Abstract
[Purpose] This study compared the effects on neck-shoulder pain and mobility of strengthening exercises for the neck flexors and scapular retractors performed on a Swiss ball and a mat. [Subjects] Twenty student volunteers were the subjects. [Methods] The students were randomly assigned to two groups: Mat group (n=10), and Swiss ball group (n=10). At pre-test, post-test, and 1-week follow-up pain was assessed using the visual analogue scale (VAS), the pain pressure threshold (PPT) of the shoulder was measured with an algometer, and neck mobility was measured with a Zebris. [Results] The data analysis revealed that there was a significant decrease in pain and significant increase in neck flexion in both groups, and the Swiss ball group showed better results. [Conclusion] Strengthening the neck flexors and scapular retractors for stabilization of the neck using exercises on a Swiss ball was more effective at reducing the pain and stabilizing the neck than mat exercises.
Key words: Forward head posture, Visual display terminal syndrome, Swiss ball
INTRODUCTION
In 2012, the Korea Internet Security Agency, KISA, reported that over 50% of the population of Korea are using smart phones, which were introduced in 2009, with an average usage of 2.7 hours per day1). There are large numbers of workers employed in tasks involving the use of video display terminals (VDTs), which are associated with musculoskeletal and skin problems, eye discomfort, fatigue, and stress2). Computer related neck and upper extremity pain has been reported among college and graduate students over the last ten years3). While using a VDT, static sitting postures increase muscle tension, resulting in pain, numbness, loss of function, and a variety of neuromuscular symptoms, most often in the upper body4). A forward head posture (FHP) is commonly adopted by VDT users5, 6), and approximately 60% of individuals with neck pain had FHP or significantly increased FHP as a result of using computer for more than 2 hours a day7, 8). FHP and trunk flexion may gradually develop into a fixed postural habit when workers use a VDT9), and may also affect normal shoulder elevation, as elevation of the upper extremity requires the same amount of cervical spine extension10).
FHP is defined as the external auditory meatus being anterior to the acromion process10). Support of the cervical segments is provided by the muscular sleeve formed by the longus colli, which has a major postural function in supporting and straightening cervical lordosis; the longus capitis which attaches to the cranium and anteriorly spans the upper cervical motion segments and the craniocervical (CV) region; and the semispinalis cervicis and cervical multifidus, subocciptal extensor, semispinalis, and splenius capitis muscles which span the CVregion posteriorly11). Weak neck flexors and high density muscle spindles reduce the ability to maintain an upright posture and cervical posture. A computer model showed regions of local segmental instability when the large superficial muscles of the neck were stimulated to produce movement, particularly in the near-upright and neutral postures9, 12). Weakness of the scapular retractors, middle-lower trapezius, and rhomboids, causes increased scapular abduction during relaxed standing13).
There are various self-correction exercises like chin-tuck, for strengthening the neck flexors and stretching neck extensors, and improving the endurance and tone of the cervical muscles13). Thoracic manipulation is also effective at reducing neck pain, improving dysfunction, neck posture, and neck ROM of patients with chronic mechanical neck pain14). However, only a few studies have used a Swiss ball, which has many benefits such as allowing free weight resistance exercises, neuromuscular demands on the whole body for motor coordination and facilitate on of multi-angle resistance training which elicits greater ROM8, 15), for the neck stabilization. Moreover, none have compared the effects on neck support of Swiss ball and mat exercises.
Therefore, the purpose of this study was to investigate the effects on shoulder pain and neck mobility of strengthening neck flexors and scapular retractors using a Swiss ball to provide useful clinical guidelines for reducing pain or increasing cervical ROM, in comparison with mat exercises.
SUBJECTS AND METHODS
One-hundred thirty-seven university students answered 17 questions about VDT syndrome and 20 university students (4 males, 16 females) aged 21 to 23 years participated in this study. The subjects had experienced VDT syndrome but had not received treatment for it and didn’t do any regular exercise. All participants signed a written informed consent form approved by the Institutional Review Board of the Catholic University of Daegu. After selection, the subjects were randomly and equally allocated to one of two groups: a Swiss ball group which performed strengthening exercises for the neck flexors and scapular retractors, and a mat group which performed the same exercises on a mat. The study was conducted on college premises and the exercises were performed under the supervision of an instructor. The subjects were asked not to receive any specific intervention for neck-shoulder pain.
For strengthening the neck flexors, subjects lay supine with the head up and chin-tuck. Both hands were placed on the abdomen16). The mat group placed a towel on middle of the thorax to reduce abdominal muscle tension. For strengthening the scapular retractors, the subjects lay prone with the shoulders in 90–120° abduction, then extended spine by external rotation of the arms with chin-tuck14). Both groups performed the same exercises twice a week for 4 weeks, a total of 8 sessions. The training consisted of 10 repetitions 10- second holds in the first two weeks, followed by 15 second holds in the final two weeks.
