We report the first quality-of-life assessment of a MEK inhibitor in metastatic melanoma from a phase III study. Trametinib prolonged progression-free survival and improved overall survival versus chemotherapy in patients with BRAF V600 mutation-positive melanoma. Less functional impairment, smaller declines in health status, and less exacerbation of symptoms were observed with trametinib.
Keywords: BRAF, chemotherapy, MEK, melanoma, quality of life, trametinib
Abstract
Background
In a randomized phase III study, trametinib prolonged progression-free survival and improved overall survival versus chemotherapy in patients with BRAF V600 mutation-positive melanoma.
Patients and methods
Patients' quality of life (QOL) was assessed at baseline and follow-up visits using the European Organisation for Research and Treatment of Cancer Core QOL questionnaire.
Results
In the primary efficacy population (BRAF V600E+, no brain metastases) from baseline to weeks 6 and 12, patients' global health status scores worsened by 4–5 points with chemotherapy but improved by 2–3 points with trametinib. Rapid and substantive reductions in QOL functionality (e.g. role functioning, 8–11 points at weeks 6 and 12) and symptom exacerbation (e.g. fatigue, 4–8 points; nausea and vomiting, 5 points, both at weeks 6 and 12) were observed in chemotherapy-treated patients. In contrast, trametinib-treated patients reported small improvements or slight worsening from baseline at week 12, depending on the functional dimension and symptom. The mean symptom-scale scores for chemotherapy-treated patients increased from baseline (symptoms worsened) for seven of eight symptoms at week 6 (except insomnia) and six of eight symptoms at week 12 (except dyspnea and insomnia). In contrast, at weeks 6 and 12, the mean symptom-scale scores for trametinib decreased from baseline (symptoms improved) for pain (11–12 points), insomnia (10–12 points), and appetite loss (1–5 points), whereas those for diarrhea worsened (15–16 points). Mixed-model repeated-measures analyses showed significant (P < 0.05) and/or clinically meaningful improvements (small to moderate) from baseline in favor of trametinib for global health; physical, role, and social functioning; fatigue; pain; insomnia; nausea and vomiting; constipation; dyspnea; and appetite at weeks 6 and/or 12. QOL results for the intent-to-treat population were consistent.
Conclusions
This first QOL assessment for a MEK inhibitor in metastatic melanoma demonstrated that trametinib was associated with less functional impairment, smaller declines in health status, and less exacerbation of symptoms versus chemotherapy.
introduction
Activating mutations in BRAF, a constituent of the mitogen-activated protein kinase (MAPK) signal transduction pathway, are found in ∼50% of patients with advanced melanoma [1, 2]. The two most common BRAF mutations, V600E and V600K, account for 95% of all BRAF mutations in melanoma. BRAF activates MAPK/extracellular signal-regulated kinase kinase 1 (MEK1) and MEK2—which in turn activate downstream MAPKs—and regulates tumor cell proliferation and survival in many cancers, including melanoma [3].
Until recently, only two agents had been approved for the treatment of metastatic melanoma in the United States: dacarbazine (DTIC) and interleukin‐2. Ipilimumab, a monoclonal antibody targeting cytotoxic T-lymphocyte-associated antigen 4, and vemurafenib, a selective BRAF inhibitor (BRAFi), were approved in the United States and Europe in 2011/2012 to treat metastatic melanoma. Dabrafenib, another selective BRAFi, and trametinib, a highly selective allosteric inhibitor of MEK1 and MEK2 (MEKi), were both approved recently in the United States (May 2013) for unresectable or metastatic melanoma with BRAF V600 mutation.
In the pivotal METRIC study, trametinib decreased the risk of progression or death by 55% versus chemotherapy in patients with BRAF V600E or V600K mutation-positive metastatic melanoma (intent-to treat [ITT] population; progression-free survival [PFS] of 4.8 versus 1.5 months; hazard ratio [HR] = 0.45; 95% confidence interval [CI] 0.33–0.63; P < 0.0001) [4]. At 6 months, the rate of overall survival (OS) was 81% in the trametinib group and 67% in the chemotherapy group despite crossover (HR = 0.54; 95% CI, 0.32–0.92; P = 0.01). The primary efficacy analysis was restricted to patients with the BRAF V600E mutation who did not have brain metastases at baseline (PFS of 4.8 versus 1.4 months; HR = 0.44; 95% CI 0.31–0.64; P < 0.001 and OS HR = 0.53; 95% CI 0.30–0.94; P = 0.0181).
