Abstract
Purpose
To investigate whether the gender gap in obesity prevalence is greater among US Blacks than Whites in a study designed to account for racial differences in socioeconomic and environmental conditions.
Methods
We estimated age-adjusted, race-stratified gender gaps in obesity (female obesity minus male obesity, defined as BMI ≥ 30 kg/m2) in the National Health Interview Survey 2003 (NHIS) and the Exploring Health Disparities in Integrated Communities-Southwest Baltimore 2003 study (EHDIC-SWB). EHDIC-SWB is a population-based survey of 1381 adults living in two urban, low-income, racially integrated census tracts with no race difference in income.
Results
In NHIS, the obesity gender gap was larger in Blacks than Whites: 7.7 percentage-points (ppts) (95% confidence interval (CI): 3.4, 11.9) in Blacks versus −1.5 ppts (95% CI: −2.8, −0.2) in Whites. In EHDIC-SWB, the gender gap was similarly large for Blacks and Whites: 15.3 ppts (95% CI: 8.6, 22.0) in Blacks versus 14.0 ppts (95% CI: 7.1, 20.9) in Whites.
Conclusions
In a racially integrated, low-income urban community, gender gaps in obesity prevalence were similar for Blacks and Whites.
Keywords: gender, obesity, race, socioeconomic status, health disparities
Introduction
In the United States, Black women are much more likely to be obese than the general population [1]. For example, in the 2009–2010 National Health and Nutrition Examination Survey, obesity prevalence was 26 percentage points (ppts) higher in Black women than in White women (58.5% Black vs. 32.2% White obese) [1]. Although a large literature has explored this racial disparity in obesity among women [2–4], much less research has investigated why Black women also have 20 percentage-point higher obesity prevalence than Black men (58.5% female vs. 38.8% male obese) [1]. This gender disparity, or “gender gap,” is negligible in Whites (32.2% female vs. 36.2% male obese) [1].
There are two broad theories that attempt to explain the pronounced gender gap in obesity among Blacks. One theory suggests that Black women are a unique group with higher susceptibility to obesity than almost all other groups, including White women, White men, and Black men [5]. Suggested mechanisms underlying this “cultural and genetic theory” include unique dietary preferences, early childbearing, and selection of the thrifty genotype [5]. Alternatively, the “contextual theory” posits that among any demographic group, low socioeconomic status (SES) and poor residential environments exacerbate obesity in females but not males through psychosocial and biological processes [6]. While this phenomenon of high female obesity has been found in other developing economies [7], it may manifest more prominently in US Blacks than Whites because Blacks are more likely to belong to lower SES groups and live in environments that have harmful exposures [6, 8–10] because of the enduring effect of segregation [11, 12].
Differences in social and environmental exposures experienced by Blacks and Whites present methodological challenges to investigating these two broad theories, which requires defining a population of Blacks and Whites who have similar distributions of independent risk factors for obesity [8]. That is, conditional on measured covariates, the distribution of potential obesity outcomes does not depend on being Black or White because all predictors of obesity, including social and environmental exposures, are similarly distributed in Blacks and Whites [13]. However, this condition of similarity is likely invalid because pervasive residential segregation, mass incarceration, and pronounced Black-White differences in lifetime socioeconomic position and trajectories have led to divergent social and environmental exposures for Blacks and Whites [8, 11]. In particular, capturing the cumulative effects of lifetime exposure to poor environments using covariate-adjustment for adult SES or neighborhood-level variables is problematic [14], especially when Blacks are unlikely to experience similar neighborhood and socioeconomic conditions as Whites across the lifecourse [15].
This study investigates the extent to which racial differences in social and environmental conditions account for Black-White differences in the obesity gender gap. To overcome the methodological issues that result from social stratification by race [11, 12], we controlled for racial differences in SES using a unique study population: an urban, racially integrated community of Blacks and Whites with no race difference in income. We hypothesized that, in a low-income, racially integrated community where Blacks and Whites have similar income distributions, the obesity gender gap would be similarly large for Blacks and Whites. We compared these findings to a national sample that does not account for differing social and environmental conditions experienced by Blacks and Whites.
Methods
Study Population
The Exploring Health Disparities in Integrated Communities study (EHDIC) is an ongoing multi-site study of race disparities within communities where Blacks and Whites live together and where there are no race differences in SES, as measured by median income. In the 2000 Census, less than 1% of all census tracts met the study criteria for racial integration, balance, and equality in SES [12]. This analysis is based on data from the first EHDIC study site in Southwest Baltimore, Maryland (EHDIC-SWB), a low-income urban area.
EHDIC-SWB is a cross-sectional face-to-face survey of the adult population (age ≥18 years) in two contiguous census tracts collected between June and September 2003. The median income for the study area was $24,002, and the distribution of household income did not differ by race. In addition to being economically homogenous, the study area was also racially balanced and integrated, with almost equal proportion of black (51%) and white (44%) residents living in a study area of 3 square miles. The census tracts were block-listed to identify all occupied residential housing units in the study area, and up to five attempts were made to contact an eligible adult at each residence. Of the 1,244 occupied housing units, 65.8% were enrolled in the study, resulting in 1,489 participants (41.9% of 3,555 adults recorded in the 2000 Census). Comparisons to the 2000 Census for the study area indicated that the EHDIC-SWB sample included a higher proportion of Blacks and women, but was otherwise similar on other demographic and socioeconomic indicators, including the lack of race difference in median income [12]. Of the seven census block groups represented in the study, four had a black/white ratio of residents close to 1, while six had a black/white ratio < 2, suggesting that black and white residents in this community tended to live near one another [16]. Because the survey had similar coverage across each census block group including the study area, the bias to geographic locale and its relationship with SES should be minimal [12].
