Abstract
Cysteinyl leukotrienes (cysLTs) are bronchoconstricting lipid mediators that amplify eosinophilic airway inflammation by incompletely understood mechanisms. We recently found that leukotriene C4 (LTC4), the parent cysLT, potently activates platelets in vitro and induces airway eosinophilia in allergen sensitized and challenged mice by a platelet- and type 2 cysLT receptor (CysLT2R)-dependent pathway. We now demonstrate that this pathway requires production of thromboxane A2 (TXA2) and signaling through both hematopoietic and lung tissue-associated T prostanoid (TP) receptors. Intranasal administration of LTC4 to ovalbumin (OVA) sensitized C57BL/6 mice markedly increased the numbers of eosinophils in the bronchoalveolar lavage (BAL) fluid, while simultaneously decreasing the percentages of eosinophils in the blood by a TP receptor-dependent mechanism. LTC4 upregulated the expressions of intracellular adhesion molecule-1 (ICAM)-1 and vascular cell adhesion molecule (VCAM)-1 in an aspirin-sensitive and TP receptor-dependent manner. Both hematopoietic and non-hematopoietic TP receptors were essential for LTC4 to induce eosinophil recruitment. Thus, the autocrine and paracrine functions of TXA2 act downstream of LTC4/CysLT2R signaling on platelets to markedly amplify eosinophil recruitment through pulmonary vascular adhesion pathways. The findings suggest applications for TP receptor antagonists in cases of asthma with high levels of cysLT production.
Introduction
Cysteinyl leukotrienes (cysLTs) are a class of potent inflammatory mediators derived from arachidonic acid that is metabolized by myeloid cells expressing 5-lipoxygenase (5-LO) and LTC4 synthase (LTC4S) (1). LTC4, the short-lived parent of the cysLTs, is transported across the plasma membrane, and converted extracellularly to LTD4 by enzymatic removal of a glutamic acid residue (2). LTD4, a potent smooth muscle spasmogen, is rapidly metabolized to LTE4 by removal of glycine (3). Circulating eosinophils, basophils, and monocytes, as well as tissue-associated mast cells, dendritic cells and macrophages all generate LTC4 in response to activation. In inflammatory foci, cysLTs are detectable with a relative abundance of LTE4>LTC4>>LTD4, reflecting differences in biologic half-lives (4). CysLTs mediate smooth muscle constriction (5), vascular leakage (6), and inflammatory cell recruitment (7). They are established therapeutic targets in asthma (8) and potential targets in cardiovascular disease (9). While LTD4 and LTE4 are extracellular metabolites that diffuse through the fluid phase before binding their receptors, LTC4 may function at close range between the cells of origin and its targets after its transport to the cell surface and before its conversion to LTD4.
CysLTs bind and activate at least three G protein coupled receptors (GPCRs), termed the types 1 and 2 cysLT receptors (CysLT1R (10) and CysLT2R (11), respectively), and GPR99 (12). CysLT1R preferentially binds LTD4 over LTC4; CysLT2R binds LTC4 and LTD4 with equal affinity; and GPR99 exhibits preferential binding of LTE4. Both hematopoietic and non-hematopoietic cells express these three receptors in various combinations. Mice lacking LTC4S are markedly protected from the development of eosinophilic pulmonary inflammation (13,14), a hallmark of asthma, but not all of the relevant cell targets of cysLTs are known. Studies using receptor null mice reveal that each cysLT serves highly ligand- and cell target-specific functions in innate immunity and allergic inflammation (12,15,16). Drugs that block CysLT1R are modestly efficacious in the treatment of asthma (17), but there are no data on the effects of blocking CysLT2R or GPR99 in human disease. Preclinical models are essential to understand the contributions from these other receptors to disease pathophysiology in order to determine whether they are potential therapeutic targets.
In addition to their role in hemostasis, activated platelets bind via P-selectin to circulating granulocytes, particularly to eosinophils, in inflammatory disease states (18). This binding enhances the expression and avidity of both β1 and β2 integrins on eosinophils (18,19), which facilitates firm adhesion to intracellular adhesion molecule (ICAM)-1 and vascular cell adhesion molecule (VCAM)-1. Hence, platelets, like cysLTs, can amplify eosinophil recruitment to the lung in mouse models of allergen-induced pulmonary inflammation (20). Platelets also express CysLT1R and CysLT2R (21), suggesting that their functions may be influenced by cysLTs. We recently discovered that LTC4, but not LTD4 or LTE4, potently induced platelet P-selectin expression, the release of the granule-associated chemokine CXCL7, and the generation of thromboxane A2 (TXA2) entirely by signaling through CysLT2R (22). Furthermore, in a model of eosinophilic pulmonary inflammation induced by the inhalation of low-dose ovalbumin (OVA) by sensitized mice, intranasal administration of LTC4 markedly (∼10-fold) increased the numbers and percentages of eosinophils recovered from the bronchoalveolar lavage fluid by a CysLT2R and platelet-dependent pathway. Because of the potential pathobiologic significance of this pathway in eosinophilic inflammation, we sought to understand the mechanisms by which LTC4 amplifies eosinophilic inflammation in this model. We now report that platelet-derived TXA2 and its T prostanoid (TP) receptor are central to the amplification of pulmonary eosinophilia by LTC4, revealing potential therapeutic targets.
Materials and Methods
Animals
All animal protocols were approved by the Dana Farber Cancer Institute Animal Care and Utilization Committee. Tbxar-/- (TP receptor-null) mice were obtained from Dr. Thomas Coffman (Duke University, Durham, NC) (23). WT C57BL/6 mice were purchased from Charles River. Animals were housed for at least 2 weeks at the Smith Building before experiments were done.
Reagents
Ovalbumin and PBS were obtained from Sigma-Aldrich (St. Louis, MO). ELISA kits for thromboxane B2 and prostaglandins were purchased from Cayman Chemical (Ann Arbor, MI). The ELISA kit for mouse CXCL7 was from Abcam (Cambridge, MA). Goat anti-mouse ICAM-1 and Goat anti-mouse VCAM-1 antibodies were purchased from R&D Systems (Minneapolis, MN). Rabbit anti-mouse GAPDH was from Cell Signaling (Danvers, MA).
