Abstract
Escherichia coli remains as one of the most important bacteria causing infections in pediatrics and producing extended-spectrum beta-lactamases (ESBLs) making them resistant to beta-lactam antibiotics. In this study we aimed to genotype ESBL-producing E. coli isolates from pediatric patients for ESBL genes and determine their association with antimicrobial resistance. One hundred of the E. coli isolates were initially considered ESBL producing based on their MIC results. These isolates were then tested by polymerase chain reaction (PCR) for the presence or absence of CTX, TEM, SHV, GES, and VEB beta-lactamase genes. About 30.5% of isolated E. coli was ESBL-producing strain. The TEM gene was the most prevalent (49%) followed by SHV (44%), CTX (28%), VEB (8%), and GES (0%) genes. The ESBL-producing E. coli isolates were susceptible to carbapenems (66%) and amikacin (58%) and showed high resistance to cefixime (99%), colistin (82%), and ciprofloxacin (76%). In conclusion, carbapenems were the most effective antibiotics against ESBl-producing E. coli in urinary tract infection in North of Iran. The most prevalent gene is the TEM-type, but the other resistant genes and their antimicrobial resistance are on the rise.
1. Introduction
Multidrug resistant Gram-negative bacilli have been increasingly responsible for life-threatening infections all over the world [1, 2]. The extended-spectrum beta-lactamases (ESBLs) are class A plasmid mediated enzymes that hydrolyze oxyiminocephalosporin and monobactam antibiotics but are inhibited by clavulanic acid in vitro [3, 4]. Bacteria harboring ESBLs confer significant resistance to penicillin, narrow and extended-spectrum cephalosporin, and aztreonam antibiotics. They also frequently show resistance to aminoglycosides, trimethoprim/sulfamethoxazole, and quinolones [5, 6]. Different types of ESBLs have been found in different countries. The TEM and SHV types were first reported from Klebsiella pneumoniae in Western Europe [7]. The VEB was first found in a single isolate of E. coli in Vietnam [5]. But recently, the CTX type (mainly cefotaximases) is being detected with increasing frequency, particularly in ESBL-producing E. coli [8]. The GES-5 gene was first detected on plasmid in Escherichia coli from Greece in 2004 and later it was isolated from Klebsiella pneumoniae, Enterobacter cloacae, and Pseudomonas aeruginosa [9]. The CTX-M enzymes are much more active against cefotaxime and ceftriaxone than against ceftazidime [3, 10, 11].
Genotypes of ESBLs producing isolates may be associated with the antibiotic resistance pattern, as it has been reported previously that the presence of CTX-M gene has been associated with the resistance to fluoroquinolones, aminoglycosides, and cotrimoxazole [11].
Extensive use of expanded-spectrum antibiotics is one of the most important factors associated with high resistance to antibiotics and high prevalence of ESBLs [12–14].
Since increasing the rate of multidrug resistant ESBL in North of Iran and antibiotics use varies in different regions and can cause variation in the prevalence of ESBL genotypes, we decided to determine the genotype of ESBL-producing E. coli in urinary tract infection regarding the CTX, TEM, SHV, GES, and VEB genes and their antimicrobial resistance in the North of Iran.
2. Material and Methods
2.1. Urine Collection and Bacterial Isolation
Urine samples were collected from pediatric patients during a 6-month period at Buali Sina Hospital (a tertiary referral pediatric hospital) in the North of Iran. Urine samples were collected by either midstream clean catch, suprapubic bladder aspiration (SPA), or transurethral bladder catheterization (TUBC) [15]. The samples were inoculated on 5% blood agar and MacConkey's agar and the E. coli isolates were identified by using standard methods.
2.2. Antimicrobial Susceptibility Testing
Antibiotic susceptibility was determined by the Kirby-Bauer disc diffusion test on Mueller Hinton agar plate and the results were evaluated according to the Clinical Laboratory Standards Institute (CLSI) guideline 2011 [16].
2.3. Detection of ESBL-Producing E. coli by MIC
The E. coli isolates were considered potential carrier of ESBL enzyme when they showed resistance to cefotaxime and ceftriaxone. The MIC (minimum inhibitory concentration) of fourteen antibiotics including ceftazidime, ceftriaxone, cefotaxime, ceftizoxime, cefepime, cefixime, gentamicin, amikacin, meropenem, imipenem, ciprofloxacin, cotrimoxazole, colistin, and piperacillin/tazobactam (Sigma Chemical Co., Germany) for resistant E. coli strains was determined by the agar dilution method [3]. The MIC was determined on Mueller Hinton agar with twofold dilutions of antibiotics concentration (from 0.5 μg/mL to 256 μg/mL and 10 μL of microbial suspension). Microbial growth was observed and documented after 24 hours of incubation at 35°C. The result was reported according to CLSI 2011 guidelines and divided into three categories: resistant, intermediate, and susceptible. The ESBL-producing E. coli isolates were considered resistant to both cefotaxime and ceftazidime if their MIC was ≥2 μg/mL in accordance with CLSI criteria [17].
