
|---|---|---|---|---|
| Pre-VDO, fiscal year 2011 | Post-VDO, fiscal year 2013 | |||
| Actual cost | The cost of a surgical implant is determined from the supply management system and assigned to a given encounter based on actual use | Supplies Most medications Labs by external entity |
12.3 | 30.5 |
| Time-based allocation | The cost of operating the medical intensive care unit is identified by adding up all costs involved in running the unit, including labor, office supplies, equipment, etc. The per-hour cost is calculated by dividing the total cost by the total number of patient hours in the unit, and then costs are allocated to encounters based on actual hours spent in the unit. As another example, radiology technician cost is allocated according to the number of minutes an exam is estimated to take in the radiology scheduling system | Facility utilization (emergency department, inpatient units and operating room) Radiology |
13.5 | 32.6 |
| Work RVU-based allocation | A physician's clinical costs are compared to his or her total work RVUs in a given period to identify a cost per work RVU, where the work RVU is an estimate of the relative level of time, skill, training and intensity required by a clinician to provide a given clinical service.25 This per-RVU cost is multiplied by the work RVUs associated with a given patient encounter to allocate physician costs to an encounter | Professional costs | 0 | 0* |
| Quantity-based allocation | The cost of operating a procedural unit is identified by adding up all costs involved in running the unit. The per-procedure cost is calculated by dividing the total costs by the total number of procedures performed by the unit. The cost is then estimated by multiplying the number of procedures performed by the per-unit cost. | Respiratory therapy Counseling programs |
8.9 | 1.6 |
| Cost-to-cost ratio | The fee for laboratory management by a third party is allocated to individual labs in proportion to the item-level payments made to the third party for those labs | Laboratory management fee | 0 | 1.8 |
| Cost-to-charge ratio | The total cost for operating the cardiac catheterization unit is compared to the total charges billed by that unit. This information is used to generate a cost-to-charge ratio for the unit, and this ratio is applied to charges from a given encounter to estimate costs for that unit | Procedures without time estimates Medications for which acquisition costs are not available Labs done internally Air ambulance |
15.6 | 18.5† |
| Equal allocation among all encounters | The labor costs associated with operating an outpatient clinic are divided equally among all completed encounters at that clinic | Facility utilization (outpatient) | 0 | 9.9 |
| Equal allocation among encounters with facility charges | The labor costs associated with operating an outpatient clinic are divided equally among all encounters at that clinic that generated a charge | Anesthesiology Intravenous therapy Pre-transplant care |
49.6 | 5.2 |
*Work RVU-based allocation is not used for facility costs (the focus of this table). For professional costs, work RVU-based allocation was the sole costing method used for FY2013.
†The slight increase in the use of the cost-to-charge ratio in FY2013 reflects the use of this approach in areas previously costed through equal allocation among encounters with facility charges.
RVUs, relative value units; VDO, Value Driven Outcomes.
For each method category, table 1 outlines its current use and the proportion of total direct facility costs allocated using the approach before and after implementing VDO. VDO currently allocates all professional costs according to work relative value units (RVUs), whereas professional costing was not available before VDO.
Facility costs allocated using actual costs and time-based methods increased from 25.8% pre-implementation to 63.0% post-implementation. We prioritized the application of true costs and time-based methods to high-cost areas where required data were already being captured. We are currently pursuing the application of these cost methods to additional facility costs and to professional costs.
VDO enables the co-existence and incremental evolution of varying costing methods. For example, VDO currently considers the per-minute utilization cost for a given operating room to be the same across all surgeries. This method could be enhanced to account for differential resource utilization. For example, surgeries requiring more nurses could be allocated a higher per-minute cost than surgeries requiring fewer nurses, and surgeries involving the use of robotics systems could be allocated a higher per-minute cost than surgeries which do not. Such enhancements are iteratively implemented based on available resources and prioritization.
