Abstract
There is a strong link between teamwork and patient safety. Emerging evidence supports the efficacy of teamwork improvement interventions. However, the availability of reliable, valid, and practical measurement tools and strategies is commonly cited as a barrier to long-term sustainment and spread of these teamwork interventions. This article describes the potential value of sensor-based technology as a methodology to measure and evaluate teamwork in healthcare. The article summarizes the teamwork literature within healthcare, including team improvement interventions and measurement. Current applications of sensor-based measurement of teamwork are reviewed to assess the feasibility of employing this approach in healthcare. The article concludes with a discussion highlighting current application needs and gaps and relevant analytical techniques to overcome the challenges to implementation. Compelling studies exist documenting the feasibility of capturing a broad array of team input, process, and output variables with sensor-based methods. Implications of this research are summarized in a framework for development of multi-method team performance measurement systems. Sensor-based measurement within healthcare can unobtrusively capture information related to social networks, conversational patterns, physical activity, and an array of other meaningful information without having to directly observe or periodically survey clinicians. However, trust and privacy concerns present challenges that need to be overcome through engagement of end users in healthcare. Initial evidence exists to support the feasibility of sensor-based measurement to drive feedback and learning across individual, team, unit, and organizational levels. Future research is needed to refine methods, technologies, theory, and analytical strategies.
Keywords: teamwork, patient safety, sensor-based measurement, team performance measurement
Breakdowns in teamwork and communication are an independent cause of, and a cross-cutting theme in, many of the system failures leading to patient harm.1–3 Teamwork improvement strategies can be effective,4,5 but the lack of ongoing measurement, evaluation, and feedback impedes sustainment of good team performance.6 Few valid and reliable teamwork measurement systems exist in healthcare, and labor costs associated with implementing these systems can be prohibitive.
Sensor-based technology offers a novel low-cost method for augmenting the current approaches to teamwork measurement. In turn, this creates an opportunity for medical informatics to contribute in new ways to teamwork improvement and patient safety. This article reviews the emerging literature and proposes a framework rooted in the science of teams for designing multi-method measurement systems for teamwork in healthcare.
TEAMWORK AND MEASUREMENT IN HEALTHCARE
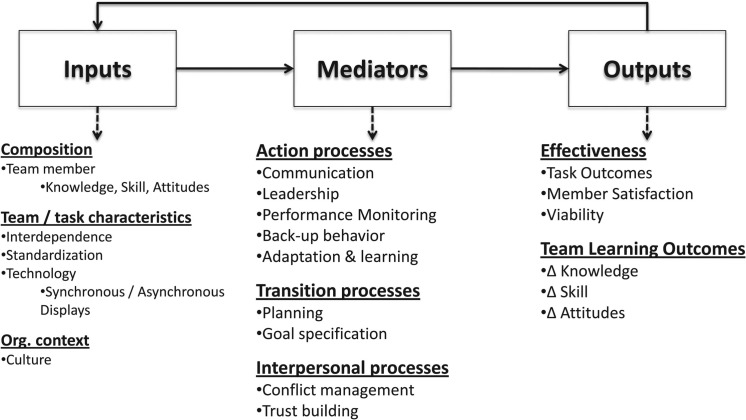
The large, multidisciplinary science of teams has informed the development of measurement systems.7–9 Figure 1 illustrates the input–mediator–output (IMO) framework underlying much of this research.9 Table 1 provides definitions from the science of teams and sensor-based measurement used here. Team ‘inputs’ are relatively stable features of the team, its members, the task and environment. Team ‘mediators’ are dynamic team member interactions (ie, processes) or transient products of interactions (ie, emergent states) that translate team inputs into team ‘outputs’ such as effectiveness, viability, and learning.
Figure 1:
Overview of input–mediator–output (IMO) framework and examples of dimensions of teamwork and factors influencing team effectiveness.