2.4. DNA Isolation and Genotyping
A single colony from each ESBL-producing isolate was transferred into 100 μL of distilled water and the bacterial DNA was extracted by using a commercial DNA extraction kit (RTA, Ankara, Turkey). Bacterial genes associated with antimicrobial resistance phenotypes were detected by PCR amplification of target genes by using specific PCR primers (Table 1) in Eppendorf thermal cycler (Eppendorf, Germany). Table 1 shows primer sequences and specific thermal profile from TEM, SHV, CTX, VEB, and GES genes. PCR mixtures were prepared by using 5 μL template DNA, 12.5 μL PCR master mix; 1 × PCR buffer [Tris-Cl, KCl, (NH4)2SO4, 1.5 mM MgCl2] (pH 8.7), 200 μM dNTP, and 1 μL of each 10 pM primer and 0.5 U Taq DNA polymerase (Takara, Kyoto, Japan) in a final volume of 25 μL. In all experiments, the following reference strains were used as positive controls: K. pneumoniae 7881 (CTX-M), K. pneumoniae 7881 strain (containing TEM and SHV), P. aeruginosa ATCC 27853 (VEB-1), and K. pneumoniae (GES) which was kindly provided by Professor P. Nordmann CHU Bicetre, France. A non-ESBL-producing strain (E. coli ATCC 25922) was used as a negative control.
Table 1.
The sequences of primers and thermal condition used in PCR amplification.
| Target genes | Primer used (5′-3′) | Thermal cycling condition | PCR product size |
|---|---|---|---|
| TEM | TAATCAGTGAGGCACCTATCTC GAGTATTCAACATTTCCGTGTC [18, 19] |
94°C 3 min → 35 × [94°C 30 sec, 45°C 45 sec, 72°C 40 sec] → 72°C 7 min |
800 bp |
|
| |||
| CTX | TTTGCGATGTGCAGTACCAGTAA CGATATCGTTGGTGGCATA [20] |
94°C 5 min → 40 × [94°C 45 sec, 53.1°C 45 sec, 72°C 1 min] → 72°C 7 min |
593 bp |
|
| |||
| VEB | CGACTTCCATTTCCCGATGC GGACTCTGCAACAAATACGC [9] | 93°C 3 min → 40 × [93°C 1 min, 54.9°C 1 min, 72°C 1 min] → 72°C 7 min |
585 bp |
|
| |||
| SHV | GGTTATGCGTTATATTCGCC TTAGCGTTGCCAGTGCTC [21] |
1 cycle of 5 min at 96°C; 35 cycles of 1 min at 96°C, 1 min at 60°C, 1 min at 72°C; 1 cycle of 10 min at 72°C |
867 bp |
|
| |||
| GES | ATGCGCTTCATTCACGCAC CTATTTGTCCGTGCTCAGG [22] | 1 cycle of 5 min at 95°C; 30 cycles of 1 min at 95°C, 45 sec at 55°C, 1 min 30 sec at 72°C; 1 cycle of 8 min at 72°C |
846 bp |
3. Results
3.1. ESBL-Producing E. coli
Of 327 uropathogen E. coli isolates, one hundred (30.5%) were positive for extended-spectrum beta-lactamases. The ESBL isolates showed highest susceptibility to carbapenems (66%) and amikacin (58%) which is in accordance with 2011 CLSI criteria for MIC test (Table 2). The highest rate of resistance was observed for the following antibiotics: cefixime (99%), colistin (82%), and ciprofloxacin (76%).
Table 2.