Technical details of implementation approach
Online supplementary appendix C provides detailed information on the VDO implementation approach. These technical details include the software and informatics approaches used in VDO, the software and data needed for replicating the VDO approach at other institutions, an entity-relationship diagram of the core VDO database tables, and detailed explanations of how source data are transformed into encounter-level costs using two representative VDO costing methodologies. Online supplementary appendix C also describes how data are organized to support drill-down capabilities in reports.
Costing timeframe and process
VDO provides cost analyses from fiscal year 2012 onward. The costing process is fully automated, takes approximately 4 h to execute, and is repeated monthly and at the end of each fiscal year. Following processing, financial professionals validate the results. Any identified issues, such as unexpected cost variance due to changes in the general ledger structure, are corrected before release of the data.
Quality, outcome, and value measurement
In addition to cost accounting, which is the focus of this manuscript, VDO supports the measurement and analysis of quality, outcome, and value. An overview of VDO's approach in this area is provided in online supplementary appendix D.
Reporting and analytics
Web-based reports enable end-users to efficiently engage with and analyze VDO data, which encompass the entire healthcare system and over 100 million rows of data based on over a million annual encounters. The reports are designed to be intuitive, with dropdown menus and filters that enable users to ‘slice and dice’ the data in real-time. Hover-over and drill-down capabilities are also heavily leveraged, and department-specific reports provide a customized experience while optimizing performance by limiting the dataset. The default, user-adjustable timeframe for most reports is a fiscal year.
Figures 2–6 provide samples of core VDO reports. The Opportunity Identification Report (figure 2) enables the identification of case types (by Diagnosis-Related Group (DRG) or International Classification of Diseases, 9th revision (ICD-9) diagnosis or procedure category) that are the most common, have the highest total costs, and/or have the largest coefficient of variation (SD/mean) for costs across attending physicians. In the example shown, among cardiothoracic surgery procedures with a common ICD-9 code, the insertion of an implantable heart assist system demonstrated the highest ‘relative rank,’ computed as the coefficient of variation multiplied by total costs. A related Opportunity Visualization Report (figure 3) provides this information more graphically. The hover-enabled bubbles represent case types, with bubble sizes reflecting the magnitude of the opportunity.
The Value Dashboard (figure 4) provides outcome metrics on the y-axis, average cost per visit on the x-axis, and bubbles to represent individual attending providers, with bubble sizes corresponding to case volumes. The example shown delineates the relationship between cost and 30-day readmission rates for patients hospitalized for sepsis.
The Physician Care Cost Dashboard (figure 5) compares average costs for specified case types stratified by attending provider and grouped into cost categories. Cost categories can be drilled down to individual orderables, enabling real-time investigation of the sources of intra-institutional cost variation. For the example shown, the average hip replacement cost was almost 70% higher for the highest-cost provider (leftmost bar) compared to the lowest-cost provider (rightmost bar), with the costs of the implant and facility utilization being the greatest drivers.
Finally, the Cost Trend Report (figure 6) provides costs for selected encounter types (intracranial injury in this case) over time. Additional reports are also available, with new reports being added iteratively based on need.
Evaluation
Implementation timeliness
A functioning prototype, including most core reports, was available 3 months into the project, and institutional leaders decided VDO was ready for production use as the institutional costing system 6 months into the project. Thus, the aggressive goals for implementation timeliness were fulfilled.
System performance
Thirty representative requests for the reports in figures 2–6 averaged 1.8 s (SD 0.8 s), with all requests taking less than the targeted 5 s.
Completeness
Total direct costs accounted for in VDO are generally within 0.5% of general ledger costs, and well under the target of 2%. Discrepancies may occur, for example, if a new clinic has been established and is incurring costs but has not yet begun to see patients. In such cases, because there are no encounters against which to allocate costs, costs appear in the general ledger but not in VDO.
Accuracy
As noted in table 1, facility direct costs allocated using actual costs and time-based methods have increased from 25.8% pre-VDO to 63.0% post-VDO implementation.
System extensibility
System extensibility has been validated through multiple iterative enhancements to the initial system. Major completed and in-progress enhancements include: a major hardware upgrade; the addition of multiple new reports; the enhancement of data interfaces; the development and incorporation of outcome metrics; and various enhancements to our costing methodologies.
