Abstract
Objectives
The factors affecting the acceptance of mobile obesity-management applications (apps) by the public were analyzed using a mobile healthcare system (MHS) technology acceptance model (TAM).
Methods
The subjects who participated in this study were Android smartphone users who had an intent to manage their weight. They used the obesity-management app for two weeks, and then completed an 18-item survey designed to determine the factors influencing the acceptance of the app. Three questions were asked pertaining to each of the following six factors: compatibility, self-efficacy, technical support and training, perceived usefulness, perceived ease of use, and behavior regarding intention to use. Cronbach's alpha was used to assess the reliability of the scales. Pathway analysis was also performed to evaluate the MHS acceptance model.
Results
A total of 94 subjects participated in this study. The results indicate that compatibility, perceived usefulness, and perceived ease of use significantly affected the behavioral intention to use the mobile obesity-management app. Technical support and training also significantly affected the perceived ease of use; however, the hypotheses that self-efficacy affects perceived usefulness and perceived ease of use were not supported in this study.
Conclusions
This is the first attempt to analyze the factors influencing mobile obesity-management app acceptance using a TAM. Further studies should cover not only obesity but also other chronic diseases and should analyze the factors affecting the acceptance of apps among healthcare consumers in general.
Keywords: Obesity, Weight Loss, Telemedicine, Mobile Health Units, Statistical Factor Analysis
I. Introduction
With the recent popularization of wireless devices, such as tablet PCs, PDAs, and smartphones, mobile healthcare (mHealth) has also become widespread [1]. Mobile healthcare systems (MHSs) are being developed for healthcare professionals, and in particular, for emergency care and the management of chronic illness [2]. However, most MHSs for healthcare professionals have either failed at the developmental stage [3] or have not been applied as predicted in the hospital setting [4]. Among these implementation failures, 30% can be attributed to non-technical factors, the most significant of which was insufficient user acceptance, a factor that has long been considered as an obstacle to the successful adoption of information technology (IT) and information systems (IS) [5].
Several models have been introduced to explain the acceptance of technological products and services, including mobile products and services. Technology acceptance models (TAMs) and their extensions, such as TAM2 and the unified theory of acceptance and use of technology (UTAUT), are the most commonly used models for examining users' acceptance of mHealth products and services. For example, Wu et al. [6] used the original TAM to examine the adoption of mobile computing by healthcare professionals in hospital settings; Zhang et al. [7] used TAM2 to study the factors influencing the adoption of mobile IT by homecare nurses; and Lee and Rho [8] used UTAUT to examine the factors influencing the acceptance of mobile health monitoring by users.
Obesity is one of the most pressing issues in healthcare for the general public, including in the Republic of Korea. According to the regional health statistics data of the Korean Ministry of Health and Welfare, the prevalence of obesity in Korea was 23.3% in 2011, which represents a 0.8% increase from the previous year [9]. To control obesity, it is important to help the patient to control his/her weight over the long term, taking into account the obesity level and treatment demands of the individual [10]. To this end, nursing interventions using IT that provide continuous interventions and are free from temporal and spatial limitations, such as the Internet and mobile devices, have been proven effective in terms of accessibility, equity, and cost [11]. A study that analyzed the quality of health information offered by obesity-management apps in the United States found that there were 204 iOS-based obesity-management apps in 2009 [12], while another study on the quality of health information provided by obesity-management apps in Korea found 148 iOS-based obesity-management apps in 2013 [13]. The total number of obesity-management apps is predicted to be even higher given that Android-based apps were excluded from these studies.
The market size of mobile apps in the healthcare field, including those for obesity management, has increased by 44% annually from US $500 million in 2010, with the industry's sales profit increasing more than tenfold in 2012 [14]. Despite this increase, no research on the factors influencing the acceptance of mobile obesity-management apps by the general public has yet been conducted. Therefore, the aim of this study was to elucidate the factors affecting the public's acceptance of an obesity-management app. An obesity-management app that was developed by the author in 2012 based on the clinical guidelines for obesity [15] were used in this study.
