Abstract
Most studies of childhood asthma management use data from a single family reporter and fail to capture the parent-child dyadic influences. In this descriptive exploratory study with 183 parent-child dyads, data were collected from both parents and children. Using structural equation modeling, the relationships of parents’ and children’s asthma knowledge, self-efficacy to manage asthma, and asthma management on the child’s quality of life were examined. Direct significant relationships from knowledge to self-efficacy to asthma management were found for each member of the dyad. The associations between parents’ and children’s self-efficacy and asthma management were not statistically significant. Only the children’s self-efficacy to manage asthma was significantly associated with children’s asthma-related quality of life.
Keywords: asthma self-management, self-efficacy, quality of life
Asthma is a significant health problem for children, with 10 million children (14%) having a history of asthma and 7 million (10%) children experiencing asthma symptoms in the previous 12 months (U.S. Department of Health and Human Services [USDHHS], 2011). Asthma is a complex condition with features of underlying airway inflammation, smooth muscle hyperresponsiveness, and immunological factors that are released in response to a variety of environmental irritants (Orihara, Dil, Anaparti, & Moqbel, 2010). The family’s work to manage children’s asthma is complicated by the variable nature of asthma symptom onset (e.g. in the presence of seasonal allergens or when children participate in sports) and in response to a wide range of stimuli, many of which are not allergens (e.g., hot or cold weather, scents, odors, exercise: American Academy of Allergy and Immunology [AAAAI], 2004; Orihara et al., 2010). While parents are seen as having the primary responsibility for asthma management in the home, as children mature and develop they take on more responsibility for the day-to-day management of asthma while their parents assume a more supervisory-type role (Horner, Brown, & Walker, 2012; Parke, 2004). Overtime responsibility for asthma management in childhood becomes work that is shared between the parent and the child with asthma (Dixon & Stein, 2000; Parke, 2004).
While many studies have been conducted to improve parents’ and children’s management of this complex condition, they fail to capture the work that is shared by the parent-child dyad (Marcellus, 2006). In many studies of childhood chronic illness a single respondent, usually the parental caregiver, provides all the data for the family. In this instance, the parent report is seen as a proxy for child data but this approach fails to capture the child’s perspective (Gannoni & Shute, 2010). Studies have shown that parents tend to underestimate illness symptoms and associated limitations (Taggart, Wittich, & Yawn, 2006). In other studies that collect data from both parent and child, the data are treated as independent factors rather than being treated as non-independent or correlated factors due to the intra-familial influences family members have on each other (Knafl, et al., 2009; Marcellus, 2006). In a recently completed longitudinal study, data pertaining to asthma management were collected from both the primary parental caregiver and the child with asthma to examine changes over time in these factors (Horner & Brown, 2014). The purpose of the current analysis was to explore the dyadic influences on asthma management and children’s asthma-related quality of life.
Literature Review
This literature review will focus on methodological studies that used dyadic approaches and were conducted with parents and their children who had chronic illnesses. In addition, studies examining the effect of asthma management interventions on children’s asthma-related quality of life will be summarized.
Studies Using Dyadic Analysis
Dyadic analysis is used when the assumption of data independence is violated. Most statistical analyses in which comparisons are made between groups are based on the principle of independence of the data collected, meaning that the behaviors of one participant are not seen to influence the other participant’s behaviors (Field, 2013). However, when it is possible that the behaviors of one participant do influence another’s behaviors, then these data are considered to be non-independent (Kenny, Kashy, & Cook, 2006). Specifically, when data are obtained from different members of the same family they are expected to be correlated given the shared experiences of family members (Knafl et al., 2009). Dyadic analysis has most commonly been used in studies of couple’s relationships (e.g. Anderson & Johnson, 2010; Pruchno, Wilson-Genderson, & Cartwright, 2009), far fewer studies have examined parent-child dyadic experiences. In this section we will review studies using dyadic analytic approaches with parents and children who have chronic illnesses.
For children with chronic illnesses the developmental transition to adolescence is complicated by the physiological changes of puberty and the psychosocial tasks to achieve greater independence in role functions (Anderson et al., 2009; Dixon & Stein, 2000). During early adolescent, youth with type 1 diabetes are found to have poor glycemic control due in part to increased insulin resistance present during puberty but also due to increased non-adherence to the diabetes management routine. Anderson et al. (2009) conducted a study in families (n = 121) with a child (aged 9 – 14 years) who had type 1 diabetes, to examine parents’ and children’s reports of responsibility for type 1 diabetes mellitus management and to see if this perception affected glycemic control. Responsibility was assessed by asking parents and children to rate “who” (i.e., the parent, the child, or both) was responsible for specific tasks of diabetes management. When agreement was high between the parent-child dyad scores of diabetes-management responsibility, the child had better glycemic control (r = −.21, p = .02). Discordance occurred in parent-child dyad scores when the child’s and parent’s ratings of ‘who’ was responsible for a task were not in agreement. Discordance was found more among the younger children (< 12 years: r = −.24, p = .007). The authors indicate that in the pre-pubertal years, parents begin to assign specific diabetes self-management tasks to their younger children in an effort to prepare them to become more independent. However, if the child is not yet ready to assume these responsibilities, then their scores on these tasks would not agree with their parents’ scores on the same tasks.
