Currently on-going clinical trials in hematological malignancies are unlikely to significantly improve our knowledge of the optimal treatment for older patients as those outcome measures that are of primary importance to this patient population are still included in only a minority of studies. As a scientific community, we cannot continue to simply acknowledge this issue but must all participate in taking the necessary steps to enable the delivery of evidence-based, tailor-made and patient-focused cancer care to our rapidly growing elderly patient population.
Keywords: clinical trials, elderly, study objectives
Abstract
Background
Cancer societies and research cooperative groups worldwide have urged for the development of cancer trials that will address those outcome measures that are most relevant to older patients. We set out to determine the characteristics and study objectives of current clinical trials in hematological patients.
Method
The United States National Institutes of Health clinical trial registry was searched on 1 July 2013, for currently recruiting phase I, II or III clinical trials in hematological malignancies. Trial characteristics and study objectives were extracted from the registry website.
Results
In the 1207 clinical trials included in this overview, patient-centered outcome measures such as quality of life, health care utilization and functional capacity were only incorporated in a small number of trials (8%, 4% and 0.7% of trials, respectively). Even in trials developed exclusively for older patients, the primary focus lies on standard end points such as toxicity, efficacy and survival, while patient-centered outcome measures are included in less than one-fifth of studies.
Conclusion
Currently on-going clinical trials in hematological malignancies are unlikely to significantly improve our knowledge of the optimal treatment of older patients as those outcome measures that are of primary importance to this patient population are still included in only a minority of studies. As a scientific community, we cannot continue to simply acknowledge this issue, but must all participate in taking the necessary steps to enable the delivery of evidence-based, tailor-made and patient-focused cancer care to our rapidly growing elderly patient population.
introduction
Hematological malignancies are frequently diagnosed in older patients. For disease entities such as myelodysplastic syndrome, acute myeloid lymphoma, Non-Hodgkin lymphoma, chronic lymphocytic leukemia and multiple myeloma, the median age at diagnosis is 65 years of age or higher [1]. With the imminent ageing of society [2], hematologists will be faced with increasing numbers of elderly patients with blood cancer.
Historically, older patients and those with comorbidities have been excluded from clinical trials [3]. Among the Food and Drug Administration (FDA) approved treatments for cancer, only 9% of patients enrolled in registration trials were older than 75 years of age, whereas 31% of patients with cancer fall within that age group [4]. Owing to differences in physiological reserves, comorbidity, functional capacity and geriatric syndromes, the elderly represent a heterogeneous population, requiring tailoring of care [5]. It is incorrect to assume that those treatment regimens that are most beneficial to younger patients will also be the best choice for the older individual.
Furthermore, treatment goals for older patients are not always the same as for younger patients. Multiple studies have demonstrated that age is an important factor affecting patient's choices. Although willing to receive chemotherapy [6], elderly patients are generally less willing to accept toxicity for additional survival time [7], particularly when treatment could potentially have a negative impact on quality of life or functional status [8]. Data on these aspects are severely lacking, further complicating the decision-making process for cancer specialists as well as patients and caregivers.
Since the end of the 20th century, cancer societies and research cooperative groups worldwide as well as countless publications have urged for the development of clinical trials that will facilitate or at least allow the inclusion of older patients and those with comorbidity, and that will address those outcome measures that are most relevant to this already significant and rapidly growing patient population [3, 9–11]. Fifteen years onward, many questions remain unanswered. There are still no adequate data on which to base treatment choice, adjust dosing or anticipate possible side-effects for the elderly [9]. Given the time that transpires between the first conceptualization of a study and the actual publication of final results, any progress in the next 10 years is most likely to come from clinical trials that are currently ongoing. However, this is only possible if these trials will incorporate those outcome measures that are most relevant to elderly patients. To evaluate this question, we set out to determine the characteristics and study objectives of current clinical trials in hematological patients.
methods
To identify on-going phase I, II or III clinical trials in hematological malignancies, the United States National Institutes of Health clinical trial registry (www.clinicaltrials.gov) was searched on 1 July 2013, using the search terms ‘cancer’ and ‘hematological neoplasm’. The search was limited to interventional phase I, II and III trials, or mixed phase I/II or II/III trials, currently recruiting patients or due to start recruiting within the next 6 months; trials with unknown recruitment status or without any verification of recruitment status in the last 12 months were excluded.