Table 1:
Key definitions from the science of teams and sensor-based measurement
| Teamwork definitions | A team consists of two or more individuals with specific roles working together interdependently and adaptively towards a shared goal.51 Teams can be partially or wholly distributed in space (ie, collocated vs virtual teams)52 and time (ie, using synchronous vs asynchronous communication technologies).53 |
| Taskwork is defined as clinical activities that do not demand interdependence (ie, tasks each team member complete without input from other team members).51 Understanding the taskwork of individuals in teams is important because of workload balancing (ie, team members must complete their individual tasks as well as their team tasks). | |
| Teamwork is defined as dynamic interactions among team members such as coordination and communication events.54 | |
| Team performance is defined as the summation of taskwork and teamwork activities.51 | |
| Team effectiveness is an assessment of the quality of team performance outcomes in relation to specified standards (ie, task outcomes, team member satisfaction and viability, learning outcomes).54 | |
| Multi-team systems (MTSs) are defined as a network of component teams that share at least one mutual goal that is interdependent with another team, although each component team may also pursue different objectives at times.55 | |
| Sensor-based measurement definitions | The terms sensors and sensor-based technology for human and team performance describe automated data collection tools including radio frequency identification (RFID) tags, infrared sensors, video and audio recording devices, and accelerometers56 implemented for the purpose of capturing real-time sociometric data (eg, behavior, speech analysis, proximity to other team members, devices, and workplace location). |
| Sensor-based measurement refers to the use of sensors to capture team performance data. Unlike traditional approaches to team performance measurement in healthcare, sensor-based measurement is automated and objective, and activity data are collected in real time. | |
| Activity traces are defined as information collected about team member interaction as a byproduct of completing tasks or using information systems. This includes an increasing array of data streams such as paging and phone systems, emails, and use patterns of and entries into electronic medical records. Such activity traces complement sensor-based technology, but do not dynamically capture sociometric data in a physical environment (ie, ‘sense’ behaviors, relative proximity, etc). |
There are two general methods for measuring teamwork: self-report and observation.10 Self-report methods involve asking team members to rate: themselves as individuals; their team; or the entire facility. These methods capture inherently subjective attitude competencies (eg, mutual trust, collective efficacy and orientation, psychological safety) as well as perceptions of teamwork,11 and have notable limitations, including systematic bias in self-ratings and challenges achieving adequate response rates.12–14 Observational measures incur labor costs of time spent observing, training, and monitoring raters over time.15 This can be a large investment in effort, up to 20 h for some systems,16 and largely limit observations to funded research. Although self-reporting and observation can serve critical roles in the training and periodic peer review processes, the frequency of feedback to clinicians likely remains low. Sensor-based measurement of teamwork (ie, use of sensors such as RFID (radio frequency identification) tags, audio recording, and video recording to capture team performance data) and activity traces (ie, information collected about team member interaction as a byproduct of task completion through email, paging, and electronic health record systems, for example) offer approaches to augment current capabilities.
Past reviews of team performance measurement in healthcare indicated a lack of tools with strong theoretical grounding and methodologically rigorous development and validation processes.17,18 More recent reviews indicate improvements in the quality of tools,19,20 with some notable exemplars.16,21–23 Continued progress in this area is needed, but the burdens of administration will probably constrain routine use. Less costly methods are needed to complement traditional approaches.
A FRAMEWORK FOR SENSOR-BASED MEASUREMENT OF TEAM PERFORMANCE
The traditional (self-report and observation) and novel (sensor-based measurement and activity traces) methods of team performance measurement each have unique strengths and weaknesses. Figure 2 presents the IMO framework and the emerging literature on sensor-based measurement of teams to illustrate factors to consider when building multi-method measurement systems. For team mediators—the primary focus of team measurement systems—the framework delineates how physical distribution of team members and the specificity of behavioral expectations for effective teamwork influence the utility of different measurement and analysis approaches. For team inputs and outputs, we describe applications of both direct and inference-based measurement. Table 2 summarizes existing validity evidence for sensor-based measurement of components of the IMO framework.
Figure 2:
Framework mapping applications of sensor-based measurement to the input–mediator–output (IMO) framework of team performance.
Table 2:
Summary of existing applications of sensors to team performance measurement
| Team inputs, mediators, and outputs | Feasibility evidence |
|---|---|
| Input: team composition—personality |
|
| Input: task structure and interdependence |
|
| Mediator: taskwork |
|
| Mediator: teamwork |
|
| Mediator: emergent states |
|
| Output: effectiveness |
|
| Output: staff satisfaction |
|
Team inputs
Sensor-based measurement can be applied to at least two categories of team inputs: team composition and task interdependence structures.