Some dyadic studies have been conducted preliminarily to enacting large scale projects to determine whether researchers should rely solely on parental report (i.e., as a proxy for the child) or if the child should also self-report. For example, school personnel have been faced with children who exhibit health problems that were not reported by their parents on the school health record because the parents thought it would not be a problem in the school setting (Taggart et al., 2006). To identify which children in a school would benefit from a proposed intervention, Wittich, Li, and Gerald (2006) conducted a study comparing children’s self-reports with their parents’ proxy reports of asthma diagnosis and asthma symptoms. Complete data were obtained from a largely African American (91%) sample of parent-child dyads (n = 2593 dyads) with children in grades 1–4 at one of 10 public elementary schools. Using McNemar’s test of agreement between children’s and parents’ responses (i.e., yes or no) to questions about asthma and asthma symptoms, the investigators found the dyad’s responses were consistent (p < .0001). The kappa coefficient measured the degree of agreement between the dyad’s responses and was found to range from low (.15) to good (.60). There was good agreement between parents and children that the children did or did not have a diagnosis of asthma (k = .60) and were taking medications for asthma (k = .59), but children reported more asthma symptoms in comparison to their parents’ reports (e.g. waking up with asthma symptoms, k = .15; having asthma symptoms in past 12 months, k = .33). Wittich et al. attributed these differences to the more subjective nature of asthma symptoms experienced by the children that the parents may not have observed in contrast to the more objective information about having a diagnosis of asthma. Based on parent report alone, only 25% of the children would be deemed eligible for the project, whereas the children’s reports of symptom frequency indicated that 53% would have been classified as possibly having asthma and could be invited to participate in the planned program.
Similarly, in a study to identify children with asthma who could be invited to take part in a self-management study, Yawn, Wollan, Kurland, and Bertram (2006) compared parents’ and children’s (grades 3–12) responses to asthma surveys in a private school setting (n = 1429 dyads). There was considerable agreement (83%–94%) between parents and their children on questions pertaining to asthma medications and health care visits (McNemar’s test p = .02 to < .0001). But they also found some disagreements as to the frequency of asthma symptoms. The children reported having more frequent asthma symptoms than their parents reported (p < .05). Noting that children spend nearly one-third of their days away from parental supervision (e.g. at school, at play), the sole reliance by health care providers on parental data may overlook asthma symptomatic episodes experienced by the children when they are not in the parents’ presence. However, investigators also found some dyads reported asthma-type symptoms even though the child was not diagnosed with asthma. In this case, the presence of undiagnosed asthma is a possibility and indicates the need for further assessments to determine whether referral is needed.
Joseph, Havstad, Johnson, Vinuya, and Ownby (2006) evaluated the degree of agreement between African American adolescents’ (n = 63) and their parents’ reports of asthma control and management to determine which is the better informant of adolescents’ health – the adolescent, the parent, or both. The mean differences between parents’ and adolescents’ report of the frequency of daytime symptoms, activity limitations, and sleep disturbance due to asthma were fairly small and not statistically significant. In contrast, parents rated their adolescents’ asthma severity and degree of asthma control worse than did the adolescents themselves (p = .04). The adolescents may be down-playing their asthma to avoid being seen as being different from their peers (Dixon & Stein, 2000). In addition, fewer parents reported their adolescent smoked than did the adolescents themselves (k = .62, p < .01). Consistent with the previous studies, the findings highlight the importance of gathering data from both adolescents and parents.
These studies showcased the degree of agreement and disagreement between parents’ and children’s reports of health care visits, symptom frequency, medication management, and responsibility for self-management. In general, the dyads agreed on health care visits and medications, but there were disagreements about frequency of symptoms, degree of control of symptoms, and who was responsible for self-management tasks. More importantly, these studies highlight the importance of gathering data from both parents and children. What has not been captured in these studies is the contribution of parents and children to the work of managing asthma and how this work influences children’s asthma-related quality of life (Knafl et al., 2009).
Asthma-related Quality of Life Studies
Quality of life (QOL) is a multidimensional concept based on subjective perceptions of health status, functional limitations, impairments, and symptom experiences in the context of past experiences and hopes for the future (Clarke & Calam, 2012; Van Bragt et al., 2012; Walker et al., 2008). Perceptions of QOL are frequently based on one’s ability to work or perform activities whether or not symptoms are present (Walker et al., 2008). Factors that can affect asthma-related QOL (ARQOL) include asthma severity, asthma control, limitations to engaging in usual activities (e.g., school attendance, play, work absenteeism), and socioeconomic status (Everhart & Fiese, 2009; Gandhi et al., 2013; Walker et al., 2008). In this section we will review intervention studies designed to improve children’s ARQOL.
Psychosocial interventions designed to improve asthma self-management and ARQOL have been tested with families of children who have asthma (Clarke & Calam, 2012). In a systematic review of asthma educational interventions that used standardized measures of ARQOL, Clarke and Calam (2012) found only four of 18 studies showed significant improvements in QOL. These four studies used a variety of learning approaches but the factors they had in common were the use of multiple educational sessions rather than a single session, interactive learning strategies with hands-on activities and problem-solving, and engagement of the child participants rather than focusing exclusively or primarily on parents.
Watson et al. (2007) randomized children (n = 398) who were seen in the ED to treatment or control groups. The children were an average of 7.4 years old (range = 3 to 16 years) and a majority (67%) were non-Hispanic whites. Interactive education sessions were provided to small groups (e.g., 6–8 families) of children and their caregivers in the treatment group during four weekly meetings. The education sessions targeted parents-only if they had young children (ages 3–6 years), both parents and child together for school-aged children (ages 7–11), and separate parent and child groups for older children (ages 12–16 years). Post-intervention data were collected over 12-months. While all children demonstrated improvements in their ARQOL, the treatment group had significant improvements in the frequency of asthma symptoms (p = .03) and reductions in ED visits (p = .0037). Parent’s QOL significantly improved, but this was not different between the treatment or control groups. Providing the intervention to both parents and children led to significant improvements in health care utilization for the treatment group. However, this study did not examine dyadic factors.