Immunization and challenge
The mice were sensitized i.p. on days 0 and 5 with Alum-precipitated chicken egg OVA (10 µg). On days 16-18, the mice received intranasal challenge of 2.2 nmol LTC4 or vehicle. On days 17-19, mice were challenged by inhalation of 0.1% OVA (22,24). In some experiments, the mice received 1 mg/ml lysine-aspirin (Lys-ASA) in drinking water from day 15 to day 20. Twenty-four hours after the final OVA aerosol challenge, the mice were euthanized and exsanguinated. The lungs were lavaged three times with 0.7 ml PBS/5 mM EDTA. Bronchoalveolar lavage (BAL) fluid cells were cytocentrifuged onto slides, stained with Diff-Quick (Fisher Diagnostics, Middletown, VA), and differentially counted. In some experiments, the selective TP receptor antagonist SQ 29,548 was injected to mice each day (2 mg/kg of body weight, intraperitoneal), or lysine aspirin (1 mg/ml) was added to the drinking water during the period of LTC4 challenge.
Flow cytometry
Whole heparinized blood obtained by cardiac puncture was kept at room temperature, and assayed within 1 hour of collection. 10μL of unstimulated blood was incubated with directly conjugated antibodies specific for CD41 and CD45, or appropriate isotype controls (all antibodies from BD Biosciences, San Jose CA) for 20 minutes and fixed in 1% paraformaldehyde. At least 20,000 CD45+ cells were recorded for each sample on a BD FACSAria™ Flow Cytometer and were analyzed with FlowJo (Tree Star, Ashland, OR). CD45+ leukocytes were classified as eosinophils or neutrophils according to their known scatter characteristics, relative autofluorescence, and levels of CD45 expression. They were assessed for the presence of adherent platelets by relative expression of CD41.
SDS PAGE immunoblotting
Lung protein was extracted with T-PER tissue protein extraction reagent (Thermo Fisher Scientific, Rockford, IL), Lysates were subjected to 12% SDS-PAGE and transferred to PVDF membranes. The membranes were incubated with antibodies against ICAM-1, VCAM-1 and GAPDH in PBS, 5% dry milk, and 0.1% Tween-20 (1:1,000) overnight at 4°C on shaker and then with secondary antibody (peroxidase-conjugated anti–goat or anti–rabbit). Bands were visualized with enhanced chemiluminescence (Thermo Fisher Scientific).
Bone marrow transfer
Five-week old sex-matched WT and tbxar-/- mice were lethally irradiated with 1200 Rads (12 Gy) in 2 split doses, 4 hours apart. Within 24 hours from the irradiation the bone marrow of WT and tbxar-/- donors were collected and 1×107 nucleated cells were infused via the tail vein into sex-matched irradiated mice in 200 µl of PBS. As a result of the bone marrow transfer, four groups of chimeric mice were generated: WT bone marrow into WT mice (WT → WT), WT → tbxar-/-, tbxar-/- → WT, and tbxar-/- → tbxar-/-. Ten weeks after the injection, mice were exposed to OVA and saline or LTC4 sensitization/challenge according to the same protocol used above and euthanized 24 hours after the last challenge. Peripheral blood cell counts were performed before the beginning of treatment to ensure full engraftment.
Immunohistology
Lung tissue was fixed in 10% neutral buffered formalin and embedded in paraffin. Tissue sections were incubated with rabbit anti-VCAM-1 (Santa Cruz Biotechnology Ab H-276/sc8304) or non-immune rabbit IgG, and bound Abs were visualized with Dako EnVision+System-HRP and AEC chromogen (3-amino-9-ethylcarbazole). Other sections were incubated with rat anti-ICAM-1 mAb (Biolegend clone YN1/1.7.4) or isotype control, and bound Abs were visualized with the Rat on Mouse HRP-Polymer system (Biocare Medical) and diaminobenzidine. Platelets were visualized with rabbit IgG anti-mouse CD41 (Ab H-160; Santa Cruz Biotechnology) or nonimmune rabbit IgG for 1 h at room temperature. Ab binding was visualized with an avidin-biotin complex (Santa Cruz Biotechnology)(25). All sections were counterstained with Gill's hematoxylin #2.
Statistical analysis
Data are expressed as ±SEM from at least 10 mice from at least two experiments, except where otherwise indicated. Analyses were performed with Prism software (Graphpad). Differences between two treatment groups were assessed using Student t test, and differences among multiple groups were assessed using one-way ANOVA and Bonferroni post hoc test. P<0.05 was considered statistically significant. * p<0.05, ** p<0.01, *** p<0.001.
Results
Intrapulmonary LTC4 challenges induce the release of platelet-derived products in vivo
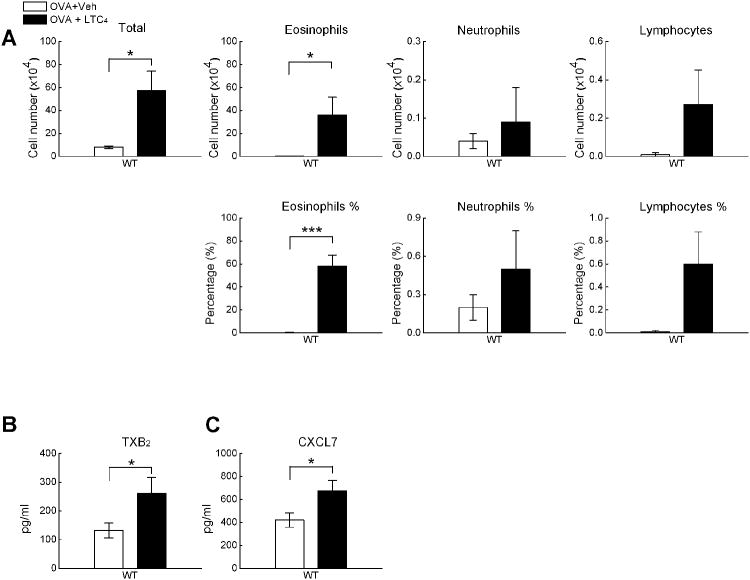
To determine whether LTC4 directly activated platelets in the lung, WT C57BL/6 mice were sensitized with OVA intraperitoneally on days 0 and 5, then challenged with 0.1% OVA on days 18-20 for 30 min each day. Twelve hours before each OVA challenge, mice received intranasal LTC4 or a buffer control. Twenty four hours after the last OVA challenge, mice were euthanized, BAL fluid was collected, and the lungs were analyzed histologically. Compared with BAL fluid from the mice that received OVA + vehicle, the BAL fluid from the mice receiving OVA + LTC4 contained significantly higher numbers and percentages of eosinophils (Fig. 1A), as well as increased numbers and percentages of neutrophils and lymphocytes (though at much lower levels than eosinophils, not shown). BAL fluid from LTC4-treated mice also contained higher levels of TXB2 (a stable metabolite of TXA2) and the platelet-derived chemokine CXCL7 (Fig. 1B and 1C, respectively) than did BAL fluid from mice challenged with OVA alone. Histologic exam verified that LTC4 treated mice had substantially more bronchovascular cellular infiltrates and goblet cell metaplasia than did mice challenged with OVA alone (not shown). Immunohistology revealed CD41+ platelets in the bronchial submucosa of the OVA-treated mice that appeared more prominent in the lungs of the LTC4-treated mice than in those challenged with OVA alone (Supplemental Fig. 1). In the absence of OVA inhalaton, challenge of sensitized mice with LTC4 did not elicit any cellular influx (Supplemental Fig. 2).