Team composition (ie, the mix of attributes of individual team members) greatly influences team processes and outcomes.24,25,26 Measuring team composition can be challenging in complex and dynamic work environments where team boundaries are permeable, individuals may be members of multiple teams, and team membership frequently changes.27 When combined with activity traces, sensors can help answer basic questions, such as who is currently on the team, and infer attributes of individual team members based on their interaction patterns. The existing literature on individual attributes pertains to personality traits,28,29 but could be broadened to include teamwork-related attitudes30,31 and individual teamwork competencies.
Task and interdependence structures (ie, the configuration of how task inputs and outputs are distributed across team members, and the types of interactions required to complete tasks) influence team outcomes.32 In healthcare, many work practices appear to have evolved over time, rather than being engineered.33 Sensor-based measurement of teamwork can descriptively map these organic interdependence structures within a unit or facility, explore variations in work practices, and ultimately develop alternative methods of organizing teams. For example, using a more traditional survey-based social network analysis approach, Effken and colleagues34 showed that communication patterns within units correlated with safety and quality metrics. Higher levels of adverse drug events were associated with higher levels of betweenness centrality (ie, more information gatekeepers). Sensor-based measurement can capture these types of structural attributes of teamwork in a low-cost way.
Team mediators
Strengths and weaknesses of different measurement approaches can be delineated on two dimensions: (1) the physical distribution of team members, and (2) the specificity of behavioral expectations for effective teamwork. First, physical distribution of team members varies dramatically in healthcare organizations (eg, a surgical team with primarily colocated members; a cancer treatment multi-team system with primarily distributed team members) as well as within teams (eg, an intensive care unit with phases of collocated—rounds—and distributed activity). Second, as with the technical work,35 expectations for teamwork behaviors are highly specified in certain situations (eg, protocolized cardiac or trauma resuscitations) and much less specified in others. Self-report methods are equally applicable across these team configurations and situations, but physical distribution and specificity of expectations have unique implications for the relevance of observation, sensor-based, and activity trace methods as well as for the appropriateness of analysis techniques applied to the data collected.
Physical distribution primarily affects the relevance of sensor-based measurement and activity trace data. Sensor-based measurement of teamwork primarily detects face-to-face interaction patterns including proximity and conversational dynamics. As the physical distribution of teams and multi-team systems decreases, the relevance of sensor-based measurement is likely to increase. As physical distribution increases, the relevance of activity traces is likely to increase because these data are captured primarily through interaction in distributed communication systems (eg, emails, pages, texts, entries into electronic medical records). Understanding when and how the physical distribution of a team may vary over time is necessary for planning an appropriate measurement system. However, aside from entirely colocated or entirely distributed teams, most situations will call for a blended approach using both sensor-based measurement and activity traces to capture a team's interaction patterns. Olguín and colleagues36 found that staff satisfaction was significantly associated with the total amount of communication measured through both sensors and activity traces, but not with each measure of communication in isolation.
The degree of behavioral specificity of expectations for effective teamwork has implications for observational methods and analysis techniques applied to sensor-based measurement. For observational methods, structured observation is applicable with high degrees of behavioral specificity, and unstructured or ethnographic observation with low specificity of performance expectations. Similarly, methods of analysis for sensor-based measures emphasizing the detection of a priori defined patterns of interaction will be most relevant for areas of a team's work with defined behavioral expectations. For example, Vankipuram et al.37 identified very specific interaction patterns in sensor-based measures of teamwork in trauma resuscitation teams with highly protocolized interactions. Conversely, more exploratory or descriptive analysis methods are appropriate in areas of low behavioral specificity. In a pediatric unit with relatively low specificity of teamwork expectations, Isella and colleagues38 applied an exploratory analytical approach to discover patterns of interaction that could be targeted to prevent infections.