Because previous research has demonstrated disagreements between parents and children’s reports of asthma symptoms and the impact of asthma on daily life, Burks and colleagues (2013) conducted a clinic-based study to compare children’s (ages 7–17 years) self-reports of ARQOL with their parents’ proxy reports of their children’s ARQOL using the same tool (i.e., Juniper’s Pediatric Asthma QOL Questionnaire). The analysis was based on complete data from 67 parent-child dyads and a majority of the children were boys (73%) and Hispanic (75%). Results found no significant differences between children’s total ARQOL, emotional functioning ARQOL, or asthma symptom ARQOL and their parents’ proxy scores on these same scales. However, there was a statistically significant difference in the activity limitation subscale (p = .001) with children reporting better ARQOL in this domain. The researchers then examined the data by gender subgroups. Boys reported significantly better ARQOL in the activity limitations domain (p < .001), emotional functioning domain (p = .02), and total QOL (p = .009) than their parents’ proxy reports. Girls tended to score lower than their parents, but this difference was not statistically significant. Noting that one’s assessment of QOL is based on one’s ability to work or engage in activities (see Walker et al., 2008), boys may rate their activity limitations QOL higher if they can continue to participate in sports or active play with friends despite asthma symptoms. In fact, some boys have indicated that their breathing problems were no different from their team mates who did not have asthma (see Horner, 1999). The results highlight the importance of gathering data from both the child and their parent, rather than relying solely on the parent proxy reports. Clarifying differences between parents’ and children’s perceptions of asthma may help guide health care providers as they work with families to improve children’s health outcomes.
Methods
As part of a randomized control trial to test an intervention to improve parents’ and children’s asthma self-management, data were collected from both parents and children. Few studies have examined the influence of parents’ and children’s behaviors on each other or on the child’s health outcomes. The present analysis examined the dyadic influences of parents’ and children’s asthma management behaviors and other factors on the children’s ARQOL as a health outcome. Data were analyzed to answer the following research question: “While controlling for the child’s asthma severity, gender, race/ethnicity, school absences, and family socioeconomic status, what are the dyadic influences of parents’ and children’s asthma knowledge, asthma management, and asthma self-efficacy on the children’s asthma-related quality of life?”
Study Framework
The study is based on Bruhn’s (1983) theoretical model of asthma management, which incorporated Bandura’s (2004) constructs of human agency and reciprocal causation (parent-child influences). The model identifies background factors (asthma severity, knowledge of asthma) that influence self-management activities that in turn lead to outcome factors (quality of life).
Figure 1 depicts the exploratory study model. Consistent with Bandura’s concept of reciprocal causation, the background factors of parents’ and children’s knowledge of asthma are assumed to be correlated and partly informed by the severity of asthma. Asthma knowledge in turn supports asthma management self-efficacy or the belief that one’s actions will be effective (Bandura, 2004). Self-efficacy is a personal factor that develops over time and so associations between parents’ and children’s self-efficacy are not necessarily correlated. Self-efficacy in turn leads one to actually enact behaviors to manage asthma (Bandura, 2004). Taken together, these phenomena should influence the children’s ARQOL.
Figure 1.
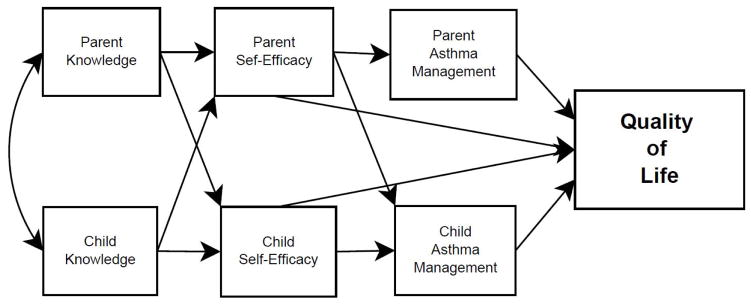
Hypothesized model
Study Procedures
After approval to conduct the study was obtained from the university’s Institutional Review Board, sample recruitment, consent and assent, and data collection began. All written documents were written in Spanish and English in a dual language format so that all families received materials with both languages. Potential families were identified through a review of children’s health records at elementary schools. Confidentiality was maintained by having the school nurse office handle the identification and mailing of invitation letters sent to all eligible families. Families could return a stamped response-postcard addressed to the school nurse or telephone the nurses’ offices to grant their permission to release their contact information to the investigators. Only those families who gave permission were contacted by the research team to explain the study, verify that sample criteria were met, and to schedule a home visit meeting to obtain consent, assent, and baseline data.
Sample Criteria
Sample inclusion criteria were a child who (a) has a diagnosis of asthma on the school health record, (b) had asthma symptoms in the previous 12 months, (c) is in grade 2–5, and (d) spoke either English or Spanish. Children were excluded if they had a significant co-morbidity that would preclude participation in classes or major pulmonary problem (e.g., cystic fibrosis, bronchopulmonary dysplasia).