End-user adoption
VDO data and reports are made available primarily to institutional decision makers such as service line directors, department chairs, and division chiefs. As of June 2014, there are 53 registered report users, and reports were accessed an average of 185 times per month during the first 6 months of 2014. Furthermore, many institutional stakeholders, including VDO team members, directly access VDO data through the data warehouse for custom analyses and reports.
Institutional leaders now use VDO to determine the profitability of individual clinical areas, which is then used to guide investment decisions. Also, VDO serves as the source of truth for a program that incentivizes physician-led value improvement efforts by transferring 50% of efficiency gains to those physicians’ clinical units. Furthermore, multiple value improvement initiatives use VDO to identify opportunities for process improvement and for assessing the impact of interventions and return on investment. We are also exploring the use of VDO for contract negotiations.
Ability to support value improvement
To date, in tandem with a health system-wide Lean management initiative, and in collaboration with the School of Business, over 50 value improvement initiatives have been initiated or evaluated using the VDO value analysis framework. These initiatives include bottom-up efforts conceived by frontline clinicians, as well as top-down efforts prioritized by service line directors and the Chief Medical Quality Officer using VDO.
User satisfaction
Of 79 invited survey participants, 47 (59%) responded, of whom 37 identified themselves as VDO users and were included in the analysis. As noted in table 2, users expressed satisfaction with VDO, in particular with regard to accuracy. Further details, including a summary of free-text comments, are available in online supplementary appendix B.
Table 2:
User satisfaction survey results
| Category | Question | Sample size* | Median (IQR) | % positive responses (4 or 5) |
|---|---|---|---|---|
|
Questions from Doll and Torkzadeh's validated survey instrument for end-user computing satisfaction23 Scale: 1—almost never, 2—some of the time, 3—about half of the time, 4—most of the time, 5—almost always | ||||
| Content | Overall responses for content-related questions below | 147 | 4 (4, 5) | 88 |
| Does VDO data provide the precise information you need? | 37 | 4 (4, 5) | 92 | |
| Does the VDO information content meet your needs? | 37 | 4 (4, 5) | 87 | |
| Does VDO provide data or reports that seem to be just about exactly what you need? | 37 | 4 (4, 5) | 84 | |
| Does VDO data provide sufficient information to support your work? | 36 | 4 (4, 5) | 89 | |
| Accuracy | Overall responses for accuracy-related questions below | 74 | 5 (4, 5) | 95 |
| Is VDO data accurate? | 37 | 5 (4, 5) | 95 | |
| Are you satisfied with the accuracy of VDO data? | 37 | 5 (4, 5) | 95 | |
| Format | Overall responses for format-related questions below | 72 | 4 (4, 5) | 93 |
| Do you think the VDO output is presented in a useful format? | 35 | 4 (4, 5) | 94 | |
| Is the VDO information clear? | 37 | 4 (4, 5) | 92 | |
| Ease of use | Overall responses for ease of use-related questions below | 72 | 4 (4, 5) | 81 |
| Are VDO data and reports user friendly? | 37 | 4 (4, 5) | 81 | |
| Are VDO data and reports easy to use? | 35 | 4 (4, 5) | 80 | |
| Timeliness | Overall responses for timeliness-related questions below | 67 | 4 (4, 5) | 90 |
| Do you get the information you need in time? | 31 | 4 (4, 5) | 87 | |
| Does VDO data provide up-to-date information? | 36 | 4 (4, 5) | 92 | |
|
Additional questions Scale: 1—strongly disagree, 2—disagree, 3—neither agree nor disagree, 4—agree, 5—strongly agree | ||||
| Overall | Overall responses for overall satisfaction questions below | 74 | 5 (4, 5) | 93% |
| Overall, I am satisfied with VDO. | 37 | 5 (4, 5) | 95% | |
| Overall, VDO is successful in enabling University of Utah Health Care to measure and improve care value. | 37 | 5 (4, 5) | 92% | |
*Sample size refers to the number of responses analyzed. Responses of N/A (not applicable to my use of VDO), which were allowed for all questions, were excluded from analysis. See online supplementary appendix B for methodology details.
