Abstract
Objective:
Given conflicting data regarding the association of HIV infection and ischemic stroke risk, we sought to determine whether HIV infection conferred an increased ischemic stroke risk among male veterans.
Methods:
The Veterans Aging Cohort Study–Virtual Cohort consists of HIV-infected and uninfected veterans in care matched (1:2) for age, sex, race/ethnicity, and clinical site. We analyzed data on 76,835 male participants in the Veterans Aging Cohort Study–Virtual Cohort who were free of baseline cardiovascular disease. We assessed demographics, ischemic stroke risk factors, comorbid diseases, substance use, HIV biomarkers, and incidence of ischemic stroke from October 1, 2003, to December 31, 2009.
Results:
During a median follow-up period of 5.9 (interquartile range 3.5–6.6) years, there were 910 stroke events (37.4% HIV-infected). Ischemic stroke rates per 1,000 person-years were higher for HIV-infected (2.79, 95% confidence interval 2.51–3.10) than for uninfected veterans (2.24 [2.06–2.43]) (incidence rate ratio 1.25 [1.09–1.43]; p < 0.01). After adjusting for demographics, ischemic stroke risk factors, comorbid diseases, and substance use, the risk of ischemic stroke was higher among male veterans with HIV infection compared with uninfected veterans (hazard ratio 1.17 [1.01–1.36]; p = 0.04).
Conclusions:
HIV infection is associated with an increased ischemic stroke risk among HIV-infected compared with demographically and behaviorally similar uninfected male veterans.
HIV infection in the highly active antiretroviral therapy (HAART) era is associated with coronary heart disease and hemorrhagic stroke.1–5 Most investigations regarding HIV and ischemic stroke come from pre-HAART studies and were limited to younger patients and those with AIDS.6,7
People infected with HIV are living longer. Aging, conditions associated with aging (e.g., hypertension and atrial fibrillation), and HAART-related toxicities (e.g., dyslipidemia, impaired glucose tolerance) may all increase the risk of ischemic stroke.8,9 Hepatitis C virus (HCV) infection, common among HIV-infected people, may also increase vascular risk.1,10–12 Duration of HIV infection and its associated chronic inflammatory state may also increase the risk of stroke.13 Large studies comparing ischemic stroke risk in HIV-infected patients with demographically and behaviorally similar uninfected patients in the HAART era are lacking.14–16 Recently, HIV infection was found to be an independent risk factor for acute ischemic stroke among women, but not men,17 conflicting with findings from another large, recent study with an uninfected comparator group from within the same health care system18 and a cohort of HIV-infected and uninfected men.16 These important studies included an uninfected comparator group of subjects who had a lower burden of comorbid disease associated with stroke despite age, sex, and race matching.
We examined the independent association between HIV and ischemic stroke in a relatively older, male population in the early HAART era, with uninfected comparators who had a similar (or higher) burden of comorbid disease.
METHODS
Patients.
The Veterans Aging Cohort Study–Virtual Cohort (VACS-VC) is a cohort of veterans with HIV infection each matched to 2 uninfected veterans on age, sex, race/ethnicity, and geographical location. Participants were identified from United States Veterans Affairs (VA) administrative data starting in 1998 using a modified existing algorithm.19 This cohort consists of data from the immunology case registry; the VA HIV registry; the pharmacy benefits management database; the decision support system, a national database of VA clinical and laboratory data; and the National Patient Care Database, and health factors data collected from physician clinical reminders within the VA electronic medical record system. The institutional review boards at the University of Pittsburgh, Yale University, and the West Haven VA Medical Center approved this study.
All participants alive and enrolled in the VACS-VC on or after 2003 (n = 99,688) were eligible for the current study. Baseline was a participant's first clinical encounter on or after April 1, 2003. After excluding women and participants with baseline cardiovascular disease (CVD) (i.e., coronary heart disease, acute myocardial infarction, cardiovascular revascularization, or heart failure) and stroke (ischemic/hemorrhagic), our final sample size was 76,835 veterans (33% HIV-infected). Prevalent CVD and stroke were identified by the occurrence of ICD-9-CM20 codes at any time before and up to 6 months after their baseline date. All participants in the final sample were followed from their baseline date to either an ischemic stroke event, death, or the date of last follow-up. All analyses were truncated to December 31, 2009, to correspond with the end of our event data.
Independent variable.
The presence of HIV infection was defined as a participant with ≥1 inpatient and/or ≥2 outpatient ICD-9 codes for HIV infection and confirmed by the participant's presence in the VA immunology case registry.19
Dependent variable.
Incident ischemic stroke was defined as ≥1 inpatient and/or ≥2 outpatient ICD-9 codes for the diagnosis. These included occlusion and stenosis of precerebral arteries (433.x1), occlusion of cerebral arteries, excluding cerebral thrombosis/embolism without infarction (434, excluding 434.x0), and acute but ill-defined cerebrovascular disease (436).21 Prior work in the Cardiovascular Health Study and elsewhere has demonstrated high agreement of these codes with formal chart adjudication (positive predictive value = 81.6%–90.0%, κ = 0.86).2,20,22 Incident hemorrhagic strokes defined by ICD-9 codes were excluded, except where an ischemic stroke later underwent hemorrhagic transformation.
Covariates.