In addition to the clinical benefits of any new treatment option, another important goal is to preserve, and when possible, improve patients' quality of life (QOL). Patient-perceived QOL captures clinical benefit and the impact of adverse events in a single assessment. The objective of these analyses was to evaluate the impact of the recently approved MEKi, trametinib, on patients' QOL versus chemotherapy. Patients in the analysis reported here had been enrolled in the METRIC phase III trial [4] and had BRAF V600E mutation-positive metastatic melanoma with no history of brain metastases. There were no a priori hypotheses and no adjustments for multiple testing; all results should be considered exploratory.
methods
study design and treatment regimen
METRIC (MEK114267; NCT01245062) is a randomized, two-arm, open-label, international phase III study to evaluate the efficacy and safety of single-agent trametinib versus chemotherapy (DTIC or paclitaxel) [4]. Briefly, patients with histologically confirmed cutaneous advanced or metastatic melanoma (stage IIIC or IV), with a BRAF V600E/K mutation-positive tumor sample were randomized 2:1 to receive either trametinib 2 mg once daily or chemotherapy. QOL was a secondary end point. Treatment continued until disease progression, death, or withdrawal from the study. Patients on chemotherapy could cross over to receive trametinib after disease progression that had been confirmed by an independent review. The primary efficacy population was patients with advanced/metastatic BRAF V600E mutation-positive melanoma without a history of prior brain metastases. Of the 322 patients enrolled in the study, 273 patients (trametinib, n = 178; chemotherapy, n = 95) were included in the primary efficacy population and are presented herein. QOL results for the ITT population were consistent and hence are not reported here.
QOL assessments
The European Organisation for Research and Treatment of Cancer QOL Questionnaire (EORTC QLQ-C30) [5, 6] was used to evaluate QOL in this study. The EORTC QLQ-C30 is a self-reported, 30-item generic instrument for use in cancer patients across tumor types that include overall health/global QOL, five functional scales, and nine symptom scales or single-item questions. For global health status and the functional scales, a higher score reflects better global health or functioning. Conversely, for symptom scales or single items, higher scores indicate greater symptom severity. QOL assessments were carried out at baseline (before any study drug was administered); at weeks 6, 12, 21, 30, and every 12 weeks thereafter during treatment; on progression; and 6 weeks after progression was first determined. Data at baseline, weeks 6 and 12, and on progression with chemotherapy are presented because of lower sample size/limited data availability after week 12.
statistical analysis
QOL data from the primary efficacy population collected until the data cut-off used for analyses of the primary end point were included. Analyses were carried out for the randomized phase and for patients who crossed over to trametinib on progression with chemotherapy. Baseline scores (defined as QOL assessment before first dose) were reported with standard descriptive statistics. For the crossover phase analysis, the assessment at disease progression while on chemotherapy was used as the baseline score. Changes in score from baseline at each assessment were summarized for global health and for each functional and symptom scale or single item. Analysis of covariance—adjusted for baseline score using mixed-model repeated measures with time, treatment, and treatment by time interaction as fixed effects—was carried out to assess differences between arms for global health and all functional and symptom dimension scores. Time was treated as the repeated variable within patients. Unstructured covariance matrices were used for these analyses.
results
randomized phase
baseline characteristics and QOL completion rates
Treatment groups were well balanced, although more patients in the trametinib group had M1c disease (characterized by metastasis to sites beyond skin, lymph node, and lung or to any site with an elevated lactate dehydrogenase level) and ≥3 sites of disease, as reported previously [4]. At baseline, 92 and 87% of patients in the trametinib and chemotherapy arms, respectively, completed QOL assessments. The majority of patients (77%) in the trametinib arm either completed all required QOL assessments or missed <3 post-baseline assessments; the corresponding percentage was 62% for patients in the chemotherapy arm (Supplementary Table S1, available at Annals of Oncology online). At baseline, patients in both arms reported comparable levels of mean functional and symptom-related QOL with no difference between arms exceeding 6 points (Table 1). Baseline scores here were comparable with EORTC QLQ-C30 reference values from an international sample of patients with stage III/IV malignant melanoma [7].