Figure 1.
Effect of LTC4 on eosinophilic pulmonary inflammation and platelet activation. OVA-sensitized C57BL/6 were challenged with 0.1% OVA on three successive days, with or without inhalation of LTC4 (2.2 nmol) 12 h before each challenge. BAL fluid was collected 24 h after the last OVA challenge. A. Total cell counts, total eosinophils, and percentage of eosinophils and in BAL fluids. B. Levels of TXB2 in BAL fluid lipid fractions. C. Levels of BAL fluid CXCL7. Results in A-C are from ten mice/group from two separate experiments. * p<0.05, *** p<0.001.
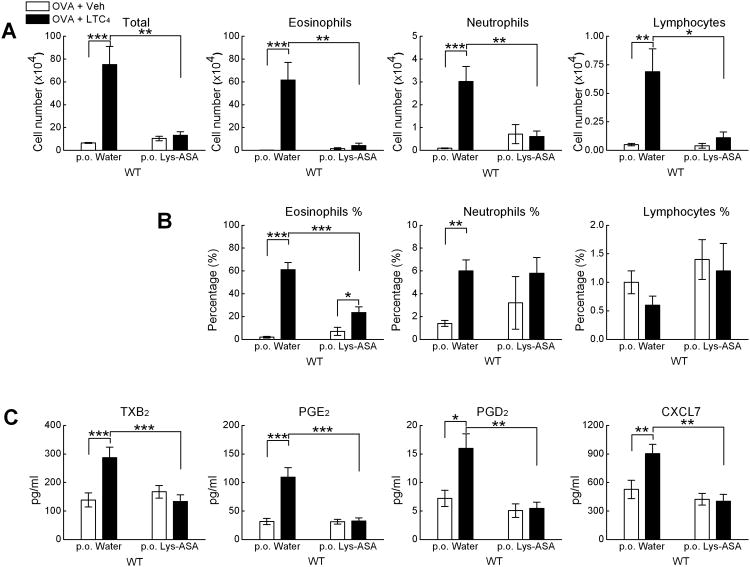
Potentiation of lung eosinophilia by LTC4 is sensitive to treatment with aspirin
To determine whether the potentiation of lung eosinophilia in response to LTC4 involved contributions from cyclooxygenase (COX) pathway products, mice received aspirin in their drinking water from day 15 (one day before the first dose of LTC4) today 21 (the day of euthanasia). BAL fluids were collected for cell counts, differentials, and mediator measurements. Compared with the mice not receiving aspirin, the aspirin-treated mice showed markedly diminished LTC4-induced increases in total cells, eosinophils, neutrophils, and lymphocytes (Fig. 2A). The percentages of eosinophils and neutrophils remained higher in the LTC4-challenged aspirin treated group than in the group challenged with OVA alone, although the percentages of eosinophils decreased by more than 50% (Fig. 2B). Treatment with aspirin eliminated LTC4-induced increments in TXB2, PGD2, and PGE2 elicited by LTC4 (Fig. 2C). Treatment with aspirin also reduced the levels of CXCL7 detected in the BAL fluids of the LTC4-treated mice (Fig. 2C).
Figure 2.
Effect of aspirin on LTC4-induced pulmonary inflammation. Sensitized and challenged mice were treated with Lysine aspirin (1 mg/ml in drinking water) or water alone for 5 d before collection of BAL fluid. A. Numbers of total cells, eosinophils, neutrophils and lymphocytes in BAL fluids. B. Percentages of neutrophils and eosinophils in BAL fluid. C. Prostaglandins in BAL fluid lipid fractions and BAL fluid levels of CXCL7. Results in A-C are from ten mice/group from two separate experiments. * p<0.05, ** p<0.01, *** p<0.001.
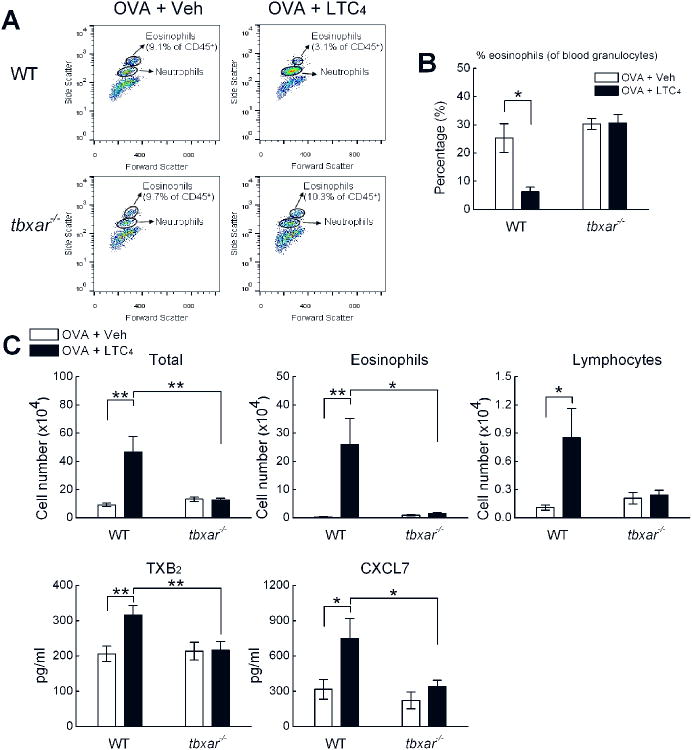
Eosinophil recruitment in response to LTC4 is eliminated by the absence of TP receptors
To determine whether TXA2 and its receptor contributed directly to the recruitment of eosinophils to the lung in response to LTC4, WT and tbxar-/- mice were sensitized with OVA and challenged with OVA with or without LTC4. We simultaneously monitored the BAL fluid for total and differential cell counts, and monitored the peripheral blood for both total and platelet-adherent eosinophils and neutrophils. WT mice and tbxar-/- mice had similar BAL fluid cell counts and differentials following challenges with OVA alone (Fig. 3A). The percentages of peripheral blood CD45+ cells that were eosinophils (based on light scatter, as shown in Fig. 3A), and the fractions of the eosinophils with adherent platelets based on CD41 staining (not shown) were similar in the OVA-treated WT and tbxar-/- mice, respectively (3B). LTC4 challenge sharply decreased the percentages of CD45+ cells that were eosinophils (from 9.1 ± 2.0 to 3.1 ± 0.7%), but had no effect in the tbxar-/- mice (from 9.7 ± 0.4 to 11.3 ± 1.7%) (Fig. 3B, as shown for representative samples, Fig. 3A). LTC4 challenge also tended to decrease the percentages of blood eosinophils that were platelet-adherent (from 31.0 ± 7.4 to 19 ± 4.7%) in the WT mice, but not in the tbxar-/- mice (from 26.6 ± 0.8 to 26.0 ± 2.0%, not shown). LTC4-challenged tbxar-/- mice were nearly completely protected from the increases in BAL fluid total cells, eosinophils, neutrophils, and lymphocytes induced by LTC4 (Fig. 3C). The increases in BAL fluid levels of TXB2 and of CXCL7 induced by LTC4 were blunted in the tbxar-/- mice (Fig. 3C). Treatment of the LTC4-challenged mice with a single IP dose of the selective TP receptor antagonist SQ29.548 markedly suppressed the induction of pulmonary eosinophilia by LTC4 (Supplemental Fig. 3).