Sociodemographic data included age in 10-year increments, sex, and race/ethnicity. Hypertension, diabetes, dyslipidemia, renal disease, and anemia were measured using outpatient and clinical laboratory data closest to the baseline date. Medications including 3-hydroxy-3-methylglutaryl–coenzyme A (HMG-CoA) reductase inhibitor use and antiretroviral therapy were based on pharmacy data, and body mass index and smoking were measured from the health factors data, which contains information collected from clinical reminders that providers are required to complete on patients. Hypertension was defined as nonhypertensive (<140/90 mm Hg and no evidence of medication therapy), controlled hypertensive (<140/90 mm Hg but on medication), and uncontrolled hypertension (>140/90 mm Hg).23 Blood pressure measurement was the average of the 3 routine outpatient clinical measurements closest to the baseline date. Diabetes was defined using a combination of an abnormal glucose measurement, use of insulin or oral hypoglycemic agents, and/or ICD-9 codes.24 Dyslipidemia was defined as triglycerides ≥150 mg/dL, high-density lipoprotein <40 mg/dL, or low-density lipoprotein ≥160 mg/dL. HMG-CoA reductase inhibitor use was within 180 days of the baseline date. Smoking was defined as current, past, and never smoking based on documentation from the VA electronic medical record health factor dataset. Our prior work demonstrates a high agreement between participant self-completed smoking data from the VACS and health factors data (agreement = 79.5%, κ = 0.66).25 HCV infection was defined as a positive HCV antibody test or ≥1 inpatient and/or ≥2 outpatient codes for this diagnosis.26 Alcohol abuse or dependence, cocaine abuse or dependence, and atrial fibrillation (427.31) were defined using ICD-9 codes.27,28