VDO, Value Driven Outcomes.
Key challenges and solutions
We encountered several key challenges when implementing VDO. Online supplementary appendix E summarizes challenges we had anticipated and corresponding solutions we implemented or are considering for future implementation. These challenges included: changes in underlying data sources; the need to integrate information from multiple data sources; system performance; availability of required data; and the aggressive timeline. Of note, many of these anticipated issues, as well as the solutions devised, were related to core issues pertaining to the management and use of healthcare data warehouses in general.24,26
Furthermore, table 3 summarizes those challenges we had not anticipated, as well as potential solutions for those challenges.
Table 3:
Key unanticipated challenges and solutions
| Challenge | Example | Solutions | Comments |
|---|---|---|---|
| Identification of expenses attributable to clinical care within a school of medicine | A physician-scientist faculty member may conduct research, teach, and provide clinical care. Only the portion of his or her salary related to clinical care should be allocated to patient encounters as a direct clinical cost | Survey physicians and administrators regarding proportion of expenses (eg, physician salaries) that are attributable to patient care Capture the mission associated with expenses (clinical vs research vs education) as a part of the standard operating procedure |
UUHSC is currently enhancing frontline business processes to capture the mission associated with all expenses |
| Disclosure of provider identities | Surgeon A has significantly higher average costs for hip replacement surgery compared to his peers. Should his identity be visible to his division chief in VDO reports? How about to his surgical peers? | Hold open discussions to develop consensus on institutional approach to the issue Mask provider identities as the default and make provider identities available as required |
Opinions on this issue can differ significantly among providers Regardless of explicit identification, provider identities can often be inferred by other information provided, such as case volume |
| Sensitivity of cost data | Physician B holds admitting privileges at both the University Hospital and a competing hospital. Should the physician be provided full access to VDO cost data? | Establish clear institutional policies and procedures for access to the cost data Limit access to a need-to-know basis |
Accurate cost data can provide a competitive advantage, for example, for negotiating with healthcare payors The differences between costs and charges can present a public relations challenge if they are made public |
| Inherent heterogeneity of patients | Surgeon A has significantly higher average costs for hip replacement surgery compared to his peers. Is it because he is inefficient, or is it because his patients are more complex? | Define patient cohorts with greater precision, eg, patients with an elective, first-time hip replacement Search for and remove cost outliers from analyses, eg, a hip replacement case with significantly higher costs due to the patient having a congenital blood clotting disorder |
Inter-institutional comparisons with benchmark data oftentimes require the use of Medicare Severity Diagnosis-Related Groups (MS-DRGs) to categorize patients, whereas individual MS-DRGs oftentimes contain heterogeneous patient populations |
| Cost allocation method does not account for unused capacity of personnel time or resources | Allocation for imaging costs per unit time on an MRI scanner is based on total capital and operating costs divided by total time utilized. If the scanner is utilized only 75% of the time, the available capacity is not reflected in the cost allocation | Implement time-driven activity based costing (TD-ABC),27 which models the time required for tasks and enables the identification of excess capacity Recognize that with this approach, reconciliation with the general ledger requires accounting for capacity that was productively utilized and capacity that was not | UUHSC is collaborating with Harvard Business School to implement TD-ABC in several pilot projects |
| Indirect costs are allocated as a fixed percentage of direct costs | Whereas billing costs might be significantly higher for complex medical cases and readmissions than for routine outpatient visits, the indirect cost allocation is currently fixed at the same constant multiplier for all direct costs | Allocate indirect costs using TD-ABC Allocate indirect costs using more accurate methods, such as allocation of actual malpractice insurance costs by specialty, allocation of utility costs based on square footage, and allocation of human resource costs based on FTE count |
Inter-institutional benchmarking is difficult to conduct in this area due to limited national standards on what costs should be counted and how they should be allocated |
| Outcomes and quality metrics are numerous and varied for every case type, making presentation of overall ‘outcome’ versus cost challenging | For a procedure as routine as total joint replacement, important outcomes measurements include physical therapy timeliness, length of stay, use of spinal vs general anesthesia, readmission, Surgical Care Improvement Project (SCIP) measures, Hospital-Acquired Conditions (HAC) measures, and Patient Safety Indicator (PSI) measures, not to mention patient reported outcomes such as pain and recovery of function | Our providers have developed outcome indices which represent weighted averages of multiple important outcomes measured, which they refer to as ‘perfect care’ |
FTE, full time equivalent; UUHSC, University of Utah Health Sciences Center; VDO, Value Driven Outcomes.