Enrollment Procedure
At the first meeting, the bilingual research assistant (RA) explained the study to the parent and child in their preferred language. The RA reviewed the consent document with the parent, answered questions, and then the parent signed the consent form signifying agreement to participate in the study. After the parent consented, the RA read the assent form to the child, answered the child’s questions, and then the child signed the assent form signifying agreement to participate in the study. Copies of the consent and assent forms were given to the parent and child to keep.
Instruments
All instruments were translated into Spanish and English. The descriptive statistics for the instruments are reported in Table 1. Cronbach’s alpha were unknown for the Spanish versions before this study, but are reported here for the present study.
Table 1.
Descriptive Statistics for Instruments
| Variable | Respondent | Mean (SD) | Cronbach Alpha | |
|---|---|---|---|---|
| English | Spanish | |||
| Asthma Knowledge | Parent | 85.65 (8.67) | .76 | .70 |
| Child | 74.39 (14.11) | .63 | .59 | |
| Asthma Self-Efficacy | Parent | 3.91 (.70) | .89 | .79 |
| Child | 3.53 (.75) | .79 | .93 | |
| Asthma Management | Parent | 3.47 (.77) | .88 | .88 |
| Child | 3.76 (.59) | .76 | .74 | |
| Quality of Life (QOL) Total | Child | 2.19 (.83) | .92 | .91 |
| QOL Activity Limitations | Child | 2.27 (.98) | .72 | .58 |
| QOL Emotional Functioning | Child | 1.99 (.93) | .83 | .83 |
| QOL Asthma Symptoms | Child | 2.32 (.92) | .85 | .89 |
| Child Asthma Severity | Parent | 4.17 (1.49) | n/a | n/a |
Demographics and history
Demographic data including parent’s age, education level, occupation, and marital status, and child’s age, gender, and race/ethnicity were obtained. Family socioeconomic status (SES) was calculated based on the parent’s education level and occupation using the Hollingshead (1975) Four Factor Index (HFFI) calculation, which yields a continuous variable (possible range of 8 – 66; α = .69). The HFFI manual has both a description of the nine occupational categories (e.g. semiskilled, clerical, professional) and exemplar occupations (e.g. police officer, teacher, nurse). The occupations were reviewed by the research team for every participant and assigned an occupation code based on the HFFI manual. Absenteeism was calculated by dividing absences by days enrolled and multiplying by 100 using data provided by the child’s school. Parents also completed an asthma history form that included age of diagnosis, medications used, and asthma triggers or factors that provoke asthma symptoms.
Asthma severity
The 3-item Severity of Chronic Asthma (SCA) scale was used to measure asthma severity. Parents were asked to indicate the frequency of daily symptoms, activity limitations, and nights disrupted by asthma symptoms. The 4-point ordinal scale ranges from 1 for “0–2 times per week,” to 4 for “constant” and corresponds to national asthma guidelines (National Heart, Lung, and Blood Institute, 2007). Horner, Kieckhefer, and Fouladi (2006) found statistically significant associations between the SCA scores and children’s asthma morbidity in terms of ED visits (r = .39), hospitalizations (r = .38), and school absenteeism (r = .32). The SCA has strong item-to-total scale correlations (r =.64 to .81).
Asthma knowledge
Parcel, Nader, and Tiernan (1980) developed the Questions about Asthma (QA) instrument to assess knowledge of asthma symptoms and asthma management behaviors of parents and children. The parent version of the QA has 30 true-false items and the child version of the QA has 20 true-false items. The QA for parents demonstrated strong reliability (K-R = .88) in Parcel et al.’s study with White, Mexican American, and Black families; and in the present study (α =.76). The QA for children demonstrated adequate reliability (K-R = .56) in Parcel et al.’s study; and similar reliability is found in the present study (α = .63).
Asthma management self-efficacy
Bursch, Schwankovsky, Gilbert, and Zeiger (1999) created parallel instruments to measure parents’ and children’s self-efficacy for managing asthma. Parents complete the 13-item Parent Asthma Self-Efficacy scale that has a 5-point response scale indicating “how sure” the parent is that the behavior can be enacted, ranging from 1, “not at all sure,” to 5, “completely sure.” Children complete the 14-item Child Asthma Self-Efficacy scale that uses the same 5-point response scale. The summed mean scale score was obtained for each participant. The scales have previously been tested in a sample with Hispanic, African American, White, and Asian families. Bursch et al. found acceptable internal consistency for the parents’ scale (α =.87) and for the children’s scale (α = .87). In the present study the Cronbach’s alphas for the parent and child scales were acceptable (α = .89, .79, respectively).
Asthma self-management
Both parents and children engage in asthma management. Parents completed the 16-item Management Behavior Survey that had good internal consistency (α = .92) in the original study (Mesters, Meertens, Crebolder, & Parcel, 1993) and α = .88 in the current study. Parents rate how often they perform a behavior on a 5-point scale with 0 for “never” to 4 for “always.” The summed mean scale score was obtained for each participant. Children completed the 13-item Asthma Inventory for Children (AIC) scale (Kieckhefer, 1987). Children rate how often they perform the behaviors on a 5-point scale ranging from 0 for “never” to 4 for “always.” The summed mean scale score was obtained for each participant. Internal consistency of the tool was adequate in a predominately White (89%) sample of school age children (α = .71: Kieckhefer, 1987), and was α = .76 in the current study.
Asthma-related quality of life
The child’s ARQOL was measured with the 23-item Pediatric Asthma Quality of Life scale that is composed of three subscales (Juniper et al., 1996). Children rate “how bothered” they were on a 5-point scale that ranged from 1 for “none or never” to 5 for “always.” In the current study, good internal consistency was found for the total scale (α = .92), the 10-item symptom subscale (α = .85), the 8-item emotional function subscale (α = .83), and the 5-item activity limitations subscale (α = .72). Higher scores indicate greater bother with asthma or activity limitations.