Team outputs
Sensor-based measures of teamwork can be applied to at least three categories of team outputs: task efficiency, team learning, and affective outcomes. Task efficiency is the most straightforward where sensor-based measurements of teamwork capture reaction times to alerts and alarms. Assessing team learning through sensor-based measurements can include evaluating changes in a priori defined patterns of effective and ineffective teamwork, or changes in more descriptive measures of communication structures. Affective team outcomes, such as staff satisfaction, can be inferred through analyzing patterns of team interaction.29
Summary
Sensor-based measurement is one of several strategies for evaluating teamwork. It is most applicable for teams, or phases of team performance, where members are at least partially colocated. Different analytical approaches should be applied to sensor-based measurement data collected in aspects of work with high (ie, prospective pattern-detection methods such as tensor decomposition described below) versus low (ie, exploratory techniques) specificity of behavioral team performance expectations. This review has focused primarily on sensor-based measurement and not activity traces, reflecting a disproportionately low number of studies on activity traces used for team performance measurement and indicating a strong need for work in this area.
APPLICATIONS: MULTILEVEL PERFORMANCE EVALUATION AND LEARNING
Sensor-based measurement can contribute to interventions for improving individual, team, unit, and organizational learning in healthcare. For individuals, sensor-based measurement can provide real-time support for clinicians to balance their individual workload efforts and provide feedback on the quantity and quality of interactions with other clinicians or patients. For teams, sensor-based measurement can serve to augment traditional methods of team improvement, such as self-guided team reflective activities,39,40 by providing visualization of performance patterns to aid diagnosis of performance deficits. Unit-level learning involves the detection of work system issues that can be addressed through policies, procedures, equipment, work processes, staffing, and so forth.41 Sensor-based measurement can automate process mapping in an ongoing way to identify bottlenecks in flow or other inefficiencies. Mechanisms for sharing innovation and knowledge within an organization are a marker of high reliability and safety.42 Widespread adoption of sensor-based measurement can provide an analog to aviation's flight data recorder, allowing playback of real events in simulated environments and sharing knowledge generated from that experience.43
ANALYTICAL STRATEGIES
Sensor-based measurement captures a dynamic network of who interacts with whom, and when, where, and how, together with myriad covariates and dependent variables. Dynamic network analysis involves visualization, exploratory data analysis, and statistical inference. Methods exist for simple Euclidean representation of time series of graphs, and inference thereon.44–47 Recent theoretical results have proven this representation of the dynamic network to be a principled representation for visualization, exploratory data analysis, and quantitative statistical inference regarding team-based causes and effects for the evaluation of teamwork and the development of improvement strategies.
DISCUSSION
Teamwork is critical for safe patient care. Interventions can improve teamwork, but their impact is limited by the absence of reliable, valid, and practical measurement approaches. Sensor-based measurement can augment existing approaches and improve access to developmental and real-time feedback on team interactions. There is much to learn, both in the science and practice of this new domain. The initial work is exciting and encouraging, but new methods, technologies, theories, and analytical approaches must be developed and refined to make the most of this approach.
Managing the cultural complexities of implementing sensor systems may be one of the biggest challenges. Building trust in the system will be critical, or staff will devise workarounds to corrupt the quality and utility of the data.48,49 Privacy and security concerns associated with accessing these data must be addressed. The aviation industry faced a similar crossroads in the 1960s, when the introduction of cockpit voice recorders depended on ‘the bold support of the airline pilots and the wisdom of the aviation community’50 (p6). However, to reach the ultimate outcomes of improved safety and quality, team performance measurement must be put to use.
CONCLUSION
Large practical benefits to care providers, patients, and their loved ones can be realized by addressing the technical, theoretical, cultural, and methodological issues involved in sensor-based measurement. Consequently, this represents a problem where practical application can drive fundamental advancements in our conceptual understanding of human dynamics and technological capability.
ACKNOWLEDGEMENTS
We would like to thank Julie A Wu, PhD for comments and suggestions on a previous version of this manuscript.
CONTRIBUTORS
All authors contributed to the conception and design of the work and drafting and critically revising the manuscript. All authors gave final approval and agree to be accountable for the integrity of the work.
FUNDING
This work was partially supported by the Gordon and Betty Moore Foundation, grant number 113703 (to PP, the principal investigator).