Percentage of antimicrobial susceptibility in ESBL-producing E. coli strains based on MIC results.
| Antimicrobial agents | R (%) | I (%) | S (%) |
CLSI breakpoints (µg/mL) |
|
|---|---|---|---|---|---|
| S | R | ||||
| Cephalosporins | |||||
| Cefepime | 67 | 13 | 20 | ≤8 | ≥32 |
| Cefixime | 99 | 0 | 1 | ≤0.25 | ≥1 |
| Ceftriaxone | 28 | 42 | 30 | ≤8 | ≥64 |
| Ceftazidime | 19 | 26 | 55 | ≤16 | ≥32 |
| Ceftizoxime | 46 | 27 | 27 | ≤8 | ≥64 |
| Cefotaxime | 13 | 40 | 47 | ≤8 | ≥64 |
| Carbapenems | |||||
| Imipenem | 23 | 11 | 66 | ≤4 | ≥16 |
| Meropenem | 18 | 15 | 67 | ≤4 | ≥16 |
| Aminoglycosides | |||||
| Amikacin | 34 | 8 | 58 | ≤16 | ≥64 |
| Gentamicin | 37 | 12 | 51 | ≤4 | ≥16 |
| Others | |||||
| Ciprofloxacin | 76 | 0 | 24 | ≤1 | ≥4 |
| Colistin | 82 | 0 | 18 | ≤2 | ≥4 |
| Trimethoprim/sulfamethoxazole | 65 | 7 | 28 | ≤2/38 | ≥4/76 |
| Piperacillin/tazobactam | 20 | 38 | 42 | ≤16/4 | ≥128/4 |
R: resistance, I: intermediate, S: sensitive, CLSI: Clinical Laboratory Standards Institute, and ESBL: extended-spectrum beta-lactamase.
3.2. Prevalence of ESBL Genes
The results of ESBL genotyping are shown in Figure 1. The TEM gene was the most prevalent (49%) followed by SHV (44%), CTX (28%), VEB (8%), and GES (0%) genes. None of our isolates carried the GES gene. About 12% of ESBL isolates were shown to have both TEM and CTX-M genes. Overall, 30% of isolates carried 2 resistant genes (Figure 2).
Figure 1.
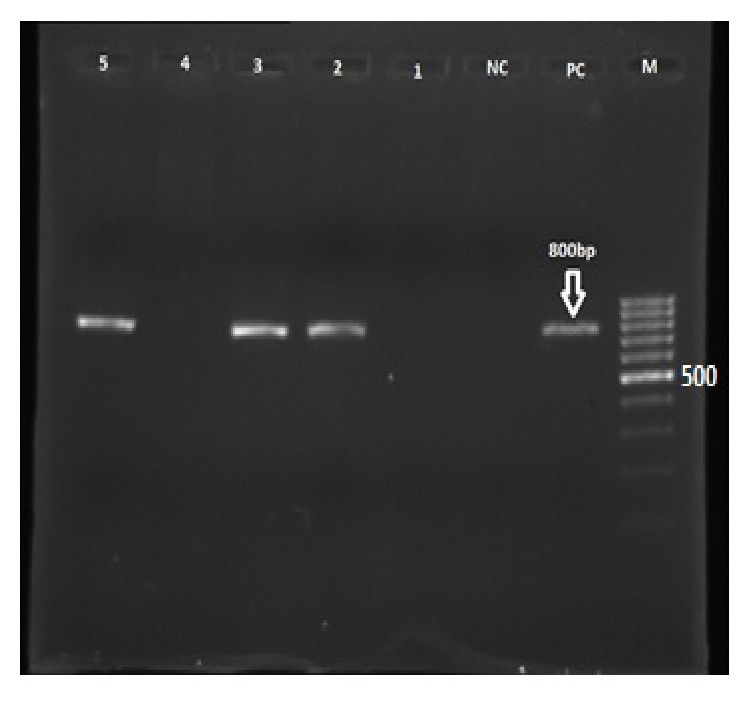
Agarose gel showing the 800 bp PCR fragments band for TEM gene from ESBL-producing E. coli isolates. Lanes: M: molecular weight marker (100 bp); PC: K. pneumoniae 7881 (positive control); NC: E. coli ATCC 25922 (negative control); 2, 3, and 5: TEM positive clinical samples; 1 and 4: TEM negative clinical samples.
Figure 2.
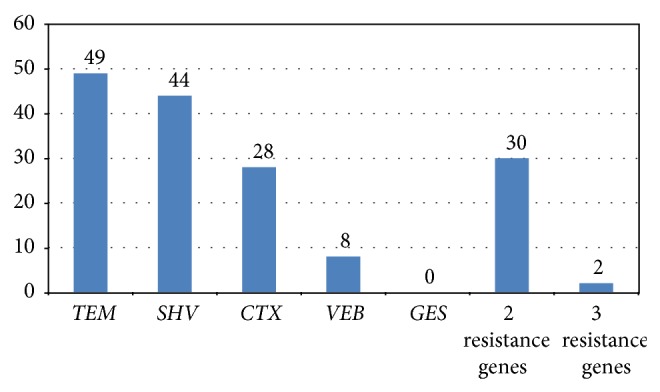
Distribution of TEM, CTX, SHV, GES, and VEB genes in ESBL-producing E. coli isolates.