We also collected data on baseline CD4+ cell counts, HIV-1 RNA levels, and HAART. Baseline CD4+ cell counts and HIV-1 RNA levels were collected within 180 days of our baseline date. Baseline antiretroviral therapy use was defined as use of nonnucleoside reverse transcriptase inhibitor, nucleoside reverse transcriptase inhibitor, and protease inhibitor, within 180 days of the baseline date. We have previously shown within a nested sample of veterans with HIV infection that 98% receive antiretroviral therapy within the VA.19
Statistical analysis.
We assessed all descriptive statistics using t tests or its nonparametric counterpart for continuous variables and χ2 test for categorical variables. Among those with ischemic stroke, risk factors were compared by HIV status. We calculated age- and race/ethnicity-adjusted incident ischemic stroke rates per 1,000 person-years. Cox proportional hazard models were used to estimate the hazard ratio (HR) and confidence intervals (CIs) for incident ischemic stroke associated with HIV status after adjusting for demographics, traditional ischemic stroke risk factors, comorbidities, and substance use. Secondary analyses stratified HIV status by CD4+ T-cell count, HIV-1 RNA levels, and HAART use. The proportional hazards assumption was assessed using the Grambsch-Therneau method and was not violated for any analyses.29 Given the low percentage of women in the cohort and prior work suggesting an interaction by sex on the effect of HIV on stroke risk, women were excluded from these analyses. Multiple imputation techniques were used to include missing data into these analyses; these techniques generated 5 datasets with complete covariance values, increasing the robustness and efficiency of estimated HRs.
Standard protocol approvals, registrations, and patient consents.
The development of VACS-VC was approved by the institutional review boards of the VA Connecticut Healthcare System and Yale University School of Medicine, granted a waiver of informed consent, and is HIPAA (Health Insurance Portability and Accountability Act)-compliant.