The survey was administered in person by a trained interviewer and consisted of a structured questionnaire modeled after the 2003 National Health Interview Survey (NHIS). NHIS a cross-sectional, multistage stratified health survey of non-institutionalized, civilian US households that is administered annually by the National Center for Health Statistics [17]. Participants consented to an in-person interview on health status, health behaviors, and demographics. The same questions from the NHIS were asked to the EHDIC-SWB participants to facilitate comparison across studies. The EHDIC study has been described in greater detail elsewhere [12]. The Committee on Human Research at the Johns Hopkins Bloomberg School of Public Health approved EHDIC-SWB. The Research Ethics Review Board at the National Center for Health Statistics approved NHIS.
To contextualize results from EHDIC-SWB, we analyzed data on non-Hispanic Black and non-Hispanic White adults in the Sample Adult Core section of NHIS (N=29,630). Pregnant women and participants missing data on weight, height, race, or age were excluded from these analyses (missing values for each covariate ≤ 5%), resulting in final sample sizes of 1,381 participants in EHDIC-SWB and 27,867 participants in NHIS.
Key variables
The outcome, obesity, was defined as body mass index (BMI, weight (kg)/height (m)2) ≥30 kg/m2 and calculated based on self-reported height and weight. The exposure, gender, was self-reported in EHDIC-SWB and NHIS. Self-reported race was categorized as White or Black in EHDIC-SWB and NHIS. Self-reported age was categorized as 18–19 years, 5-year intervals from 20 to 84 years, and ≥85 years. Other self-reported variables, including marital status (married/living as married, widowed, divorced/separated, never married), attained education (less than high school (HS) graduate, HS graduate or equivalent, more than HS), and household income (<$20,000, ≥$20,000), provided information on social conditions but, as described below, were not included as covariates in the analyses.
Conceptual Model for Analyses
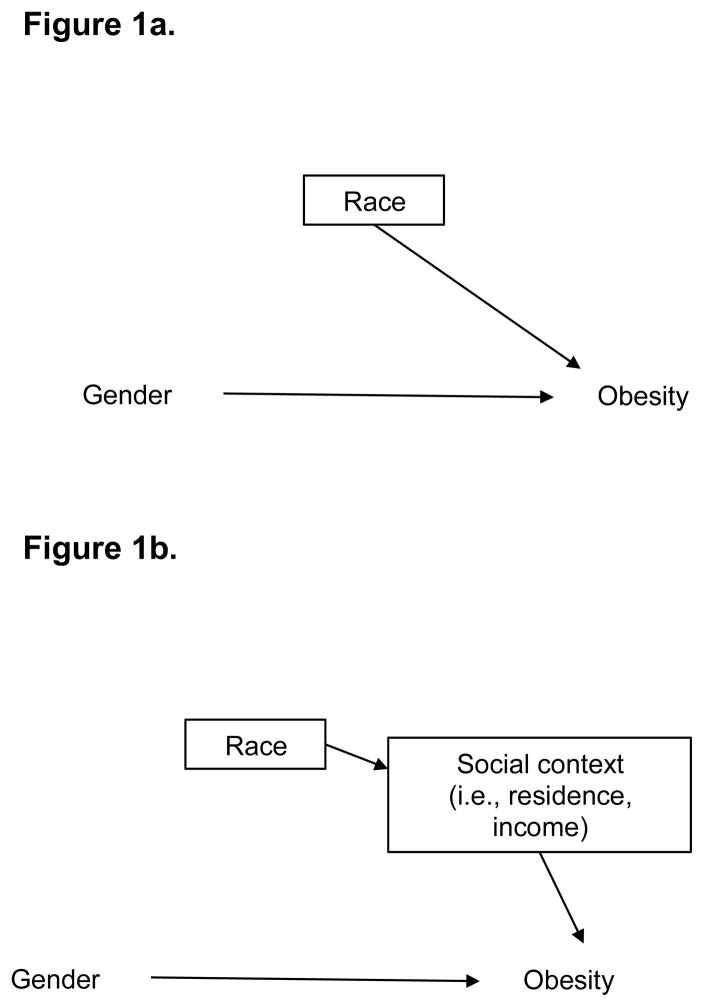
We used directed acyclic graphs (DAGs) to guide our analyses by encoding relationships between gender, race, and obesity. First, we conceptualized the strong gender-obesity relationship observed in Blacks but not in Whites as effect-measure modification, whereby Black-White race modifies the relationship between the exposure, “Gender,” and the outcome, “Obesity”. Although we used causal diagrams, we did not estimate, nor sought to ascribe meaning to, the causal effect of Black-White race or Female-Male gender on obesity because their multifactorial and context-specific nature makes them ill-suited to be considered causes [13, 18]. Instead we sought to describe associations between gender and obesity within categories of race.