Figure 3.
Effect of TP receptor deletion on LTC4-mediated eosinophil recruitment to the lung. A. Cytofluorographic detection of eosinophils and neutrophils (based on light scatter characteristics within the CD45+ gate) in the blood of representative C57BL/6 WT and tbxar-/- mice challenged with OVA alone or OVA + LTC4. B. Percentages of blood granulocytes identified as eosinophils from the same groups of mice. C. Total BAL fluid cells, eosinophils, and lymphocytes from sensitized WT and tbxar-/- mice challenged with OVA with or without LTC4. BAL fluid levels of TXB2 and CXCL7 are shown from the same mice. Results in A-C are from 10 mice/group from two separate experiments. * p<0.05, ** p<0.01.
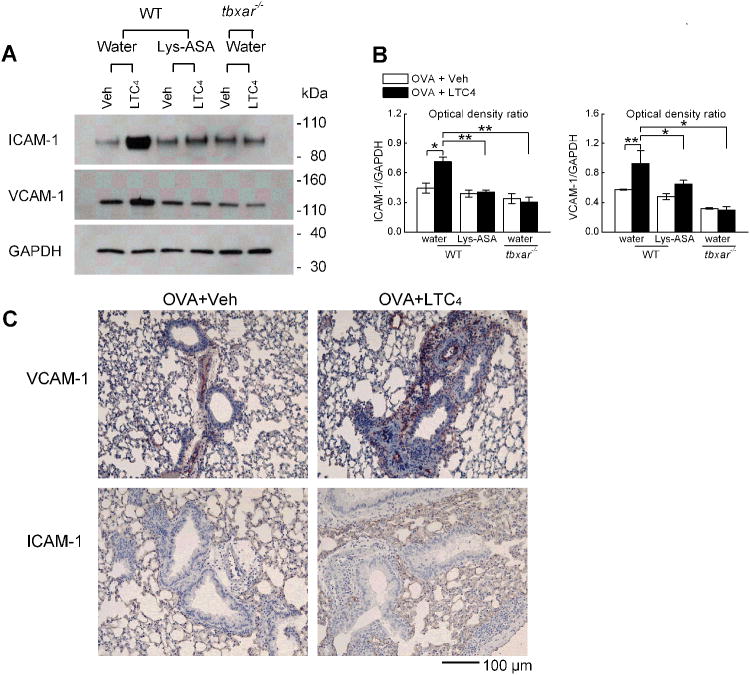
Inductions of ICAM-1 and VCAM-1 by LTC4 are sensitive to aspirin and depend on TP receptors
To determine whether the administration of LTC4 induced the expressions of endothelial cell adhesion molecules in the lung, whole lung homogenates were used to generate western blots. Compared to the lungs of WT mice treated with OVA without LTC4, the lungs of LTC4-treated WT mice expressed higher levels of both ICAM-1 and VCAM-1 proteins (Fig. 4A, 4B). These LTC4-mediated increases were completely abrogated in the lungs of mice treated with aspirin, and were absent in the lungs of LTC4-treated tbxar-/- mice. Neither treatment with aspirin nor deletion of TP receptors altered the baseline levels of ICAM-1 or VCAM-1 proteins expressed in response to OVA alone. Immunohistochemistry revealed stronger staining for both VCAM-1 and ICAM-1 proteins in the lungs of mice treated with OVA + LTC4 than those treated with OVA alone. VCAM-1 staining localized to both venules and arterioles in the vicinity of the endothelium, whereas ICAM-1 staining localized to the alveolar walls as well as venules (Fig. 4C).
Figure 4.
LTC4-mediated upregulation of pulmonary ICAM-1 and VCAM-1 proteins. Lysates were prepared from whole lung of the indicated strains of sensitized mice obtained 24 h after challenge with OVA with or without LTC4. Some mice received aspirin in their drinking water. A. Western blots showing ICAM-1, VCAM-1, and GAPDH from the lungs of representative mice. B. Quantitative densitometry from the lungs of 5 mice/group. C. Immunohistochemical stains of lungs of representative OVA-sensitized mice challenged with low dose OVA either with vehicle or with LTC4. * p<0.05, ** p<0.01.