For included trials, the following data were extracted from the registry website: target disease entities, source of funding, type of intervention, in- and exclusion criteria with regard to age and performance status (PS), primary and secondary study objectives and start year of the study. Trials were considered as exclusively for older patients if they excluded patients <60 years of age.
To allow combining of data on PS, Karnofsky PS of 100 was considered equivalent of World Health Organization PS 0, Karnofsky PS 80–90 equivalent to WHO PS 1, 60–70 as WHO PS 2, 40–50 as WHO PS 3 and ≤30 as WHO PS 4 [12].
Study objectives (both primary and secondary) were classified into 10 categories (Appendix 1): overall survival, progression-free survival, efficacy, toxicity, treatment completion, pharmacological parameters, health care utilization, biological outcome parameters, quality of life and functional outcomes.
statistical analysis
To assess differences between categories, the χ2 test was used or a trend test (linear-by-linear) when levels were ordered. A P-value of <0.05 was considered significant.
results
A total of 39 376 trials were identified in the trial registry search (Figure 1); of which, 1207 were included in this overview. The study characteristics of these trials are summarized in Table 1. The trials covered a wide range of diagnoses, with the most frequent being multiple myeloma (16%), acute myeloid leukemia (11%) and Non-Hodgkin lymphoma (10%). Almost all trials included some form of chemotherapy (96%), with 43% using biologicals and 8% involving some type of transplantation. Phase II trials comprised 43% of included trials; 24% were phase I trials, 19% combined phase I and II, 1% combined phase II and III and 12% phase III trials. Overall, 47% of trials were industry-sponsored.
Figure 1.
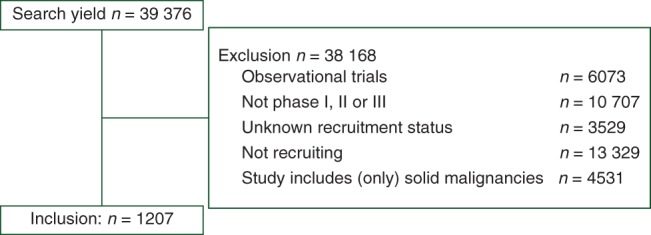
Search results and trial selection.
Table 1.
Characteristics of selected trials
| All trials (N = 1207) |
Trials exclusively for the elderlya (N = 62) |
|||
|---|---|---|---|---|
| n | % | n | % | |
| Diagnosis | ||||
| Multiple hematological malignancies | 451 | 37 | 16 | 26 |
| Acute lymphocytic leukemia | 49 | 4 | 1 | 2 |
| Acute myeloid leukemia | 135 | 11 | 26 | 42 |
| Chronic lymphocytic leukemia | 81 | 7 | 6 | 10 |
| Chronic myeloid leukemia | 46 | 4 | 0 | –b |
| Multiple myeloma | 196 | 16 | 5 | 8 |
| Myelodysplastic syndrome | 64 | 5 | 0 | –b |
| Non-Hodgkin lymphoma | 122 | 10 | 5 | 8 |
| Hodgkin's lymphoma | 36 | 3 | 2 | 3 |
| Other diagnoses | 27 | 2 | 1 | 2 |
| Start of inclusion | ||||
| ≤2005 | 34 | 3 | 2 | 3 |
| 2006–2007 | 54 | 5 | 0 | – |
| 2008–2009 | 140 | 12 | 3 | 5 |
| 2010–2011 | 395 | 33 | 24 | 39 |
| 2012–2013 | 584 | 48 | 33 | 53 |
| Interventionc | ||||
| Chemotherapy | 1161 | 96 | 62 | 100 |
| Biologicals | 514 | 43 | 23 | 37 |
| HSCTd | 98 | 8 | 1 | 2 |
| Other interventions | 41 | 4 | 0 | - |
| Phase | ||||
| I | 307 | 25 | 7 | 11 |
| I/II | 227 | 19 | 10 | 16 |
| II | 513 | 43 | 28 | 45 |
| II/III | 13 | 1 | 1 | 2 |
| III | 147 | 12 | 16 | 26 |
| Industry-sponsored | 568 | 47 | 33 | 53 |
| Lower age limits, years | ||||
| <21 | 1129 | 94 | –b | –b |
| 22–59 | 16 | 1 | –b | –b |
| 60–64 | 43 | 4 | 43 | 69 |