3.3. Association of Antimicrobial Resistance with Resistant Genes
Table 3 shows the presence or absence of resistant genes, susceptibility, and resistance to different antimicrobial agents. In most cases, there were not any significant differences regarding presence or absence of genes expression. Interestingly, higher resistance to cefotaxime, amikacin, and ceftriaxone was found in TEM negative group (P = 0.04, P = 0.008, and P = 0.02, resp.).
Table 3.
Association between gene expression and antimicrobial nonsusceptibility in ESBL-producing E. coli.
| Antimicrobial agents | TEM | CTX | VEB | SHV | ||||
|---|---|---|---|---|---|---|---|---|
| Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | |
| Cephalosporins | ||||||||
| Cefepime | 38 (77.6%) | 42 (82.4%) | 23 (82.1%) | 57 (79.2%) | 6 (75%) | 74 (80.4%) | 38 (86.4%) | 42 (75%) |
| Cefixime | 49 (100%) | 50 (98%) | 27 (96.4%) | 72 (100%) | 8 (100%) | 91 (98.9%) | 43 (97.7%) | 56 (100%) |
| Ceftriaxone | 29 (59.2%) | 41 (80.4%)∗ | 22 (78.6%) | 48 (66.7%) | 4 (50%) | 66 (71.7%) | 33 (75%) | 37 (66.7%) |
| Ceftazidime | 22 (44.9%) | 23 (45.1%) | 11 (39.3%) | 34 (47.2%) | 6 (75%)∗ | 39 (42.4%) | 17 (38.6%) | 28 (50%) |
| Ceftizoxime | 34 (69.4%) | 39 (76.5%) | 23 (82.1%) | 50 (69.4%) | 6 (75%) | 67 (72.8%) | 32 (12.7%) | 41 (73.2%) |
| Cefotaxime | 21 (42.9%) | 32 (62.7%)∗ | 18 (64.3%) | 35 (48.6%) | 5 (62.5%) | 48 (52.2%) | 21 (47.7%) | 32 (57.1%) |
| Carbapenems | ||||||||
| Imipenem | 14 (28.6%) | 20 (39.2%) | 11 (39.3%) | 23 (31.9%) | 3 (37.5%) | 31 (33.7%) | 15 (34.1%) | 19 (34%) |
| Meropenem | 12 (24.5%) | 21 (42.2%) | 9 (32.1%) | 24 (33.3%) | 3 (37.5%) | 30 (32.6%) | 13 (29.5%) | 20 (35.7%) |
| Aminoglycosides | ||||||||
| Amikacin | 14 (28.6%) | 28 (54.9%)∗ | 13 (46.4%) | 29 (40.3%) | 3 (37.5%) | 39 (42.4%) | 24 (54.5%)∗ | 18 (32%) |
| Gentamicin | 21 (42.9%) | 28 (54.9%) | 14 (50%) | 35 (48.6%) | 5 (62.5%) | 44 (47.8%) | 27 (61.4%)∗ | 22 (39.3%) |
| Others | ||||||||
| Ciprofloxacin | 34 (69.4%) | 42 (82.4%) | 21 (75%) | 55 (76.4%) | 5 (62.5%) | 71 (77.2%) | 39 (88.6%)∗ | 37 (66%) |
| Colistin | 39 (79.6) | 43 (84.3%) | 23 (82.1%) | 59 (81.9%) | 6 (75%) | 76 (82.6%) | 38 (86.4%) | 44 (78.6%) |
| TMP/SXT | 34 (69.4%) | 38 (74.5%) | 21 (75%) | 51 (70.8%) | 4 (50%) | 68 (73.9%) | 29 (65.9%) | 43 (76.8%) |
| Pip/TBZ | 29 (59.2%) | 29 (59.2%) | 15 (53.6%) | 43 (59.7%) | 4 (50%) | 4 (50%) | 25 (56.8% ) | 33 (59%) |
R: resistance, I: intermediate, S: sensitive, and ESBL: extended-spectrum beta-lactamase.
∗Significant differences (P < 0.05).
Resistance to cotrimoxazole, imipenem, amikacin, and third generation cephalosporins was observed more in CTX-M positive isolates than in CTX-M negative isolates. The presence of VEB gene was associated with higher resistance to carbapenems, gentamicin, and third generation cephalosporins. The presence of VEB gene was significantly associated with resistance to ceftazidime (P = 0.05). The presence of SHV gene was also associated with aminoglycosides and ciprofloxacin resistance. Our results also showed a correlation between the presence of resistant genes and high rate of resistance to cefixime, colistin, and cefepime.
