Abstract
[Purpose] We evaluated the relationship between knee alignment and the electromyographic (EMG) activity of the vastus medialis (VM) to the vastus lateralis (VL) muscles in patients with knee osteoarthritis (OA) in a cross-sectional study. [Subjects and Methods] Forty subjects with knee OA were assessed by anatomic radiographic knee alignment and the VM/VL ratio was calculated. Surface EMG from both the VM and VL muscles were evaluated during maximal isometric contraction at 60° knee flexion. Simultaneously, peak quadriceps torque was assessed using an isokinetic dynamometer. Subjects were categorized into low, moderate, and high varus groups according to knee malalignment. The peak quadriceps torque and VM/VL ratio across groups, and their relationships with varus malalignment were analyzed. [Results] All subjects had medial compartment OA and the VM/VL ratio of all subjects was 1.31 ± 0.28 (mean ± SD). There were no significant differences in the peak quadriceps torque or VM/VL ratios across the groups nor were there any significant relationships with varus malalignment. [Conclusion] The VM/VL ratio and peak quadriceps torque were not associated with the severity of knee varus malalignment.
Key words: Malalignment, Knee, Quadriceps
INTRODUCTION
Joint malalignment and a disproportionate axial load on the knee joint may contribute to the pathogenesis of knee osteoarthritis (OA)1, 2), although they could also be caused by the progression of OA3). An increased disproportional load on the joint in the frontal plane causes progressive cartilage loss on the medial or lateral side of the knee articular surface and bony angular deformity4). A prospective longitudinal cohort study5) demonstrated that, in primary knee OA, varus alignment increases the risk of medial OA progression (adjusted odds ratio [OR] 4.09) and valgus alignment increases the risk of lateral OA progression (adjusted OR 4.89). Additionally, varus or valgus alignment exceeding 5° at baseline was associated with greater functional deterioration over 18 months than an alignment of 5° or less.
As a biomechanical factor in the pathogenesis in knee OA, knee malalignment influences the external knee moment in the frontal plane during gait, in addition to the static load distribution across the knee joint6). Some studies have demonstrated that subjects with medial compartment knee OA walk with a greater than normal peak external knee adduction moment, and the baseline adduction moment of the knee predicted radiographic OA progression at the 6 year follow-up of patients with medial compartment knee OA7, 8).
Knee alignment depends on not only bony or articular geometry, but also on the peri-articular tissues, such as joint laxity or the strength of the surrounding muscles9, 10). Among these factors, the latter are reversible and modifiable. Although quadriceps weakness is a well-known risk factor of knee OA progression and quadriceps strengthening has been emphasized for knee OA rehabilitation, it is unclear how quadriceps strength is associated with knee malalignment. One study11) reported that the benefits of quadriceps strengthening on pain were more evident in those with more neutral alignment, while another study12) showed that greater quadriceps strength at baseline was associated with an increased likelihood of tibiofemoral OA progression in malaligned and lax knees.
This study focused on the relationship between quadriceps strength and knee alignment, and we postulated that specific strengthening of separate components of the quadriceps according to the malalignment direction would be required if the vastus medial (VM) or lateral (VL) quadriceps strength is associated with varus or valgus alignment, respectively. A recent study showed that the VM to VL ratio of the cross-sectional area obtained by magnetic resonance imaging (MRI) was significantly higher in the genu varum group than in the neutral or genu valgum groups of young healthy volunteers13).
In this study, we investigated the relationship between the VM to VL activity ratio and knee alignment in subjects with knee OA. We hypothesized that the VM to VL electromyographic (EMG) activity ratio would be significantly greater in subjects with more varus malalignment than in those with a more neutral alignment.