Data Collection Procedures
Data were collected at four time points in the 12-month study. Baseline data were collected at study enrollment, post-intervention data were collected at 1-, 4- and 7-months after the intervention. The data were collected over the course of one school year (e.g. October, February, May, August) from the primary family caregiver who managed the child’s asthma and from the child with asthma. The child completed self-report questionnaires with the assistance of a graduate research assistant who read scale directions and items aloud. The child then marked responses in the booklet.
Data Analysis
According to Kenny, Kashy, and Cook (2006), analysis of dyadic data may involve the analysis of dyads that are either distinguishable (e.g. wife and husband, parent and child) or indistinguishable (e.g. coworkers, roommates). This type of analysis is important when considering the shared experiences of the respondents that when considered jointly may have significant effects on the outcome variable of interest. Structural equation modeling was used to answer the research question because it allows for exploration of relationships and inter-relationships between variables and is an especially useful approach to analyzing dyadic data (Kenny et al., 2006; Marcellus, 2006). SEM was used to explore the effects of asthma knowledge, self-efficacy to manage asthma, and asthma management on the child’s QOL
Prior to performing an SEM analysis, correlation procedures are run to assess the relationships among the variables to identify which variables to retain in the subsequent SEM analysis (Byrne, 2011). Bivariate correlation analysis found that parent asthma knowledge was significantly related to parent self-efficacy (r =.20, p <.05) and parent self-efficacy in turn was significantly related to parent asthma management (r =.53, p <.001). Child knowledge was significantly related to child self-efficacy (r =.33, p <.001), and child self-efficacy was significantly correlated with child asthma management (r =.47, p <.001). Asthma management was not significantly related to ARQOL for children (r =−.05, p >.05) or their parents (r =−.13, p >.05), whereas, child self-efficacy was found to be significantly related to ARQOL (r =−.23, p <.001).
For this study, five basic steps were taken to assess the proposed dyadic structural equation model (Byrne, 2011; Kline, 2005). The five steps include specification, identification, estimation, testing, and modification. First, the model was “specified” based on existing and hypothesized relationships regarding asthma knowledge, self-efficacy, asthma management and child quality of life. As shown in Figure 1, parent and child asthma knowledge were believed to be correlated and were specified as such in the model. Parent and child asthma knowledge were hypothesized to have direct impacts on feelings of self-efficacy, which in turn, was hypothesized to be directly related to asthma management and child quality of life. Both parent asthma management and child asthma management were hypothesized to have a direct effect on child quality of life. All control variables (e.g. asthma severity, absenteeism, triggers, SES, and race/ethnicity) as well as parent and child knowledge were based on data obtained in the fall of the school year. Parent and child self-efficacy along with parent and child asthma management scores were derived from data collected at the end of the school year in May. Child quality of life was collected at the study end in August.
The next key step is to ensure that the proposed model is mathematically identified. It is ideal to have a model that is “over identified;” that is a model in which the number of equations is greater than the unknown parameter estimates (Kline, 2005). Using the formula p(p+1)/2, where p is the number of variables in the model, we find that the possible number of equations equals 28. The number of parameters to be estimated is 16 (8 paths, 1 covariance, and 7 variances), which is less than the 28 possible known equations. Thus, the proposed model is shown to be over identified.
In the third step, estimation was done using full information maximum likelihood methods. One advantage of SEM is that models can be “estimated” even when data are missing randomly (Byrne, 2011). Exogenous variables or those factors that are outside the hypothesized model (e.g. race/ethnicity, SES, asthma severity, absenteeism) and intervention status (i.e., intervention versus control group) were correlated with the error terms and allowed us to account for non-independence of the data.
In step four, the full model as presented in Figure 1 was tested and the results are discussed below. In the fifth and final step, the model was verified through modification procedures. In this step different paths are removed and the model reanalyzed to see if this “modified” model is a better fit. None of the suggested modifications were theoretically appropriate. Results of the overall model fit and statistical significance of each path in the model are provided below (see Figure 2).
Figure 2.
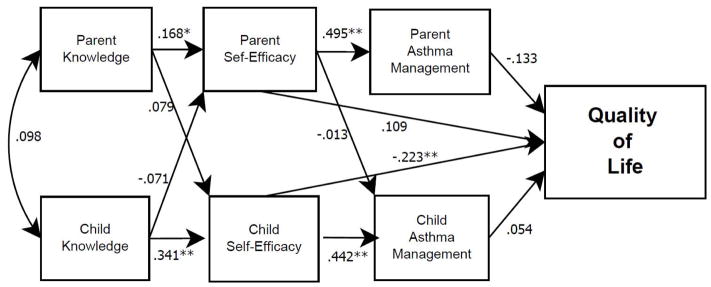
Final model
Results
A total of 183 parent-child dyads were enrolled in the study. The sample was composed of 46% Mexican American, 31% White, and 22% African American children, with 108 (59%) boys and 75 (41%) girls, who were an average of 8.78 years old (sd = 1.24; range 7–12 years). The primary caregivers were mothers (98%), who were married (60.7%), had high school or better education (84.4%), and were an average of 36.57 years old (sd = 9.37; range 25–58 years). Because the sample was composed of three racial or ethnic groups, this factor was controlled for in the analyses.