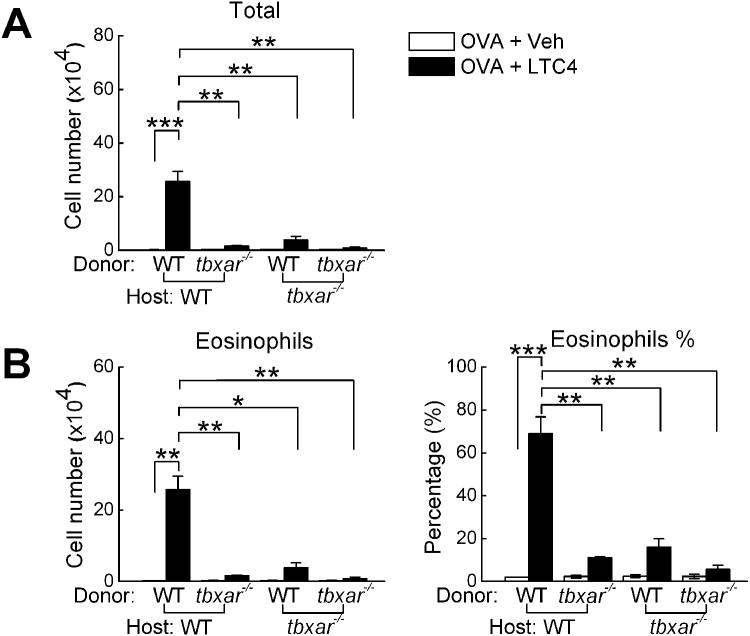
LTC4-induced lung eosinophil recruitment requires both hematopoietic and non-hematopoietic TP receptor expression
To determine the most critical anatomic sites of TP receptor expression necessary for the amplifying effect of LTC4 on eosinophil recruitment, lethally irradiated WT and tbxar-/- mice were engrafted with WT or tbxar-/- bone marrow. The resultant chimeric mice were then sensitized and challenged with OVA with or without the administration of intranasal LTC4. Compared with WT hosts receiving WT marrow, tbxar-/- mice receiving tbxar-/- marrow demonstrated a markedly blunted response to LTC4. Both the respective chimeric strains lacking only hematopoietic TP receptors and lacking only host tissue TP receptors also displayed dramatic reductions in BAL fluid total cell and eosinophil counts compared with the WT + WT mice (Fig. 5). Blood counts on the engrafted mice revealed complete restoration of all lineages (not shown).
Figure 5.
Contributions from hematopoietic and non-hematopoietic TP receptors to LTC4-induced pulmonary inflammation. Lethally irradiated mice from the indicated recipient strains received bone marrow cells from the indicated donors. Ten weeks later, the mice were sensitized and challenged with OVA with or without LTC4. A. Total BAL fluid cell counts and B. BAL eosinophil counts and percentages are displayed for 5 mice in each group. * p<0.05, ** p<0.01, *** p<0.001.
Discussion
Although cysLTs were initially recognized for their contractile effects on smooth muscle, they are also inducers and amplifiers of a range of immune and inflammatory responses. CysLT production is a consistent feature of the eosinophilic airway inflammation that is typical of asthma. This is especially true of aspirin exacerbated respiratory disease (AERD), a syndrome in which severe eosinophilic airway inflammation, asthma, sinonasal disease and respiratory reactions to nonselective cyclooxygenase inhibitors are accompanied by markedly elevated levels of cysLT generation (26). AERD is also associated with markedly increased numbers of platelet-adherent eosinophils in the blood and tissue (19). Although antagonists of CysLT1R can blunt the severity of clinical reactions to aspirin in AERD (27) and reduce exacerbation frequency in asthma in general (17), their effects are modest and they do not affect airway inflammation, suggesting that additional cysLT receptors and downstream effectors are involved. We had previously reported that LTC4, administered at a dose (2.2. nmol) equivalent to the maximally efficacious dose of LTE4 in a similar model, far exceeded the potency of its metabolites for amplifying eosinophilic inflammation in C57BL/6 mice challenged with 0.1% OVA (a dose that elicits minimal inflammation (28) with minimal/negligible contributions from endogenous cysLTs (24,29)). These effects were strikingly platelet- and CysLT2R-dependent (29). We therefore sought to better understand the mechanisms by which LTC4, CysLT2R, and platelets facilitated eosinophilic inflammation in this model.
In addition to priming leukocyte adhesion pathways by P selectin-dependent adherence to eosinophils and other leukocytes (20), platelets contain preformed mediators such as chemokines, and generate COX-1-derived lipid mediators that can amplify inflammation. The sharp increments in lung eosinophils induced by intrapulmonary LTC4 in our model (Fig. 1A) were accompanied by increases in TXB2 (a stable metabolite of TXA2, the dominant COX product of platelets) (Fig. 1B), CXCL7 (a platelet-derived chemokine) (Fig. 1C). Intrapulmonary platelets were present in the bronchial submucosa of OVA-challenged mice, both with and without LTC4 inhalation (Supplemental Fig. 1), suggesting that LTC4 directly activated platelets that had been recruited to the lung in response to allergen, as demonstrated in previous studies (30). LTC4 did not induce pulmonary eosinophilia on its own (Supplemental Fig. 2), indicating that chemotactic or viability-sustaining factors induced by the immune response to OVA are required for LTC4 to amplify cell recruitment. Because platelets are both sources and responders to effector COX products, we next focused on the potential role of TXA2 (and potentially other COX products) in our model.
Aspirin suppresses TXA2 formation and platelet function sufficiently to induce vasoprotection in studies of cardiovascular disease (31). Aspirin also provokes clinical reactions in AERD that reflect depletion of bronchoprotective prostaglandins such as PGE2 (32,33) due to a deficit in COX-2, a largely aspirin-resistant enzyme (34). Subsequently, aspirin induces desensitization and substantial clinical benefit by unknown mechanisms (35). We found that treatment of the mice with aspirin markedly suppressed LTC4-induced potentiation of airway eosinophilia and neutrophilia (Fig. 2A), as well as the percentages of eosinophils but not of neutrophils (Fig. 2B). Concomitantly, aspirin markedly suppressed the formation of TXA2 (as indicated by TXB2 concentrations), PGD2 (a product of both platelets and mast cells, Fig. 2C), and PGE2 (a product of epithelial cells and macrophages) (Fig. 2C). The increases in all three prostaglandins by LTC4 suggest that this ligand activates both platelets and additional cellular targets in this model. The suppression of CXCL7 generation by aspirin (Fig. 2C) likely reflects a loss of autocrine functions of TXA2 on platelet activation. The capacity of TXA2 and TP receptor signaling to facilitate lung inflammation in other models (36,37) led us to focus on whether TXA2 might drive LTC4-induced eosinophil accumulation using transgenic and pharmacologic approaches.