SUBJECTS AND METHODS
Forty females with knee OA were recruited from the Department of Rehabilitation Medicine at Seoul St. Mary’s Hospital in South Korea. All subjects were 50 years old or over and had knee pain. They also met inclusion criterion 1) or at least two of criteria 2)–6) established by the American College of Rheumatology (ACR)14): 1) Kellgren and Lawrence (K/L) grade ≥II, 2) morning stiffness <30 min in duration, 3) crepitus on movement of the knee joint, 4) bony tenderness at the knee joint margins, 5) palpable or visible bony enlargement, and 6) no palpable warmth. Study exclusion criteria were a history of lower limb surgery or trauma, a knee injection in the preceding 2 months, a history of inflammatory arthritis, peripheral polyneuropathy, or balance or gait disturbance.
The study was approved by the Ethics Committee of the Catholic University of Korea and written consents to participication in the study was obtained from all subjects in accordance with the Declaration of Helsinki.
Radiographs were taken of a weight-bearing anteroposterior view of the most painful knee in full extension to assess joint alignment and OA severity. The subjects stood without footwear, with the tibial tubercles facing forward. Anatomic knee alignment was determined using the method of Moreland et al.15) and mechanical knee alignment was extrapolated using the regression equation of Hinman et al.16): mechanical alignment = 0.915 × (anatomic alignment) + 13.895. Anatomic alignment was measured as the angle at the intersection of the femoral and tibial anatomic axes (Fig. 1).
Fig. 1.
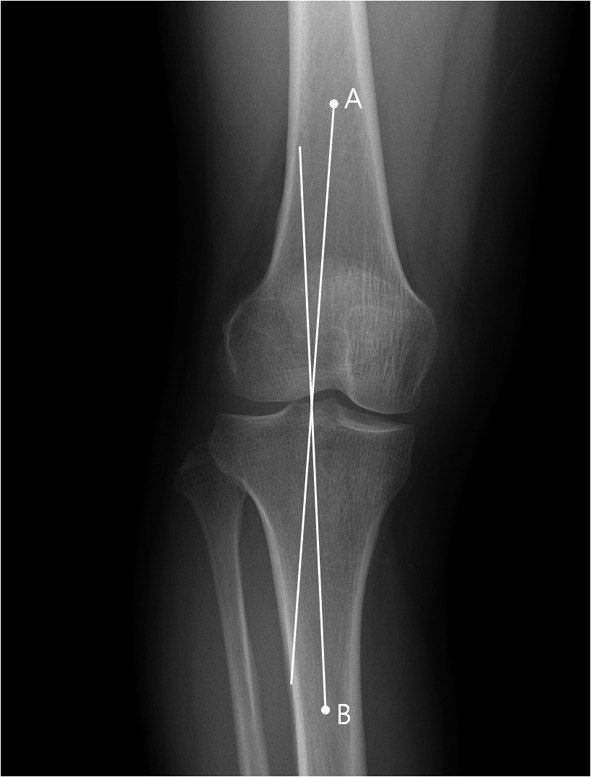
Radiographic analysis. The anatomic knee alignment is measured as the angle of the intersection of lines A and B. Line A is the line of the femoral anatomic axis; Line B is the line of the tibia anatomic axis. Mechanical alignment = 0.915 × (anatomic alignment) + 13.895.
The femoral anatomic axis was determined by drawing a line from the center of the tibial spines to a point located 10 cm proximally, midway between the medial and lateral femoral surfaces. In the same manner, the line of the tibia anatomic axis was drawn from the center of the tibial spines to a point 10 cm distally, midway between the medial and lateral tibial surfaces. In this study, the angle of knee alignment was defined as the deviation from neutral (0°) in the varus direction. OA severity was assessed using the K/L grade. All subjects were analyzed radiographically in a blinded manner by an experienced radiologist.
The peak quadriceps torque was assessed using an isokinetic dynamometer (Primus RS, BTE Technologies, Colorado) during maximal isometric contraction at 60° knee flexion. The lateral epicondyle of the femur was aligned with the axis of rotation of the dynamometer. Straps were secured firmly over the distal tibia, distal third of the thigh, and waist to limit extraneous movement. A submaximal warm-up was followed by three maximal 4-s contractions with 1-min rests between trials. The highest peak force determined by averaging the data of the three trials was multiplied by the lever length, which was then normalized by body mass (Nm/kg). The subjects were encouraged verbally, but they were blinded to the torque levels they produced.