Table 1.
Summary of EORTC QLQ-C30 functionality and symptom dimensions of QOL at baseline (primary efficacy population)—randomized phase
| QOL dimension | Trametinib (n = 178) |
Chemotherapy (n = 95) |
||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| Global health status/QOL | 175 | 63.3 | 21.6 | 88 | 68.7 | 20.9 |
| Physical functioning | 173 | 81.2 | 20.1 | 86 | 82.8 | 18.9 |
| Role functioning | 172 | 73.1 | 30.5 | 87 | 74.3 | 28.2 |
| Emotional functioning | 174 | 72.3 | 23.6 | 87 | 76.5 | 20.8 |
| Cognitive functioning | 175 | 88.3 | 17.4 | 89 | 90.6 | 17.2 |
| Social functioning | 175 | 75.5 | 29.0 | 89 | 78.3 | 25.4 |
| Fatigue | 172 | 32.6 | 26.6 | 89 | 28.8 | 24.8 |
| Nausea and vomiting | 175 | 10.2 | 18.7 | 89 | 8.6 | 16.7 |
| Pain | 173 | 28.8 | 30.0 | 88 | 28.6 | 26.0 |
| Dyspnea | 174 | 20.1 | 30.0 | 89 | 15.0 | 21.9 |
| Insomnia | 175 | 30.3 | 31.0 | 88 | 24.6 | 27.5 |
| Appetite loss | 174 | 19.5 | 29.8 | 89 | 16.1 | 26.2 |
| Constipation | 175 | 11.1 | 21.9 | 89 | 12.4 | 22.7 |
| Diarrhea | 175 | 7.6 | 16.9 | 89 | 6.4 | 14.1 |
EORTC QLQ-C30, European Organisation for Research and Treatment of Cancer Core Quality of Life Questionnaire; QOL, quality of life; SD, standard deviation.
Values are rounded to one decimal place.
impact on global health and functional QOL
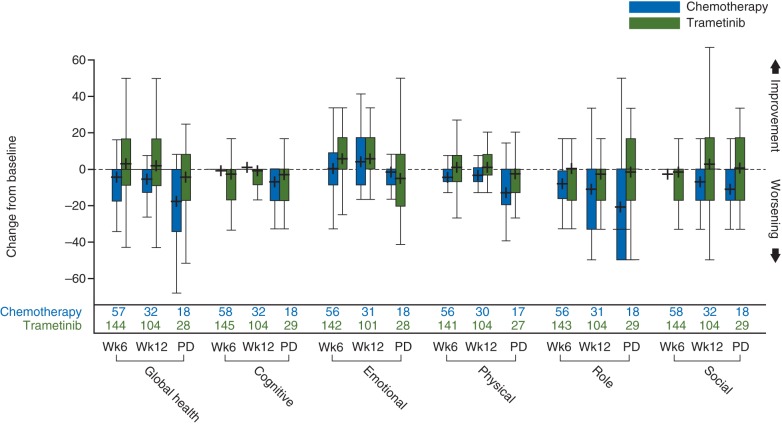
Global health and most functionality dimensions (Figure 1) worsened from baseline for chemotherapy patients at weeks 6 and 12. For trametinib patients, at weeks 6 and 12, global health and physical and emotional functioning improved, but role and cognitive functioning slightly worsened. In addition, global health status scores worsened from baseline by 4–5 points for chemotherapy patients but improved by 2–3 points for trametinib patients. Rapid and substantive reductions in QOL functionality (e.g. role functioning = 8–11 points at weeks 6 and 12) were observed in chemotherapy-treated patients, consistent with the faster progression observed within this group. In contrast, trametinib-treated patients reported either small decreases or improvements from baseline at week 12, depending upon the functional dimension. Emotional functioning improved most at week 6 (5 points) and week 12 (6 points). At progression, large decreases (≥10 points) in global health and physical, role, and social functional dimensions of QOL were observed for chemotherapy versus trametinib.
Figure 1.
Change from baseline for EORTC QLQ-C30 global health and functional dimension scores (randomized phase). + indicates the mean. Boxes show 25th to 75th percentiles. EORTC QLQ-C30, European Organisation for Research and Treatment of Cancer Core Quality of Life Questionnaire; PD, progressive disease; Wk, week.