Figure 2 depicts the model including the parameter estimates. Among the exogenous control variables, intervention status, absenteeism, and asthma severity had no significant effect on the other exogenous or endogenous variables in the model. The overall model fit was reasonable with Χ2 = 18.76, df = 9, p = .027. The CFI was .98 and the RMSEA was .07.
In terms of other exogenous variables, race/ethnicity had a significant negative effect on parent knowledge β = −.18, t = −2.389, p = .02, and on child knowledge β = −.15, t = −1.964, p = .05, suggesting a disparity in the level of asthma knowledge by race for both parents and children. Post-hoc ANOVA was run comparing asthma knowledge by race/ethnic group and found that Hispanic parents (F = 6.02, p = .003) and their children (F = 3.09, p = .05) had significantly lower asthma knowledge in comparison to non-Hispanic White parents and children. Socioeconomic status was also significantly related to asthma knowledge for both the parent β = .35, t = 5.391, p <.001 and the child β =.24, t =3.396, p = .001, indicating that higher levels of SES were positively related to asthma knowledge. Asthma triggers (factors that provoke asthma) were significantly associated with parent asthma knowledge β =.215, t = 3.011, p = .003 and child ARQOL β = .287, t = 3.736, p < .001.
The hypothesized effects of knowledge on self-efficacy and self-efficacy on asthma management were supported in this model. The paths leading from knowledge to self-efficacy for parents β =.168, t = 2.492, p = .013 and children β = .341, t = 4.282, p < .001 were both significant and in the expected direction. The paths leading from self-efficacy to asthma management were also significant and in the expected direction for both parents β =.495, t = 9.630, p < .001 and children β = .442, t = 8.113, p < .001.
The hypothesized effects of parent and child asthma management and parent asthma self-efficacy on the child’s quality of life were not supported in this model. However, findings suggest that child self-efficacy was significantly related to the child’s ARQOL β = −.223, t = −2.947, p = .003. The association between parents’ and children’s asthma knowledge was in the predicted direction, but was not statistically significant.
Discussion
The direct relationships proposed in the model (see Figure 1) between asthma knowledge, asthma self-efficacy, and asthma management for parents and children were supported in the analyses. However, the absence of dyadic associations between children’s and parents’ asthma management data would seem to indicate that the dyads are not co-managing but rather are working independently to achieve asthma control.
As the analysis showed, asthma knowledge had a significant positive influence on self-efficacy for both children and their parents. But the correlation between the parent’s and child’s knowledge scores was weak, indicating a weak source of influence between the dyads on knowledge (Knafl et al., 2009). The knowledge scale required parents and children to interpret asthma situations rather than simply recall facts (Parcel et al., 1980). As such, this finding is more consistent with Wittich et al. (2006) and Yawn et al. (2006) who found incongruence or disagreements in parents’ and children’s data that measured more subjective factors.
In addition, the analysis showed that Hispanic families had significantly lower levels of asthma knowledge than the African American or white families. Family SES was also found to be a significant factor influencing asthma knowledge with high SES associated with better asthma knowledge scores. If parents have less knowledge, they may be less effective in guiding their children’s efforts to self-manage (Clark & Callam, 2012). These findings highlight an area where specific support could be provided to families in the form of targeted education that addresses their knowledge gaps (AAAI, 2004), individualized to fit their personal situations related to economic resources and should be provided in their preferred language (Horner & Brown, 2014). In addition, parents can be supported to develop their “teaching skills” so that as their knowledge of asthma improves, it can be better communicated to their child as a means of fostering the child’s knowledge and self-confidence to manage asthma (Watson et al., 2007).
Self-efficacy had a significant and positive influence on asthma management. Self-efficacy is the belief in one’s ability to manage anticipated situations (Bandura, 2004). In this study, self-efficacy was a crucial factor influencing asthma management. This finding points to the need to build self-efficacy through social learning strategies including verbal persuasion wherein information is provided that is meaningful to the person, gaining skills needed to manage asthma, and modeling of asthma management behaviors (Bandura, 2004). Ideally, these learning strategies should be enacted within the context of the family so that self-efficacy is developed and supported over time. Further, these strategies which are interactional in nature (e.g. persuasion, modeling, skills practice) should help to established shared asthma management strategies within the family.
The significant negative influence of children’s self-efficacy on their ARQOL indicates a beneficial outcome. As the children’s self-efficacy increased over the course of the study, their ratings of how bothered they are by their asthma decreased significantly. It is curious that asthma management did not significantly contribute to children’s ARQOL. In fact, the findings would suggest that both asthma management and ARQOL are distinct outcomes. Because asthma management is often triggered by the presence of asthma symptoms, the lack of associations found between parents’ and children’s asthma management data may be partially due to the differences in awareness of asthma symptom occurrence. If, as was found in Wittich et al. (2006) and Yawn et al. (2006) that children reporting more frequent symptoms than their parents report, it is possible that the parents are not aware of all the times that children are having asthma symptoms and therefore do not enact asthma management strategies. The findings support the need for parents to take a more direct role in talking with their children about how to monitor and manage asthma symptoms.
Unlike the cross-sectional studies (see Burks et al., 2013; Joseph et al., 2006; Wittich et al., 2006; Yawn et al., 2006) reviewed earlier that looked for degree of agreement on relatively objective measures (e.g. diagnosis, medicines, absences, smoking) and some subjective measures (e.g. symptoms), this longitudinal repeated-measures study focused on changes in the complex subjective variables of asthma knowledge, self-efficacy, self-management, and ARQOL over time. Further, in this study each member of the dyad was asked to report on their own information and were not asked to rate the other person. It is possible that greater congruence would have been found if both members of the dyad were reporting on the same person’s behaviors (e.g. both parent and child reporting on the child’s asthma management behaviors), such as was done in the studies by Yawn et al. (2006) and Burks et al. (2013).