RESULTS
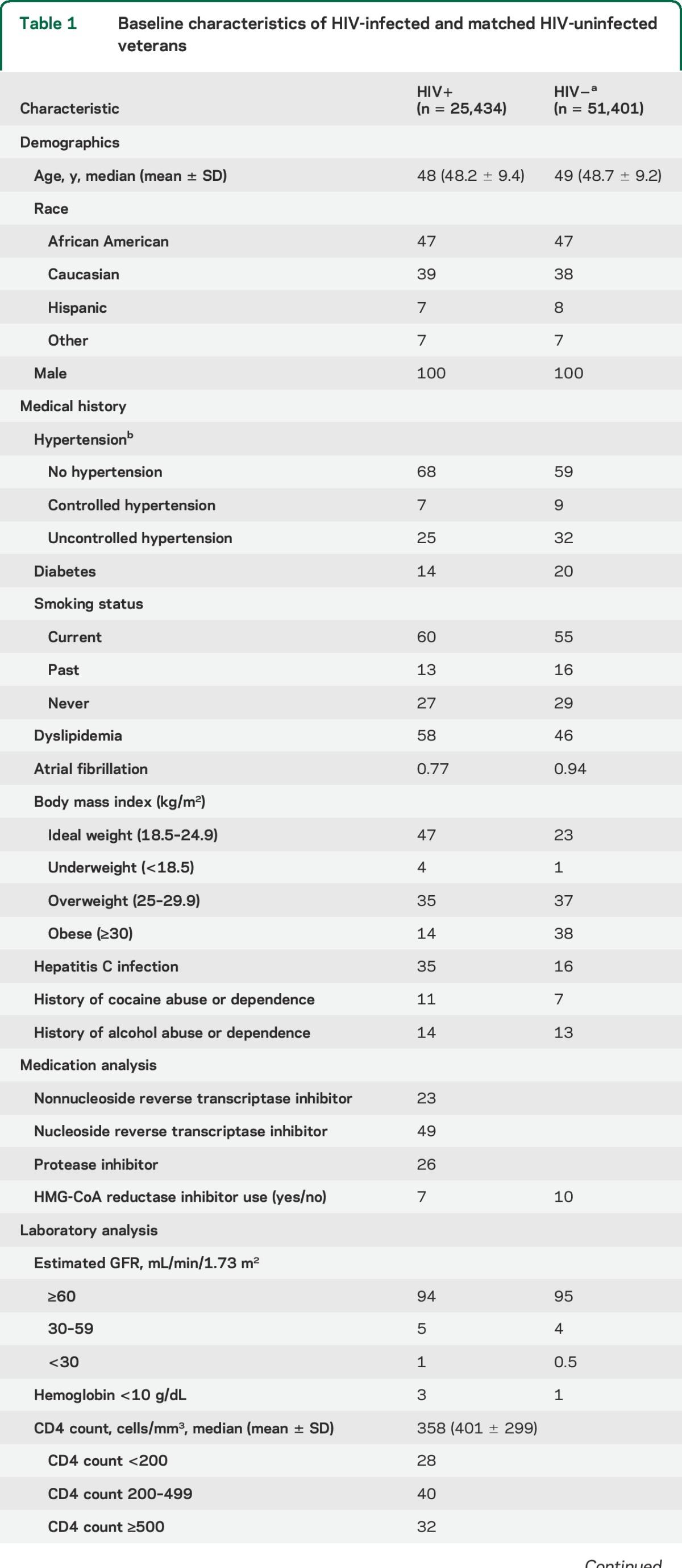
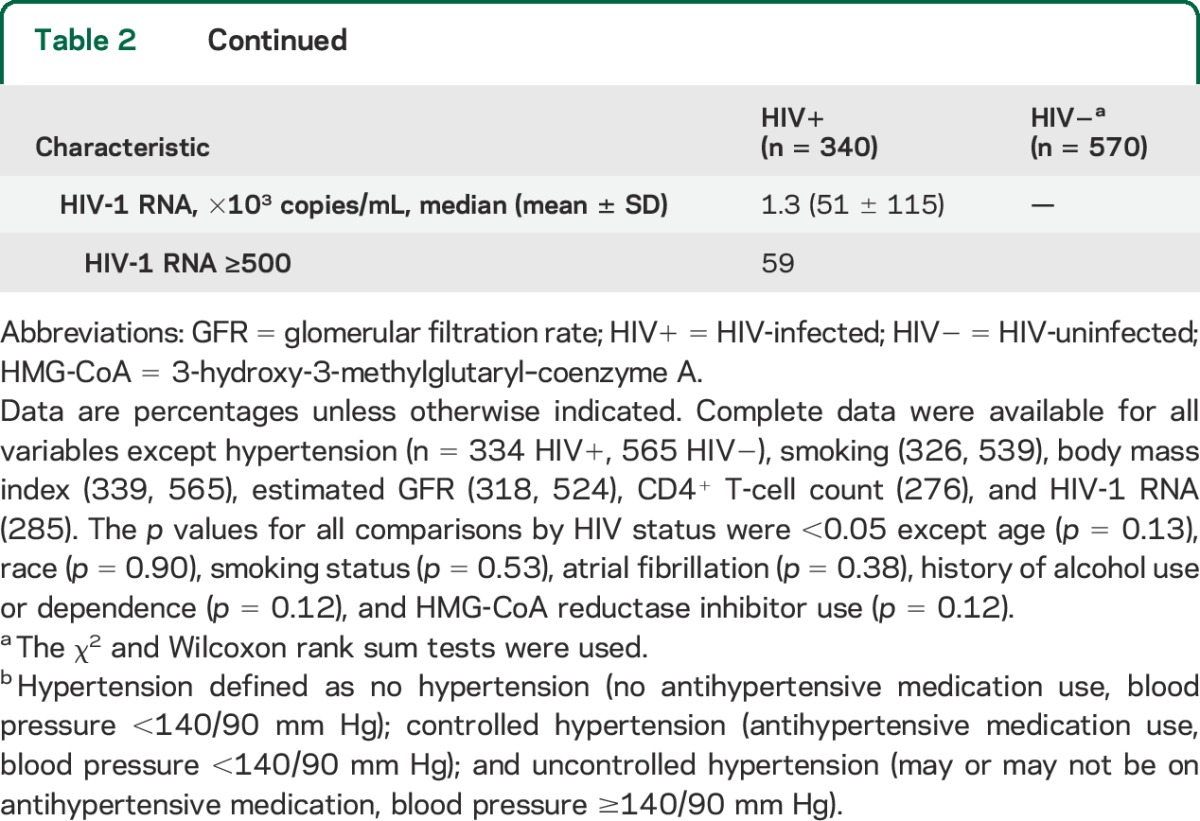
After excluding participants with known baseline CVD (n = 20,502) and women (n = 2,187), our final sample was 76,835 participants (33% HIV-infected). Compared with uninfected veterans, those with HIV infection had a higher prevalence of dyslipidemia, current smoking, cocaine abuse and dependence, renal disease, and anemia, and a lower prevalence of hypertension, diabetes, obesity, atrial fibrillation, and HMG-CoA reductase inhibitor use (table 1). Alcohol abuse and dependence was similar between both groups (table 1). Among the veterans with HIV infection, more than half had HIV-1 RNA ≥500 copies/mL and almost 30% had CD4+ T-cell counts <200 cells/mm3 at baseline (table 1).
Table 1.
Baseline characteristics of HIV-infected and matched HIV-uninfected veterans
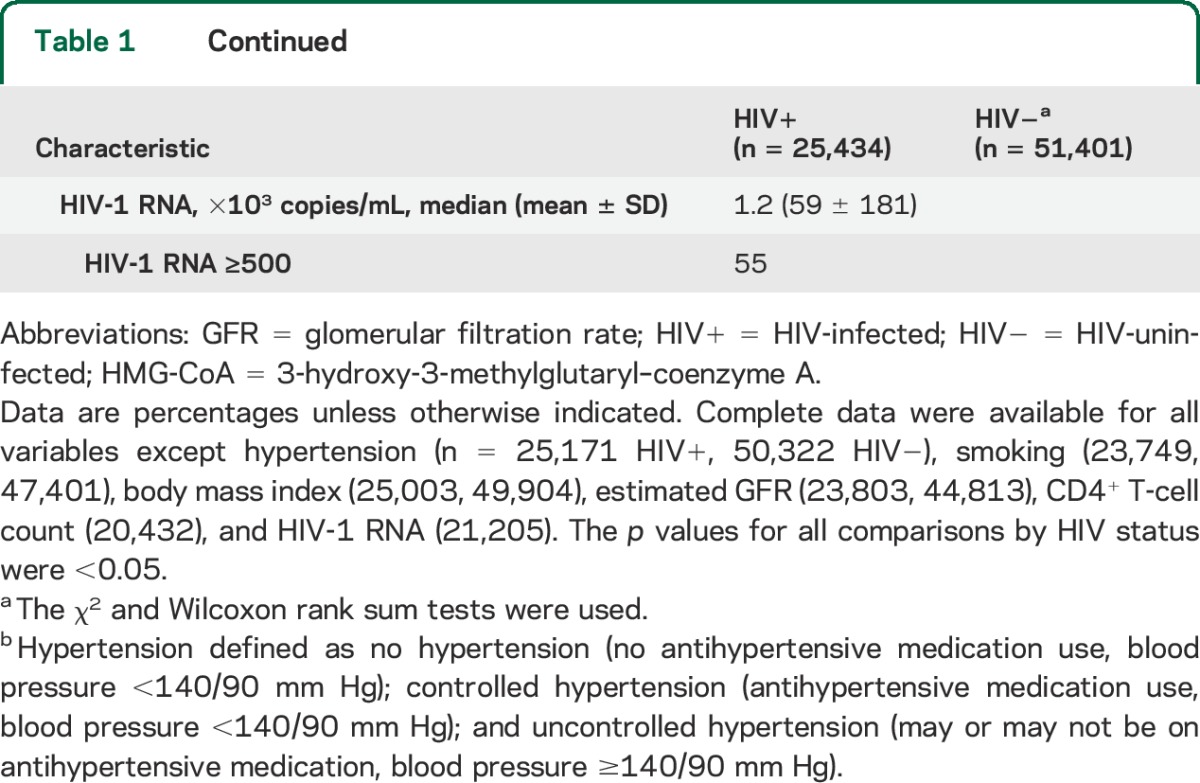
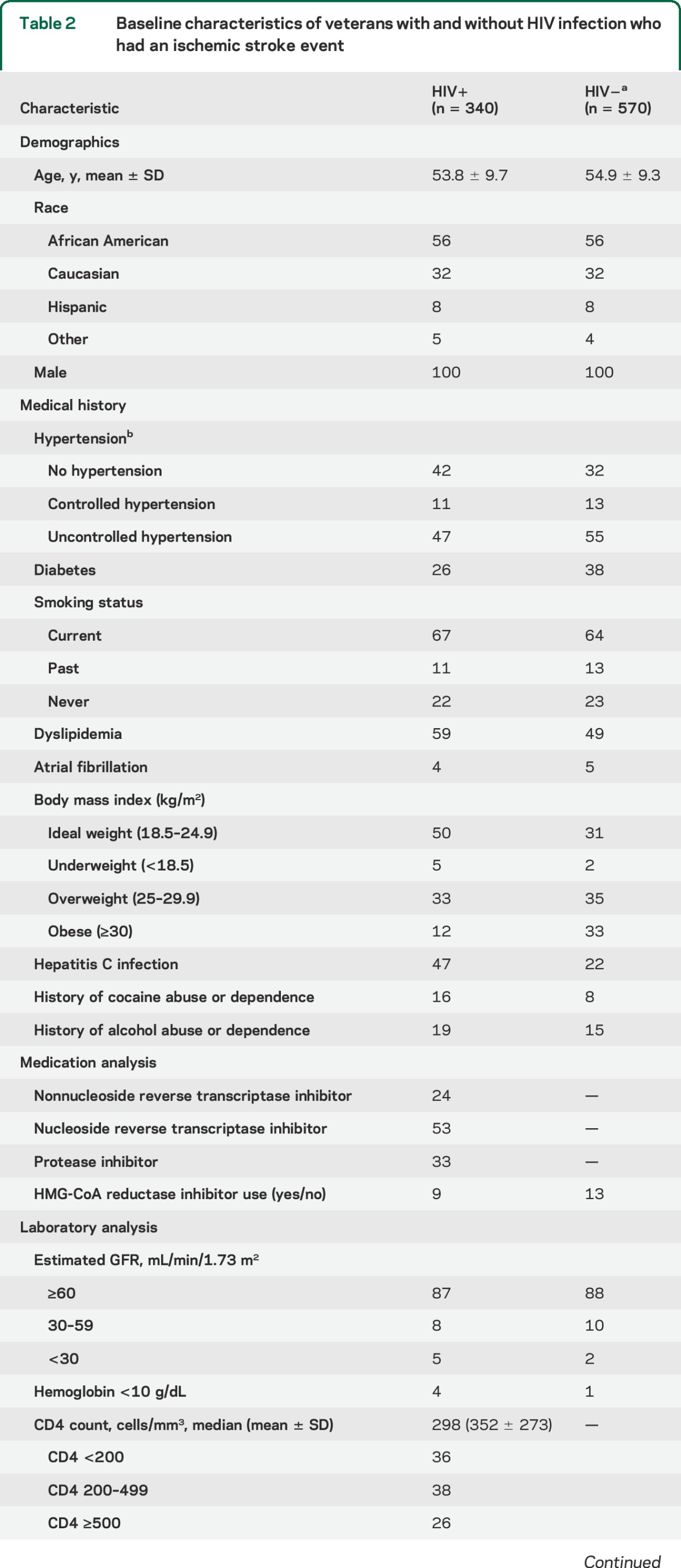
During a median follow-up of 5.9 (interquartile range 3.5–6.6) years, there were 910 incident ischemic stroke events, with 340 events occurring among veterans with HIV infection (table 2). Among those with ischemic stroke, there were no differences in race/ethnicity, smoking status, atrial fibrillation, or alcohol abuse and dependence or HMG-CoA reductase inhibitor use by HIV status. Mean (SD) age at stroke event was 57.2 (9.8) and 58.4 (9.3) years and mean (SD) time to stroke event was 3.4 (1.8) and 3.5 (1.7) years for HIV-infected and uninfected participants, respectively (p > 0.05 for both comparisons). Compared with uninfected veterans, HIV-infected veterans had a lower prevalence of hypertension, diabetes, and obesity, and a higher prevalence of dyslipidemia, HCV infection, cocaine abuse and dependence, renal disease, and anemia. Among the veterans with HIV infection, 60% had HIV-1 RNA ≥500 copies/mL and 36% had CD4+ T-cell counts <200 cells/mm3 at baseline (table 2).
Table 2.