| 65–69 | 15 | 1 | 15 | 24 |
| 70+ | 4 | 0 | 4 | 7 |
| Upper age limits, years | ||||
| None | 830 | 69 | 53 | 85 |
| <50 | 66 | 5 | –b | –b |
| 51–64 | 45 | 4 | –b | –b |
| 65–69 | 73 | 6 | 1 | 2 |
| 70–74 | 73 | 6 | 0 | –b |
| 75–79 | 78 | 7 | 4 | 7 |
| 80–84 | 32 | 3 | 4 | 7 |
| 85–90 | 10 | 1 | 0 | –b |
| Performance status (PS)c | ||||
| PS 0 included | 1198 | 99 | 58 | 94 |
| PS 1 included | 1199 | 99 | 59 | 95 |
| PS 2 included | 1012 | 84 | 54 | 87 |
| PS 3 included | 328 | 27 | 21 | 34 |
| PS 4 included | 230 | 19 | 13 | 21 |
aTrials are considered as exclusively for the elderly if they exclude patients younger than 60 years of age.
bNot applicable.
cTrials could have multiple interventions and multiple sponsors.
dHematopoietic stem cell transplantation.
Most trials had a lower age limit for inclusion <21 years of age (94%, Table 1). Two-thirds of trials did not name an upper age limit; 5% had an upper age limit <50 years of age, 10% between 51 and 69 years, 13% between 70 and 79 years and 4% between 80 years and higher. Exclusion based on older age varied greatly depending on the disease entity being targeted. For instance, only 3% of chronic lymphocytic leukemia trials excluded patients over the age of 70, compared with 63% of acute lymphocytic leukemia trials (Table 2). Industry-sponsored studies were three times less likely to exclude older patients than non-industry-sponsored trials (exclusion of patients older than 70 years in 30% versus 10%, P = 0.001).
Table 2.
Comparison of age at diagnosis of hematological malignancies with age-based exclusion
| Diagnoses | On-going clinical trials |
SEER dataa |
||
|---|---|---|---|---|
| Patients aged 65+ years excluded (%) | Patients aged 70+ years excluded (%) | Median age at diagnosis (years) | % older than 65 years at diagnosis | |
| Acute lymphocytic leukemia | 57 | 63 | 14 | 10.8 |
| Hodgkin lymphoma | 33 | 39 | 38 | 17.7 |
| Chronic myeloid leukemia | 11 | 17 | 64 | 48.8 |
| Non-Hodgkin lymphoma | 3 | 12 | 66 | 54.4 |
| Acute myeloid leukemia | 26 | 35 | 67 | 54.1 |
| Multiple myeloma | 7 | 14 | 69 | 62.4 |
| Myelodysplastic syndrome | 2 | 8 | 70 | 80.0 |
| Chronic lymphocytic leukemia | 1 | 3 | 71 | 68.1 |
aThe SEER (Surveillance Epidemiology and End-Results) program collects information on incidence, prevalence and survival from specific geographic areas representing 28 percent of the United States population.
Almost all trials allowed inclusion of patients with PS 0 or 1, 16% excluded patients with PS 2 and 73% excluded PS 3. Eight trials only included patients with PS 2 or higher.
study objectives
As was expected, outcome measures varied per trial phase (Table 3). Toxicity was the most frequently mentioned study objective (80% of all trials), followed by treatment efficacy (73%), progression-free survival (52%) and overall survival (39%). Patient-centered outcomes were included in <1% of phase I trials, 10% of phase II trials and 34% of phase III trials. Of the latter, 31% of trials addressed quality of life, 12% health care utilization, 4% completion of treatment and 2% functional outcomes. Only 2 of the 1207 trials address the prognostic value of geriatric assessments, and no studies mentioned cognitive outcome measures.
Table 3.