Because the study was conducted in one region of the country, the findings are limited to this sample and may not be reflective of other populations. Given the voluntary nature of study participation, it is possible that those families who agreed to participate were different in some characteristic from those families who declined to participate. However, randomization of participants into intervention and control groups should help control for other factors that are not part of the study design (Field, 2013). Further, other factors that were not accounted for in the model may also be influencing the outcomes (Field, 2013).
The findings do support the need to continue clinicians’ and researchers’ efforts to improve parents’ and children’s knowledge of asthma and asthma self-efficacy to thereby improve their asthma management. However, to help foster the co-management of asthma, future research should also address ways to improve parent-child communication to increase their congruence in assessing asthma symptoms and activity limitations. Future research is also needed to identify factors that would indicate ‘when’ a child is ready to take on more responsibility for asthma self-management.
Implications of the findings include the need for nurses and other health care professionals to work with both parents and their children to help them begin working together to manage asthma rather than working in tandem. It is important to clarify parents’ and children’s understandings of asthma management and to discuss the issue of “assigning” responsibility for asthma management activities. As part of learning how to co-manage asthma, parents may need to be taught strategies to facilitate their children’s efforts to become more adept at asthma self-management.
Conclusion
Findings from this SEM analysis demonstrated that asthma knowledge is a necessary component in this process, but it is not sufficient by itself to impact outcomes. Families with greater asthma knowledge had more positive self-efficacy scores and self-efficacy in turn was associated with better asthma management scores. Interventions designed to increase asthma knowledge may lead to greater self-efficacy in families dealing with asthma. Evidence of the dyadic influences between parents’ and children’s work to manage asthma and improve ARQOL was not found in this study.
Acknowledgments
Support for this study was provided to the first author as a grant R01 NR007770 from the National Institutes of Health/National Institute of Nursing Research.
This work is supported with grant funding from the National Institutes of Health, National Institute of Nursing Research and National Heart, Lung, & Blood Institute to the first author (R01 NR007770).
Footnotes
The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Declaration of Interest
The authors declare that support for this research was provided to the first author from the National Institutes of Health (R01 NR007770).
References
- American Academy of Allergy, Asthma & Immunology. Pediatric asthma: Promoting best practice, guide for managing asthma in children. Milwaukee, WI: author; 2004. [Google Scholar]
- Anderson BJ, Holmbeck G, Iannotti RJ, McKay SV, Lochrie A, Volkening LK, Laffel L. Dyadic measures of the parent-child relationship during the transition to adolescence and glycemic control in children with type 1 diabetes. Family System Health. 2009;27:141–152. doi: 10.1037/a0015759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson S, Johnson LN. A dyadic analysis of the between- and within-system alliances on distress. Family Process. 2010;49:220–235. doi: 10.1111/j.1545-5300.2010.01319.x. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bruhn JG. The application of theory in childhood asthma self-help programs. Journal of Allergy & Clinical Immunology. 1983;72:561–577. doi: 10.1016/0091-6749(83)90483-9. [DOI] [PubMed] [Google Scholar]
- Burks ML, Brooks EG, Hill VL, Peters JI, Wood PR. Assessing proxy reports: Agreement between children with asthma and their caregivers on quality of life. Annals of Allergy, Asthma, and Immunology. 111:14–19. doi: 10.1016/j.anai.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bursch B, Schwankovsky L, Gilbert J, Zeiger R. Construction and validation of four childhood asthma self-management scales: Parent barriers, child and parent self-efficacy, and parent belief in treatment efficacy. Journal of Asthma. 1999;36:115–128. doi: 10.3109/02770909909065155. [DOI] [PubMed] [Google Scholar]
- Byrne B. Structural equation modeling with Mplus: Basic concepts, applications, and programming. New York: Guilford Press; 2011. [Google Scholar]
- Clarke SA, Calam R. The effectiveness of psychosocial interventions designed to improve health-related quality of life (HRQOL) amongst asthmatic children and their families: a systematic review. Qualitative Life Research. 2012;21:747–764. doi: 10.1007/s11136-011-9996-2. [DOI] [PubMed] [Google Scholar]
- Dixon SD, Stein MT. Encounters with children: pediatric behavior and development. 3. St. Louis: Mosby; 2000. [Google Scholar]
- Everhart RS, Fiese BH. Asthma severity and child quality of life in pediatric asthma: a systematic review. Patient Education and Counseling. 2009;75:162–168. doi: 10.1016/j.pec.2008.10.001. [DOI] [PubMed] [Google Scholar]
- Field A. Discovering statistics using IBM SPSS statistics. 4. Los Angeles: Sage; 2013. [Google Scholar]