4. Discussion
In this study, attempt has been made to genotype the ESBL-producing E. coli isolates from pediatric patients for CTX, TEM, SHV, GES, and VEB genes and determine their association with antimicrobial resistance. The high prevalence of ESBL-producing E. coli (30.5%) and their high level of resistance to broad spectrum antimicrobial agents in ESBL-producing E. coli (e.g., 34% resistance to carbapenems) are reported in this study. In addition, our study also highlights an association between the presence of SHV gene and resistance to aminoglycosides and fluoroquinolones antibiotics.
The prevalence of ESBL-producing E. coli isolates varies in different parts of the world and even among different hospitals within a country. The rate of prevalence in our center was about 30.5% which is close to the results reported by other studies in different regions of Iran [18, 23–25]. The rates of ESBL-producing E. coli were lower in other countries such as India (27%), Lebanon (13.3%), Korea (9.2%), and turkey (17%) [26, 27].
In addition to beta-lactam antibiotics, ESBLs producing isolates are also resistant to other antimicrobial agents, such as aminoglycosides, tetracycline, and trimethoprim/sulfamethoxazole [28]. The isolates showed high resistance to amikacin (34%), colistin (82%), and trimethoprim/sulfamethoxazole (65%) in our study. The study by Babypadmini and Appalaraju reported 74% resistance to trimethoprim/sulfamethoxazole and 91.6% resistance to fluoroquinolone in ESBL-producing E. coli pathogens by disk diffusion method [29], which is much higher than our results (65% resistance to trimethoprim/sulfamethoxazole and 76% resistance to fluoroquinolone). This difference may be due to use of different methods of evaluation for determining the susceptibility. We determined the antimicrobial resistance by the microdilution method which is more sensitive than disk diffusion method [22]. The results from other studies from Malaysia and Spain showed lower resistance to trimethoprim/sulfamethoxazole and ciprofloxacin in urine samples from adults than this study which may be due to different patient population (adults versus pediatrics). Totally, the increasing resistance of E. coli to trimethoprim makes this drug less effective as empiric treatment of UTI [30].
The ESBL-producing E. coli isolates in our study showed high resistance to colistin which is in accordance with the studies reported by Benenson et al. [31] and Ku et al. [32]. Rapid increase in colistin resistance in K. pneumoniae strains was reported. Although some studies describe colistin activity against Pseudomonas and Acinetobacter isolates, the activity of colistin against ESBL-producing E. coli remains unclear [31, 33].
One of the most prominent and concerning findings in our study is the high resistance to broad spectrum antibiotics such as carbapenems which is in contrast with other studies that reported lower resistance (about 34%) to imipenem and meropenem in India [18], Malaysia [21], Columbia, Saudi Arabia [34], and Iran [24, 35, 36]. Although we found carbapenems as the most effective agent against the ESBL but the high rate of resistance, in comparison with other studies, is still very concerning. Recently, Alikhani et al. study in Iran showed 75% susceptibility among ESBL pathogens to carbapenems [20]. The main reason for large difference in the rate of resistance among different countries and different regions within the same country is due to the extensive use of broad spectrum antibiotics especially third generation cephalosporins and persistence of the resistant strains in health care facilities. Extensive usage of broad spectrum antibiotics specially third generation cephalosporins was reported by Salehifar et al. in our center. The rate of antibiotics consumption in our setting was significantly higher than other centers [37].
TEM was the most frequent resistant gene in ESBL-producing E. coli isolates in this study as it was also reported in several other studies [21, 24, 35]. GES resistant gene was not found in ESBL-producing E. coli isolates which is in line with the low frequency of this gene in ESBL-producing E. coli strains [36].
Analysis of the genotypes, antimicrobial resistance pattern, and MIC of different antimicrobial agents for ESBL-producing E. coli isolates showed a significantly higher resistance to ceftriaxone, cefotaxime, and amikacin in TEM genotype negative group. The study by French et al. showed that the SHV producing strains of E. coli were resistant to all aminoglycosides but sensitive to ciprofloxacin [38] but in this study the SHV genotype positive isolates were significantly resistant to both aminoglycosides and ciprofloxacin.
About 82% and 50% of CTX-M producing strains were resistant to quinolones and aminoglycosides, respectively, which was higher compared to Edelstein et al. study (21%) [39] but it was lower than the Mendonça et al. study (93%) [40]. The resistance to cefotaxime in CTX-M producers in our study was higher than those reported.
