Abstract
[Purpose] The purpose of this study was to investigate the knee joint proprioception in weight-bearing (WB) and non-weight-bearing (NWB) positions and to study the difference between the methods in chronic stroke patients. [Subjects and Methods] The subjects were 15 stroke patients who were randomly scheduled to perform both positions by a physical therapist not involved in the study. The subjects performed the positions (WB and NWB) based on a randomized controlled cross-sectional design. WB subjects were positioned in one-leg standing to assess the knee joint position sense. NWB subjects were instructed to sit comfortably in a chair and maintain the knees at 90° of flexion with the leg out of the plinth. [Results] The results revealed that the WB position showed a significant difference in knee position sense. The proprioception sense in the WB position was a higher than that in the NWB position. [Conclusion] The knee proprioception of chronic stroke patients differs between the weight-bearing and non-weight-bearing positions.
Key words: Knee proprioception, Stroke, Weight bearing
INTRODUCTION
Stroke is accompanied by a decline in muscular strength, sensory perception, neuromuscular control, and balance, consequently increasing the risk to fall1, 2). These factors cause poor neuromuscular control and problems relating to proprioceptive sense3). Proprioceptive sense is considered an essential element for activities of daily living4, 5).
There are several methods of assessing joint proprioceptive sense3, 6, 7). Most joint proprioception assessments are used to evaluate the function of conscious joint position8). From an anatomic perspective, histologic studies can be conducted to identify mechanoreceptors within specific joint structures. Neurophysiological testing can measure the sensory threshold and nerve conduction velocities. Clinically, proprioceptive sense can be assessed by measuring the two components that make up the proprioceptive mechanism, namely, kinesthesia and joint position sense. Most studies have conducted testing knee proprioception with participants in a non-weight-bearing (NWB) position. In recent years, increasing numbers of authors have recommended a weight-bearing (WB) test for joint position sense, as weight-bearing tests are more functional and involve all of the cutaneous, articular, and muscular proprioceptors during activities of daily living9, 10). There have been few studies describing assessment of joint position sense by using functional WB protocols. In a study performed by Lokhande et al.11), the authors investigated the differences in reproducibility of knee joint angles in healthy subjects during a WB task performed while standing and an NWB task performed while sitting. More accurate reproduction of knee joint angles was noted during the WB protocol. In a study performed by Magalhaes et al.9), a WB task offered more proprioception and sensorimotor feedback than an NWB task. On the other hand, Keifer et al.12) reported greater position error during a WB task compared with an NWB task. In stroke patients, both the more affected side and less affected side showed deficits in joint position sense1). However, the differences between the sides have been little studied in previous studies, and few studies have compared WB and NWB positions in chronic stroke patients. Thus, our study aimed to assess knee joint proprioception in WB and NWB positions and to study the difference between the positions in chronic stroke patients.
SUBJECTS AND METHODS
The subjects were fifteen people who had had a stroke and had been admitted to a rehabilitation clinic. They were randomly scheduled by a physical therapist not involved in the study. Random scheduling was performed by selection of a sealed opaque envelope from among envelopes containing different schedules. The selected schedules were given to the physiotherapist in sealed numbered envelopes. The inclusion criteria were (1) stroke experienced more than 6 months before the study; (2) sufficient cognition to participate in the study, that is, a Mini-Mental State Examination (MMSE)13) score of 24 or higher; (3) ability to stand independently for more than 30 seconds; (4) sufficient knee flexion and extension of more than 150°; (5) no excessive spasticity, defined as a grade of 2 or higher on the Modified Ashworth Scale14); and (6) not participating in any experimental rehabilitation or drug studies. The exclusion criteria were (1) any comorbidity or disability and (2) any uncontrolled health condition for which this study was contraindicated. Participation in the study was voluntary, and the subjects fully understood its contents. All subjects were informed about the test methods and the use of the results, and were asked to sign a written statement in which the formally consented to inclusion in the study. The study was approved by the Daejeon University institutional review board.