Discussion
Understanding and improving care value is a key challenge facing healthcare delivery organizations as well as society. Here, we provide guidance on the design and implementation of a pragmatic, modular, and extensible technical platform for measuring and visualizing healthcare costs relative to outcomes.
Critical role of biomedical informatics
Traditionally, biomedical informatics has focused on the quality and outcomes component of the healthcare value equation. Today, as value becomes a central driving force for health care, it will be imperative for clinical informaticists to gain expertise in healthcare costing. Indeed, many of the challenges of healthcare costing—such as the need to integrate disparate data sources and to derive actionable information from data—are already core focal areas of biomedical informatics. Furthermore, accurate healthcare costs are required for properly evaluating the cost-effectiveness of informatics interventions.11 The increased use of cost data in health care also poses a myriad of operational and research questions directly relevant to clinical informatics, such as how best to attribute costs and profits to individual clinicians, as well as how to leverage cost-based incentives most effectively. Thus, it will be critical for value measurement and improvement to be integrated into the research and practice agenda of clinical informatics.
Importance of accuracy
Cost and related profitability data are used to inform significant decisions, including clinician compensation and the allocation of institutional resources. As a result, new ways of costing will inevitably lead to ‘winners and losers’. In our experience, it is critical that cost data are accurate and understandable, so as to avoid situations where stakeholders can simply claim that ‘the data are no good’. Key aspects of accuracy include the use of robust and transparent costing methodologies, as well as risk adjustment to account for the higher expected costs of more complicated cases. In our survey, VDO users reported being highly satisfied with data accuracy (table 2).
Limitations and strengths of approach
One limitation of VDO is that it has not been replicated elsewhere. Thus, while we believe the approach is generalizable, we lack empirical evidence to that effect. Also, VDO can support the analysis of indirect costs, but such costing has thus far been mostly out of the project scope. Finally, our approach requires electronic data sources and a data warehouse to function optimally, and these resources may not always be available. However, adoption of key health IT systems such as EHR systems is increasing rapidly in the USA,28 and our approach is specifically designed for incremental enhancement based on available capabilities.
A key advantage of VDO is its modularity and flexibility. Furthermore, the approach can be implemented relatively quickly, without the need for global adoption of highly resource-intensive activities such as time and motion studies. VDO also provides a variety of actionable reports and dashboards to identify top priorities for improvement, rapidly investigate potentially unwarranted variation in care, and monitor progress as care improvement interventions are instituted. Finally, the approach is designed to be transferable to other institutions.
Future directions
We are currently implementing major system enhancements, including the incorporation of various outcome metrics and the implementation of an improved approach to professional costing. Moreover, we are developing and refining systematic processes for leveraging VDO to improve care value, and we are exploring its use for contract negotiation and management. We are also actively investigating potential improvements to the underlying costing methodologies, such as through a collaboration with Professor Robert Kaplan of the Harvard Business School to incorporate time-driven activity-based costing methods that can enable better assessment of unused capacity.27 We also are exploring opportunities to enable other healthcare institutions to leverage our approach.
Conclusion
The measurement and improvement of care value is a critical imperative facing the US healthcare system. We speculate that the technical approach described in this manuscript will help guide other institutions’ efforts to address this challenge and improve both the efficiency and effectiveness of health care.