1. Conceptual Model and Research Hypotheses
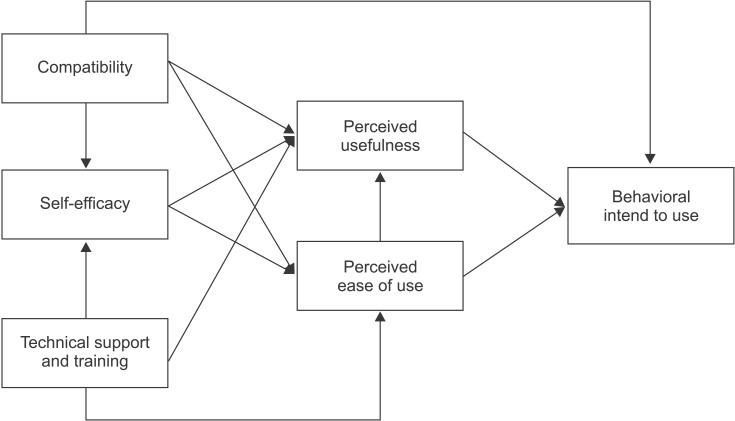
This study analyzed the factors influencing the acceptance of an obesity-management app using the MHS acceptance model (Figure 1) developed by Wu et al. [6].
Figure 1. Mobile healthcare system (MHS) acceptance model.
1) The MHS acceptance model
Wu et al. [6] developed the MHS acceptance model by bringing together perceived usefulness (PU), perceived ease of use (PEOU), and behavioral intention (BI) to use, the three concepts of the extended technology acceptance model (TAM2) [16], the concept of compatibility from innovation diffusion theory (IDT) [17], the concept of self-efficacy proposed by Venkatesh and Davis [16] and Compeau and Higgins [18], and the concept of technical support and training presented by Igbaria et al. [19].
BI, extracted from TAM2, is defined as the individual's interest in using an IS for future work, PEOU is defined as the degree to which a person believes that using a particular IS would be free from effort, and PU is defined as the degree to which a person believes that using a particular IS would enhance his or her job performance. BI is directly influenced by PU and PEOU [16,20].
Compatibility, a concept extracted from IDT, refers to the degree to which a technological innovation is consistent with the values, experiences, and needs of the potential users. Compatibility was found to be a factor that directly influences BI, such that a technology that is more compatible with the user's previous experience is more likely to be accepted [21]. A previous study also asserted that compatibility influences PU and PEOU, in that the user believes that an IS is more useful and easy to use if the system is compatible with their current practice [22]. Compatibility also positively influences MHS self-efficacy; that is, the user will feel more comfortable and confident in using the MHS, and this will result in higher self-efficacy when the mobile IT/IS is more compatible with the user's existing values, previous experiences, and practical needs.
According to Compeau and Higgins [18], self-efficacy in the use of IT is the user's perception of his or her capability to use IT for the accomplishment of a specific task. Self-efficacy using technology such as computers has been widely studied and was found to be positively influenced by the individuals' PEOU and PU [18].
Technical support and training, a concept presented by Igbaria et al. [19], refers to the provision of a tutorial program on IT or IS. Previous research has shown that when sufficient technical support and training is provided for a new IT/IS, self-efficacy for the technology was improved [18,19]. Another study also suggested that providing valuable training programs and technical support will increase the user's PEOU and PU [19].
2) Research hypotheses
The relationships among the various concepts included in the MHS acceptance model were examined in this study using a mobile obesity-management app. From the hypothesized model, each pathway becomes a hypothesis of the study.
The research hypotheses for the dependent variable, BI, were the following:
H1: Compatibility has a direct effect on the BI to use the mobile obesity-management app.
H2: Perceived usefulness has a direct effect on the BI to use the mobile obesity-management app.
H3: Perceived ease of use has a direct effect on the BI to use the mobile obesity-management app.
The research hypotheses for the mediating variable, PU, were the following:
H4: Compatibility has a direct effect on the PU of the mobile obesity-management app.
H5: Self-efficacy has a direct effect on the PU of the mobile obesity-management app.
H6: Technical support and training have a direct effect on the PU of the mobile obesity-management app.
H7: PEOU has a direct effect on the PU of the mobile obesity-management app.
The research hypotheses for the mediating variable, PEOU, were the following:
H8: Compatibility has a direct effect on the PEOU of the mobile obesity-management app.