COMPETING INTERESTS
None.
PROVENANCE AND PEER REVIEW
Not commissioned; externally peer reviewed.
REFERENCES
- 1.Levinson DR, General I. Adverse events in hospitals: national incidence among Medicare beneficiaries. Department of Health & Human Services, 2010. [Google Scholar]
- 2.Kohn LT, Corrigan JM, Donaldson MS. eds. To err is human: Building a safer health system. Washington, DC: National Academy Press, 2000. [PubMed] [Google Scholar]
- 3.Pham JC, Aswani MS, Rosen M, et al. Reducing medical errors and adverse events. Annu Rev Med 2012;63:447–63. [DOI] [PubMed] [Google Scholar]
- 4.Weaver SJ, Dy SM, Rosen MA, et al. Team-training in healthcare: a narrative synthesis of the literature. BMJ Qual Saf 2014;23:359–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buljac-Samardzic M, Dekker-van Doorn CM, van Wijngaarden JD, et al. Interventions to improve team effectiveness: a systematic review. Health Policy 2010;94:183–95. [DOI] [PubMed] [Google Scholar]
- 6.Salas E, Almeida SA, Salisbury M, et al. What are the critical success factors for team training in health care? Jt Comm J Qual Patient Saf 2009;35:398–405. [DOI] [PubMed] [Google Scholar]
- 7.Salas E, Rosen MA, Burke CS, et al. The wisdom of collectives in organizations: an update of the teamwork competencies. Team effectiveness in complex organizations: cross-disciplinary perspectives and approaches. New York: Routledge, 2009:39–79. [Google Scholar]
- 8.Kozlowski SW, Ilgen DR. Enhancing the effectiveness of work groups and teams. Psychol Sci Public Interest 2006;7:77–124. [DOI] [PubMed] [Google Scholar]
- 9.Ilgen DR, Hollenbeck JR, Johnson M, et al. Teams in organizations: From input-process-output models to IMOI models. Annu Rev Psychol 2005;56:517–43. [DOI] [PubMed] [Google Scholar]
- 10.Rosen MA, Schiebel N, Salas E, et al. How can team performance be measured, assessed, and diagnosed? In: Salas E, Frush K. eds. Improving patient safety through teamwork and team training. Oxford, UK: Oxford University Press, 2012:59–79. [Google Scholar]
- 11.Malec JF, Torsher LC, Dunn WF, et al. The Mayo high performance teamwork scale: reliability and validity for evaluating key crew resource management skills. Simulation Healthc 2007;2:4–10. [DOI] [PubMed] [Google Scholar]
- 12.Dunning D, Johnson K, Ehrlinger J, et al. Why people fail to recognize their own incompetence. Current Dir Psychol Sci 2003;12:83–7. [Google Scholar]
- 13.Hodges B, Regehr G, Martin D. Difficulties in recognizing one's own incompetence: novice physicians who are unskilled and unaware of it. Acad Med 2001;76:S87–9. [DOI] [PubMed] [Google Scholar]
- 14.Kruger J, Dunning D. Unskilled and unaware of it: How difficulties in recognizing one's own incompetence lead to inflated self-assessments. J Pers Soc Psychol 1999;77:1121–34. [DOI] [PubMed] [Google Scholar]
- 15.Feldman M, Lazzara EH, Vanderbilt AA, et al. Rater training to support high-stakes simulation-based assessments. J Contin Educ Health Prof 2012;32:279–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hull L, Arora S, Kassab E, et al. Observational teamwork assessment for surgery: content validation and tool refinement. J Am Coll Surg 2011;212:234–43 e5. [DOI] [PubMed] [Google Scholar]
- 17.Jeffcott SA, Mackenzie CF. Measuring team performance in healthcare: review of research and implications for patient safety. J Crit Care 2008;23:188–96. [DOI] [PubMed] [Google Scholar]