Upper trapezius pain was evaluated using the visual analog scale and an algometer (JETCH, Japan), and a Zebris (Zebris Medical GmbH, CMS100, Germany) was used to measure neck mobility. Measurements were taken at pre- and post test, and a follow-up was also performed a week after the intervention.
The data was analyzed using SPSS version 18.0. The independent t-test was used to compare age, heights, and weight between groups. The independent variable in this study was strengthening exercises and the dependent variables were shoulder pain and neck mobility. Repeated measures ANOVA was used to find significance of differences in the dependent variables according to time between groups. The results were accepted as significant for p<0.05.
RESULTS
There were 20 subjects, 2 males and 8 females, in each group. Subjects mean ages, heights, and weights were 21.8±1.1 years, 167.6±8.9 cm, 60.0±14.6 kg in the Swiss ball group, and 21.8±1.9 years, 167.7±8.3 cm, 58.4±11.6 kg in the mat group. Subject characteristics were homogeneous at baseline (All p>0.05).
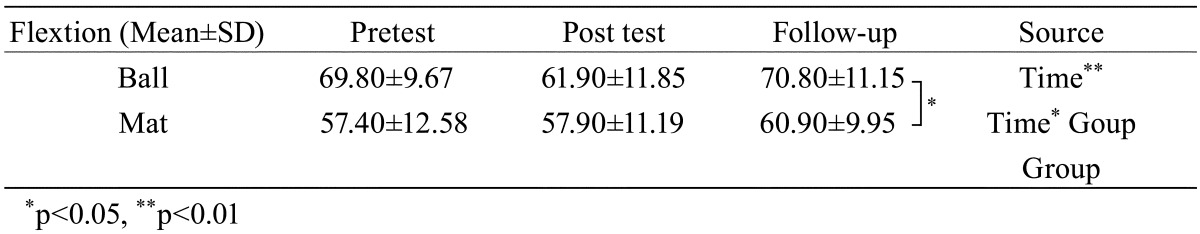
VAS significantly decreased with time (p<0.05) in both the left and right upper trapezius, especially at follow-up (p<0.05) on the right side, and at post-test (p<0.05) on the left side. Both sides showed no interaction within the groups (p<0.05, Table 1). Algometer pain showed a significant time effect (p<0.05) for right upper trapezius and a group effect (p<0.05) for the left upper trapezius. There was no interaction within groups (p>0.05, Table 2). Neck flexion significantly increased with time too (p<0.05), especially at follow-up (p<0.05). There was no interaction within the groups (p<0.05, Table 3 ).
Table 1. Comparison of VAS of the right/left upper trapezius by repeated measures ANOVA.
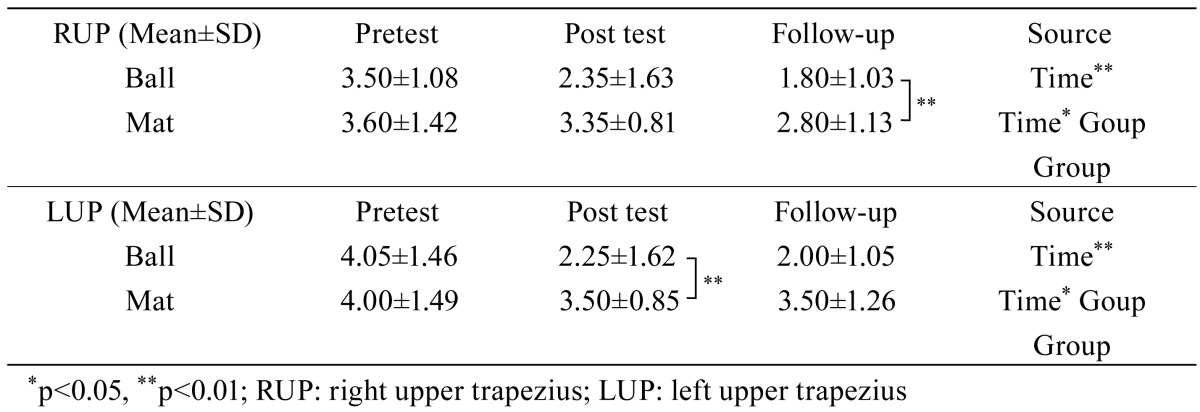
Table 2. Comparison of the pain pressure threshold of the right/left upper trapezius by repeated measures ANOVA.
| RUP (Mean±SD) | Pretest | Post test | Follow-up | Source |
| Ball | 1.74±0.67 | 0.90±0.39 | 1.46±0.66 | Time* |
| Mat | 1.70±0.41 | 1.04±0.35 | 1.36±0.47 | Time*Group |
| Group | ||||
| LUP (Mean±SD) | Pretest | Post test | Follow-up | Source |
| Ball | 1.63±0.43 | 1.21±0.39 | 1.47±0.55 | Time |
| Mat | 1.35±0.35 | 0.89±0.38 | 1.11±0.20 | Time*Group |
| Group* | ||||
*p<0.05, **p<0.01; RUP: right upper trapezius; LUP: left upper trapezius
Table 3. Comparison of neck flexion by repeated measures ANOVA.