Statistical differences for global health and functional dimensions between arms were assessed using mixed-model repeated-measures analysis (Table 2). A 5- and 6-point significant improvement (P < 0.05) from baseline in favor of trametinib was observed for physical functioning at weeks 6 and 12, respectively (Table 2). These mean changes in score can be considered ‘small’ clinically meaningful improvements [8]. Similarly a 7-point significant improvement in role functioning at week 6 (P = 0.043) and a 10-point significant improvement in social functioning at week 12 (P = 0.032) were observed in favor of trametinib, both considered ‘small’ clinically meaningful improvements [8].
Table 2.
Summary of mixed-model repeated-measures analysis for change from baseline in global health and functional dimension scores in randomized phase
| Domain | Change from baseline to | Treatment group | n available for QOL | Adjusted mean | SEM | Difference (trametinib versus chemotherapy) |
|---|---|---|---|---|---|---|
| Global health | Week 6 | Trametinib | 144 | 2.3 | 1.3 | 4.0 |
| Chemotherapy | 57 | −1.7 | 2.2 | |||
| Week 12 | Trametinib | 104 | 1.2 | 1.7 | 5.7 | |
| Chemotherapy | 32 | −4.6 | 3.0 | |||
| Cognitive functioning | Week 6 | Trametinib | 145 | −3.4 | 1.1 | −3.8 |
| Chemotherapy | 58 | 0.3 | 1.8 | |||
| Week 12 | Trametinib | 104 | −2.6 | 1.2 | −2.7 | |
| Chemotherapy | 32 | 0.1 | 2.2 | |||
| Emotional functioning | Week 6 | Trametinib | 142 | 4.4 | 1.3 | 4.0 |
| Chemotherapy | 56 | 0.4 | 2.1 | |||
| Week 12 | Trametinib | 101 | 5.6 | 1.5 | 3.8 | |
| Chemotherapy | 31 | 1.8 | 2.6 | |||
| Physical functioning | Week 6 | Trametinib | 141 | 0.6 | 1.1 | 5.2a |
| Chemotherapy | 56 | −4.6 | 1.8 | |||
| Week 12 | Trametinib | 104 | −0.9 | 1.3 | 6.2a | |
| Chemotherapy | 30 | −7.1 | 2.4 | |||
| Role functioning | Week 6 | Trametinib | 143 | −0.5 | 1.8 | 7.0a |
| Chemotherapy | 56 | −7.4 | 2.9 | |||
| Week 12 | Trametinib | 104 | −4.0 | 2.4 | 8.9 | |
| Chemotherapy | 31 | −12.9 | 4.3 | |||
| Social functioning | Week 6 | Trametinib | 144 | −2.4 | 1.8 | −0.6 |
| Chemotherapy | 58 | −1.8 | 2.9 | |||
| Week 12 | Trametinib | 104 | 0.7 | 2.2 | 9.5a | |
| Chemotherapy | 32 | −8.8 | 3.8 |
Trametinib, n = 178; chemotherapy, n = 95.
Values have been rounded to one decimal place.
QOL, quality of life; SEM, standard error of the mean.
aP < 0.05.
impact on symptoms
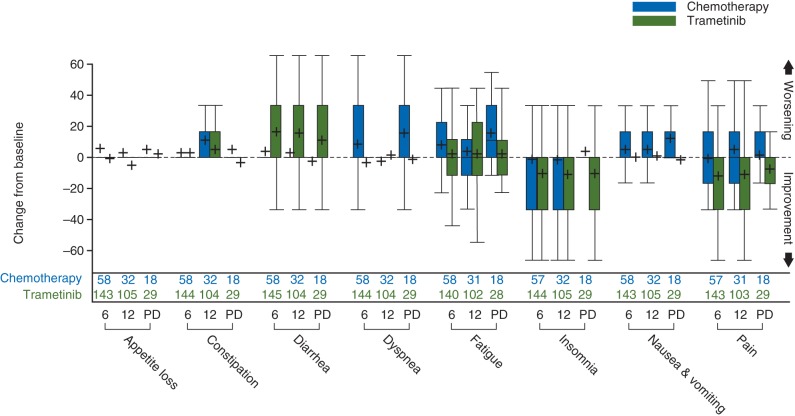
At weeks 6 and 12, the mean symptom scale scores for trametinib had decreased from baseline (symptoms improved) for pain (11–12 points), insomnia (10–12 points), and appetite loss (1–5 points), whereas those for diarrhea worsened (15–16 points) (Figure 2).