Baseline characteristics of veterans with and without HIV infection who had an ischemic stroke event
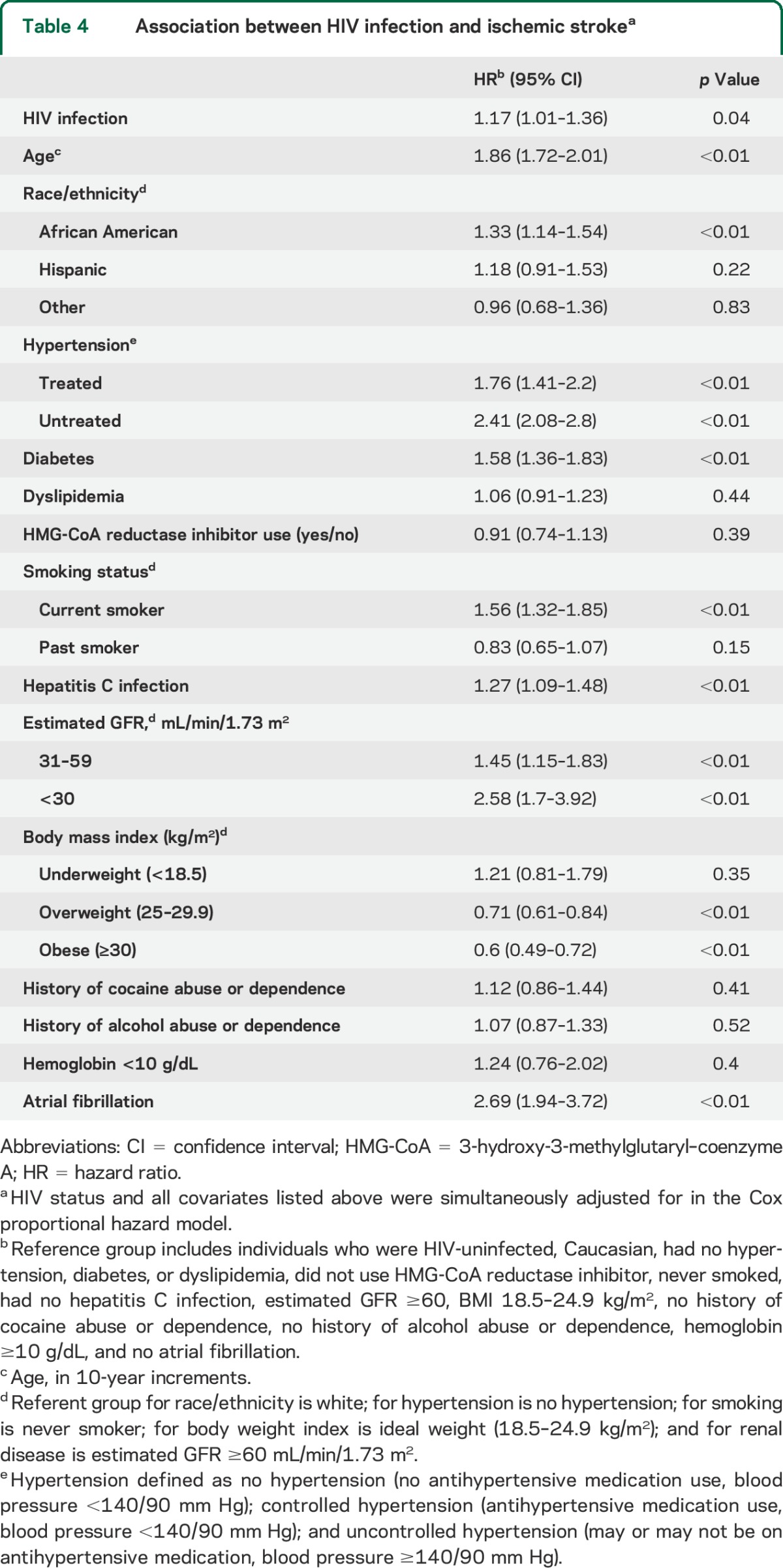
Stroke rates per 1,000 person-years increased with age (table 3) and were higher for veterans with HIV infection (2.79, 95% CI 2.51–3.10) than for veterans without infection (2.24, 95% CI 2.06–2.43) (incidence rate ratio 1.25 [1.09–1.43]; p < 0.01). After adjusting for demographics, ischemic stroke risk factors, comorbid diseases, and substance abuse or dependence, HIV-infected veterans had a significantly increased risk of ischemic stroke compared with uninfected veterans (HR = 1.17 [1.01–1.36]; p = 0.04) (table 4). Other risk factors significantly associated with ischemic stroke were age, African American race/ethnicity, diabetes, hypertension, atrial fibrillation, HCV infection, current smoking, overweight and obesity, and renal disease (table 4).
Table 3.
Rates of stroke (95% CI) per 1,000 person-years stratified by age
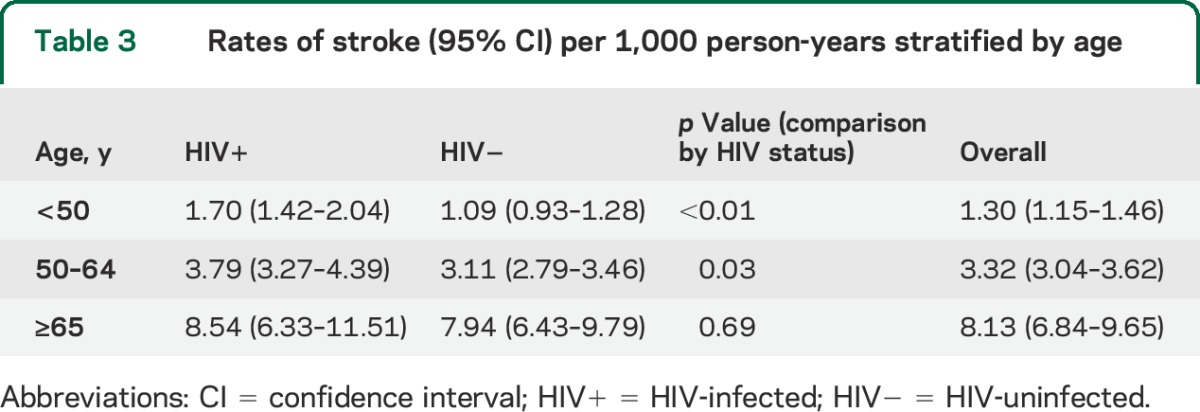
Table 4.