Surface EMG recordings were performed using a Synergy EMG (Medelec, Surrey, UK) with the following equipment settings: low-frequency filter 20 Hz, high-frequency filter 1,000 Hz, and a common mode rejection ratio of over 110 dB. Before electrode placement, the skin was cleaned with alcohol to reduce signal impedance. A custom-designed disposable electrode (CareFusion, Hoechberg, Germany) was used to measure surface EMG activity. Active electrodes were placed over the motor points of the VM and VL muscles, and reference electrodes were placed over the tendons of the VM and VL, respectively. The ground electrode was positioned over the medial malleolus.
For each subject, the EMG activities were measured over the 2-s period corresponding to the time of maximum activation, during testing of peak quadriceps torque. The root mean square (RMS) value was calculated and used for the EMG amplitude17). Measurements were taken three times at 1-min intervals and the RMS average values were used in the analysis.
Statistical analyses were performed using SPSS software (ver. 11.5). First, subjects were classified into three groups based on the degree of their varus alignment: subjects with knee alignment ≤ 2 degrees varus were categorized as low varus, those with 2–4 degrees varus as moderate varus, and those ≥ 4 degrees varus were categorized as high varus18). One-way analysis of variance (ANOVA) was used to compare normally distributed variables (i.e., age, height, weight, body mass index, peak quadriceps torque, and the VM/VL ratio) across the groups. Varus alignment and a numeric rating scale (NRS) for pain were assessed using the Kruskal-Wallis test because they were not normally distributed. The K/L grade was compared among the groups using Fisher’s exact test. Analyses of peak quadriceps torque and the VM/VL ratio were repeated using analyses of covariance, after adjusting for age and disease severity18). The relationships of the peak quadriceps torque or VM/VL ratio with respect to varus malalignment were assessed using multiple regression analyses, adjusted for age and disease severity. All tests were two-tailed, and p values < 0.05 were deemed to indicate statistical significance. The intraclass correlation coefficients [95% confidence intervals (CI)] for the tests of quadriceps torque and VM/VL ratio were 0.94 [0.84–0.98] and 0.86 [0.62–0.95], respectively.
RESULTS
The characteristics of the 40 subjects are summarized in Table 1. There were no significant differences in age, height, body weight, body mass index, NRS, or K/L grade among the groups (p > 0.05). All subjects had medial joint space narrowing greater than lateral joint space narrowing on visual inspection. The VM/VL ratio of all subjects averaged 1.31 ± 0.28 (mean ± SD). There were no significant differences in the peak quadriceps torque or VM/VL ratio among the groups after adjusting for age and disease severity (Table 2). There was no significant relationship between the peak quadriceps torque or VM/VL ratio and varus malalignment after adjusting for age and disease severity (Table 3).
Table 1. Characteristics of subjects of the 3 alignment groups.