Figure 2.
Change from baseline for EORTC QLQ-C30 symptom scores (randomized phase) at week 6 (6), week 12 (12) and at disease progression (PD). + indicates the mean. Boxes show 25th to 75th percentiles. EORTC QLQ-C30, European Organisation for Research and Treatment of Cancer Core Quality of Life Questionnaire.
In contrast, the mean scores for chemotherapy-treated patients increased from baseline (symptoms worsened) for seven of eight symptoms at week 6 (except insomnia) and six of eight symptoms at week 12 (except dyspnea and insomnia). At progression, all symptoms (except diarrhea) worsened to a much greater degree for chemotherapy- versus trametinib-treated patients. Fatigue, nausea and vomiting, and dyspnea symptoms worsened most upon progression for chemotherapy-treated patients. Pain, insomnia, constipation, dyspnea, and nausea and vomiting scores were lower than baseline (symptoms improved) upon progression for trametinib-treated patients.
Significant differences for symptom dimensions between arms were also assessed using mixed-model repeated-measures analysis (Table 3). The mean pain scores significantly improved from baseline by 11 and 15 points in favor of trametinib at weeks 6 and 12, respectively (‘moderate’ clinically meaningful improvements). A 9-point significant improvement in dyspnea (P = 0.04) at week 6 and an 8-point significant improvement in appetite at week 12 (P = 0.038) were observed in favor of trametinib (‘small’ clinically meaningful improvements). However, diarrhea scores significantly worsened (‘moderate’ clinical change) from baseline by 12 and 11 points for trametinib at weeks 6 and 12, respectively.
Table 3.
Summary of mixed-model repeated-measures analysis for change from baseline in symptom dimension scores in randomized phase
| Domain | Change from baseline to | Treatment group | n available for QOL | Adjusted mean | SEM | Difference (trametinib versus chemotherapy) |
|---|---|---|---|---|---|---|
| Fatigue | Week 6 | Trametinib | 140 | 1.4 | 1.8 | −5.0 |
| Chemotherapy | 58 | 6.4 | 2.8 | |||
| Week 12 | Trametinib | 102 | 4.4 | 2.0 | −1.7 | |
| Chemotherapy | 31 | 6.1 | 3.4 | |||
| Nausea and vomiting | Week 6 | Trametinib | 143 | 0.2 | 1.2 | −4.5a |
| Chemotherapy | 58 | 4.8 | 1.9 | |||
| Week 12 | Trametinib | 105 | 2.8 | 1.5 | −4.0 | |
| Chemotherapy | 32 | 6.8 | 2.7 | |||
| Pain | Week 6 | Trametinib | 143 | −11.4 | 1.7 | −10.5a |
| Chemotherapy | 57 | −0.9 | 2.7 | |||
| Week 12 | Trametinib | 103 | −9.5 | 2.2 | −14.8a | |
| Chemotherapy | 31 | 5.3 | 4.0 | |||
| Dyspnea | Week 6 | Trametinib | 144 | −2.5 | 1.7 | −9.3a |
| Chemotherapy | 58 | 6.8 | 2.7 | |||
| Week 12 | Trametinib | 104 | 3.4 | 2.1 | 2.9 | |
| Chemotherapy | 32 | 0.6 | 3.7 | |||
| Insomnia | Week 6 | Trametinib | 144 | −9.3 | 2.0 | −6.6 |
| Chemotherapy | 57 | −2.7 | 3.2 | |||
| Week 12 | Trametinib | 105 | −10.3 | 2.3 | −9.1 | |
| Chemotherapy | 32 | −1.2 | 4.2 | |||
| Appetite loss | Week 6 | Trametinib | 143 | −1.0 | 1.8 | −5.2 |
| Chemotherapy | 58 | 4.3 | 2.9 | |||
| Week 12 | Trametinib | 105 | −3.0 | 2.0 | −8.3a | |
| Chemotherapy | 32 | 5.4 | 3.4 | |||
| Constipation | Week 6 | Trametinib | 144 | 4.1 | 1.7 | 2.6 |
| Chemotherapy | 58 | 1.5 | 2.7 | |||
| Week 12 | Trametinib | 104 | 3.8 | 1.9 | −5.1 | |
| Chemotherapy | 32 | 9.0 | 3.4 | |||
| Diarrhea | Week 6 | Trametinib | 145 | 15.4 | 1.9 | 12.1a |
| Chemotherapy | 58 | 3.3 | 3.0 | |||
| Week 12 | Trametinib | 104 | 16.5 | 2.1 | 11.5a | |
| Chemotherapy | 32 | 5.0 | 3.7 |
Trametinib, n = 178; chemotherapy, n = 95.