Association between HIV infection and ischemic strokea
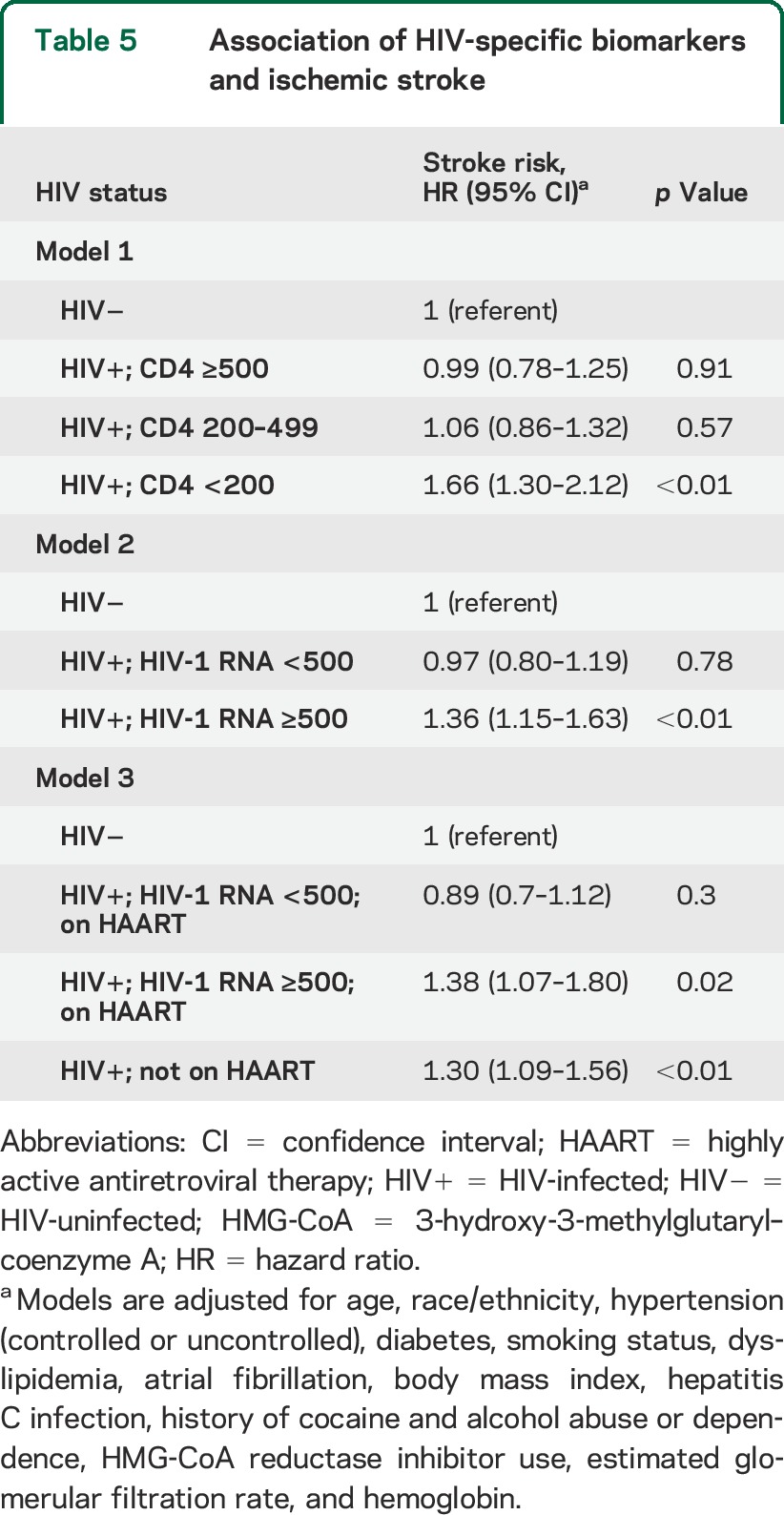
Compared with uninfected veterans, HIV-infected veterans with a CD4+ T-cell count <200 cells/mm3 (HR = 1.66, 95% CI 1.30–2.12) or HIV-1 RNA ≥500 copies/mL (HR = 1.36, 95% CI 1.15–1.63) were at highest risk of incident ischemic stroke (table 5). HIV-infected veterans with unsuppressed viremia taking HAART or any HIV-infected veteran not taking HAART at baseline had higher risk of stroke compared with uninfected veterans (table 5).
Table 5.
Association of HIV-specific biomarkers and ischemic stroke
DISCUSSION
Compared with uninfected veterans with similar (or higher) comorbidity burden, veterans with HIV infection had a significantly increased risk of ischemic stroke. These associations persisted after adjusting for traditional ischemic stroke risk factors, comorbid diseases, and substance abuse or dependence. Age, African American race/ethnicity, diabetes, hypertension, atrial fibrillation, smoking, alcohol abuse or dependence, renal disease, and CD4+ T-cell count <200 cells/mm3 were associated with ischemic stroke among veterans with HIV infection.
The increased rates and risk of ischemic stroke among veterans with HIV infection are consistent with findings from 2 recent studies with uninfected comparators from the same health care system (Kaiser Permanente and Partners Healthcare, respectively)17,18 and for findings among men in the Multicenter AIDS Cohort Study.16 Absolute stroke rates in our cohort were higher than those reported in 2 former studies possibly because of the higher prevalence of ischemic stroke risk factors among our participants. Contrary to our findings and to those by the Kaiser Permanente group and in the Multicenter AIDS Cohort Study, others did not find a significant association between HIV status and stroke risk among men in sex-stratified analyses. Reasons for the discrepancy may include differences between the cohorts. For example, our cohort participants were older at baseline (49 vs 41 years) and more likely to be African American (47% vs 22%), 2 important nonmodifiable ischemic stroke risk factors (tables 3 and 4). In addition, we excluded veterans with prevalent heart disease while others adjusted for prevalent heart disease increasing the potential for unmeasured confounding because of ascertainment bias.
The present study extends the knowledge gained from these prior studies. First, it provides data on an aging HIV-infected cohort experiencing stroke outcomes. Data on absolute and relative stroke risk from early waves of aging HIV-infected people are sparse and will improve prioritization of stroke-prevention and risk-reduction efforts in this population. Second, this aging cohort is compared with an aging HIV-uninfected cohort with a similar or higher burden of stroke risk factors (e.g., hypertension, diabetes, atrial fibrillation) at baseline. Comparing stroke risk in an HIV-infected population with that from an uninfected population with a significantly lower burden of stroke risk factors may overestimate the association of HIV status and incident stroke.
Few other large epidemiologic studies have addressed incident ischemic stroke risk among HIV-infected and uninfected people in the same cohort. Prior work was done in the pre-HAART era or limited by the low number of events, lack of a demographically and behaviorally similar HIV-uninfected comparator group, or lack of adjustment for ischemic stroke risk factors.4,14,15,30 The results of the present study are largely consistent with those from prior studies.
The mechanisms by which HIV infection confers an increased risk of ischemic stroke in the HAART era are unclear and likely multifactorial. While processes that caused strokes in the pre-HAART era (e.g., opportunistic infections, malignancies) may still affect patients who experience immunodeficiency, they may be less relevant in patients with better HIV control.10,31 With the advent of HAART and ever-increasing life expectancy, people with HIV infection are living long enough to develop traditional stroke risk factors, the ill effects of polysubstance use, and HAART-associated toxicities.9,10,15,31 Consequently, increasing age, nonwhite race, hypertension, diabetes, atrial fibrillation, current smoking, a history of alcohol abuse or dependence, and renal disease were significantly associated with increased risk of ischemic stroke in our analysis. The observation that most of these risk factors for ischemic stroke were less prevalent among veterans with HIV infection at baseline may indicate that there are additional HIV-specific mechanisms of increased stroke risk independent of these risk factors.