5. Conclusion
Although the TEM was found to be the most prevalent resistant gene, the prevalence of other resistant genes along with antimicrobial resistance is on the rise. Carbapenems were the most effective antibiotics against ESBl-producing E. coli in urinary tract infection in North of Iran. Considering the high prevalence of SHV, aminoglycosides and fluoroquinolones are not recommended for empiric therapy. The high rate of SHV and VEB transmission will result in increasing the resistance to third generation cephalosporins, aminoglycosides, and fluoroquinolones.
Acknowledgments
This study was supported by Mazandaran University of Medical Sciences, Sari, Iran. The authors acknowledge Mr. Nemati, M.S. in microbiology, for his professional support.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Girish N., Saileela K., Mohanty S. K. Extended spectrum beta-lactamase producing Klebsiella pneumoniae and Escherichia coli in neonatal intensive care unit. Journal of Bacteriology & Parasitology. 2012;3:p. 2. [Google Scholar]
- 2.Poulou A., Grivakou E., Vrioni G., et al. Modified CLSI extended-spectrum β-lactamase (ESBL) confirmatory test for phenotypic detection of ESBLs among Enterobacteriaceae producing various β-lactamases. Journal of Clinical Microbiology. 2014;52(5):1483–1489. doi: 10.1128/JCM.03361-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhat M. A., Sageerabanoo S., Kowsalya R., Sarkar G. The occurrence of CTX-M3 type extended spectrum beta lactamases among Escherichia coli causing urinary tract infections in a tertiary care hospital in puducherry. Journal of Clinical and Diagnostic Research. 2012;6(7):1203–1206. [Google Scholar]
- 4.Bhattacharjee A., Sen M. R., Prakash P., Gaur A., Anupurba S. Increased prevalence of extended spectrum β lactamase producers in neonatal septicaemic cases at a tertiary referral hospital. Indian Journal of Medical Microbiology. 2008;26(4):356–360. doi: 10.4103/0255-0857.43578. [DOI] [PubMed] [Google Scholar]
- 5.Bradford P. A. Extended-spectrum β-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clinical Microbiology Reviews. 2001;14(4):933–951. doi: 10.1128/CMR.14.4.933-951.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paterson D. L., Hujer K. M., Hujer A. M., et al. Extended-spectrum β-lactamases in klebsiella pneumoniae bloodstream isolates from seven countries: dominance and widespread prevalence of SHV- and CTX-M-Type β-lactamases. Antimicrobial Agents and Chemotherapy. 2003;47(11):3554–3560. doi: 10.1128/AAC.47.11.3554-3560.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lal P., Kapil A., Das B. K., Sood S. Occurrence of TEM & SHV gene in extended spectrum β-lactamases (ESBLs) producing Klebsiella sp. isolated from a tertiary care hospital. Indian Journal of Medical Research. 2007;125(2):173–178. [PubMed] [Google Scholar]
- 8.Rodríguez-Baño J., Navarro M. D., Romero L., et al. Clinical and molecular epidemiology of extended-spectrum β-lactamase. Producing Escherichia coli as a cause of nosocomial infection or colonization: implications for control. Clinical Infectious Diseases. 2006;42(1):37–45. doi: 10.1086/498519. [DOI] [PubMed] [Google Scholar]
- 9.Kim J., Hong S. G., Bae I. K., et al. Emergence of Escherichia coli sequence type ST131 carrying both the bla GES-5 and bla CTX-M-15 genes. Antimicrobial Agents and Chemotherapy. 2011;55(6):2974–2975. doi: 10.1128/AAC.01703-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jemima S. A., Verghese S. Multiplex PCR for blaCTX-M & blaSHV in the extended spectrum beta lactamase (ESBL) producing gram-negative isolates. Indian Journal of Medical Research. 2008;128(3):313–317. [PubMed] [Google Scholar]
- 11.Ruppé E., Hem S., Lath S., et al. CTX-M β-lactamases in Escherichia coli from community-acquired urinary tract infections, Cambodia. Emerging Infectious Diseases. 2009;15(5):741–748. doi: 10.3201/eid1505.071299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shukla I., Tiwari R., Agrawal M. Prevalence of extended spectrum β-lactamasee producing Klebsiella pneumoniae in a tertiary care hospital. Indian Journal of Medical Microbiology. 2004;22(2):87–91. [PubMed] [Google Scholar]