Values have been rounded to one decimal place.
CI, confidence interval; QOL, quality of life; SE, standard error of the mean.
aP < 0.05.
crossover phase
Patients receiving chemotherapy (n = 51) who crossed over to trametinib on progression experienced moderate-to-large clinically meaningful improvements in global health status and functional dimension scores relative to their progression visit scores. This suggested immediate benefit after receiving trametinib for 6–12 weeks; greatest improvements were observed for role functioning (19 points), global health (14 points), and physical functioning (14 points) at week 6. Large improvements were also observed for six of eight symptoms following 6 weeks of treatment with trametinib, especially for pain (22 points), insomnia (15 points), and fatigue (15 points). In contrast, scores for diarrhea worsened by 11 and 15 points and scores for constipation worsened by 2 and 11 points, at weeks 6 and 12, respectively (data not shown).
discussion
Health-related QOL is an important consideration for patients with advanced or metastatic melanoma. Although treatments can slow disease progression, thereby forestalling the effects of the disease on QOL, side-effects of treatment can adversely affect QOL. It is therefore vital to understand the impact of treatments on patients' overall QOL.
In the METRIC study, trametinib-treated patients experienced greater functional and symptomatic benefits than chemotherapy patients. These results suggest a fairly quick and substantive decrease in QOL functionality and exacerbation of symptoms across assessments for patients on chemotherapy, which were consistent with the faster progression observed for chemotherapy patients. Overall decrease in functionality and worsening of symptoms were greatest at disease progression for chemotherapy patients, whereas trametinib patients reported slight drops, slight improvements, or limited change in QOL from baseline, depending on the functional dimension and symptom. It is important to note that this study was not powered for QOL. Significant and/or clinically meaningful improvements (small to moderate) [8] from baseline in favor of trametinib were observed for global health; physical, role, and social functioning; fatigue; pain; insomnia; nausea and vomiting; constipation; dyspnea; and appetite at weeks 6 and/or 12. Additionally, chemotherapy patients who crossed over to trametinib on progression experienced large improvements in their global health status, functionality dimensions, and most symptoms (except diarrhea and constipation) within 6 weeks of trametinib treatment. However, this may have been due to these patients having a positive attitude toward a new treatment.
Approximately one-third of melanoma patients have clinically significant levels of distress, particularly around the time of diagnosis and immediately after treatment [9, 10]. In the current study, baseline values for emotional functioning were among the lowest in global health and the five functional QOL dimensions for both treatment arms, providing further evidence that patients with newly diagnosed advanced or metastatic melanoma have poor emotional state of mind. Additionally, trametinib-treated patients reported the greatest impact on emotional functioning at weeks 6 and 12 with a 5- to 6-point improvement in scores relative to baseline.
There is limited information available on the QOL impact of newer treatments for melanoma. Two studies have reported the QOL impact of ipilimumab. In a study by Kotapati et al. [11], patients were randomized to DTIC plus ipilimumab or DTIC alone for 12 weeks, followed by 12 weeks of DTIC only. Changes in score were considered as ‘no change’ (0–5 points), ‘a little’ (5–10 points), ‘moderate’ (10–20 points), and ‘very much’ (>20 points). At week 12, unadjusted mean changes from baseline in both treatment groups were ‘no change’ to ‘moderate’ for all QOL domains including symptom scores. Both groups experienced a small decline in average global health status scores (DTIC + placebo, −6.5; ipilimumab + DTIC, −10.0). In a double-blind, three-arm study [12], patients with previously treated advanced unresectable stage III or IV melanoma were randomized 3:1:1 to ipilimumab + gp100, gp100 alone, or ipilimumab alone. For all study arms, the mean changes in score from baseline to week 12 for global health (ipilimumab + gp100, −7; ipilimumab, −9; gp100, −10), the five functional dimensions (e.g. role functioning: ipilimumab + gp100, −9; ipilimumab −11; gp100, −14), and all symptom scales (e.g. fatigue: ipilimumab + gp100, +11; ipilimumab, +13; gp100, +15) suggested functional impairment and symptom exacerbation.