Next, using DAGs we visually distinguished the theories attempting to explain the racial disparity in the obesity gender gap. The cultural and genetic theory positing inherently higher obesity susceptibility for Black women is represented as Figure 1A. The box around “Race,” the modifier, indicates stratification by this covariate [19]. Here, race directly modifies the gender-obesity relationship because race has been hypothesized to directly influence obesity risk [19]. Conversely, the contextual theory—that racial differences in SES and residential exposures are the reasons behind the larger gender gap in Blacks than that in Whites—is depicted as race indirectly modifying the gender-obesity relationship through social context (i.e., residence and income) (Figure 1B). We draw social context variables downstream of race because residential segregation and social stratification create disparate social, environmental, and material exposures for Blacks and Whites in the US [20–22]. Controlling for these differences through restriction, stratification, or regression is illustrated by drawing a box around social context (Figure 1B). By restricting our analysis to a racially integrated community with no race difference in income, we control for racial differences in residential exposures and SES without encountering the non-positivity issues that arise when using regression methods to investigate racial disparities in nationally representative samples [8, 23].
Figure 1.
Causal diagrams encoding effect measure modification of gender-obesity relationship by race.
Figure 1a: Effect measure modification of relationship between gender and obesity by race.
Figure 1b: Effect measure modification of relationship between gender and obesity by race through social context.
Statistical Analyses
In both the EHDIC-SWB and NHIS samples, we estimated the obesity gender gap (female obesity minus male obesity) in Blacks and Whites and corresponding 95% confidence intervals (CIs) using the analytically derived variance estimator associated with the sample means. In each sample, we used modified Wald tests to compare the gender gaps in Blacks and Whites, and thereby tested for effect-measure modification of the obesity-gender relationship by Black-White race [24].
To identify any additional adjustment variables, we constructed a DAG (Figure 2) that encoded relationships between gender, race, obesity, age, and demographic processes such as migration, incarceration, fertility, and mortality. Sociodemographic characteristics of study participants may appear related in data because of selection effects into studies [25]. Associations involving race are already accounted for in our analysis through stratification. To account for spurious associations due to differential age distributions, we standardized the data to the age distribution of US adults in the 2000 Census [26]. For direct age standardization, we created weights corresponding with 15 age categories. We applied these weights to the individual observations in EHDIC-SWB and estimated age-adjusted obesity prevalence stratifying by race and gender. In NHIS, we also adjusted for complex, multistage sampling using Interim Annual survey weights to account for oversampling of Black households [17]. We multiplied the 2000 Census age-distribution weights and complex survey weights and applied these composite weights to obtain age- and survey-adjusted obesity prevalence estimates. All analyses were conducted in Stata 12 (StataCorp LLP, College Station, Texas).
Figure 2.
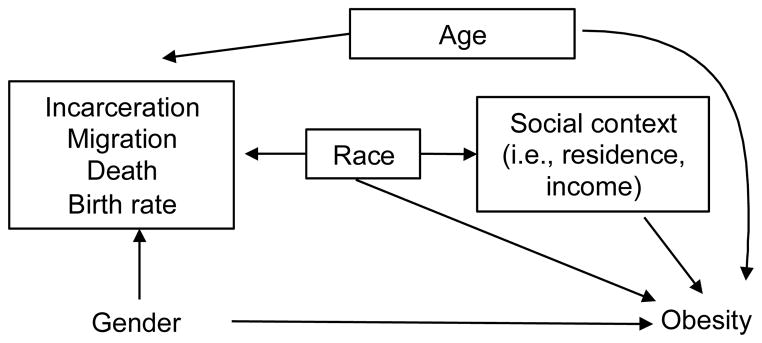
Causal diagram for covariate selection to explore racial modification of the gender-obesity relationship.
Results
In the nationally representative NHIS, Black women appeared more likely to be low-income than White women (i.e., 35% Black women low-income vs. 20% White women low-income), and Black men appeared more likely than White men to be low-income (27% Black men low-income vs. 15% White men low-income) (Table 1). Furthermore, NHIS Blacks had lower educational attainment and were less likely to be married than Whites. Overall, there appeared to be pronounced race differences in SES among NHIS adults.
Table 1.