- 13.Liem T. B. Y., Filius M., van der Linden P. D., Janknegt R., Natsch S., Vulto A. G. 3.1 Changes in antibiotic use in Dutch hospitals over a 6-year period: 1997–2002. Antimicrobial Drug Use in Hospitalized Children. 2011;63:p. 60. [PubMed] [Google Scholar]
- 14.Oteo J., Bautista V., Lara N., et al. Parallel increase in community use of fosfomycin and resistance to fosfomycin in extended-spectrum β-lactamase (ESBL)-producing Escherichia coli . Journal of Antimicrobial Chemotherapy. 2010;65(11):2459–2463. doi: 10.1093/jac/dkq346. [DOI] [PubMed] [Google Scholar]
- 15.Liaison Representatives. Practice parameter: the diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. American Academy of Pediatrics. Committee on Quality Improvement. Subcommittee on Urinary Tract Infection. Pediatrics. 1999;103(4):843–852. doi: 10.1542/peds.103.4.843. [DOI] [PubMed] [Google Scholar]
- 16.Cockerill F. R. Performance Standards for Antimicrobial Susceptibility Testing: Twenty-First Informational Supplement. Clinical and Laboratory Standards Institute (CLSI); 2011. [Google Scholar]
- 17.Wayne P. CLSI Document. M100-S21. Clinical and Laboratory Standards Institute; 2011. Performance standards for antimicrobial susceptibility testing. Twenty firt informational supplement. [Google Scholar]
- 18.Manoharan A., Premalatha K., Chatterjee S., Mathai D. Correlation of TEM, SHV and CTX-M extended-spectrum beta lactamases among Enterobacteriaceae with their in vitro antimicrobial susceptibility. Indian Journal of Medical Microbiology. 2011;29(2):161–164. doi: 10.4103/0255-0857.81799. [DOI] [PubMed] [Google Scholar]
- 19.Poirel L., Le Thomas I., Naas T., Karim A., Nordmann P. Biochemical sequence analyses of GES-1, a novel class A extended-spectrum β-lactamase, and the class 1 integron In52 from Klebsiella pneumoniae . Antimicrobial Agents and Chemotherapy. 2000;44(3):622–632. doi: 10.1128/AAC.44.3.622-632.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alikhani M. Y., Karimi Tabar Z., Mihani F., et al. Antimicrobial resistance patterns and prevalence of blaPER-1 and blaVEB-1 genes among ESBL-producing Pseudomonas aeruginosa isolates in West of Iran. Jundishapur Journal of Microbiology. 2014;7(1) doi: 10.5812/jjm.8888.e8888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benenson S., Navon-Venezia S., Carmeli Y., et al. Carbapenemresistant Klebsiella pneumoniae endocarditis in a young adult. Successful treatment with gentamicin and colistin. International Journal of Infectious Diseases. 2009;13(5):e295–e298. doi: 10.1016/j.ijid.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 22.Lee Y. H., Cho B., Bae I. K., Chang C. L., Jeong S. H. Klebsiella pneumoniae strains carrying the chromosomal SHV-11 β-lactamase gene produce the plasmid-mediated SHV-12 extended-spectrum β-lactamase more frequently than those carrying the chromosomal SHV-1 β-lactamase gene. Journal of Antimicrobial Chemotherapy. 2006;57(6):1259–1261. doi: 10.1093/jac/dkl115. [DOI] [PubMed] [Google Scholar]
- 23.Kochaksaraii B., Omran N. A., Javid N., Shakeri F., Yazdi M., Ghaemi E. Extended spectrum beta lactamase producing E.coli isolated from Gorgan, North of Iran. Medical Laboratory Journal. 2012;6(1) [Google Scholar]
- 24.Moosavian M., Deiham B. Distribution of TEM, SHV and CTX-M Genes among ESBL-producing Enterobacteriaceae isolates in Iran. African Journal of Microbiology Research. 2012;6:5433–5439. [Google Scholar]
- 25.Arbabi L., Rahbar M., Jabbari M., et al. Extended-spectrum beta-lactamase-producing E. coli and Klebsiella pneumoniae isolated from urinary tract infections in Milad Hospital, Tehran, Iran. HealthMED Journal. 2012 [Google Scholar]
- 26.Shahcheraghi F., Nikbin V. S., Feizabadi M. M. Prevalence of ESBLs genes among multidrug-resistant isolates of pseudomonas aeruginosa isolated from patients in Tehran. Microbial Drug Resistance. 2009;15(1):37–39. doi: 10.1089/mdr.2009.0880. [DOI] [PubMed] [Google Scholar]