| Entire cohort (n = 40) |
Low varus (n = 12) |
Moderate varus (n = 15) |
High varus (n = 13) |
|
|---|---|---|---|---|
| Age, years | 56.7 ± 4.4 | 58.8 ± 4.6 | 56.0 ± 3.9 | 55.6 ± 4.3 |
| Height, cm | 154.6 ± 4.5 | 155.0 ± 5.7 | 154.9 ± 3.8 | 153.8 ± 4.3 |
| Body weight, kg | 57.7 ± 7.5 | 59.4 ± 7.4 | 58.8 ± 6.4 | 54.8 ± 8.4 |
| BMI, kg/m2 | 24.1 ± 2.4 | 24.7 ± 2.0 | 24.5 ± 2.2 | 23.1 ± 2.7 |
| Varus alignment (degrees) | 3.2 ± 2.6 | 0.2 ± 1.3* | 3.1 ± 0.6* | 6.0 ± 1.9* |
| Pain score (NRS) | 3.2 ± 0.7 | 3.1 ± 0.5 | 3.3 ± 0.7 | 3.1 ± 0.9 |
| K/L grade, no. | ||||
| I | 3 | 1 | 1 | 1 |
| II | 23 | 7 | 9 | 7 |
| III | 11 | 4 | 3 | 4 |
| IV | 3 | 0 | 2 | 1 |
| Quadriceps torque, Nm/kg | 1.10 ± 0.33 | 1.14 ± 0.37 | 0.99 ± 0.31 | 1.17 ± 0.32 |
| VM/VL ratio | 1.31 ± 0.28 | 1.31 ± 0.27 | 1.31 ± 0.31 | 1.30 ± 0.28 |
Values are the mean ± SD unless otherwise indicated. BMI: body mass index; NRS: numeric rating scale; K/L: Kellgren/Lawrence; no: number; VM: vastus medialis; VL: vastus lateralis. * Significant difference, p < 0.05.
Table 2. Quadriceps measurements of the 3 alignment groups adjusted for age and disease severity.
| Least varus (n = 12) |
Moderate varus (n = 15) |
Most varus (n = 13) |
|
|---|---|---|---|
| Quadriceps torque, Nm/kg | 1.10 ± 0.10 | 1.01 ± 0.09 | 1.19 ± 0.09 |
| VM/VL ratio | 1.21 ± 0.08 | 1.36 ± 0.06 | 1.35 ± 0.07 |
Values are expressed as adjusted mean ± SE unless otherwise indicated. VM: vastus medialis; VL: vastus lateralis. *Significant difference, p < 0.05.
Table 3. Association between quadriceps measurements and knee alignment as determined by regression analyses adjusted for age and disease severity.
| B | R2 | |
|---|---|---|
| Quadriceps torque, Nm/kg | −0.001 | 0.066 |
| VM/VL ratio | 3.224 | 0.141 |
B: unstandardized regression coefficient. VM: vastus medialis; VL: vastus lateralis. *Significant difference, p < 0.05.
DISCUSSION
Although we hypothesized that the VM/VL ratio would be significantly greater in subjects with greater varus malalignment than in those with a more neutral alignment, there were no significant associations between the VM/VL ratio and the knee varus alignment categories. However, the EMG activity of the VM was greater than that of the VL, with the mean VM/VL ratio being approximately 1.3. This is consistent with the results of a recent study12), in which the VM/VL ratio of the cross-sectional area obtained by MRI was higher in a genu varum group than in a neutral or genu valgum groups. A previous study showed that the ratio of VM oblique to VL EMG activity during knee flexion-extension movement in subjects with no knee pain was almost 1:119). However, we cannot directly compare our results with these results because we evaluated the VM/VL ratio of knee OA patients during maximal isometric contraction, and most of them had varus alignment. Thus, further study including OA patients with valgus alignment is needed.
There were no significant differences in the peak quadriceps torque and pain score (VAS) among the groups, which is a finding similar to that reported in a recent study18). The mean isometric strength at 60° knee flexion of our subjects was 1.1 Nm/kg, which was similar to that reported by Lim et al.18), considering that our study included only female patients. However, there was no significant correlation between the peak quadriceps torque and varus malalignment, in contrast to a previous study18) which reported that knee alignment accounted for a small, but significant proportion of the variance in quadriceps strength. It is unclear why our findings differed from this result. There are several possible reasons. First, the number of subjects was small, and it may have been insufficient to show a correlation between the peak quadriceps torque and varus malalignment. Second, the distribution of alignment was somewhat narrow, most of the subjects had moderate varus malalignment, of 2–5 degrees, and only five patients had mild valgus alignment. Third, a potential health-based selection bias could exist, because volunteers with knee OA were recruited for our study and they had active life styles, which might have lessened the differences in quadriceps activities across the groups.