Characteristics of NHIS 2003 and EHDIC-SWB by race and gender
| NHIS (N = 27 867)a
|
EHDIC-SWB (N = 1381)
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Black (N = 4019) | White (N = 23 848) | Black (N = 817) | White (N = 564) | |||||||||||||
|
|
|
|||||||||||||||
| Females | Males | Females | Males | Females | Males | Females | Males | |||||||||
|
|
|
|||||||||||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |
| Age (years, median) | 43 | 43 | 47 | 44 | 37 | 39 | 42 | 42 | ||||||||
| Marital status | ||||||||||||||||
| Married/living as married | 655 | 38 | 691 | 55 | 6610 | 64 | 6422 | 69 | 62 | 14 | 61 | 16 | 83 | 26 | 62 | 25 |
| Widowed | 328 | 12 | 71 | 3 | 2001 | 11 | 461 | 3 | 29 | 7 | 10 | 3 | 47 | 15 | 13 | 5 |
| Divorced/separated | 578 | 19 | 313 | 13 | 2190 | 12 | 1454 | 9 | 83 | 19 | 66 | 17 | 88 | 28 | 62 | 25 |
| Never married | 866 | 31 | 485 | 29 | 2068 | 14 | 2525 | 19 | 265 | 60 | 241 | 64 | 98 | 31 | 110 | 45 |
| Missing | 24 | 8 | 57 | 60 | 1 | |||||||||||
| Education | ||||||||||||||||
| Less than HS graduate | 558 | 22 | 349 | 22 | 2446 | 16 | 2041 | 16 | 154 | 35 | 132 | 35 | 157 | 50 | 110 | 45 |
| HS graduate/GED | 723 | 31 | 494 | 33 | 3739 | 31 | 3082 | 29 | 199 | 46 | 171 | 45 | 103 | 32 | 91 | 37 |
| More than HS | 1146 | 48 | 700 | 45 | 6630 | 54 | 5688 | 55 | 84 | 19 | 75 | 20 | 57 | 18 | 46 | 19 |
| Missing | 24 | 25 | 111 | 111 | 2 | |||||||||||
| Household Income | ||||||||||||||||
| <$20 000 | 1000 | 35 | 475 | 27 | 3467 | 20 | 2148 | 15 | 287 | 65 | 200 | 53 | 196 | 62 | 114 | 46 |
| ≥$20 000 | 1278 | 65 | 967 | 73 | 8602 | 80 | 8103 | 85 | 152 | 35 | 178 | 47 | 121 | 38 | 133 | 54 |
| Missing | 173 | 126 | 857 | 671 | ||||||||||||
EHDIC-SWB, Exploring Health Disparities in Integrated Communities Southwest Baltimore; GED, General Education Development; NHIS, National Health Interview Survey.
In NHIS, percentages adjusted for clustered sampling design and unequal probability of selection into the dataset. Numbers are absolute unadjusted numbers for each level of that particular variable.
In EHDIC-SWB, over 60% of women were low-income, but low-income status was similar across race (i.e., 65% Black women vs. 62% White women low income). This racial equality was a function of the EHDIC study design [12], but a slightly higher proportion of Black males were in low-income households compared to White males (i.e., 53% Black men vs. 46% White men low-income). Furthermore, over a third of EHDIC-SWB adults had less than high school education completed, and educational attainment was lower in EHDIC-SWB Whites than Blacks (e.g., 35% Black women vs. 50% White women with less than high school completed; 35% Black men vs. 45% White men with less than high school completed). Compared to the nationally representative adults in NHIS, EHDIC-SWB adults were particularly disadvantaged and less likely to be married, but Blacks and Whites in EHDIC-SWB had similar SES.
In NHIS, the age-adjusted mean percent obese for Black females and males was 37.8% and 30.2%, respectively, as compared with 22.2% and 23.7% for White females and males, respectively (Table 2). Among NHIS Blacks, the gender gap was 7.7 percentage points (ppts; 95% Confidence Interval (CI): 3.4, 11.9). Among Whites, the gender gap was −1.5 ppts (95% CI: −2.8, −0.2). Race modified the obesity gender gap (two-sided P < 0.001).
Table 2.
Prevalence of obesity by race and gender, NHIS 2003 and EHDIC-SWB 2003
| Females % (SE)
|
Males % (SE)
|
Gap % points (SE)
|
P-valuea
|
|
|---|---|---|---|---|
| NHIS 2003 (n = 27,867)b | ||||
| Unadjusted prevalence | ||||
| Black | 38.3 (1.4) | 28.1 (1.3) | 10.3 (2.0) | |
| White | 22.1 (0.5) | 23.1 (0.5) | −1.0 (0.6) | |
| Racial modification of gender difference | <0.001 | |||
| Age-adjusted prevalence | ||||
| Black | 37.8 (1.5) | 30.2 (1.4) | 7.7 (2.2) | |
| White | 22.2 (0.5) | 23.7 (0.5) | −1.5 (0.7) | |
| Racial modification of gender difference | <0.001 | |||
| EHDIC-SWB (n = 1,381) | ||||
| Unadjusted prevalence | ||||
| Black | 39.4 (2.3) | 23.3 (2.2) | 16.1 (3.2) | |
| White | 35.3 (2.7) | 22.7 (2.7) | 12.7 (3.8) | |
| Racial modification of gender difference | 0.48 | |||
| Age-adjusted prevalence | ||||
| Black | 38.3 (2.5) | 23.0 (2.4) | 15.3 (3.4) | |
| White | 35.1 (2.5) | 21.1 (2.4) | 14.0 (3.5) | |
| Racial modification of gender difference | 0.79 | |||
EHDIC-SWB, Exploring Health Disparities in Integrated Communities-Southwest Baltimore; NHIS National Health Interview Survey.
P-values for modified Wald tests for racial difference in the obesity gender difference.
Adjusted for clustered sampling design and unequal probability of selection into the data set.