- Gandhi PK, Kenzik KM, Thompson LA, DeWalt DA, Revicki DA, Shenkman EA, Huang IC. Exploring factors influencing asthma control and asthma-specific health-related quality of life among children. Respiratory Research. 2013;14:26. doi: 10.1186/1465-9921-14-26. Accessed at: http://respiratory-research.com/content/14/1/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gannoni AF, Shute RH. Parental and child perspectives on adaptation to childhood chronic illness: a qualitative study. Clinical Child Psychology and Psychiatry. 2010;15:39–53. doi: 10.1177/1359104509338432. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. New Haven, CT: Yale; 1975. [Google Scholar]
- Horner SD. Asthma self-care: Just another piece of school work. Pediatric Nursing. 1999;25:597, 600–604. [PubMed] [Google Scholar]
- Horner SD, Brown A. Evaluating the effect of an asthma self-management intervention for rural families. Journal of Asthma. 2014;51:168–177. doi: 10.3109/02770903.2013.855785. [DOI] [PubMed] [Google Scholar]
- Horner SD, Brown SA, Walker VG. Is rural school-aged children’s quality of life affected by their responses to asthma? Journal of Pediatric Nursing. 2012;27:491–499. doi: 10.1016/j.pedn.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner SD, Kieckhefer GM, Fouladi RT. Measuring Asthma Severity: Instrument Refinement. Journal of Asthma. 2006;43:533–538. doi: 10.1080/02770900600857192. [DOI] [PubMed] [Google Scholar]
- Joseph CLM, Havstad S, Johnson CC, Vinuya R, Ownby DR. Agreement between teenager and caregiver responses to questions about teenager’s asthma. Journal of Asthma. 2006;43:119–124. doi: 10.1080/02770900500498246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in children with asthma. Quality of Life Research. 1996;5:35–46. doi: 10.1007/BF00435967. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York: Guilford Press; 2006. [Google Scholar]
- Kieckhefer GM. Testing self-perception of health theory to predict health promotion and illness management behavior in children with asthma. Journal of Pediatric Nursing. 1987;2:381–391. [PubMed] [Google Scholar]
- Kline RB. Principles and practices of structural equation modeling. New York: Guildford Press; 2005. [Google Scholar]
- Knafl GJ, Dixon JK, O’Malley JP, Grey M, Deatrick JA, Gallo AM, Knafl KA. Analysis of cross-sectional univariate measurements for family dyads using linear mixed modeling. Journal of Family Nursing. 2009;15:130–151. doi: 10.1177/1074840709331641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcellus L. Looking at families in nursing research: Strategies for study design. Issues in Comprehensive Pediatric Nursing. 2006;29:225–245. doi: 10.1080/01460860601115130. [DOI] [PubMed] [Google Scholar]
- Mesters I, Meertens R, Crebolder H, Parcel G. Development of a health education program for parents of preschool children with asthma. Health Education Research. 1993;8:53–68. doi: 10.1093/her/8.1.53. [DOI] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute. National Asthma Education and Prevention Program. Expert panel report 3: Guidelines for the diagnosis and management of asthma. 2007 NIH Publication No. 07-4051. [PubMed] [Google Scholar]
- Orihara K, Dil N, Anaparti V, Moqbel R. What’s new in asthma pathophysiology and immunopathology? Expert Review of Respiratory Medicine. 2010;4:605–629. doi: 10.1586/ers.10.57. [DOI] [PubMed] [Google Scholar]
- Parcel GS, Nader PR, Tiernan K. A health education program for children with asthma. Developmental and Behavioral Pediatrics. 1980;1:128–132. [PubMed] [Google Scholar]
- Parke RD. Development in the family. Annual Review of Psychology. 2004;55:365–399. doi: 10.1146/annurev.psych.55.090902.141528. [DOI] [PubMed] [Google Scholar]
- Pruchno R, Wilson-Genderson M, Cartwright FP. Depressive symptoms and marital satisfaction in the context of chronic disease: A longitudinal dyadic analysis. Journal of Family Psychology. 2009;23:573–584. doi: 10.1037/a0015878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taggart VS, Wittich AR, Yawn B. Comparison of parent and student responses to asthma surveys: 2 different experiences with similar results. Journal of School Health. 2006;76:235–236. doi: 10.1111/j.1746-1561.2006.00103.x. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Summary health statistics for U.S. children: National Health Interview Survey, 2010. Vital and Health Statistics, Series. 2011;10:250. DHHS Pub. No. (PHS)-2012-1578. [PubMed] [Google Scholar]
- Van Bragt S, van den Bernt L, Thoonen B, van Weel C, Merkus P, Schermer T. PELICAN: a quality of life instrument for childhood asthma. BioMed Central Pediatrics. 2012;12:137. doi: 10.1186/1471-2431-12-137. Accessed at: http://www.biomedcentral.com/1471-2431/12/137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker J, Winkelstein M, Land C, Lewis-Boyer L, Quartey R, Pham L, Butz A. Factors that influence quality of life in rural children with asthma and their parents. Journal of Pediatric Health Care. 2008;22:343–350. doi: 10.1016/j.pedhc.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson WTA, Gillespie C, Thomas N, Filuk SE, McColm J, Piwniuk MP, Becker AB. Small-group, interactive education and the effect on asthma control by children and their families. Canadian Medical Association. 2007;181:257–263. doi: 10.1503/cmaj.080947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittich AR, Li Y, Gerald LB. Comparison of parent and student response to asthma surveys: Students grades 1-4 and their parents from an urban public school setting. Journal of School Helath. 2006;76:236–240. doi: 10.1111/j.1746-1561.2006.0104_1.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yawn BP, Wollan P, Kurland M, Bertram S. Comparison of parent and student responses to asthma surveys: Students grades 3–12 and their parents from a suburban private school setting. Journal of School Health. 2006;76:241–245. doi: 10.1111/j.1746-1561.2006.0104_2.x. [DOI] [PubMed] [Google Scholar]