Study objectives
| All trials (N = 1207) (%) | Phase I (N = 307) (%) | Phase II (N = 513) (%) | Phase III (N = 147) (%) | |
|---|---|---|---|---|
| Toxicity | 80 | 96 | 69 | 60 |
| Efficacy | 73 | 60 | 75 | 78 |
| Progression-free survival | 51 | 21 | 64 | 84 |
| Overall survival | 39 | 15 | 46 | 67 |
| Biological parameters | 28 | 35 | 29 | 21 |
| Pharmacological parameters | 19 | 38 | 12 | 16 |
| Quality of life | 8 | 1 | 7 | 31 |
| Health care utilization | 4 | 1 | 4 | 12 |
| Completion of treatment | 2 | 0 | 3 | 4 |
| Functioning | 0.7 | 0.3 | 0.8 | 2 |
For each trial phase, industry-sponsored trials were more likely to address patient-centered outcome measures such as quality of life (overall 9.9% versus 5.5% in non-industry-sponsored trials, P = 0.004) and health care utilization (overall 6.2% versus 2.2% in non-industry-sponsored trials, P < 0.001).
trials exclusively for older patients
Sixty-two trials focused exclusively on the elderly (Table 1). Over two-thirds of trials used a lower age limit of 60 years, 24% limited inclusion to patients aged 65 years and older, 7% to 70 years or older of which one trial used a lower age limit of 80 years. Nine elderly-specific trials also used an upper age limit, with four trials using a cut-off of 75 years and four a cut-off of 80 years; one study only including patients between 60 and 65 years.
Acute myeloid leukemia was the target disease in 26 of these 62 trials, representing 42% (Table 1); other frequently targeted conditions were chronic lymphocytic leukemia (10%), multiple myeloma (8%) and Non-Hodgkin lymphoma (8%). Most trials focused on chemotherapy, with 37% using biologicals and only one study involving some form of transplantation. Approxi-mately two-thirds of trials were phase II or combined phase I/II or II/III trials. Over half of the trials were industry-sponsored, 8% were sponsored by the National Institutes of Health and 71% had other sponsors.
Efficacy, toxicity and progression-free survival were the most studied outcome measures, each being included in over two-thirds of trials; overall survival was included in 58% (Table 4). Quality of life was addressed in 18% of trials, pharmacological parameters in 15%, biological outcome measures in 10% and health care utilization in 7%. Only one trial addressed the functional outcome (2%). Two trials addressed the prognostic value of geriatric assessments (3%).
Table 4.
Study objectives for trials exclusively for the elderly
| Trials exclusively for elderlya (%) | All other trials (%) | P-value | |
|---|---|---|---|
| Toxicity | 71 | 80 | 0.08 |
| Efficacy | 76 | 73 | 0.61 |
| Progression-free survival | 66 | 51 | 0.02 |
| Overall survival | 58 | 38 | 0.002 |
| Biological parameters | 10 | 29 | 0.001 |
| Pharmacological parameters | 15 | 20 | 0.31 |
| Quality of life | 18 | 7 | 0.002 |
| Health care utilization | 7 | 4 | 0.33 |
| Completion of treatment | 3 | 2 | 0.40 |
| Functioning | 2 | 0.7 | 0.42 |
aTrials were considered as exclusively for the elderly if they exclude patients aged 60 years of age or younger.
Compared with all the other trials, those specifically targeting the elderly more often focus on progression-free survival (66% versus 51%, P = 0.01; Table 4) and overall survival (58% versus 38%, P = 0.001) as well as quality of life (18% versus 7%, P = 0.001) and less on biological outcome parameters (10% versus 29%, P = 0.001). There was also a trend towards less focus on toxicity (71% versus 80%, P = 0.08).
discussion
In this overview of phase I–III hematological trials registered in the National Institutes of Health clinical trial registry, patient-centered outcome measures such as quality of life, health care utilization and functional capacity were only incorporated in a small number of trials (8%, 4% and 0.7% of trials, respectively). Even in trials developed exclusively for older patients, the primary focus lies on standard end points such as toxicity, efficacy and survival, while patient-centered outcome measures are included in less than one-fifth of studies.