In EHDIC-SWB, age-adjusted obesity prevalence in Black females and males was 38.3% and 23.0%, respectively; in White females and males, prevalence was 35.1% and 21.1%, respectively. Among Blacks, the gender gap was 15.3 ppts (95% CI: 8.6, 22.0); among Whites, obesity was higher in females than males by 14.0 ppts (95% CI: 7.1, 20.9). We found no evidence of effect-measure modification of the obesity gender gap by race (P = 0.79).
Discussion
In a low-income, urban, racially integrated community where the distribution of income was similar across race, there was no evidence that race modifies the gender-obesity relationship as it does in a national sample. Previous studies investigated contributions of social and environmental conditions on the racial difference in obesity among women [27] and among men only [28]; however, neither of these studies investigated differences between men and women. While we found no excess obesity in nationally representative White females compared to White males, pronounced excess was apparent in Black females compared to Black males. In contrast, we find that in a low-income, urban, racially integrated community, Black and White men had similarly low obesity prevalence, while Black and White women had similarly high obesity prevalence. These findings are not consistent with theories positing high obesity as being specific to Black females due to their genetic or inherited characteristics; rather, we find evidence in favor of the contextual theory positing that in challenging social and environmental conditions, obesity prevalence is higher in females than males irrespective of race.
Mechanisms underlying these large gender gaps in obesity remain unclear; however, previous research points to differential associations between neighborhood deprivation and obesity in women and men [3, 29]. Worse physical characteristics measured by lesser walkability and unavailability of healthy foods may have stronger, positive associations with obesity in women than in men [3, 30]. Conversely, neighborhood social quality measured by violent crime rates and social cohesion may be inversely related with obesity in men, but not associated with obesity in women [3]. In disadvantaged neighborhoods, the relatively higher obesity risk for women associated with worse physical environments and the lower obesity risk for men associated with worse social environments may result in large obesity gender gaps. Gender-specific responses to perceived neighborhood disorder, use of public spaces for physical activity [31], and other contextual influences on weight status also appear stronger for women than men [32, 33].
Another set of hypothesized mechanisms involves gender-specific psychosocial and behavioral responses to chronic stress arising from structural and material disadvantage. For example, women may cope by overeating [34], while men may use other coping strategies such as substance abuse and smoking [35]. Perceived stressors may vary in type and influence by gender; for instance, general life constraints and strained familial relationships are associated with weight gain in women but not men [36]. Moreover, social norms surrounding femininity, childrearing, and food allocation [37] may compel women to assume roles associated with weight gain. Coupled with lower female earnings, these roles may make women in low SES neighborhoods susceptible to food insecurity [38]. While food-insecure mothers are more likely to be obese than food-insecure, childless women, obesity prevalence is similar among food-insecure fathers and childless men [39].
Additionally, early-life socioeconomic disadvantage may have gender-specific, lasting biologic or behavioral effects on adult obesity risk [40, 41]. In animal models, in utero malnutrition can lead to increased postnatal weight gain and fat deposition in females, but not males, due to sex differences in hypothalamic function [42–46]. These permanent effects of early life deprivation on adult obesity are mirrored in quasi-experimental studies of men and women born during famine [6, 47]. Furthermore, nutritional deprivation during early childhood may have differential impact on male and female obesity risk [40] through regulatory systems controlling energy balance [48, 49] and gender norms surrounding eating behaviors that continue into adulthood.
Large obesity gender gaps are not confined to the United States; rather, they are observed in populations undergoing rapid economic development [50–52]. For example, in an urban South African community with high poverty, obesity prevalence was 42 ppts higher in women than men [40]. In the US, one study has explored socioeconomic explanations of racial differences in the obesity gender gap and found larger gender gaps in White and Black adolescents from low-SES families than higher-SES families; however, at all levels of childhood SES, the gender gap remained larger in Blacks than in Whites [9]. These remaining racial differences may be due to unaccountable differences in neighborhood and socioeconomic characteristics. Measuring and harmonizing SES across race is untenable because Blacks have been historically placed in positions of disadvantage. Because of methodological issues related to differential social and environmental exposures in Blacks and Whites after adjustment for area- and individual-level SES, observed Black-White differences in nationally representative data should be interpreted cautiously.
Although our unique study design addresses methodological challenges in health disparities research, restriction to the EHDIC-SWB population limits the generalizability of these results to other racial/ethnic groups and higher SES or rural communities. Although the EHDIC-SWB sample can be generalized to a national sample with similarly low SES [12], our findings may not generalize to other racially integrated, low-income, urban populations if social and environmental factors are unique to this study area. Additionally, differences in length of exposure to these potentially obesogenic environmental factors may explain the obesity gender gap; however, length of residence in this community was similar across gender and obese status (data not shown). Future research should investigate other communities where Blacks and Whites live in close proximity and have similar SES to elucidate the contributions of neighborhood and social factors on obesity risk.