- 18.Rosen MA, Weaver SJ, Lazzara EH, et al. Tools for evaluating team performance in simulation-based training. J Emergencies Trauma Shock 2010;3:353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Havyer RD, Wingo MT, Comfere NI, et al. Teamwork assessment in internal medicine: a systematic review of validity evidence and outcomes. J Gen Intern Med 2014;29:894–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dietz A, Pronovost PJ, Benson K, et al. A systematic review of behavioral marker systems in healthcare: what do we know about their attributes, validity, and application? BMJ Qual Safety. In Press. [DOI] [PubMed] [Google Scholar]
- 21.Fletcher G, Flin R, McGeorge P, et al. Anaesthetists’ Non-Technical Skills (ANTS): evaluation of a behavioural marker system. Br J Anaesth 2003;90:580–8. [DOI] [PubMed] [Google Scholar]
- 22.Yule S, Flin R, Maran N, et al. Surgeons’ non-technical skills in the operating room: reliability testing of the NOTSS behavior rating system. World J Surg 2008;32:548–56. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell L, Flin R, Yule S, et al. Evaluation of the scrub practitioners’ list of intraoperative non-technical skills (SPLINTS) system. Int J Nurs Stud 2012;49:201–11. [DOI] [PubMed] [Google Scholar]
- 24.Peeters MA, Van Tuijl HF, Rutte CG, et al. Personality and team performance: a meta-analysis. Eur J Pers 2006;20:377–96. [Google Scholar]
- 25.Bell ST. Deep-level composition variables as predictors of team performance: a meta-analysis. J Appl Psychol 2007;92:595. [DOI] [PubMed] [Google Scholar]
- 26.Bowers CA, Pharmer JA, Salas E. When member homogeneity is needed in work teams a meta-analysis. Small Group Res 2000;31:305–27. [Google Scholar]
- 27.Mathieu JE, Tannenbaum SI, Donsbach JS, et al. A review and integration of team composition models moving toward a dynamic and temporal framework. J Managt 2014;40:130–60. [Google Scholar]
- 28.Mehl MR, Gosling SD, Pennebaker JW. Personality in its natural habitat: Manifestations and implicit folk theories of personality in daily life. J Pers Soc Psychol 2006;90:862. [DOI] [PubMed] [Google Scholar]
- 29.Wearable sensors for pervasive healthcare management. Pervasive Computing Technologies for Healthcare, 2009. PervasiveHealth 2009. 3rd International Conference on: IEEE; 2009. [Google Scholar]
- 30.Costa AC. Work team trust and effectiveness. Personnel Rev 2003;32:605–22. [Google Scholar]
- 31.Edmondson A. Psychological safety and learning behavior in work teams. Adm Sci Q 1999;44:350–83. [Google Scholar]
- 32.Saavedra R, Earley PC, Van Dyne L. Complex interdependence in task-performing groups. J Appl Psychol 1993:78:61. [Google Scholar]
- 33.Durso FT, Drews FA. Health care, aviation, and ecosystems a socio-natural systems perspective. Curr Dir Psychol Sci 2010;19:71–5. [Google Scholar]
- 34.Effken JA, Carley KM, Gephart S, et al. Using ORA to explore the relationship of nursing unit communication to patient safety and quality outcomes. Int J Med Inform 2011;80:507–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rosen MA, Pronovost PJ. Advancing the use of checklists for evaluating performance in health care. Acad Med 2014;89:963–5. [DOI] [PubMed] [Google Scholar]
- 36.Olguín DO, Waber BN, Kim T, et al. Sensible organizations: technology and methodology for automatically measuring organizational behavior. IEEE Trans Syst Man Cybern B Cybern 2009;39:43–55. [DOI] [PubMed] [Google Scholar]
- 37.Vankipuram M, Kahol K, Cohen T, et al. Toward automated workflow analysis and visualization in clinical environments. J Biomed Inform 2011;44:432–40. [DOI] [PubMed] [Google Scholar]
- 38.Isella L, Romano M, Barrat A, et al. Close encounters in a pediatric ward: measuring face-to-face proximity and mixing patterns with wearable sensors. PLoS ONE 2011;6:e17144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tannenbaum SI, Cerasoli CP. Do team and individual debriefs enhance performance? A meta-analysis. Hum Factors 2013;55:231–45. [DOI] [PubMed] [Google Scholar]