Immunosuppression and HIV viral replication have been associated with increased rates of stroke and risk of CVD.3,5,18,32 Similarly, we found that stroke rates and risk were higher among those with lower CD4 counts or higher HIV-1 RNA and similar among those with higher CD4+ T-cell count or lower HIV-1 RNA compared with uninfected veterans. This highlights the need for continued emphasis of early and consistent HIV control when placed in the larger context that viral suppression occurs only in an estimated 28% of those living with HIV in the United States.33
Our current study has limitations that warrant discussion. The use of stroke ICD-9 codes may have resulted in some misclassification. However, prior studies have reported that these codes have high agreement with formally adjudicated outcomes and are sensitive and specific within the veteran stroke population.2,20,21 Our analyses did not adjust for aspirin use. Aspirin use is incompletely captured using VA pharmacy records because it is frequently purchased over the counter. Aspirin use has been associated with decreased risk of stroke among patients with HIV infection.17 In one VA study that used administrative and chart review data to examine the quality of poststroke care, the median standardized rate of prescribing antithrombotic agents among eligible patients was 97% (27th, 75th percentiles: 96%, 98%).34 This suggests that the absolute number of poststroke veterans with differential aspirin use by HIV status is likely to be small assuming such a bias existed. Imaging data were not available to explore the etiology of ischemic stroke, stroke severity, or stroke subtype. This becomes important, especially among patients with lower CD4 counts and higher degrees of viral replication, because they may also be susceptible to ischemic strokes from opportunistic infections and malignancies. We also cannot comment on reasons patients in our cohort did not obtain complete viral suppression; etiologies such as medication resistance and noncompliance should be further explored in this group at high risk of cerebrovascular disease. We did not control for recent use of cocaine. As with any observational study, we cannot exclude the possibility of residual or unmeasured confounding.
Our data suggest that while traditional risk factors are important for stroke pathogenesis (especially hypertension), HIV infection, especially when less well controlled (i.e., lower CD4 counts, higher HIV-1 RNA), contributes to stroke risk independently of but in addition to traditional risk factors, substance abuse or dependence, and sociodemographic characteristics. These results have important implications in the management of those aging with HIV, and may help guide intervention strategies to decrease ischemic stroke risk in this higher-risk population.
Supplementary Material
ACKNOWLEDGMENT
The authors thank the Veterans Aging Cohort Study for their support, Dr. John Booss for his editorial comments, and the veterans who make our work possible.
GLOSSARY
- CI
confidence interval
- CVD
cardiovascular disease
- HAART
highly active antiretroviral therapy
- HCV
hepatitis C virus
- HMG-CoA
3-hydroxy-3-methylglutaryl–coenzyme A
- HR
hazard ratio
- ICD-9
International Classification of Diseases, Ninth Revision
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- VA
Veterans Affairs
- VACS-VC
Veterans Aging Cohort Study–Virtual Cohort
Footnotes
Supplemental data at Neurology.org
Contributor Information
For the Veterans Aging Cohort Study:
Chung-Chou H. Chang, Kaku So-Armah, Amy C. Justice, Elaine Hylek, Melissa Skanderson, Kathleen McGinnis, Lewis H. Kuller, Kevin L. Kraemer, David Rimland, Matthew Bidwell Goetz, Adeel A. Butt, Maria C. Rodriguez Barradas, Cynthia Gibert, David Leaf, Sheldon T. Brown, Jeffrey Samet, Lewis Kazis, Kendall Bryant, and Matthew S. Freiberg
AUTHOR CONTRIBUTIONS
Jason J. Sico: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, statistical analysis. Chung-Chou H. Chang: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, statistical analysis. Kaku So-Armah: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, statistical analysis. Amy C. Justice: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, contribution of vital reagents/tools/patients, acquisition of data, statistical analysis, study supervision, obtaining funding. Elaine Hylek: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval. Melissa Skanderson: analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, acquisition of data. Kathleen McGinnis: drafting/revising the manuscript, accepts responsibility for conduct of research and will give final approval, acquisition of data. Lewis H. Kuller: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, statistical analysis. Kevin L. Kraemer: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval. David Rimland: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, acquisition of data, study supervision. Matthew Bidwell Goetz: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval. Adeel A. Butt: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval. Maria C. Rodriguez-Barradas: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval. Cynthia Gibert: drafting/revising the manuscript, study concept or design, accepts responsibility for conduct of research and will give final approval, preparation of manuscript. David Leaf: drafting/revising the manuscript, study concept or design, accepts responsibility for conduct of research and will give final approval, acquisition of data, study supervision. Sheldon T. Brown: drafting/revising the manuscript, accepts responsibility for conduct of research and will give final approval, acquisition of data. Jeffrey Samet: drafting/revising the manuscript, accepts responsibility for conduct of research and will give final approval. Lewis Kazis: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, acquisition of data. Kendall Bryant: drafting/revising the manuscript, study concept or design, accepts responsibility for conduct of research and will give final approval, study supervision. Matthew S. Freiberg: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, acquisition of data, obtaining funding.