In addition, self-reported variables may have measurement error [53] and lead to bias if outcome misclassification is differential with respect to race/ethnicity, gender, or SES. However, studies comparing self-reported versus measured height and weight indicate that any potential misreporting is non-differential across gender [54] and race/ethnicity [55, 56]. Although the true prevalence of obesity in both males and females may be underestimated, the size of the gender gaps is likely unaffected. Additionally, selection bias may be present given 66% of eligible residences enrolled in EHDIC-SWB, while the response rate among NHIS sample adults conditional on family response was 74%. If participation is associated with gender, race, and obesity, results could be biased. Finally, gender and race are poorly defined exposures because each could encompass many different mechanisms relevant to obesity (e.g., social expectations, biological processes, behaviors) [13, 18], which would violate the consistency assumption required for causal inference [57]. However, we do not seek to make causal conclusions about race or gender; rather, interventions most relevant for policy are on exposures conducive to intervention, such as income inequality and residential segregation [13].
To our knowledge, this is the first study to explore racial differences in the obesity gender gap using an innovative study design to address methodological issues related to differential social and environmental exposures in Blacks and Whites. Our results suggest that the preponderance of high female obesity is not specific to Blacks; rather, it may be characteristic of poorer social and environmental conditions engendered by residential segregation and social stratification. To the extent that racial inequalities in social context remain unaddressed, interventions to reduce the obesity burden in Black women may fall short of desired results.
Acknowledgments
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development [T32 HD007168 and R24 HD050924 to M.J.S.], the National Cancer Institute at the National Institutes of Health [K01CA172717 to W.R.R.], and University Cancer Research Funds from Lineberger Cancer Center at UNC-Chapel Hill to W.R.R. The Exploring Health Disparities in Integrated Communities Study was supported by the National Institutes of Health, National Center on Minority Health and Health Disparities [P60 MD000214-01], and a grant from Pfizer, Inc. We are grateful to the Carolina Population Center [R24 HD050924] for general support. A version of this paper was presented at the 2013 Society for Epidemiologic Research annual meeting in Boston, MA.
List of abbreviations
- EHDIC
Exploring Health Disparities in Integrated Communities study
- EHDIC-SWB
Exploring Health Disparities in Integrated Communities – Southwest Baltimore study
- NHIS
National Health Interview Survey
- ppts
Percentage-points
- SES
Socioeconomic status
- BMI
Body mass index
- GED
General Education Development
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009–2010. NCHS data brief. 2012 Jan;(82):1–8. Epub 2012/05/24. eng. [PubMed] [Google Scholar]
- 2.Burke GL, Savage PJ, Manolio TA, Sprafka JM, Wagenknecht LE, Sidney S, et al. Correlates of obesity in young black and white women: the CARDIA Study. American journal of public health. 1992 Dec;82(12):1621–5. doi: 10.2105/ajph.82.12.1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mujahid MS, Diez Roux AV, Shen M, Gowda D, Sanchez B, Shea S, et al. Relation between neighborhood environments and obesity in the Multi-Ethnic Study of Atherosclerosis. American journal of epidemiology. 2008 Jun 1;167(11):1349–57. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiologic reviews. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 5.Kumanyika S. Obesity in black women. Epidemiologic reviews. 1987;9:31–50. doi: 10.1093/oxfordjournals.epirev.a036307. [DOI] [PubMed] [Google Scholar]
- 6.Robinson WR. Gender-specific effects of early nutritional restriction on adult obesity risk: evidence from quasi-experimental studies. Obesity. 2012 Dec;20(12):2464–6. doi: 10.1038/oby.2012.35. [DOI] [PubMed] [Google Scholar]
- 7.Kanter R, Caballero B. Global gender disparities in obesity: a review. Advances in nutrition (Bethesda, Md) 2012 Jul;3(4):491–8. doi: 10.3945/an.112.002063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Messer LC, Oakes JM, Mason S. Effects of socioeconomic and racial residential segregation on preterm birth: a cautionary tale of structural confounding. American journal of epidemiology. 2010 Mar 15;171(6):664–73. doi: 10.1093/aje/kwp435. [DOI] [PubMed] [Google Scholar]
- 9.Robinson WR, Gordon-Larsen P, Kaufman JS, Suchindran CM, Stevens J. The female-male disparity in obesity prevalence among black American young adults: contributions of sociodemographic characteristics of the childhood family. The American journal of clinical nutrition. 2009 Apr;89(4):1204–12. doi: 10.3945/ajcn.2007.25751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wells JC, Marphatia AA, Cole TJ, McCoy D. Associations of economic and gender inequality with global obesity prevalence: understanding the female excess. Social science & medicine. 2012 Aug;75(3):482–90. doi: 10.1016/j.socscimed.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 11.LaVeist TA. Disentangling race and socioeconomic status: a key to understanding health inequalities. Journal of urban health : bulletin of the New York Academy of Medicine. 2005 Jun;82(2 Suppl 3):iii26–34. doi: 10.1093/jurban/jti061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.LaVeist T, Thorpe R, Jr, Bowen-Reid T, Jackson J, Gary T, Gaskin D, et al. Exploring health disparities in integrated communities: overview of the EHDIC study. Journal of urban health : bulletin of the New York Academy of Medicine. 2008 Jan;85(1):11–21. doi: 10.1007/s11524-007-9226-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaufman JS, Cooper RS. Commentary: considerations for use of racial/ethnic classification in etiologic research. American journal of epidemiology. 2001 Aug 15;154(4):291–8. doi: 10.1093/aje/154.4.291. [DOI] [PubMed] [Google Scholar]
- 14.Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997 Nov;8(6):621–8. [PubMed] [Google Scholar]
- 15.Westreich D, Cole SR. Invited commentary: positivity in practice. American journal of epidemiology. 2010 Mar 15;171(6):674–7. doi: 10.1093/aje/kwp436. discussion 8–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gary TL, Stark SA, LaVeist TA. Neighborhood characteristics and mental health among African Americans and whites living in a racially integrated urban community. Health & place. 2007 Jun;13(2):569–75. doi: 10.1016/j.healthplace.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 17.National Center for Health Statistics. 2003 National Health Interview Survey Description. 2004 [updated June 13, 2012; cited 2013 February 5]. Available from: http://www.cdc.gov/nchs/nhis/about_nhis.htm.