- 40.Smith-Jentsch KA, Cannon-Bowers JA, Tannenbaum SI, et al. Guided team self-correction impacts on team mental models, processes, and effectiveness. Small Group Res 2008;39:303–27. [Google Scholar]
- 41.Rosen MA, Hunt EA, Pronovost PJ, et al. In situ simulation in continuing education for the health care professions: a systematic review. J Contin Educ Health Prof 2012;32:243–54. [DOI] [PubMed] [Google Scholar]
- 42.Keroack MA, Youngberg BJ, Cerese JL, et al. Organizational factors associated with high performance in quality and safety in academic medical centers. Acad Med 2007;82:1178–86. [DOI] [PubMed] [Google Scholar]
- 43.Kannampallil T, Li Z, Zhang M, et al. Making sense: sensor-based investigation of clinician activities in complex critical care environments. J Biomed Inform 2011;44:441–54. [DOI] [PubMed] [Google Scholar]
- 44.Priebe CE, Conroy JM, Marchette DJ, et al. Scan statistics on enron graphs. Comput Math Organ Theory 2005;11:229–47. [Google Scholar]
- 45.Lee NH, Priebe CE. A latent process model for time series of attributed random graphs. Stat Inference Stochastic Process 2011;14:231–53. [Google Scholar]
- 46.Sussman DL, Tang M, Fishkind DE, et al. A consistent adjacency spectral embedding for stochastic blockmodel graphs. J Am Stat Assoc 2012;107:1119–28. [Google Scholar]
- 47.Lee NH, Tang M, Yoder J, et al. On latent position inference from doubly stochastic messaging activities. Multiscale Modeling Simulation 2013;11:683–718. [Google Scholar]
- 48.Hansen TR, Bardram JE, Soegaard M. Moving out of the lab: deploying pervasive technologies in a hospital. Pervasive Comput IEEE 2006;5:24–31. [Google Scholar]
- 49.Yao W, Chu C, Li Z. The adoption and implementation of RFID technologies in healthcare: a literature review. J Med Syst 2012;36:3507–25. [DOI] [PubMed] [Google Scholar]
- 50.National Transportation Safety Board. Safety Recommendation A-00-30 and -31. http://www.ntsb.gov/doclib/recletters/2000/A00_30_31.pdf. Published April 2000 (accessed 19 Dec 2013).
- 51.Salas E, Dickinson TL, Converse S, et al. Toward an understanding of team performance and training. In: Swezey RW, Salas E. eds. Teams: their training and performance. Norwood, NJ: Ablex, 1992:3–29. [Google Scholar]
- 52.Kirkman BL, Rosen B, Tesluk PE, et al. The impact of team empowerment on virtual team performance: the moderating role of face-to-face interaction. Acad Manage J 2004;47:175–92. [Google Scholar]
- 53.Fiore SM, Rosen MA, Smith-Jentsch KA, et al. Toward an understanding of macrocognition in teams: predicting processes in complex collaborative contexts. Hum Factors 2010;52:203–24. [DOI] [PubMed] [Google Scholar]
- 54.Salas E, Cooke NJ, Rosen MA. On teams, teamwork, and team performance: discoveries and developments. Hum Factors 2008;50:540–7. [DOI] [PubMed] [Google Scholar]
- 55.Marks MA, DeChurch LA, Mathieu JE, et al. Teamwork in multiteam systems. J Appl Psychol 90:964–71. [DOI] [PubMed] [Google Scholar]
- 56.Parlak S, Sarcevic A, Marsic I, et al. Introducing RFID technology in dynamic and time-critical medical settings: requirements and challenges. J Biomed Inform 2012;45:958–74. [DOI] [PubMed] [Google Scholar]
- 57.Hendrich A, Chow MP, Skierczynski BA, et al. A 36-hospital time and motion study: how do medical-surgical nurses spend their time? Perm J 2008;12:25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kranzfelder M, Schneider A, Gillen S, et al. New technologies for information retrieval to achieve situational awareness and higher patient safety in the surgical operating room: the MRI institutional approach and review of the literature. Surg Endosc 2011;25:696–705. [DOI] [PubMed] [Google Scholar]