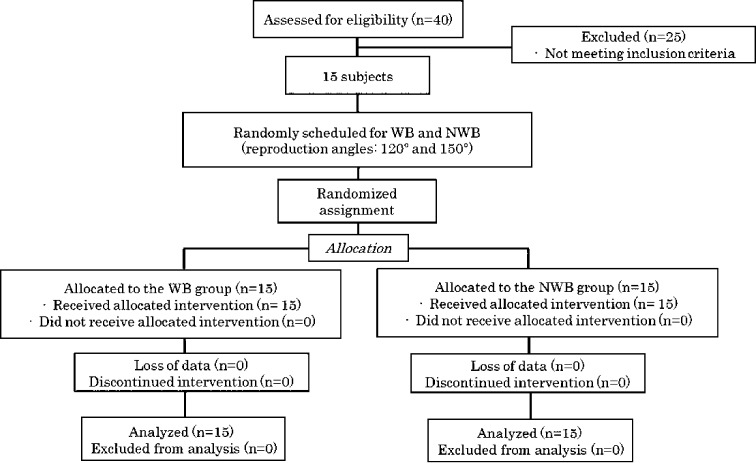
The subjects were subjected to the tests after gaining sufficient familiarity with the test protocols. All procedures are shown in the flow diagram in Fig. 1.
Fig. 1.
Flow diagram
The knee position sense was measured for both the more affected and less affected sides using the WB and NWB methods explained below. The knee position sense for both sides was assessed by an active test with the ipsilateral active limb matching response, i.e., with the examiner passively moving the limb to a knee joint angle of 120° or 150° while the subjects eyes were closed.
For the WB position method, the subjects were positioned in one-leg standing to assess knee joint position sense and blindfolded to avoid any visual cues. To minimize cutaneous input, the subjects were asked to wear short pants and to perform the tests while barefoot. A goniometer was attached to the side of the leg in such a manner that the fulcrum coincided with the lateral knee joint line; one arm of the goniometer (Seedtech., Incheon, Republic of Korea) was aligned parallel to the line joining the greater trochanter and fulcrum, while the other arm was aligned parallel to the leg. When the target angle of 120° or 150° of knee flexion was attained, the subjects were instructed to stop and to hold the position for 5 seconds. They were then instructed to straighten the knee and return to the erect standing position. After 7 seconds, the subjects indicated when they felt they had attained the target angle. The tester then instructed them to return to the starting position. The knee joint position sense was measured and recorded for both knees. The hold times used were the same as those used in previous studies3, 10).
For the NWB position method, subjects were instructed to sit comfortably in a chair and maintain the knees at 90° of flexion with legs out of the plinth and the thighs fully supported and were blindfolded to avoid any visual cues. To minimize cutaneous input, the subjects were asked to wear short and to perform the tests while barefoot. They were asked to extend the knee joint from 90° to 120° or 150°. When the target angle of 120° or 150° of knee extension was attained, the subjects were instructed to stop and hold the position for 5 seconds. They were then instructed to flex the knee. After 7 seconds, the subjects indicated when they felt they had attained the target angle. The tester instructed the subjects to return to the starting position. The knee joint position sense was measured and recorded for both knees. This sequence was repeated for a total of 5 trials. The angles of knee and extension were chosen randomly from 120° or 150° to prevent a learning effect.
Measurements were recorded as an absolute error for both the target angle and the reproduced angle. The absolute error was the arithmetic difference between tested and reproduced angles. The mean of each set of 5 absolute errors was then calculated. Paired t-tests were used to compare differences between the WB and NWB positions. One-way repeated measures ANOVA was performed for comparison of the knee joint position sense for both the more affected and less affected sides. Post hoc testing was performed with Bonferroni correction. All statistical analyses were performed by using the PASW Statistics version 18.0 software. Data are presented as the mean and SD. The level of statistics significance was set at p<0.05.
RESULTS
Fifteen people met the inclusion criteria and voluntarily agreed to participate in this study. The subjects were randomly scheduled for testing in the WB and NWB positions. All subjects characteristic are shown in Table 1.
Table 1. General characteristic of subjects.
| Variables | Mean (SD) |
|---|---|
| Age (years) | 53.1 (10.2) |
| Gender (male/female) | 6/9 |
| Site of paresis (right/left) | 7/8 |
| Body weight (kg) | 68.3 (7.5) |
| Height (cm) | 165.3 (6.7) |
| MMSE (score) | 26.6 (2.4) |
| MAS (score) | 1.5 (0.3) |
MMSE: Mini-Mental State Examination, MAS: Modified Ashworth Scale
The mean absolute error and SDs according to the WB and NWB positions for both the more affected and less affected limbs are presented in Table 2. The WB position showed a significant difference between the more affected and less affected limbs for the knee joint angle of 120° (p<0.05, F=103.14). The NWB position showed a significant difference between the more affected and less affected limb for the knee joint angle of 120° (p<0.05, F=87.35). The WB position showed a significant difference between the more affected and less affected limb for the knee joint angle of 150° (p<0.05, F=55.92). The NWB position showed a significant difference between the more affected and less affected limb for the knee joint angle of 150° (p<0.05, F=15.29). The more affected limb showed a significant difference between the positions (WB versus NWB) for the knee joint angle of 120° (p=0.03, 95% CI= 4.86–7.68). The less affected limb showed a significant difference between the positions (WB versus NWB) for the knee joint angle of 120° (p=0.04, 95% CI= 3.39–4.97). The more affected limb showed a significant difference between the positions (WB versus NWB) for the knee joint angle of 150° (p=0.04, 95% CI= 1.46–8.91). The less affected limb showed a significant difference between the positions (WB versus NWB) for the knee joint angle of 150° (p=0.03, 95% CI= 0.57–6.7).