- 18.Hernan MA, VanderWeele TJ. Compound treatments and transportability of causal inference. Epidemiology. 2011 May;22(3):368–77. doi: 10.1097/EDE.0b013e3182109296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.VanderWeele TJ, Robins JM. Four types of effect modification: a classification based on directed acyclic graphs. Epidemiology. 2007 Sep;18(5):561–8. doi: 10.1097/EDE.0b013e318127181b. [DOI] [PubMed] [Google Scholar]
- 20.Acevedo-Garcia D. Residential segregation and the epidemiology of infectious diseases. Social science & medicine. 2000 Oct;51(8):1143–61. doi: 10.1016/s0277-9536(00)00016-2. [DOI] [PubMed] [Google Scholar]
- 21.LaVeist TA, Wallace JM., Jr Health risk and inequitable distribution of liquor stores in African American neighborhood. Social science & medicine. 2000 Aug;51(4):613–7. doi: 10.1016/s0277-9536(00)00004-6. [DOI] [PubMed] [Google Scholar]
- 22.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public health reports. 2001 Sep-Oct;116(5):404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sampson RJ, Sharkey P, Raudenbush SW. Durable effects of concentrated disadvantage on verbal ability among African-American children. Proceedings of the National Academy of Sciences of the United States of America. 2008 Jan 22;105(3):845–52. doi: 10.1073/pnas.0710189104. Epub 2007/12/21. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2012. [Google Scholar]
- 25.Cole SR, Platt RW, Schisterman EF, Chu H, Westreich D, Richardson D, et al. Illustrating bias due to conditioning on a collider. International journal of epidemiology. 2010 Apr;39(2):417–20. doi: 10.1093/ije/dyp334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Center for Health Statistics. Center for Disease Control and Prevention. Standard Proportions for NHANES Population Groupings Using Census 2000 Population Data [Google Scholar]
- 27.Bleich SN, Thorpe RJ, Jr, Sharif-Harris H, Fesahazion R, Laveist TA. Social context explains race disparities in obesity among women. Journal of epidemiology and community health. 2010 May;64(5):465–9. doi: 10.1136/jech.2009.096297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thorpe RJ, Jr, Kelley E, Bowie JV, Griffith DM, Bruce M, LaVeist T. Explaining Racial Disparities in Obesity Among Men: Does Place Matter? American journal of men’s health. 2014 Sep 23; doi: 10.1177/1557988314551197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stafford M, Brunner EJ, Head J, Ross NA. Deprivation and the development of obesity a multilevel, longitudinal study in England. American journal of preventive medicine. 2010 Aug;39(2):130–9. doi: 10.1016/j.amepre.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 30.Chang VW, Hillier AE, Mehta NK. Neighborhood Racial Isolation, Disorder and Obesity. Social forces; a scientific medium of social study and interpretation. 2009 Jun 1;87(4):2063–92. doi: 10.1353/sof.0.0188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roman CG, Chalfin A. Fear of walking outdoors. A multilevel ecologic analysis of crime and disorder. American journal of preventive medicine. 2008 Apr;34(4):306–12. doi: 10.1016/j.amepre.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 32.Chang VW, Christakis NA. Income inequality and weight status in US metropolitan areas. Social science & medicine. 2005 Jul;61(1):83–96. doi: 10.1016/j.socscimed.2004.11.036. [DOI] [PubMed] [Google Scholar]
- 33.Robert SA, Reither EN. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Social science & medicine. 2004 Dec;59(12):2421–34. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 34.Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. American journal of public health. 2010 May;100(5):933–9. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams DR. The health of men: structured inequalities and opportunities. American journal of public health. 2003 May;93(5):724–31. doi: 10.2105/ajph.93.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. American journal of epidemiology. 2009 Jul 15;170(2):181–92. doi: 10.1093/aje/kwp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.DeVault ML. Feeding the family : the social organization of caring as gendered work. Chicago: University of Chicago Press; 1991. [Google Scholar]
- 38.McIntyre L, Glanville NT, Raine KD, Dayle JB, Anderson B, Battaglia N. Do low-income lone mothers compromise their nutrition to feed their children? CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 2003 Mar 18;168(6):686–91. [PMC free article] [PubMed] [Google Scholar]