This study has several limitations. First of all, we have focused exclusively on the National Institutes of Health (NIH) clinical trial registry and therefore, and we do not have a full representation of all clinical trials worldwide. However, the NIH trial registry is by far the largest; as a comparison, a search of the second largest registry (the European Union clinical trial registry—www.clinicaltrialregister.eu) using the same search terms yields only 4200 trials, nearly 1/10th of the number included in this overview. A second limitation is that we only had access to the data as reported by the primary investigators on the registry website. It is possible that other outcome measures or study objectives are included in the study protocol that was not considered of sufficient importance to be mentioned on the registry website. However, we believe that this is unlikely to occur on a large scale and therefore do not feel that an in-depth study of the trial protocols would have significantly altered the outcomes of this overview.
Previous studies have demonstrated that although willing to receive chemotherapy [6], older patients may have a more conservative approach to toxicity [7]. Although they do desire life-prolonging treatment when diagnosed with cancer, they are unwilling to suffer severe side-effects that will change their quality of life, their ability to function independently in their daily tasks, their cognitive function, their social situation and capability to remain at home or their caregiving abilities [8, 13]. Thus, prolongation of active life expectancy is much more important than that of life expectancy as such [12]. For instance, in one study, 80% of all patients gave greater priority to the quality of life than the length of life [14]. For some patients, the long-term prospects of life after treatment will not meet the individual's required minimum level of quality of life, rendering the treatment unacceptable to that person [15]. Furthermore, the heterogeneity of the older patient population may lead standard end point such as overall or relapse-free survival to take on a different meaning. For instance, older patients and those with comorbidity are more likely to die of other causes, and thus relapse will not always affect survival [13]. At the moment, we are unable to advise patients with regard to their options, as data on these outcome measures are almost entirely lacking.
As demonstrated by this overview, little is currently being done to salvage this issue. Clearly, there is a mismatch between priorities identified by patients and currently on-going cancer research. This was also demonstrated by a study carried out in the United Kingdom, in which patients were asked to rate the priority of various aspects of cancer research [16]. In this study, patients gave the highest priority to ‘the impact of cancer on life, how to live with cancer and related support issues’, while research on treatment and toxicity was given a much lower priority [16].
Over the last decade, both cancer specialists and geriatricians have indicated that research for the elderly should focus more on patient-centered outcome measures [17]. They have stated that in order to help clinicians and patients weigh the full risk and benefits of treatment, quality of life, functional status and independence of patients should be assessed in clinical trials in addition to standard efficacy end points [9, 10]. This viewpoint has been endorsed by cancer societies, research cooperatives and cancer experts worldwide and reiterated in a myriad of publications. Therefore, it is disappointing to find that these outcome measures are still rarely included, even in studies focusing specifically on older patients. As a scientific community, we cannot be satisfied with simply continuing to acknowledge the lack of evidence that is needed to provide older patients with cancer care that is tailored to their wishes and their particular situation. If we are to make any progress, researchers, cancer specialists, geriatricians, sponsors, patient advocates and government agencies must all step up and take action to resolve this issue.
A first step is developing studies that will allow for the inclusion of older patients, particularly for disease entities that occur primarily in the elderly. As demonstrated by Table 2, for at least five types of hematological malignancy, the median age at diagnosis is higher than 65 years of age [1]. However, despite this fact, a significant proportion of studies still excluded older patients based on their chronological age. Furthermore, it should become mandatory that the study population is an adequate reflection of the real-life patient population. Thus, not only should older patients be allowed to enter clinical trials, but also they should be actively recruited. Some researchers have questioned the desirability of including older patients with comorbidity, as these patients are less likely than younger patients to benefit from certain therapies, as increasing elderly participation in clinical trials could produce less-conclusive results with smaller treatment effects [18]. However, the clinical applicability of the results of a cancer treatment trial depends largely on whether the study participants are representative of the population of interest [19]. Thus, in disease entities in which the majority of patients actually are older patients with comorbidities, including these patients will supply a much more faithful reflection of the true clinical benefit [13]. Such trials will allow cancer specialists to make treatment recommendations that apply to their actual patient population rather than to a highly selected subgroup.