Table 2. Absolute errors for the knee joint positioning task in the WB and NWB positions.
| 120° (n= 15) | 150° (n=15) | |||
|---|---|---|---|---|
| WB | NWB | WB | NWB | |
| Error scores (degree) | ||||
| More affected limb | 6.5 (1.4) a*+ | 12.7 (2.7)* | 7.0 (1.0) *+ | 12.2 (7.0)* |
| Less affected limb | 3.0 (0.8) + | 7.18 (1.5) | 3.5 (2.1) + | 7.1 (5.0) |
aMeans (SD). *Significant difference within position for the same angle. +Significant difference between positions for the same angle. The significance level were set at p <0.05 for differences between the groups
DISCUSSION
This study was conducted to compare knee joint position sense between WB and NWB positions in chronic stroke patients. The results of the present study point out (1) that comparison of the mean of absolute errors in the WB and NWB positions showed a significant difference in knee position sense and (2) that there were significant differences in knee position sense between the more affected and less affected limbs.
Our study was conducted to compare the effect of the WB and NWB positions on knee joint position sense in chronic stroke patients, which has not been reported previously. However, previous studies have measured knee joint position sense with aging and in subjects with muscular skeletal diseases, injured knees, or knee ligament injuries11, 15, 16).
The absolute errors found in our study for knee joint position sense according to position in the chronic stroke patients appear to be higher than those in previous studies. In this regard, we thought that neurologic disorder affected knee position sense. However, the WB position showed lower absolute error means than the NWB position. This finding is in agreement with those of previous studies17, 18). In other words, the WB position had a positive effect on enhancing proprioception. More accurate reproduction of knee position sense was reported during the WB protocol. In a study by Hopper et al.19), the WB position was found to be more important for performance and injury prevention than the NWB position. The WB position is also more functional, and this makes it easy to perceive information for the area around the knee by co-activation.
Dominance in the lower limbs is not as distinct as in the upper limbs20), and the lack of differences in knee joint position sense between the two sides is not surprising. However, a trend was noted for the less affected limb of the stroke patients to have slightly better knee joint position sense. Both lower limbs showed decreased knee joint position sense compared with under other conditions (e.g., with aging or in individuals with muscular skeletal diseases, injured knees, or knee ligament injuries). Comparing both lower limbs, the knee of the more affected side showed a more significant increase in mean absolute error than the less affected limb. This indicates that the knee proprioception of the more affected limb was decreased by more than that of the less affected limb. However, the ranges of the mean absolute error were higher than those under other conditions. Thus, interventions for improving the proprioception of stroke patients should focus on both sides.
The central component of proprioception, that is, the integration of sensory input, is also affected by neurologic disorder. The conductive function of the central somatosensory pathway is impaired by loss of function of the dendrite system in the motor cortex21), a decrease in the number of neurons and receptors, and neurochemical modifications in the brain22, 23). Additionally, a decrease in muscle spindle sensitivity can also result from mediated changes in the gamma drive to the spindle themselves24).
The knee proprioception of chronic stroke patients differs between the weight-bearing and non-weight-bearing positions. This study also noted significant differences when comparing the more affected and less affected lower limbs. However, the study has some limitations, including the relatively small groups and lack of investigation of training effects. Therefore, the results must be interpreted with caution.