Acknowledgments
The authors wish to thank the numerous individuals who have contributed to the VDO initiative, including Dayle E Benson, MHA, John F Bohnsack, MD, Grant Lasson, MBA, and other members of the VDO Steering Committee; Jann Lefler, MBA, Jeffrey T Young, and other members of the Decision Support team; Brenda L Daurelle, MS, Michael B White, MD, MBA, Michael C Crotty, Michael S Sherwood, MSIS, and other members of the Enterprise Data Warehouse team; Brian Nordberg, Kristin Acree, MPH, David Browdy, MS, Kevin W Noonan, MBA, Stephen Petersen, MBA, and other members of the professional costing team; Christine M Turner, Darryl Barfuss, David Shields, and other members of the quality and outcomes team; Christine M Daniels, MS, MPA, Sandra Gulbransen, Michael Swanicke, MBA, Steven M Johnson, MBA, Collin Seabourne, MS, and Jace Manning, MBA from the Value Engineering team; David B Ryerse, Christopher L Fillmore, MD, MS, and all the business stakeholders who actively engaged with and supported the VDO project team. The authors also wish to thank Charlene R Weir, PhD, RN for assistance with the design of the user satisfaction survey, and Polina V Kukhareva, MS, MPH for assistance with the data analysis of the survey results.
Contributors
KK, CGP, and CH served as co-solution architects, and KK drafted the manuscript. KW and CJM created an initial prototype costing system upon which VDO was based and were instrumental to the design and implementation of the system. MT served as the principal architect for the technical solution and oversaw the development of the core costing processes. RAH, VGD, CJS, and BEB contributed to development of the costing methodologies from clinical systems and to clinical validation. SJM and MBF served as financial professionals overseeing the validity of the VDO approach in relation to the general ledger. AS served as the project manager. VSL oversaw the initiative as chair of the VDO Steering Committee, and JT, SJM, GLC, DEE, QLM, MBS, and RCP provided active direction and input as members of the Steering Committee. All authors contributed to the review and editing of the manuscript.
Funding
The work described in this manuscript was funded by the University of Utah Health Sciences Center. Use of the REDCap survey tool was supported by Clinical and Translational Sciences grant 8UL1TR000105 (formerly UL1RR025764).
Competing interests
The University of Utah Health Sciences Center is currently exploring potential options for maximizing the adoption and impact of Value Driven Outcomes, including potentially the provision of commercial products and services.
Ethics approval
University of Utah Institutional Review Board.
Provenance and peer review
Not commissioned; externally peer reviewed.
SUPPLEMENTARY MATERIAL
Supplementary material is available online at http://jamia.oxfordjournals.org/.
REFERENCES
- 1.Porter ME. What is value in health care? N Engl J Med 2010;363:2477–81. [DOI] [PubMed] [Google Scholar]
- 2.Cuckler GA, Sisko AM, Keehan SP, et al. National health expenditure projections, 2012–22: slow growth until coverage expands and economy improves. Health Aff (Millwood) 2013;32:1820–31. [DOI] [PubMed] [Google Scholar]
- 3.Organisation for Economic Co-operation and Development (OECD). OECD Health Data 2012: U.S. Health Care System from an International Perspective. http://www.oecd.org/unitedstates/HealthSpendingInUSA_HealthData2012.pdf (accessed 29 Sep 2013).
- 4.James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf 2013;9:122–8. [DOI] [PubMed] [Google Scholar]
- 5.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003;348:2635–45. [DOI] [PubMed] [Google Scholar]
- 6.Central Intelligence Agency. The World Factbook: Country Comparison—Life Expectancy at Birth. https://www.cia.gov/library/publications/the-world-factbook/rankorder/2102rank.html (accessed 29 Sep 2013).
- 7.Frakt AB, Mayes R. Beyond capitation: how new payment experiments seek to find the ‘sweet spot’ in amount of risk providers and payers bear. Health Aff (Millwood) 2012;31:1951–8. [DOI] [PubMed] [Google Scholar]
- 8.Husten L. Free Cardiac and Spine Surgery for Walmart Employees at Six Hospitals. 12 October 2012. http://www.forbes.com/sites/larryhusten/2012/10/12/free-cardiac-and-spine-surgery-for-walmart-employees-at-six-hospitals/ (accessed 29 Sep 2013).