Eosinophils represent a small fraction of circulating granulocytes, but are recruited to sites of allergic inflammation in a highly selective manner. Platelets adhere to blood eosinophils with high frequency in asthma (18), and even higher in AERD (up to 80% of peripheral blood eosinophils with adherent platelets) (19), where they accumulate in large numbers in the respiratory tissues. Since it is plausible that platelet-derived TXA2 could stimulate endothelial TP receptors to facilitate the entry of eosinophils (particularly those adherent to platelets) to the tissue, we sought to determine the role of TP receptors on LTC4-induced eosinophil recruitment in our model. While the absence of TP receptors did not alter the blood eosinophil counts or the fraction of eosinophils with adherent platelets in the OVA-treated mice, the TP receptor deficient mice were completely protected from the LTC4-induced decreases in blood eosinophils (Fig. 3A, 3B) and concomitant increases in BAL fluid eosinophil counts and platelet-derived mediators (Fig. 3C). Similarly, the TP receptor antagonist markedly decreased total BAL fluid cells and eosinophils when administered during the period of LTC4 challenges (Supplemental Fig. 3). Thus, TP receptor signaling is not required for the intravascular formation of platelet-eosinophil complexes, but is absolutely required for these complexes to be recruited to the respiratory tissues and activated in response to LTC4.
While TP receptors on platelets permit autocrine TXA2-mediated amplification of platelet activation, TP receptors on endothelial cells mediate TXA2-dependent upregulation of adhesion receptors (36,37). The lungs of WT mice treated with LTC4 before OVA challenge expressed significantly higher levels of ICAM-1 and VCAM-1 proteins than did the lungs of mice treated with OVA alone. This induction was absent in both the aspirin-treated mice and in the tbxar-/- mice (Fig. 4). The TXA2/TP-dependent upregulation of ICAM-1 and VCAM-1 likely facilitates adhesion synergistically with platelet-dependent upregulation of β1 and β2 integrins on human and mouse eosinophils previously reported by our group and others (18,19). Whereas the ICAM-1/β2 integrin pathway facilitates the adhesion of all leukocytes, the VCAM-1/β1 pathway is selective for eosinophil recruitment (38), and may explain the dominance of the eosinophilic response to LTC4 in our model. The fact that both non-hematopoietic and hematopoietic TP receptors are essential in this pathway (Fig. 5) suggests that both the autocrine and paracrine functions of platelet-derived TXA2 are necessary for LTC4 to elicit eosinophil recruitment. Since LTC4 is the only cysLT that induces this pathway (29), it is tempting to speculate that platelet activation and TXA2 formation may occur while the platelet contacts the granulocyte immediately after LTC4 is released and before it is enzymatically converted to LTD4. Given that LTC4 and TXA2 are both short-lived in vivo, rapid and successive activation of CysLT2R (on intrapulmonary platelets) and TP receptors (on platelets and endothelial cells) is likely to be followed by gene induction events (including the induced expression of adhesion molecules) that permit subsequent leukocyte recruitment to occur over several hours.
While our previous study demonstrated that LTC4 targeted CysLT2R on platelets to induce inflammation, our present findings indicate that platelet-derived COX products (specifically TXA2) are critical for this CysLT2R-mediated pathway. TP receptor antagonists improved lung function and reduced the numbers of activated eosinophils in bronchial biopsies in controlled studies of subjects with mild asthma (39,40). It is possible that TP receptor antagonism may be especially efficacious in AERD, where platelet-dependent amplification of inflammation may be prominent due to the high levels of cysLT generation that is characteristic of this disease (19). The therapeutic effect of aspirin desensitization followed by high dose aspirin in AERD is not accompanied by a reduction in the high levels of cysLT generation, but rather by markedly suppressed TXA2 (and PGD2) production (41). We therefore suspect that aspirin therapy uncouples LTC4 from its downstream COX-derived effectors as part of its therapeutic mechanism. Finally, the capacity for LTC4 to activate platelets and elicit endothelial activation via TXA2 may be relevant to the role of cysLTs in cardiovascular disease (42), in which animal models strongly support the role of CysLT2R (43).
Supplementary Material
Footnotes
This work was supported by generous contributions from the Vinik Family and National Institutes of Health Grants AI078908, AI095219, AT002782, AI082369, HL111113, HL117945, and HL36110.
References
- 1.Lam BK, Penrose JF, Freeman GJ, Austen KF. Expression cloning of a cDNA for human leukotriene C4 synthase, an integral membrane protein conjugating reduced glutathione to leukotriene A4. Proc Natl Acad Sci U S A. 1994;91:7663–7667. doi: 10.1073/pnas.91.16.7663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carter BZ, Shi ZZ, Barrios R, Lieberman MW. gamma-glutamyl leukotrienase, a gamma-glutamyl transpeptidase gene family member, is expressed primarily in spleen. J Biol Chem. 1998;273:28277–28285. doi: 10.1074/jbc.273.43.28277. [DOI] [PubMed] [Google Scholar]
- 3.Lee CW, Lewis RA, Corey EJ, Austen KF. Conversion of leukotriene D4 to leukotriene E4 by a dipeptidase released from the specific granule of human polymorphonuclear leucocytes. Immunology. 1983;48:27–35. [PMC free article] [PubMed] [Google Scholar]