- 39.Martin MA, Lippert AM. Feeding her children, but risking her health: the intersection of gender, household food insecurity and obesity. Social science & medicine. 2012 Jun;74(11):1754–64. doi: 10.1016/j.socscimed.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Case A, Menendez A. Sex differences in obesity rates in poor countries: evidence from South Africa. Economics and human biology. 2009 Dec;7(3):271–82. doi: 10.1016/j.ehb.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khlat M, Jusot F, Ville I. Social origins, early hardship and obesity: a strong association in women, but not in men? Social science & medicine. 2009 May;68(9):1692–9. doi: 10.1016/j.socscimed.2009.02.024. Epub 2009/03/20. eng. [DOI] [PubMed] [Google Scholar]
- 42.Anguita RM, Sigulem DM, Sawaya AL. Intrauterine food restriction is associated with obesity in young rats. The Journal of nutrition. 1993 Aug;123(8):1421–8. doi: 10.1093/jn/123.8.1421. [DOI] [PubMed] [Google Scholar]
- 43.Cupples WA. Physiological regulation of food intake. American journal of physiology Regulatory, integrative and comparative physiology. 2005 Jun;288(6):R1438–43. doi: 10.1152/ajpregu.00195.2005. [DOI] [PubMed] [Google Scholar]
- 44.Knight BS, Pennell CE, Shah R, Lye SJ. Strain differences in the impact of dietary restriction on fetal growth and pregnancy in mice. Reproductive sciences. 2007 Jan;14(1):81–90. doi: 10.1177/1933719106298217. [DOI] [PubMed] [Google Scholar]
- 45.Lingas RI, Matthews SG. A short period of maternal nutrient restriction in late gestation modifies pituitary-adrenal function in adult guinea pig offspring. Neuroendocrinology. 2001 May;73(5):302–11. doi: 10.1159/000054647. [DOI] [PubMed] [Google Scholar]
- 46.McMillen IC, Robinson JS. Developmental origins of the metabolic syndrome: prediction, plasticity, and programming. Physiological reviews. 2005 Apr;85(2):571–633. doi: 10.1152/physrev.00053.2003. [DOI] [PubMed] [Google Scholar]
- 47.Stein AD, Kahn HS, Rundle A, Zybert PA, van der Pal-de Bruin K, Lumey LH. Anthropometric measures in middle age after exposure to famine during gestation: evidence from the Dutch famine. The American journal of clinical nutrition. 2007 Mar;85(3):869–76. doi: 10.1093/ajcn/85.3.869. [DOI] [PubMed] [Google Scholar]
- 48.Varma A, He J, Weissfeld L, Devaskar SU. Postnatal intracerebroventricular exposure to neuropeptide Y causes weight loss in female adult rats. American journal of physiology Regulatory, integrative and comparative physiology. 2003 Jun;284(6):R1560–6. doi: 10.1152/ajpregu.00557.2001. [DOI] [PubMed] [Google Scholar]
- 49.Wagner KD, Scholz H. The long-lasting impact of postnatal neuropeptide Y. American journal of physiology Regulatory, integrative and comparative physiology. 2003 Jun;284(6):R1382–3. doi: 10.1152/ajpregu.00124.2003. [DOI] [PubMed] [Google Scholar]
- 50.Dahly DL, Gordon-Larsen P, Popkin BM, Kaufman JS, Adair LS. Associations between multiple indicators of socioeconomic status and obesity in young adult Filipinos vary by gender, urbanicity, and indicator used. The Journal of nutrition. 2010 Feb;140(2):366–70. doi: 10.3945/jn.109.114207. Epub 2009/12/25. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jahns L, Baturin A, Popkin BM. Obesity, diet, and poverty: trends in the Russian transition to market economy. European journal of clinical nutrition. 2003 Oct;57(10):1295–302. doi: 10.1038/sj.ejcn.1601691. Epub 2003/09/25.eng. [DOI] [PubMed] [Google Scholar]
- 52.Ng SW, Zaghloul S, Ali H, Harrison G, Yeatts K, El Sadig M, et al. Nutrition transition in the United Arab Emirates. European journal of clinical nutrition. 2011 Dec;65(12):1328–37. doi: 10.1038/ejcn.2011.135. Epub 2011/07/21.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stommel M, Schoenborn CA. Accuracy and usefulness of BMI measures based on self-reported weight and height: findings from the NHANES & NHIS 2001–2006. BMC public health. 2009;9:421. doi: 10.1186/1471-2458-9-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gillum RF, Sempos CT. Ethnic variation in validity of classification of overweight and obesity using self-reported weight and height in American women and men: the Third National Health and Nutrition Examination Survey. Nutrition journal. 2005;4:27. doi: 10.1186/1475-2891-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Merrill RM, Richardson JS. Validity of self-reported height, weight, and body mass index: findings from the National Health and Nutrition Examination Survey, 2001–2006. Preventing chronic disease. 2009 Oct;6(4):A121. [PMC free article] [PubMed] [Google Scholar]
- 56.Ezzati M, Martin H, Skjold S, Vander Hoorn S, Murray CJ. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. Journal of the Royal Society of Medicine. 2006 May;99(5):250–7. doi: 10.1258/jrsm.99.5.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.VanderWeele TJ. Concerning the consistency assumption in causal inference. Epidemiology. 2009 Nov;20(6):880–3. doi: 10.1097/EDE.0b013e3181bd5638. [DOI] [PubMed] [Google Scholar]