REFERENCES
- 1.Walker C, Brouwer BJ, Culham EG: Use of visual feedback in retraining balance following acute stroke. Phys Ther, 2000, 80: 886–895. [PubMed] [Google Scholar]
- 2.Cho SH, Bae CH, Gak HB: Effects of closed kinetic chain exercises on proprioception and functional scores of the knee after anterior cruciate ligament reconstruction. J Phys Ther Sci, 2013, 25: 1239–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson EO, Babis GC, Soultanis KC, et al. : Functional neuroanatomy of proprioception. J Surg Orthop Adv, 2008, 17: 159–164. [PubMed] [Google Scholar]
- 4.Lee HM, Liau JJ, Cheng CK, et al. : Evaluation of shoulder proprioception following muscle fatigue. Clin Biomech (Bristol, Avon), 2003, 18: 843–847. [DOI] [PubMed] [Google Scholar]
- 5.Choi SJ, Shin WS, Oh BK, et al. : Effect of training with whole body vibration on the sitting balance of stroke patients. J Phys Ther Sci, 2014, 26: 1411–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams DA, Farrell MJ, Cunningham J, et al. : Knee pain and radiographic osteoarthritis interact in the prediction of levels of self-reported disability. Arthritis Rheum, 2004, 51: 558–561. [DOI] [PubMed] [Google Scholar]
- 7.Ribeiro F, Mota J, Oliveira J: Effect of exercise-induced fatigue on position sense of the knee in the elderly. Eur J Appl Physiol, 2007, 99: 379–385. [DOI] [PubMed] [Google Scholar]
- 8.Riemann BL, Myers JB, Lephart SM: Sensorimotor system measurement techniques. J Athl Train, 2002, 37: 85–98. [PMC free article] [PubMed] [Google Scholar]
- 9.Magalhães T, Ribeiro F, Pinheiro A, et al. : Warming-up before sporting activity improves knee position sense. Phys Ther Sport, 2010, 11: 86–90. [DOI] [PubMed] [Google Scholar]
- 10.Smith TO, Davies L, Hing CB: A systematic review to determine the reliability of knee joint position sense assessment measures. Knee, 2013, 20: 162–169. [DOI] [PubMed] [Google Scholar]
- 11.Lokhande MV, Shetye J, Mehta A, et al. : Assessment of knee joint proprioception in weight bearing and in non-weight bearing positions in normal subjects. JKIMSU, 2013, 2: 94–101. [Google Scholar]
- 12.Kiefer G, Forwell L, Kramer J, et al. : Comparison of sitting and standing protocols for testing knee proprioception. Physiother Can, 1998, 50: 30–34. [Google Scholar]
- 13.Folstein MF, Folstein SE, McHugh PR: “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res, 1975, 12: 189–198. [DOI] [PubMed] [Google Scholar]
- 14.Bohannon RW, Smith MB: Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther, 1987, 67: 206–207. [DOI] [PubMed] [Google Scholar]
- 15.Bullock-Saxton JE, Wong WJ, Hogan N: The influence of age on weight-bearing joint reposition sense of the knee. Exp Brain Res, 2001, 136: 400–406. [DOI] [PubMed] [Google Scholar]
- 16.Givoni NJ, Pham T, Allen TJ, et al. : The effect of quadriceps muscle fatigue on position matching at the knee. J Physiol, 2007, 584: 111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ghiasi F, Akbari A: Comparison of the effects of open and closed kinematic chain and different target position on the knee joint position sense. J Med Sci, 2007, 7: 969–976. [Google Scholar]
- 18.Drouin JM, Houglum PA, Perrin DH, et al. : Weight-bearing and non-weight-bearing knee-joint reposition sense and functional performance. J Sport Rehabil, 2003, 12: 54–66. [Google Scholar]
- 19.Hopper DM, Creagh MJ, Formby PA, et al. : Functional measurement of knee joint position sense after anterior cruciate ligament reconstruction. Arch Phys Med Rehabil, 2003, 84: 868–872. [DOI] [PubMed] [Google Scholar]
- 20.Gentry V, Gabbard C: Foot-preference behavior: a developmental perspective. J Gen Psychol, 1995, 122: 37–45. [DOI] [PubMed] [Google Scholar]
- 21.Tia B, Mourey F, Ballay Y, et al. : Improvement of motor performance by observational training in elderly people. Neurosci Lett, 2010, 480: 138–142. [DOI] [PubMed] [Google Scholar]
- 22.Pakkenberg B, Gundersen HJ: Neocortical neuron number in humans: effect of sex and age. J Comp Neurol, 1997, 384: 312–320. [PubMed] [Google Scholar]
- 23.Kwon O, Lee S, Lee Y, et al. : The effect of repetitive passive and active movements on proprioception ability in forearm supination. J Phys Ther Sci, 2013, 25: 587–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ribeiro F, Oliveira J: Effect of physical exercise and age on knee joint position sense. Arch Gerontol Geriatr, 2010, 51: 64–67. [DOI] [PubMed] [Google Scholar]