- 27.Ananthan S., Subha A. Cefoxitin resistance mediated by loss of a porin in clinical strains of Klebsiella pneumoniae and Escherichia coli . Indian Journal of Medical Microbiology. 2005;23(1):20–23. doi: 10.4103/0255-0857.13867. [DOI] [PubMed] [Google Scholar]
- 28.Branger C., Zamfir O., Geoffroy S., et al. Genetic background of Escherichia coli and extended-spectrum β-lactamase type. Emerging Infectious Diseases. 2005;11(1):54–61. doi: 10.3201/eid1101.040257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Babypadmini S., Appalaraju B. Extended spectrum β-lactamases in urinary isolates of Escherichia coli and Klebsiella pneumoniae—prevalence and susceptibility pattern in a tertiary care hospital. Indian Journal of Medical Microbiology. 2004;22(3):172–174. [PubMed] [Google Scholar]
- 30.Swerkersson S., Jodal U., Åhrén C., Hansson S. Urinary tract infection in small outpatient children: the influence of age and gender on resistance to oral antimicrobials. European Journal of Pediatrics. 2014;173(8):1075–1081. doi: 10.1007/s00431-014-2289-3. [DOI] [PubMed] [Google Scholar]
- 31.Benenson S., Navon-Venezia S., Carmeli Y., et al. Carbapenem-resistant Klebsiella pneumoniae endocarditis in a young adult. Successful treatment with gentamicin and colistin. International Journal of Infectious Diseases. 2009;13(5):e295–e298. doi: 10.1016/j.ijid.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 32.Ku Y.-H., Lee M.-F., Chuang Y.-C., Chen C.-C., Yu W.-L. In vitro activity of colistin sulfate against Enterobacteriaceae producing extended-spectrum beta lactamases. Journal of Microbiology, Immunology and Infection. 2014 doi: 10.1016/j.jmii.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 33.Walkty A., DeCorby M., Nichol K., Karlowsky J. A., Hoban D. J., Zhanel G. G. In vitro activity of colistin (polymyxin E) against 3,480 isolates of gram-negative bacilli obtained from patients in Canadian hospitals in the CANWARD study, 2007–2008. Antimicrobial Agents and Chemotherapy. 2009;53(11):4924–4926. doi: 10.1128/AAC.00786-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kader A. A., Kumar A. K. Prevalence of extended spectrum β-lactamase among multidrug resistant gram-negative isolates from a general hospital in Saudi Arabia. Saudi Medical Journal. 2004;25(5):570–574. [PubMed] [Google Scholar]
- 35.Shahcheraghi F., Nasiri S., Noveiri H. Detection of extended-spectrum β-lactamases (ESBLs) in Escherichia coli . Iranian Journal of Clinical Infectious Diseases. 2009;4(2):65–70. [Google Scholar]
- 36.Hawkey P. M. Prevalence and clonality of extended-spectrum β-lactamases in Asia. Clinical Microbiology and Infection. 2008;14(1):159–165. doi: 10.1111/j.1469-0691.2007.01855.x. [DOI] [PubMed] [Google Scholar]
- 37.Salehifar E., Nasehi M. M., Eslami G., Sahraei S., Alizadeh-Navai R. Determination of antibiotics consumption in Buali-Sina pediatric Hospital, Sari 2010-2011. Iranian Journal of Pharmaceutical Research. 2014;13(3):p. 995. [PMC free article] [PubMed] [Google Scholar]
- 38.French G. L., Shannon K. P., Simmons N. Hospital outbreak of Klebsiella pneumoniae resistant to broad-spectrum cephalosporins and β-lactam-β-lactamase inhibitor combinations by hyperproduction of SHV-5 β-lactamase. Journal of Clinical Microbiology. 1996;34(2):358–363. doi: 10.1128/jcm.34.2.358-363.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Edelstein M., Pimkin M., Palagin I., Edelstein I., Stratchounski L. Prevalence and Molecular Epidemiology of CTX-M Extended-Spectrum β-Lactamase-Producing Escherichia coli and Klebsiella pneumoniae in Russian Hospitals. Antimicrobial Agents and Chemotherapy. 2003;47(12):3724–3732. doi: 10.1128/AAC.47.12.3724-3732.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mendonça N., Leitão J., Manageiro V., Ferreira E., Caniça M. Spread of extended-spectrum β-lactamase CTX-M-producing Escherichia coli clinical isolates in community and nosocomial environments in Portugal. Antimicrobial Agents and Chemotherapy. 2007;51(6):1946–1955. doi: 10.1128/AAC.01412-06. [DOI] [PMC free article] [PubMed] [Google Scholar]