- 4.Austen KF, Maekawa A, Kanaoka Y, Boyce JA. The leukotriene E4 puzzle: finding the missing pieces and revealing the pathobiologic implications. J Allergy Clin Immunol. 2009;124:406–414. doi: 10.1016/j.jaci.2009.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weiss JW, Drazen JM, Coles N, McFadden ER, Jr, Weller PF, Corey EJ, Lewis RA, Austen KF. Bronchoconstrictor effects of leukotriene C in humans. Science. 1982;216:196–198. doi: 10.1126/science.7063880. [DOI] [PubMed] [Google Scholar]
- 6.Soter NA, Lewis RA, Corey EJ, Austen KF. Local effects of synthetic leukotrienes (LTC4, LTD4, LTE4, and LTB4) in human skin. J Invest Dermatol. 1983;80:115–119. doi: 10.1111/1523-1747.ep12531738. [DOI] [PubMed] [Google Scholar]
- 7.Gauvreau GM, Parameswaran KN, Watson RM, O'Byrne PM. Inhaled leukotriene E(4), but not leukotriene D(4), increased airway inflammatory cells in subjects with atopic asthma. Am J Respir Crit Care Med. 2001;164:1495–1500. doi: 10.1164/ajrccm.164.8.2102033. [DOI] [PubMed] [Google Scholar]
- 8.Israel E, Cohn J, Dube L, Drazen JM. Effect of treatment with zileuton, a 5-lipoxygenase inhibitor, in patients with asthma. A randomized controlled trial Zileuton Clinical Trial Group. JAMA. 1996;275:931–936. [PubMed] [Google Scholar]
- 9.Di GA, Wagsater D, Mayranpaa MI, Gabrielsen A, Swedenborg J, Hamsten A, Samuelsson B, Eriksson P, Haeggstrom JZ. Increased expression of leukotriene C4 synthase and predominant formation of cysteinyl-leukotrienes in human abdominal aortic aneurysm. Proc Natl Acad Sci U S A. 2010;107:21093–21097. doi: 10.1073/pnas.1015166107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lynch KR, O'Neill GP, Liu Q, Im DS, Sawyer N, Metters KM, Coulombe N, Abramovitz M, Figueroa DJ, Zeng Z, Connolly BM, Bai C, Austin CP, Chateauneuf A, Stocco R, Greig GM, Kargman S, Hooks SB, Hosfield E, Williams DL, Jr, Ford-Hutchinson AW, Caskey CT, Evans JF. Characterization of the human cysteinyl leukotriene CysLT1 receptor. Nature. 1999;399:789–793. doi: 10.1038/21658. [DOI] [PubMed] [Google Scholar]
- 11.Heise CE, O'Dowd BF, Figueroa DJ, Sawyer N, Nguyen T, Im DS, Stocco R, Bellefeuille JN, Abramovitz M, Cheng R, Williams DL, Jr, Zeng Z, Liu Q, Ma L, Clements MK, Coulombe N, Liu Y, Austin CP, George SR, O'Neill GP, Metters KM, Lynch KR, Evans JF. Characterization of the human cysteinyl leukotriene 2 receptor. J Biol Chem. 2000;275:30531–30536. doi: 10.1074/jbc.M003490200. [DOI] [PubMed] [Google Scholar]
- 12.Kanaoka Y, Maekawa A, Austen KF. Identification of GPR99 protein as a potential third cysteinyl leukotriene receptor with a preference for leukotriene E4 ligand. J Biol Chem. 2013;288:10967–10972. doi: 10.1074/jbc.C113.453704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barrett NA, Rahman OM, Fernandez JM, Parsons MW, Xing W, Austen KF, Kanaoka Y. Dectin-2 mediates Th2 immunity through the generation of cysteinyl leukotrienes. J Exp Med. 2011;208:593–604. doi: 10.1084/jem.20100793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim DC, Hsu FI, Barrett NA, Friend DS, Grenningloh R, Ho IC, AlGarawi A, Lora JM, Lam BK, Austen KF, Kanaoka Y. Cysteinyl leukotrienes regulate Th2 cell-dependent pulmonary inflammation. J Immunol. 2006;176:4440–4448. doi: 10.4049/jimmunol.176.7.4440. [DOI] [PubMed] [Google Scholar]
- 15.Beller TC, Maekawa A, Friend DS, Austen KF, Kanaoka Y. Targeted gene disruption reveals the role of the cysteinyl leukotriene 2 receptor in increased vascular permeability and in bleomycin-induced pulmonary fibrosis in mice. J Biol Chem. 2004;279:46129–46134. doi: 10.1074/jbc.M407057200. [DOI] [PubMed] [Google Scholar]
- 16.Maekawa A, Austen KF, Kanaoka Y. Targeted gene disruption reveals the role of cysteinyl leukotriene 1 receptor in the enhanced vascular permeability of mice undergoing acute inflammatory responses. J Biol Chem. 2002;277:20820–20824. doi: 10.1074/jbc.M203163200. [DOI] [PubMed] [Google Scholar]
- 17.Israel E, Chervinsky PS, Friedman B, Van BJ, Skalky CS, Ghannam AF, Bird SR, Edelman JM. Effects of montelukast and beclomethasone on airway function and asthma control. J Allergy Clin Immunol. 2002;110:847–854. doi: 10.1067/mai.2002.129413. [DOI] [PubMed] [Google Scholar]
- 18.Johansson MW, Han ST, Gunderson KA, Busse WW, Jarjour NN, Mosher DF. Platelet activation, P-selectin, and eosinophil beta1-integrin activation in asthma. Am J Respir Crit Care Med. 2012;185:498–507. doi: 10.1164/rccm.201109-1712OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laidlaw TM, Kidder MS, Bhattacharyya N, Xing W, Shen S, Milne GL, Castells MC, Chhay H, Boyce JA. Cysteinyl leukotriene overproduction in aspirin-exacerbated respiratory disease is driven by platelet-adherent leukocytes. Blood. 2012;119:3790–3798. doi: 10.1182/blood-2011-10-384826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pitchford SC, Momi S, Giannini S, Casali L, Spina D, Page CP, Gresele P. Platelet P-selectin is required for pulmonary eosinophil and lymphocyte recruitment in a murine model of allergic inflammation. Blood. 2005;105:2074–2081. doi: 10.1182/blood-2004-06-2282. [DOI] [PubMed] [Google Scholar]
- 21.Hasegawa S, Ichiyama T, Hashimoto K, Suzuki Y, Hirano R, Fukano R, Furukawa S. Functional expression of cysteinyl leukotriene receptors on human platelets. Platelets. 2010;21:253–259. doi: 10.3109/09537101003615394. [DOI] [PubMed] [Google Scholar]
- 22.Cummings HE, Liu T, Feng C, Laidlaw TM, Conley PB, Kanaoka Y, Boyce JA. Cutting edge: Leukotriene C4 activates mouse platelets in plasma exclusively through the type 2 cysteinyl leukotriene receptor. J Immunol. 2013;191:5807–5810. doi: 10.4049/jimmunol.1302187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas DW, Coffman TM. A genetic approach for studying the role of thromboxane A2 in the kidney. Kidney Int Suppl. 1998;67:S84–S87. doi: 10.1046/j.1523-1755.1998.06717.x. [DOI] [PubMed] [Google Scholar]
