Summary
HHLA2 is a newly identified B7 family member that modulates T cell functions through interaction with TMIGD2 and possibly a second receptor, with coinhibition in two studies and costimulation in one study. HHLA2 is expressed on a variety of human cancers, and its coinhibitory function makes it a candidate for cancer immunotherapy.
In this issue of Clinical Cancer Research, Janakiram and colleagues (1) report that human endogenous retrovirus-H long terminal repeat-associating protein 2 (HHLA2) had limited expression in normal human tissues but was widely expressed in human cancers. They also identified transmembrane and immunoglobulin domain containing 2 (TMIGD2) as one of the receptors for HHLA2.
With the success of PD-1 pathway antagonists in cancer immunotherapy, there is great interest in identifying other B7/CD28 family immunosuppressive pathways that could be targeted to enhance anti-tumor immunity. HHLA2 was discovered in 1999 as a new member of the immunoglobulin (Ig) superfamily (2) and recent work has emphasized its immunologic activity and similarity to the B7 family, with alternative names of B7-H5 and B7H7 (3–5). HHLA2 is a membrane protein with three Ig-like domains (IgV-IgC-IgV) (2) (5) (4), while other members of the B7 family generally have only two Ig domains (IgV-IgC). HHLA2 is somewhat more closely related to B7-H3 and B7-H4 and shares 10–18% amino acid identity and 23–33% similarity to B7 family members (4). HHLA2 mRNA is highly expressed in kidney, colon, small intestine and lung (2) (5). By immunohistochemistry, HHLA2 protein in normal human tissues is expressed in the epithelium of kidney, gut, gallbladder and breast as well as placental trophoblast cells (1). In the immune system, HHLA2 protein is constitutively expressed on human monocytes/macrophages. HHLA2 is not expressed on immature dendritic cells but expression on both dendritic cells and monocytes is modestly upregulated by inflammatory signals like LPS, IFN-γ, and poly I:C. HHLA-2 is not expressed on resting T or B cells and is upregulated on activated B cells (4) (5).
Zhao et al used HHLA2-Ig fusion protein to show that resting T cells expressed a receptor for HHLA2 (4). They reasoned that since the HHLA2 gene was lost in mice and rats, the receptor should also be lost due to co-evolution. Janakiram et al tested Ig family members expressed in humans but not in mice and rats for binding to HHLA2-Ig and identified TMIGD2 as a receptor for HHLA2 (1). Zhu et al approached the problem from the receptor side, identifying TMIGD2 as a membrane protein with 10% amino acid identity with CD28, CTLA-4, ICOS and PD-1, hence the name CD28H (5). They identified HHLA2 as a ligand for TMIGD2 in a high throughput screen of 2300 individually transfected membrane genes for binding to TMIGD2-Ig (5). TMIGD2 has one extracellular IgV-like domain, a transmembrane region, and a proline-rich cytoplasmic domain with two tyrosine signaling motifs (6) (1) (5). HHLA2 does not interact with other known members of the CD28 or B7 gene families (4) (5).
Using a TMIGD2 monoclonal antibody (mAb), Zhu et al (5) showed that TMIGD2 protein is constitutively expressed on all naïve T cells and the majority of natural killer (NK) cells, but not on T regulatory cells or B cells. TMIGD2 expression was slowly lost with repetitive stimulation of T cells. Consistent with this, TMIGD2 was expressed on only about half of memory T cells and TMIGD2 negative T cells had a terminally differentiated, senescent phenotype. This pattern of HHLA2 receptor expression on resting T cells is consistent with the results of Zhao et al; however, they also showed expression on antigen presenting cells (APC) where TMIGD2 is not expressed, suggesting the possibility of a second receptor. TMIGD2 has also been shown to be expressed in endothelial and epithelial cells and function to reduce cell migration and promote capillary tube formation during angiogenesis (6).
Three studies have shown that HHLA2 regulates human T cell functions. All used plate-bound HHLA2-Ig and anti-CD3 to stimulate purified human T cells. Two groups reported inhibition of T cell proliferation and cytokine production (INF-γ, TNF-α, and others) (4, 7) while the other reported increased T cell proliferation and cytokine production (5). The group reporting costimulatory activity also found stimulatory activity for a plate-bound anti-TMIGD2 mAb and anti-CD3. In addition, an anti-HHLA2 mAb that blocked interaction with TMIGD2 reduced proliferative responses in a CD4 T cell allogeneic T cell response. The costimulatory function of HHLA2 and TMIGD2 interaction was also observed in vivo, using a human xenograft model of graft versus host disease or a humanized mouse model (5).
These opposing results with seemingly similar assays are reminiscent of initial results with PD-L1 (B7-H1) (8, 9) and might be explained by the complexity of interpreting whether a biological result is due to receptor engagement or blockade. Alternatively, the opposite effects of HHLA2 on T cell function may be explained by HHLA2 binding to positive and negative receptors, as shown in Figure 1. In this model, HHLA2 on APCs costimulates naïve T cell proliferation and cytokine production through TMIGD2 via serine-threonine kinase AKT phosphorylation (5). As activated T cells lose TMIGD2 expression, a second receptor for HHLA2 on activated T cells exerts a coinhibitory function (4, 7). Identification of a second receptor would clarify the functions of HHLA2 on T cell activation as well as its function in tumor environments where the interaction of activated T cells and tumor cells is involved.
Figure 1.