DISCUSSION
The purpose of this study was to determine the effects on neck-shoulder pain and mobility of exercises using a Swiss ball for strengthening the neck flexors and scapular retractors, and neck and scapular stabilizers performed by young adults who had prolonged daily exposure to VDTs.
The results for the upper trapazius VAS show that the Swiss ball group had significantly decreased right upper trapezius pain at the follow-up test (p<0.05), and left upper trapezius pain at the post-test (p<0.05, Table 1). In previous studies of neck stabilization exercises using the hold-relax technique for the upper trapezius, levator scapula, scalenus, and suboccipitals, VAS decreased significantly from 3.35 to 1.65 (p<0.001) for the neck, and from 4.55 to 2.05 for the shoulder (p<0.001), and the pain pressure threshold (PPT) of the four muscles increased (p<0.001), but ROM did not differ17). In core stability programs using a Swiss ball, Thera-bands, and a mat, The thera-band group showed the most reduced VAS followed by the Swiss ball group, and the mat group18). Cranio-cervical flexor and thoracic mobilization was effective at reducing VAS19). Chin tucks, chest stretch, wall stretch, on your back chest stretch, axial extension with neck isometrics, wall angels, Bruegger exercise, dead bug, quadruped, upper back cat performed 4 times a week for 8 weeks results in significant changes in the CV angle (p<0.001), cervical ROM (p<0.001) and PPT (p<0.001)20). There is moderate negative correlation between CV angle and neck disability7). Mat exercise had a longer retention effect21). These results show that strengthening the neck flexors and scapular retractors is effective at reducing the pain and changes the CV angle. They also show that Swiss ball exercise is more effective at reducing pain than mat exercise.
The results of Zebris measurements of neck mobility show that there was a significant increase in neck flexion at the follow-up (p<0.05, Table 3), and significantly decreased neck lateral flexion and extension, and significantly increased right-left rotation (p<0.05). Patients with small a CV angle have greater FHP and disability7). Treatment for poor cervical posture should focus on recovering normal ROM of neck flexion and extension. Increasing neck flexion reduced the CV angle and that contributed to reduce the FHP for stabilization of the neck22). Previous studies have demonstrated that Swiss ball exercise elicits greater total core muscle work than mat exercise. Petrofsky23) compared core muscle activities in exercises on a Swiss ball, 7- inch mini ball, and the floor. In a comparison of exercises on a Swiss ball and mat, floor crunches required about two thirds of the work used for the same exercises on a Swiss ball. The Swiss ball provides greater extension and flexion but the extent of that movement is limited by the diameter of the ball with a larger diameter eliciting less movement. Chek24) reported that the size of the ball enables athletes to train certain muscles through a greater ROM. While lying with the lower back on the center of the ball, athletes can perform abdominal crunches beginning with the abdominal muscles in the stretched position. This stretched position can’t be worked while lying on a flat, horizontal surface. It is claimed that the effect of the pre-stretch and potential strength development in the stretched position can enhance the effectiveness of the exercise and make the task more functionally useful to athletes. The present study didn’t start exercise in the stretched position which can increase ROM on the Swiss ball.
This study was limited to eight training sessions, and ROM was not compared between the Swiss ball and mat exercises groups. Also, the CV angle was not measured so we could not determine if there was any improvement in FHP.
The results of this study show that pain was significantly decreased by exercises on a Swiss ball, which also and increased neck flexion for stabilization of the neck. Exercises on a Swiss ball, which has a small base of support, should be used for reducing pain and stabilization of the neck, and exercises on a mat for increasing ROM. The Swiss ball and mat could be used selectively either for training or the purpose of the treatment. Further study should compare the motions of both Swiss ball and mat exercises and investigate the neurophysiological benefits of the former.
REFERENCES
- 1.Korea internet security agency, Internet use survey approve nation (12005). 2012.