- 24.Paruchuri S, Tashimo H, Feng C, Maekawa A, Xing W, Jiang Y, Kanaoka Y, Conley P, Boyce JA. Leukotriene E4-induced pulmonary inflammation is mediated by the P2Y12 receptor. J Exp Med. 2009;206:2543–2555. doi: 10.1084/jem.20091240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu T, Laidlaw TM, Katz HR, Boyce JA. Prostaglandin E2 deficiency causes a phenotype of aspirin sensitivity that depends on platelets and cysteinyl leukotrienes. Proc Natl Acad Sci U S A. 2013 doi: 10.1073/pnas.1313185110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Laidlaw TM, Boyce JA. Pathogenesis of aspirin-exacerbated respiratory disease and reactions. Immunol Allergy Clin North Am. 2013;33:195–210. doi: 10.1016/j.iac.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White A, Ludington E, Mehra P, Stevenson DD, Simon RA. Effect of leukotriene modifier drugs on the safety of oral aspirin challenges. Ann Allergy Asthma Immunol. 2006;97:688–693. doi: 10.1016/S1081-1206(10)61101-5. [DOI] [PubMed] [Google Scholar]
- 28.Honda K, Arima M, Cheng G, Taki S, Hirata H, Eda F, Fukushima F, Yamaguchi B, Hatano M, Tokuhisa T, Fukuda T. Prostaglandin D2 reinforces Th2 type inflammatory responses of airways to low-dose antigen through bronchial expression of macrophage-derived chemokine. J Exp Med. 2003;198:533–543. doi: 10.1084/jem.20022218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cummings HE, Liu T, Feng C, Laidlaw TM, Conley PB, Kanaoka Y, Boyce JA. Cutting Edge: Leukotriene C4 Activates Mouse Platelets in Plasma Exclusively through the Type 2 Cysteinyl Leukotriene Receptor. J Immunol. 2013 doi: 10.4049/jimmunol.1302187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pitchford SC, Momi S, Baglioni S, Casali L, Giannini S, Rossi R, Page CP, Gresele P. Allergen induces the migration of platelets to lung tissue in allergic asthma. Am J Respir Crit Care Med. 2008;177:604–612. doi: 10.1164/rccm.200702-214OC. [DOI] [PubMed] [Google Scholar]
- 31.De CR, Giannessi D, Bernini W, Gazzetti P, Michelassi C, L'Abbate A, Donato L, Patrignani P, Filabozzi P, Patrono P. Low-dose aspirin in patients recovering from myocardial infarction. Evidence for a selective inhibition of thromboxane-related platelet function. Eur Heart J. 1985;6:409–417. doi: 10.1093/oxfordjournals.eurheartj.a061879. [DOI] [PubMed] [Google Scholar]
- 32.Szczeklik A, Gryglewski RJ, Olszewski E, Dembinska-Kiec A, Czerniawska-Mysik G. Aspirin-sensitive asthma: the effect of aspirin on the release of prostaglandins from nasal polyps. Pharmacol Res Commun. 1977;9:415–425. doi: 10.1016/s0031-6989(77)80027-1. [DOI] [PubMed] [Google Scholar]
- 33.Sestini P, Armetti L, Gambaro G, Pieroni MG, Refini RM, Sala A, Vaghi A, Folco GC, Bianco S, Robuschi M. Inhaled PGE2 prevents aspirin-induced bronchoconstriction and urinary LTE4 excretion in aspirin-sensitive asthma. Am J Respir Crit Care Med. 1996;153:572–575. doi: 10.1164/ajrccm.153.2.8564100. [DOI] [PubMed] [Google Scholar]
- 34.Picado C, Fernandez-Morata JC, Juan M, Roca-Ferrer J, Fuentes M, Xaubet A, Mullol J. Cyclooxygenase-2 mRNA is downexpressed in nasal polyps from aspirin-sensitive asthmatics. Am J Respir Crit Care Med. 1999;160:291–296. doi: 10.1164/ajrccm.160.1.9808048. [DOI] [PubMed] [Google Scholar]
- 35.Berges-Gimeno MP, Simon RA, Stevenson DD. Long-term treatment with aspirin desensitization in asthmatic patients with aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. 2003;111:180–186. doi: 10.1067/mai.2003.7. [DOI] [PubMed] [Google Scholar]
- 36.Zarbock A, Singbartl K, Ley K. Complete reversal of acid-induced acute lung injury by blocking of platelet-neutrophil aggregation. J Clin Invest. 2006;116:3211–3219. doi: 10.1172/JCI29499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu T, Laidlaw TM, Feng C, Xing W, Shen S, Milne GL, Boyce JA. Prostaglandin E2 deficiency uncovers a dominant role for thromboxane A2 in house dust mite-induced allergic pulmonary inflammation. Proc Natl Acad Sci U S A. 2012;109:12692–12697. doi: 10.1073/pnas.1207816109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yuan Q, Austen KF, Friend DS, Heidtman M, Boyce JA. Human peripheral blood eosinophils express a functional c-kit receptor for stem cell factor that stimulates very late antigen 4 (VLA-4)-mediated cell adhesion to fibronectin and vascular cell adhesion molecule 1 (VCAM-1) J Exp Med. 1997;186:313–323. doi: 10.1084/jem.186.2.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tamaoki J, Kondo M, Nakata J, Nagano Y, Isono K, Nagai A. Effect of a thromboxane A(2) antagonist on sputum production and its physicochemical properties in patients with mild to moderate asthma. Chest. 2000;118:73–79. doi: 10.1378/chest.118.1.73. [DOI] [PubMed] [Google Scholar]
- 40.Hoshino M, Sim J, Shimizu K, Nakayama H, Koya A. Effect of AA-2414, a thromboxane A2 receptor antagonist, on airway inflammation in subjects with asthma. J Allergy Clin Immunol. 1999;103:1054–1061. doi: 10.1016/s0091-6749(99)70179-x. [DOI] [PubMed] [Google Scholar]
- 41.Cahill KN, Bensko JC, Boyce JA, Laidlaw TM. Prostaglandin D2: A dominant mediator of aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. 2015;135:245–252. doi: 10.1016/j.jaci.2014.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ingelsson E, Yin L, Back M. Nationwide cohort study of the leukotriene receptor antagonist montelukast and incident or recurrent cardiovascular disease. J Allergy Clin Immunol. 2012;129:702–707. doi: 10.1016/j.jaci.2011.11.052. [DOI] [PubMed] [Google Scholar]
- 43.Ni NC, Yan D, Ballantyne LL, Barajas-Espinosa A, St AT, Pratt DA, Funk CD. A selective cysteinyl leukotriene receptor 2 antagonist blocks myocardial ischemia/reperfusion injury and vascular permeability in mice. J Pharmacol Exp Ther. 2011;339:768–778. doi: 10.1124/jpet.111.186031. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.