Secondly, trialists must resolve to incorporate patient-centered outcome measures in all clinical trials carried out in diseases that occur primarily in older patients and should be specifically powered to detect differences in these outcomes. Longitudinal changes in functional status, cognitive function and quality of life should be standard end points in such clinical trials [20]. These outcomes could be affected both positively by cancer treatment, for instance by countering cancer-related symptoms and fatigue, as well as negatively due to treatment-related complications and toxicity. Potentially, composite end points combining efficacy, toxicity and patient acceptability, such as therapeutic success [21] or overall treatment utility [22] or quality-adjusted treatment outcomes such as the Q-TWIST (quality-adjusted time without symptoms of disease or toxicity of treatment) [23], could be a useful method of integrating multiple relevant but potentially conflicting outcome measures into one end point.
Finally, it is adamant that a geriatric evaluation be incorporated as a routine part of baseline assessment for all older trial participants. Geriatric assessments provide a more detailed description of the study population, thus allowing insights into which elderly patients were actually included in the trial and how representative the trial population is of the general older population [13]. Furthermore, assessing the predictive value of geriatric impairments for unwanted outcomes can aid in resolving the on-going discussion on the role that should be given to a geriatric assessment in treatment decision-making process. Of the 1207 trials included in this overview, including the 62 trials focusing specifically on older patients, on two report the incorporation of a geriatric assessment on the trial registry website.
In conclusion, currently on-going clinical trials in hematological malignancies are unlikely to significantly improve our knowledge of the optimal treatment of older patients as those outcome measures that are of primary importance to this patient population are still included in only a minority of studies. We cannot continue to simply acknowledge this issue, but must all participate in taking the necessary steps to enable the delivery of evidence-based, tailor-made and patient-focused cancer care to our rapidly growing elderly patient population.
disclosure
The authors have declared no conflicts of interest.
appendix
Table A1.
Classification of study objectives
| Study objective | Classified as … |
|---|---|
| Overall survival | Overall survival |
| Mortality at a particular time point during follow-up | |
| Progression-free survival | Progression-free survival |
| Event-free survival | |
| Disease-free survival | |
| Time-to-progression | |
| Duration of response | |
| Toxicity | Toxicity |
| Safety | |
| Feasibility | |
| Maximum-tolerated dose | |
| Response | Efficacy |
| Efficacy | |
| Time-to-response | |
| Engraftment | |
| Completion of planned treatment | Completion |
| Achieved dose intensity | |
| Compliance to treatment | |
| Pharmacokinetics | Pharmacological parameters |
| Pharmacodynamics | |
| Health care utilization | Healthcare utilization |
| Health economics | |
| Laboratory parameters | Biological parameters |
| Genetic parameters | |
| Tumor biology | |
| Quality of life | Quality of life |
| Care dependence | Functioning |
| Institutionalization |
references
- 1. seer.cancer.gov. 2013.
- 2.Gundrum DJ, Go RS. Cancer in the oldest old in the United Status: current statistics and projections. J Geriatr Oncol. 2012;3:299–306. [Google Scholar]
- 3.Hutchins LF, Unger JM, Crowley JJ, et al. Underrepresentation of patients 65 years of age or older in cancer-treatment trials. N Engl J Med. 1999;341(27):2061–2067. doi: 10.1056/NEJM199912303412706. [DOI] [PubMed] [Google Scholar]
- 4.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291(22):2720–2726. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- 5.Extermann M, Aapro M, Bernabei R, et al. Use of comprehensive geriatric assessment in older cancer patients: recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG) Crit Rev Oncol Hematol. 2005;55(3):241–252. doi: 10.1016/j.critrevonc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Extermann M, Albrand G, Chen H, et al. Are older French patients as willing as older American patients to undertake chemotherapy? J Clin Oncol. 2003;21(17):3214–3219. doi: 10.1200/JCO.2003.08.091. [DOI] [PubMed] [Google Scholar]