The roles of joint malalignment have not been clearly determined for knee OA progression. Knee malalignment might cause progressive cartilage loss, further progression of unilateral compartment OA, and a decline in physical function after as little as 18 months of observation4, 5). Malalignment might disturb the normal transmission of force across the knee by shifting the load-bearing axis, the line drawn from the middle of the femoral head to the middle of the ankle. This line passes medial or lateral to the knee in varus or valgus malalignment, respectively20). Disproportionate loading of the knee joint during static postures can be increased by dynamic activities, such as gait. Osteoarthritic changes in the knee joint commonly involve the medial compartment, so varus malalignment is more common than valgus malalignment, as seen in our study. As noted above, varus malalignment may further increase the medial load during gait21) with increased adduction moment, contributing to the progression of medial compartment knee OA6,7,8).
Mechanical stress generated from geometric alignment induces specific muscle loading, which may elicit hypertrophy of that muscle. In our study, the VM activity was greater than the VL activity in all but two subjects. An exploration of whether the VM/VL ratio is associated with varus or valgus alignment is important for knee OA rehabilitation. Quadriceps strengthening has long been emphasized for knee OA rehabilitation. However, there is some evidence that generic quadriceps strengthening is not always helpful for knee OA, especially in patients with knee malalignment. Sharma et al.12) revealed that greater absolute quadriceps strength in people with malaligned knees may have deleterious consequences in terms of primary knee OA progression. With malalignment, the muscle force is not generated on the joint structures evenly and the extensor muscles might function less efficiently than with a normally aligned knee22). Thus, specific muscle training rather than a generic strengthening program is required for knee OA rehabilitation.
If a relationship exists between knee alignment and the VM/VL ratio, it would provide evidence in support of the development of specific strengthening programs tailored to knee alignment. Although we found no correlation between knee alignment and the VM/VL ratio, the VM/VL ratio was high in the subjects who had varus alignment. To our knowledge, this is the first study to examine the relationship between the VM/VL ratio and knee alignment.
Our study had several limitations. First, we did not obtain full-limb radiographs to determine mechanical alignment. Although the tibia or femur anatomic axis can be mistaken with a bow curvature, a good to excellent correlation between the anatomic and mechanical axes (r = 0.65–0.88) has been reported16, 23). Thus, it seems unlikely that our results would change with use of the mechanical axis. Second, our study had a cross-sectional design, so a cause-and-effect relationship could not be inferred from our present results. Third, as mentioned above, the number of subjects in our study was small and the distribution of alignment was narrow.
Future studies should evaluate more subjects, including patients with valgus alignment. More dynamic analyses are needed to confirm the relationship between the VM/VL ratio and knee alignments during walking or jogging, and the effects of separate quadriceps muscle strengthening on malalignment should also be evaluated.
In conclusion, neither the VM/VL ratio nor the peak quadriceps torque were not associated with the severity of knee varus malalignment.
Acknowledgments
The authors wish to acknowledge the financial support of the Catholic Medical Center Research Foundation made in the program year of 2012.