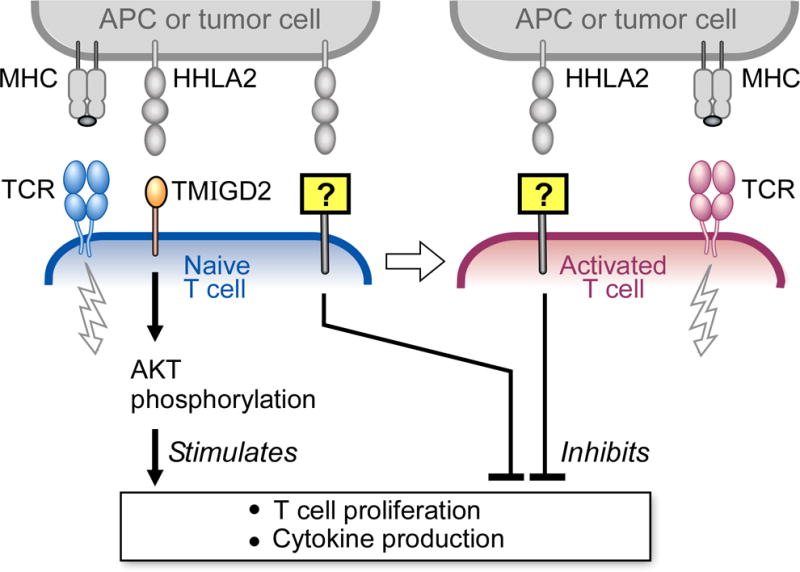
Model for HHLA2 interaction with two receptors to regulate T cell functions. Concomitant with T cell receptor (TCR) signaling, TMIGD2 on naïve T cells interacts with HHLA2 on APCs and costimulates T cell proliferation and cytokine production via a pathway involving AKT phosphorylation. With repetitive T cell activation, expression of TMIGD2 is gradually lost, allowing expression of a second receptor to become dominant. HHLA2 on APCs or tumor cells can interact with this second receptor and exert a coinhibitory function.
Janakiram et al. show that HHLA2 is expressed in 20–70% of a wide range of human cancers from the breast, lung, thyroid, melanoma, pancreas, ovary, liver, bladder, colon, prostate, kidney, and esophagus but not on endometrial, gallbladder, larynx, stomach, uterine, or lymphoma (1). Their data demonstrated that more than 50% of triple negative breast cancer (TNBC) tumors have high HHLA2 expression and that patients with higher levels of HHLA2 on their tumors have a higher risk of disease spread and advanced stage. Analysis of the cancer genome atlas (TCGA) database showed that TNBC had higher HHLA2 copy number gains than other subtypes of breast cancer, which provides a possible mechanism for overexpression. Since HHLA2 can suppress T cell function, the up-regulation of HHLA2 expression on tumor cells and inducible HHLA2 expression on APCs provides a novel mechanism for tumor immune evasion. Therefore, HHLA2 could be an attractive target for human cancer immunotherapy.
Further understanding the immunologic functions of the HHLA2 pathway will guide the selection of agents for cancer immunotherapy. Resolution of these functional differences will not come through the study of knockout mice or syngeneic mouse tumor models since HHLA2 and TMIGD2 do not exist in mice. Additional work with monomeric Fab, fusion proteins and mAbs mutated to not engage Fc receptor, HHLA2 transfected cells, non-rodent animal models, and others will all be welcome.
Acknowledgments
Grant Support:
This work was supported by NIH grants P01AI056299, U54CA163125, P50CA101942 and HHSN272201100018C (GF).
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Janakiram M, Chinai JM, Fineberg S, Fiser A, Montagna C, Medaverepu R, et al. Expression, clinical significance, and receptor identification of the newest B7 family member HHLA2 protein. Clin Cancer Res. 2014 doi: 10.1158/1078-0432.CCR-14-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mager DL, Hunter DG, Schertzer M, Freeman JD. Endogenous retroviruses provide the primary polyadenylation signal for two new human genes (HHLA2 and HHLA3) Genomics. 1999;59:255–263. doi: 10.1006/geno.1999.5877. [DOI] [PubMed] [Google Scholar]
- 3.Flajnik MF, Tlapakova T, Criscitiello MF, Krylov V, Ohta Y. Evolution of the B7 family: co-evolution of B7H6 and NKp30, identification of a new B7 family member, B7H7, and of B7’s historical relationship with the MHC. Immunogenetics. 2012;64:571–590. doi: 10.1007/s00251-012-0616-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao R, Chinai JM, Buhl S, Scandiuzzi L, Ray A, Jeon A, et al. HHLA2 is a member of the B7 family and inhibits human CD4 and CD8 T-cell function. Proc Natl Acad Sci U S A. 2013;110:9879–9884. doi: 10.1073/pnas.1303524110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu Y, Yao S, Iliopoulou BP, Han X, Augustine MM, Xu H, et al. B7-H5 costimulates human T cells via CD28H. Nat Commun. 2013;4:2043. doi: 10.1038/ncomms3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rahimi N, Rezazadeh K, Mahoney JE, Hartsough E, Meyer RD. Identification of IGPR-1 as a novel adhesion molecule involved in angiogenesis. Mol Biol Cell. 2012;23:1646–1656. doi: 10.1091/mbc.E11-11-0934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang J, Manick B, Wu G, Hao R. Biofunctions of three new B7 family members (IRM7P.486) J Immunol. 2014;192(Supplement 126.111) [Google Scholar]
- 8.Freeman GJ, Long AJ, Iwai Y, Bourque K, Chernova T, Nishimura H, et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med. 2000;192:1027–1034. doi: 10.1084/jem.192.7.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dong H, Zhu G, Tamada K, Chen L. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med. 1999;5:1365–1369. doi: 10.1038/70932. [DOI] [PubMed] [Google Scholar]