The impact of dabrafenib (BRAFi) on QOL has been evaluated versus DTIC in patients with BRAF V600E mutation-positive metastatic melanoma [13]. All functionality dimensions, except role, worsened from baseline for DTIC at weeks 6 and 12. For dabrafenib, all functionality scores remained close to baseline or improved at week 6; however, by week 12, physical, role, and cognitive functioning scores worsened by 1–3 points. A clinically meaningful improvement in emotional function with dabrafenib compared with DTIC was observed at weeks 6 (11 points) and 12 (15 points). The mean change in symptom dimensions represented improvements from baseline (except fatigue) with dabrafenib, particularly for appetite loss, insomnia, nausea and vomiting, and pain. Symptom dimensions worsened or did not change from baseline for all symptoms (except pain at week 6) with DTIC, the greatest exacerbations being for fatigue, nausea and vomiting, appetite loss, and dyspnea.
The following limitations of this study should be considered when interpreting the results. Patients participating in clinical studies may be more motivated and optimistic and therefore more likely to report benefit and endure more treatment-related toxicity. This was an open-label study; therefore, any expectations about the potential effects of treatment may have biased the responses to the EORTC QLQ-C30 questionnaire. Furthermore, although the questionnaire is a widely used, reliable, and valid instrument for evaluating QOL in cancer [6, 14–17], the QOL aspects were not specific to melanoma. Finally, all patients had an ECOG performance status of 0 or 1 with a median age of 55 years, hence a relatively younger and healthier patient cohort, potentially making it difficult to demonstrate QOL improvement. Preservation of QOL would be the desirable outcome.
This first report of QOL assessment with an MEKi in metastatic melanoma demonstrated that trametinib conferred a significant PFS and OS benefit versus chemotherapy and that trametinib-treated patients reported a better global health and functional status and less exacerbation of symptoms. With several targeted and immunotherapies being evaluated as combinations or in sequence for the treatment of melanoma QOL assessment will be of importance when assessing the clinical benefit of such treatments.
funding
This work (NCT01245062) was supported by GlaxoSmithKline. All authors listed meet the criteria for authorship set forth by the International Committee for Medical Journal Editors.
disclosure
DS has received research funding from Merck, and has had consultancies and/or participated in advisory boards with GlaxoSmithKline, Roche, Bristol Myers-Squibb, Merck, Amgen, Delcath, and Novartis. RD has received research funding from, and has had consultancies or participated in advisory boards with GlaxoSmithKline. CG is currently conducting research sponsored by GlaxoSmithKline. CR has had consultancies with GlaxoSmithKline, Roche, Bristol Myers-Squibb, and Novartis. PR has received honoraria from Bristol Myers-Squibb and Roche, and participated in advisory board with GlaxoSmithKline, Bristol Myers-Squibb, and Roche. NS has recruited patients for trials sponsored by GlaxoSmithKline, and has received fees to his institution. GU has acted as a medical expert for GlaxoSmithKline. MMA, MC, KG, KP, and FSW are employed by, and hold stocks of, GlaxoSmithKline.