- 9.Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harv Bus Rev 2011;89:46–52 54, 56–61 passim. [PubMed] [Google Scholar]
- 10.Porter ME, Lee TH. Why Health Care is Stuck—And How to Fix It. http://blogs.hbr.org/2013/09/why-health-care-is-stuck-and-how-to-fix-it/ (accessed 29 Sep 2013).
- 11.Ohno-Machado L. Cost-effectiveness of informatics and health IT: impact on finances and quality of care. J Am Med Inform Assoc 2012;19:327. [Google Scholar]
- 12.West TD, Balas EA, West DA. Contrasting RCC, RVU, and ABC for managed care decisions. A case study compares three widely used costing methods and finds one superior. Healthc Financ Manage 1996;50:54–61. [PubMed] [Google Scholar]
- 13.Cao P, Toyabe S, Akazawa K. Development of a practical costing method for hospitals. Tohoku J Exp Med 2006;208:213–24. [DOI] [PubMed] [Google Scholar]
- 14.Chiang B. Estimating nursing costs—a methodological review. Int J Nurs Stud 2009;46:716–22. [DOI] [PubMed] [Google Scholar]
- 15.Tan SS, Rutten FF, van Ineveld BM, et al. Comparing methodologies for the cost estimation of hospital services. Eur J Health Econ 2009;10:39–45. [DOI] [PubMed] [Google Scholar]
- 16.Barnett PG, Rodgers JH. Use of the Decision Support System for VA cost-effectiveness research. Med Care 1999;37(4 Suppl Va):AS63–70. [DOI] [PubMed] [Google Scholar]
- 17.Vogl M. Assessing DRG cost accounting with respect to resource allocation and tariff calculation: the case of Germany. Health Econ Rev 2012;2:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.James BC, Savitz LA. How Intermountain trimmed health care costs through robust quality improvement efforts. Health Aff (Millwood) 2011;30:1185–91. [DOI] [PubMed] [Google Scholar]
- 19.Vogl M. Improving patient-level costing in the English and the German ‘DRG’ system. Health Policy 2013;109:290–300. [DOI] [PubMed] [Google Scholar]
- 20.Bellanger MM, Tardif L. Accounting and reimbursement schemes for inpatient care in France. Health Care Manag Sci 2006;9:295–305. [DOI] [PubMed] [Google Scholar]
- 21.Oostenbrink JB, Rutten FF. Cost assessment and price setting of inpatient care in the Netherlands. The DBC case-mix system. Health Care Manag Sci 2006;9:287–94. [DOI] [PubMed] [Google Scholar]
- 22.O'Reilly J, Busse R, Hakkinen U, et al. Paying for hospital care: the experience with implementing activity-based funding in five European countries. Health Econ Policy Law 2012;7:73–101. [DOI] [PubMed] [Google Scholar]
- 23.Doll WJ, Torkzadeh G. The measurement of end-user computing satisfaction. MIS Q 1988;12:259–74. [Google Scholar]
- 24.Chute CG, Beck SA, Fisk TB, et al. The Enterprise Data Trust at Mayo Clinic: a semantically integrated warehouse of biomedical data. J Am Med Inform Assoc 2010;17:131–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glass KP, Anderson JR. Relative value units: from A to Z (Part I of IV). J Med Pract Manage 2002;17:225–8. [PubMed] [Google Scholar]
- 26.Dewitt JG, Hampton PM. Development of a data warehouse at an academic health system: knowing a place for the first time. Acad Med 2005;80:1019–25. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan RS, Anderson SR. Time-driven activity-based costing. Harv Bus Rev 2004;82:131–8, 50. [PubMed] [Google Scholar]
- 28.Office of the National Coordinator for Health IT. Health IT Adoption and Use Dashboard. http://dashboard.healthit.gov/HITAdoption (accessed 1 Oct 2013).