- 2.World Health Organization: Visual display terminals and workers’ health. Geneva: WHO, Offset publication No 99, 1987. [PubMed] [Google Scholar]
- 3.Menéndez CC, Amick BC, 3rd, Jenkins M, et al. : Upper extremity pain and computer use among engineering graduate students: a replication study. Am J Ind Med, 2009, 52: 113–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pascarelli EF, Hsu YP: Understanding work-related upper extremity disorders: clinical findings in 485 computer users, musicians, and others. J Occup Rehabil, 2001, 11: 1–21. [DOI] [PubMed] [Google Scholar]
- 5.Moore MK: Upper crossed syndrome and its relationship to cervicogenic headache. J Manipulative Physiol Ther, 2004, 27: 414–420. [DOI] [PubMed] [Google Scholar]
- 6.Szeto GP, Straker LM, O’Sullivan PB: A comparison of symptomatic and asymptomatic office workers performing monotonous keyboard work—2: neck and shoulder kinematics. Man Ther, 2005, 10: 281–291. [DOI] [PubMed] [Google Scholar]
- 7.Yip CH, Chiu TT, Poon AT: The relationship between head posture and severity and disability of patients with neck pain. Man Ther, 2008, 13: 148–154. [DOI] [PubMed] [Google Scholar]
- 8.Lehman GJ, Hoda W, Oliver S: Trunk muscle activity during bridging exercises on and off a Swiss ball. Chiropr Osteopat, 2005, 13: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Winters JM, Peles JD: Neck muscle activity and 3D head kinematics during static and dynamic tracking movements. In: Winters JM, Woo SLY, eds. Multiple Muscle Systems: Biomechanics and Movement Organization. New York: Springer-Verlag, 1990: 46180. [Google Scholar]
- 10.Starkey C, Ryan J: Evaluation of orthopedics-Assessment of posture, 2nd ed. Philadelphia: FA Davis, 2002. [Google Scholar]
- 11.Mayoux-Benhamou MA, Revel M, Vallee C, et al. : Longuscolli has a postural function on cervical curvature. Surg Radiol Ana, 1994, 16: 36771. [DOI] [PubMed] [Google Scholar]
- 12.Falla D, Jull G, Russell T, et al. : Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther, 2007, 87: 408–417. [DOI] [PubMed] [Google Scholar]
- 13.Carolyn K, Allen CL: Therapuetic Exercise-foundation and Techniques Chapter 15: Subacute Chronic and Postural Pproblems, 3rd ed. Philadelphia: FA David Co, 1996. [Google Scholar]
- 14.Harman K, Hubley-Kozey CL, Butler H: Effectiveness of an exercise program to improve forward head posture in normal adults: a randomized, controlled 10-week trial. J Manual Manip Ther, 2005, 13: 163–176. [Google Scholar]
- 15.Morrissey MC, Harman EA, Johnson MJ: Resistance training modes: specificity and effectiveness. Med Sci Sports Exerc, 1995, 27: 648–660. [PubMed] [Google Scholar]
- 16.Dalton E: Strategies to address forward head posture. Massage magazine, 2006, 119: 99–103. [Google Scholar]
- 17.Kim YM: Effects of the use of the hold relax technique to treat female VDT workers with work-related neck-shoulder complaints. Korean J Occup Environ Med, 2009, 21: 18–27. [Google Scholar]
- 18.Naik VA: 4 week core stability exercise programme using Swiss ball, theraband and floor exercises in cricketers with low back pain”: a randomised clinical trail, 2012.
- 19.Ko T, Jeong U, Lee K: Effects of the inclusion thoracic mobilization into cranio-cervical flexor exercise in patients with chronic neck pain. J Phys Ther Sci, 2010, 22: 87–91. [Google Scholar]
- 20.Shenoy S, Sodhi J, Sandhu JS: Effectiveness of strengthening exercises in the management of forward head posture among computer professionals. Ind J Phys Occup Ther, 2010, 4. [Google Scholar]
- 21.Dusunceli Y, Ozturk C, Atamaz F, et al. : Efficacy of neck stabilization exercises for neck pain: a randomized controlled study. J Rehabil Med, 2009, 41: 626–631. [DOI] [PubMed] [Google Scholar]
- 22.Yoo WG, An DH: The relationship between the active cervical range of motion and changes in head and neck posture after continuous VDT work. Ind Health, 2009, 47: 183–188. [DOI] [PubMed] [Google Scholar]
- 23.Petrofsky JS, Batt J, Davis N,, et al. : Core muscle activity during exercise on a mini stability ball compared with abdominal crunches on the floor and on a Swiss ball. J Applied Research, 2007, 7: 255–272. [Google Scholar]
- 24.Chek P: Jungle Gym Exercise Revisited. Muscle Media, 1998, 69: 136–214. [Google Scholar]