Supplementary Material
acknowledgements
Editorial support in the forms of editorial suggestions to draft versions of this manuscript, collating author comments, copyediting, referencing, and graphic services was provided by Helen Brown at Clinical Thinking and was funded by GlaxoSmithKline.
references
- 1.Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417:949–954. doi: 10.1038/nature00766. [DOI] [PubMed] [Google Scholar]
- 2.Jakob JA, Bassett RL, Jr, Ng CS, et al. NRAS mutation status is an independent prognostic factor in metastatic melanoma. Cancer. 2012;118:4014–4023. doi: 10.1002/cncr.26724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Montagut C, Settleman J. Targeting the RAF-MEK-ERK pathway in cancer therapy. Cancer Lett. 2009;283:125–134. doi: 10.1016/j.canlet.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 4.Flaherty KT, Robert C, Hersey P, et al. Improved survival with MEK inhibition in BRAF-mutated melanoma. N Engl J Med. 2012;367:107–114. doi: 10.1056/NEJMoa1203421. [DOI] [PubMed] [Google Scholar]
- 5.European Organisation for Research and Treatment of Cancer. EORTC quality of life questionnaire (EORTC QLQ-C30) http://groups.eortc.be/qol/eortc-qlq-c30 . [DOI] [PubMed]
- 6.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 7.Scott NW, Fayers PM, Aaronson NK, et al. European Organisation for Research and Treatment of Cancer. EORTC QLQ-C30 reference values. http://groups.eortc.be/qol/sites/default/files/img/newsletter/reference_values_manual2008.pdf . [Google Scholar]
- 8.Osoba D, Rodrigues G, Myles J, et al. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16:139–144. doi: 10.1200/JCO.1998.16.1.139. [DOI] [PubMed] [Google Scholar]
- 9.Al-Shakhli H, Harcourt D, Kenealy J. Psychological distress surrounding diagnosis of malignant and nonmalignant skin lesions at a pigmented lesion clinic. J Plast Reconstr Aesthet Surg. 2006;59:479–486. doi: 10.1016/j.bjps.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 10.Newton-Bishop JA, Nolan C, Turner F, et al. A quality-of-life study in high-risk (thickness ≥or 2 mm) cutaneous melanoma patients in a randomized trial of 1-cm versus 3-cm surgical excision margins. J Investig Dermatol Symp Proc. 2004;9:152–159. doi: 10.1046/j.1087-0024.2003.09118.x. [DOI] [PubMed] [Google Scholar]
- 11.Kotapati S, Francis S, Sherrill B. Health related quality of life (HRQL) of patients receiving ipilimumab with dacarbazine as first-line treatment for unresectable stage III/IV melanoma. Pigment Cell Melanoma Res. 2011;24:1037. abstr SMR-P50. [Google Scholar]
- 12.Revicki DA, van den Eertwegh AJ, Lorigan P, et al. Health related quality of life outcomes for unresectable stage III or IV melanoma patients receiving ipilimumab treatment. Health Qual Life Outcomes. 2012;10:66. doi: 10.1186/1477-7525-10-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grob J, Algarra SM, Amonkar MM, et al. Dabrafenib vs dacarbazine (DTIC) in patients with BRAF V600+ advanced and metastatic melanoma in BREAK-3: quality of life (QOL) analysis. Pigment Cell Melanoma Res. 2013;26:152. [Google Scholar]
- 14.Osoba D, Aaronson N, Zee B, et al. Modification of the EORTC QLQ-C30 (version 2.0) based on content validity and reliability testing in large samples of patients with cancer. The Study Group on Quality of Life of the EORTC and the Symptom Control and Quality of Life Committees of the NCI of Canada Clinical Trials Group. Qual Life Res. 1997;6:103–108. doi: 10.1023/a:1026429831234. [DOI] [PubMed] [Google Scholar]
- 15.Osoba D, Zee B, Pater J, et al. Psychometric properties and responsiveness of the EORTC Quality of Life Questionnaire (QLQ-C30) in patients with breast, ovarian and lung cancer. Qual Life Res. 1994;3:353–364. doi: 10.1007/BF00451727. [DOI] [PubMed] [Google Scholar]
- 16.Hjermstad MJ, Fossa SD, Bjordal K, et al. Test/retest study of the European Organization for Research and Treatment of Cancer Core Quality-of-Life Questionnaire. J Clin Oncol. 1995;13:1249–1254. doi: 10.1200/JCO.1995.13.5.1249. [DOI] [PubMed] [Google Scholar]
- 17.Kaasa S, Bjordal K, Aaronson N, et al. The EORTC Core Quality of Life Questionnaire (QLQ-C30): validity and reliability when analysed with patients treated with palliative radiotherapy. Eur J Cancer. 1995;31A:2260–2263. doi: 10.1016/0959-8049(95)00296-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.