REFERENCES
- 1.Hafez AR, Al-Johani AH, Zakaria AR, et al. : Treatment of knee osteoarthritis in relation to hamstring and quadriceps strength. J Phys Ther Sci, 2013, 25: 1401–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim H, Song CH: Comparison of the VMO/VL EMG ratio and onset timing of VMO relative to VL in subjects with and without patellofemoral pain syndrome. J Phys Ther Sci, 2012, 24: 1315–1317. [Google Scholar]
- 3.Hunter DJ, Niu J, Felson DT, et al. : Knee alignment does not predict incident osteoarthritis: the Framingham osteoarthritis study. Arthritis Rheum, 2007, 56: 1212–1218. [DOI] [PubMed] [Google Scholar]
- 4.Cicuttini F, Wluka A, Hankin J, et al. : Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology (Oxford), 2004, 43: 321–324. [DOI] [PubMed] [Google Scholar]
- 5.Sharma L, Song J, Felson DT, et al. : The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA, 2001, 286: 188–195. [DOI] [PubMed] [Google Scholar]
- 6.Hurwitz DE, Ryals AB, Case JP, et al. : The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. J Orthop Res, 2002, 20: 101–107. [DOI] [PubMed] [Google Scholar]
- 7.Baliunas AJ, Hurwitz DE, Ryals AB, et al. : Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage, 2002, 10: 573–579. [DOI] [PubMed] [Google Scholar]
- 8.Miyazaki T, Wada M, Kawahara H, et al. : Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis, 2002, 61: 617–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooke TD, Sled EA, Scudamore RA: Frontal plane knee alignment: a call for standardized measurement. J Rheumatol, 2007, 34: 1796–1801. [PubMed] [Google Scholar]
- 10.Lewek MD, Rudolph KS, Snyder-Mackler L: Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthritis Cartilage, 2004, 12: 745–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim BW, Hinman RS, Wrigley TV, et al. : Does knee malalignment mediate the effects of quadriceps strengthening on knee adduction moment, pain, and function in medial knee osteoarthritis? A randomized controlled trial. Arthritis Rheum, 2008, 59: 943–951. [DOI] [PubMed] [Google Scholar]
- 12.Sharma L, Dunlop DD, Cahue S, et al. : Quadriceps strength and osteoarthritis progression in malaligned and lax knees. Ann Intern Med, 2003, 138: 613–619. [DOI] [PubMed] [Google Scholar]
- 13.Sogabe A, Mukai N, Miyakawa S, et al. : Influence of knee alignment on quadriceps cross-sectional area. J Biomech, 2009, 42: 2313–2317. [DOI] [PubMed] [Google Scholar]
- 14.Altman R, Asch E, Bloch D, et al. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association: Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Arthritis Rheum, 1986, 29: 1039–1049. [DOI] [PubMed] [Google Scholar]
- 15.Moreland JR, Bassett LW, Hanker GJ: Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am, 1987, 69: 745–749. [PubMed] [Google Scholar]
- 16.Hinman RS, May RL, Crossley KM: Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Rheum, 2006, 55: 306–313. [DOI] [PubMed] [Google Scholar]
- 17.Qi Z, Ng G: EMG analysis of vastus medialis obliquus/vastus lateralis activities in subjects with patellofemoral pain syndrome before and after home exercise program. J Phys Ther Sci, 2007, 19: 131–137. [Google Scholar]
- 18.Lim BW, Hinman RS, Wrigley TV, et al. : Varus malalignment and its association with impairments and functional limitations in medial knee osteoarthritis. Arthritis Rheum, 2008, 59: 935–942. [DOI] [PubMed] [Google Scholar]
- 19.Powers CM, Landel R, Perry J: Timing and intensity of vastus muscle activity during functional activities in subjects with and without patellofemoral pain. Phys Ther, 1996, 76: 946–955, discussion 956–967. [DOI] [PubMed] [Google Scholar]
- 20.Sharma L: The role of varus and valgus alignment in knee osteoarthritis. Arthritis Rheum, 2007, 56: 1044–1047. [DOI] [PubMed] [Google Scholar]
- 21.Hsu RW, Himeno S, Coventry MB, et al. : Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res, 1990, (255): 215–227. [PubMed] [Google Scholar]
- 22.Marks R, Percy JS, Semple J, et al. : Quadriceps femoris activation changes in genu varum: a possible biomechanical factor in the pathogenesis of osteoarthrosis. J Theor Biol, 1994, 170: 283–289. [DOI] [PubMed] [Google Scholar]
- 23.Kraus VB, Vail TP, Worrell T, et al. : A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum, 2005, 52: 1730–1735. [DOI] [PubMed] [Google Scholar]