- 7.Yellen SB, Cella DF, Leslie WT. Age and clinical decision making in oncology patients. J Natl Cancer Inst. 1994;86(23):1766–1770. doi: 10.1093/jnci/86.23.1766. [DOI] [PubMed] [Google Scholar]
- 8.Chouliara Z, Miller M, Stott D, et al. Older people with cancer: perceptions and feelings about information, decision-making and treatment—a pilot study. Eur J Oncol Nurs. 2004;8(3):257–261. doi: 10.1016/j.ejon.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Hurria A, Mohile SG, Dale W. Research priorities in geriatric oncology: addressing the needs of an aging population. J Natl Compr Canc Netw. 2012;10(2):286–288. doi: 10.6004/jnccn.2012.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pallis AG, Ring A, Fortpied C, et al. EORTC workshop on clinical trial methodology in older individuals with a diagnosis of solid tumors. Ann Oncol. 2011;22(8):1922–1926. doi: 10.1093/annonc/mdq687. [DOI] [PubMed] [Google Scholar]
- 11.Hurria A, Cohen HJ, Extermann M. Geriatric Oncology Research in the Cooperative Groups: a report of a SIOG special meeting. J Geriatr Oncol. 2010;1(1):40–44. doi: 10.1016/j.jgo.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ma C, Bandukwala S, Burman D, et al. Interconversion of three measures of performance status: an empirical analysis. Eur J Cancer. 2010;46(18):3175–3183. doi: 10.1016/j.ejca.2010.06.126. [DOI] [PubMed] [Google Scholar]
- 13.Wildiers H, Mauer M, Pallis A, et al. End points and trial design in geriatric oncology research: a Joint European Organisation for Research and Treatment of Cancer-Alliance for Clinical Trials in Oncology-International Society of Geriatric Oncology Position Article. J Clin Oncol. 2013;31(29):3711–3718. doi: 10.1200/JCO.2013.49.6125. [DOI] [PubMed] [Google Scholar]
- 14.Meropol NJ, Egleston BL, Buzaglo JS, et al. Cancer patient preferences for quality and length of life. Cancer. 2008;113(12):3459–3466. doi: 10.1002/cncr.23968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kiebert GM, Stiggelbout AM, Kievit J, et al. Choices in oncology: factors that influence patients' treatment preference. Qual Life Res. 1994;3(3):175–182. doi: 10.1007/BF00435382. [DOI] [PubMed] [Google Scholar]
- 16.Corner J, Wright D, Hopkinson J, et al. The research priorities of patients attending UK cancer treatment centres: findings from a modified nominal group study. Br J Cancer. 2007;96(6):875–881. doi: 10.1038/sj.bjc.6603662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Puts MT, Girre V, Monette J, et al. Clinical experience of cancer specialists and geriatricians involved in cancer care of older patients: a qualitative study. Crit Rev Oncol Hematol. 2010;74(2):87–96. doi: 10.1016/j.critrevonc.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 18.Lewis JH, Kilgore ML, Goldman DP, et al. Participation of patients 65 years of age or older in cancer clinical trials. J Clin Oncol. 2003;21(7):1383–1389. doi: 10.1200/JCO.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 19.Townsley CA, Selby R, Siu LL. Systematic review of barriers to the recruitment of older patients with cancer onto clinical trials. J Clin Oncol. 2005;23(13):3112–3124. doi: 10.1200/JCO.2005.00.141. [DOI] [PubMed] [Google Scholar]
- 20.Lichtman SM. Clinical trial design in older adults with cancer: the need for new paradigms. J Geriatr Oncol. 2012;3(4):368–375. [Google Scholar]
- 21.Ardizzoni A, Favaretto A, Boni L, et al. Platinum-etoposide chemotherapy in elderly patients with small-cell lung cancer: results of a randomized multicenter phase II study assessing attenuated-dose or full-dose with lenograstim prophylaxis—a Forza Operativa Nazionale Italiana Carcinoma Polmonare and Gruppo Studio Tumori Polmonari Veneto (FONICAP-GSTPV) study. J Clin Oncol. 2005;23(3):569–575. doi: 10.1200/JCO.2005.11.140. [DOI] [PubMed] [Google Scholar]
- 22.Seymour MT, Thompson LC, Wasan HS, et al. Chemotherapy options in elderly and frail patients with metastatic colorectal cancer (MRC FOCUS2): an open-label, randomised factorial trial. Lancet. 2011;377(9779):1749–1759. doi: 10.1016/S0140-6736(11)60399-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldhirsch A, Gelber RD, Simes RJ, et al. Costs and benefits of adjuvant therapy in breast cancer: a quality-adjusted survival analysis. J Clin Oncol. 1989;7(1):36–44. doi: 10.1200/JCO.1989.7.1.36. [DOI] [PubMed] [Google Scholar]