STUDY FUNDING
Research funding was made possible by the NIH, National Institute on Alcohol Abuse and Alcoholism (grant 5U10AA013566-10); NIH, National Heart Lung and Blood Institute (grant R01 HL095136-05); and Department of Veteran Affairs Health Services Research and Development (grant 11-262). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veteran Affairs. No conflicts of interest are reported.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Freiberg M, Cheng DM, Kraemer KL, Saitz R, Kuller LH, Samet JH. The association between hepatitis C infection and prevalent cardiovascular disease among HIV-infected individuals. AIDS 2007;21:193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Justice AC, Zingmond DS, Gordon K, et al. Drug toxicity, HIV progression, or comorbidity of aging: does tipranavir use increase the risk of intracranial hemorrhage? Clin Infect Dis 2008;47:1226–1230. [DOI] [PubMed] [Google Scholar]
- 3.Freiberg MS, Chang CH, Kuller LH. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med 2013;173:614–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strategies for Management of Antiretroviral Therapy (SMART) Study Group, El-Sadr WM, Lundgren J, et al. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med 2006;355:2283–2296. [DOI] [PubMed] [Google Scholar]
- 5.D:A:D Study Group, Sabin CA, Worm SW, et al. Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D:A:D study: a multi-cohort collaboration. Lancet 2008;371:1417–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pinto AN. AIDS and cerebrovascular disease. Stroke 1996;27:538–543. [DOI] [PubMed] [Google Scholar]
- 7.Qureshi AI, Janssen RS, Karon JM, et al. Human immunodeficiency virus infection and stroke in young patients. Arch Neurol 1997;54:1150–1153. [DOI] [PubMed] [Google Scholar]
- 8.Adams RJ, Albers G, Alberts MJ, et al. Update to the AHA/ASA recommendations for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke 2008;39:1647–1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jain RG, Furfine ES, Pedneault L, White AJ, Lenhard JM. Metabolic complications associated with antiretroviral therapy. Antiviral Res 2001;51:151–177. [DOI] [PubMed] [Google Scholar]
- 10.Bedimo RJ, McGinnis KA, Dunlap M, Rodriguez-Barradas MC, Justice AC. Incidence of non-AIDS-defining malignancies in HIV-infected versus noninfected patients in the HAART era: impact of immunosuppression. J Acquir Immune Defic Syndr 2009;52:203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freiberg MS, Chang CC, Skanderson M, et al. The risk of incident coronary heart disease among veterans with and without HIV and hepatitis C. Circ Cardiovasc Qual Outcomes 2011;4:425–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee MH, Yang HI, Wang CH, et al. Hepatitis C virus infection and increased risk of cerebrovascular disease. Stroke 2010;41:7. [DOI] [PubMed] [Google Scholar]
- 13.Di Napoli M, Schwaninger M, Cappelli R, et al. Evaluation of C-reactive protein measurement for assessing the risk and prognosis in ischemic stroke: a statement for health care professionals from the CRP Pooling Project members. Stroke 2005;36:1316–1329. [DOI] [PubMed] [Google Scholar]
- 14.Cole JW, Pinto AN, Hebel JR, et al. Acquired immunodeficiency syndrome and the risk of stroke. Stroke 2004;35:51–56. [DOI] [PubMed] [Google Scholar]
- 15.Hoffmann M, Berger JR, Nath A, Rayens M. Cerebrovascular disease in young, HIV-infected, black Africans in the KwaZulu Natal province of South Africa. J Neurovirol 2000;6:229–236. [DOI] [PubMed] [Google Scholar]
- 16.Mateen FJ, Post WS, Sacktor N, et al. Long-term predictive value of the Framingham Risk Score for Stroke in HIV-positive vs HIV-negative men. Neurology 2013;81:2094–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chow F, Regan S, Feske S, Meigs JB, Grinspoon SK, Triant VA. Comparison of ischemic stroke incidence in HIV-infected and non-HIV-infected patients in a US health care system. J Acquir Immune Defic Syndr 2012;60:351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marcus JL, Leyden WA, Chao CR, et al. HIV infection and incidence of ischemic stroke. AIDS 2014;28:1911–1919. [DOI] [PubMed] [Google Scholar]
- 19.Fultz SLM, Skanderson MM, Mole LAP, et al. Development and verification of a “virtual” cohort using the National VA Health Information System. Med Care 2006;44:S25–S30. [DOI] [PubMed] [Google Scholar]
- 20.Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events: the Cardiovascular Health Study. Ann Epidemiol 1995;5:278–285. [DOI] [PubMed] [Google Scholar]
- 21.Ekundayo OJ, Vassar SD, Williams LS, Bravata DM, Cheng EM. Using administrative databases to calculate Framingham scores within a large health care organization. Stroke 2011;42:1982–1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tirschwell DL, Longstreth WT. Validating administrative data in stroke research. Stroke 2002;33:2465–2470. [DOI] [PubMed] [Google Scholar]
- 23.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 24.Butt AA, McGinnis K, Rodriguez-Barradas MC, et al. HIV infection and the risk of diabetes mellitus. AIDS 2009;23:1227–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGinnis KA, Brandt CA, Skanderson M, et al. Validating smoking data from the Veteran's Affairs Health Factors dataset, an electronic data source. Nicotine Tob Res 2011;13:1233–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goulet JL, Fultz SL, McGinnis KA, Justice AC. Relative prevalence of comorbidities and treatment contraindications in HIV-mono-infected and HIV/HCV-co-infected veterans. AIDS 2005;19:S99–S105. [DOI] [PubMed] [Google Scholar]
- 27.Kraemer KL, McGinnis KA, Skanderson M, et al. Alcohol problems and health care services use in human immunodeficiency virus (HIV)-infected and HIV-uninfected veterans. Med Care 2006;44:S44–S51. [DOI] [PubMed] [Google Scholar]
- 28.Jensen PN, Johnson K, Floyd J, Heckbert SR, Carnahan R, Dublin S. A systematic review of validated methods for identifying atrial fibrillation using administrative data. Pharmacoepidemiol Drug Saf 2012;21:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994;81:515–526. [Google Scholar]
- 30.Corral I, Quereda C, Moreno A, et al. Cerebrovascular ischemic events in HIV-1-infected patients receiving highly active antiretroviral therapy: incidence and risk factors. Cerebrovasc Dis 2009;27:559–563. [DOI] [PubMed] [Google Scholar]
- 31.The Antiretroviral Therapy Cohort Collaboration. The changing incidence of AIDS events in patients receiving highly active antiretroviral therapy. Arch Intern Med 2005;165:416–423. [DOI] [PubMed] [Google Scholar]
- 32.Baker JV, Peng G, Rapkin J, et al. CD4+ count and risk of non-AIDS diseases following initial treatment for HIV infection. AIDS 2008;22:841–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Vital signs: HIV prevention through care and treatment—United States. MMWR Morb Mortal Wkly Rep 2011;60:1618–1623. [PubMed] [Google Scholar]
- 34.Ross JS, Arling G, Ofner S, et al. Correlation of inpatient and outpatient measures of stroke care quality within veterans health administration hospitals. Stroke 2011;42:2269–2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