H9: Self-efficacy has a direct effect on the PEOU of the mobile obesity-management app.
H10: Technical support and training have a direct effect on the PEOU of the mobile obesity-management app.
The research hypotheses for the mediating variable, selfefficacy, were the following:
H11: Compatibility has a direct effect on the self-efficacy of using the mobile obesity-management app.
H12: Technical support and training have a direct effect on the self-efficacy of using the mobile obesity-management app. II. Methods
II. Methods
1. Research Design
This was a survey study designed to examine the factors involved in the adoption of a mobile obesity-management app using the MHS acceptance model.
2. Study Subjects
The subjects for this study were 110 adult Android smartphone users who had an intent to manage their weight. The number of subjects required for the study was calculated based on the recommendation for the structural equation model: at least 15 subjects per observed variable [23]. Since there are six variables in the MHS acceptance model, at least 90 subjects were required. However, the final number of study subjects was 110 to compensate for potential dropout. Subjects who were receiving professional medical care for obesity management, including any medications or surgery, were excluded from this study.
A convenience sample of the study subjects was recruited from the College of Medicine, College of Dentistry, College of Nursing of Seoul National University Yongon Campus, and Seoul National University Hospital through public notices posted on bulletin boards or websites at these institutions.
3. Study Procedure
Subjects responding to the recruitment notice received a URL via SMS from which the obesity-management app could be downloaded. On first execution of the app, the subject was briefed about the research and asked to provide informed consent to participate. If the subject signed the consent form, the form was stored and an image file of the form was sent to the researcher. The subjects who agreed to participate in the study then received an instructional video on how to use the app. After receiving the instructions, each subject was asked to use the app for two weeks and then to complete a survey provided as a pop-up window. The survey collected demographical data and data on obesity-management app acceptance factors. The completed survey data, along with the data entered over the two-week study period (diet records, exercise records, body mass index (BMI), body weight, weight-loss goal, and weight-loss period) and usage logs of the app (access time) were sent to the researcher. The researcher analyzed the collected data using descriptive statistics and structural equation modeling. The study was conducted between November 12 and December 2, 2013.
4. Instruments
The factors affecting mobile obesity-management app acceptance were assessed using 18 questions, comprising three questions for each of the six factors [6]. Three of the six acceptance factors (PU, PEOU, and BI) were derived from two previous studies on TAM [16,20]. Technical support and training was elicited from Igbaria et al. [19], and compatibility was derived from Rogers [17] and Chau and Hu [24], whereas the items for MHS self-efficacy were captured using three items tailored from Compeau and Higgins [18] and Venkatesh et al. [25]. All questions used a five-point Likert-type response scale (1 = 'strongly disagree' to 5 = 'strongly agree').
The survey instrument was translated from English into Korean by the second author, and the translated questionnaire was back-translated into English by an independent professional translator [26]. Four nurse informatists holding a master's degree or higher then compared the back-translated instrument against the original instrument to ensure the equivalence of the translation.
5. Data Analysis
The subjects' demographic information, length of smartphone use, prior experience of obesity management, and prior experience of using an MHS app were analyzed for descriptive statistics using SPSS ver. 20.0 software (IBM SPSS, Armonk, NY, USA).
Descriptive statistics of the observed variables for mobile obesity-management app acceptance factors were analyzed for frequency, average, and standard deviation using SPSS ver. 20.0, and the reliability of the instrument was assessed using Cronbach's alpha. The correlations between the six acceptance factors were analyzed using Pearson correlation coefficients.
The MHS acceptance model was analyzed by path analysis using AMOS ver. 20.0 (IBM SPSS). The goodness of fit of a hypothetical model constructed based on the TAM was evaluated with the various goodness-of-fit indices including chi-square (χ2) statistics, the goodness-of-fit index (GFI), and the normed fit index (NFI). The cutoff for statistical significance was set at p < 0.05.
III. Results
1. Demographics of the Study Subjects
A total of 110 subjects participated in this study, of whom 95 completed the survey (response rate, 86.4%). One of these subjects returned an incomplete response and was therefore excluded; thus, the data of 94 subjects were used in the further analysis.
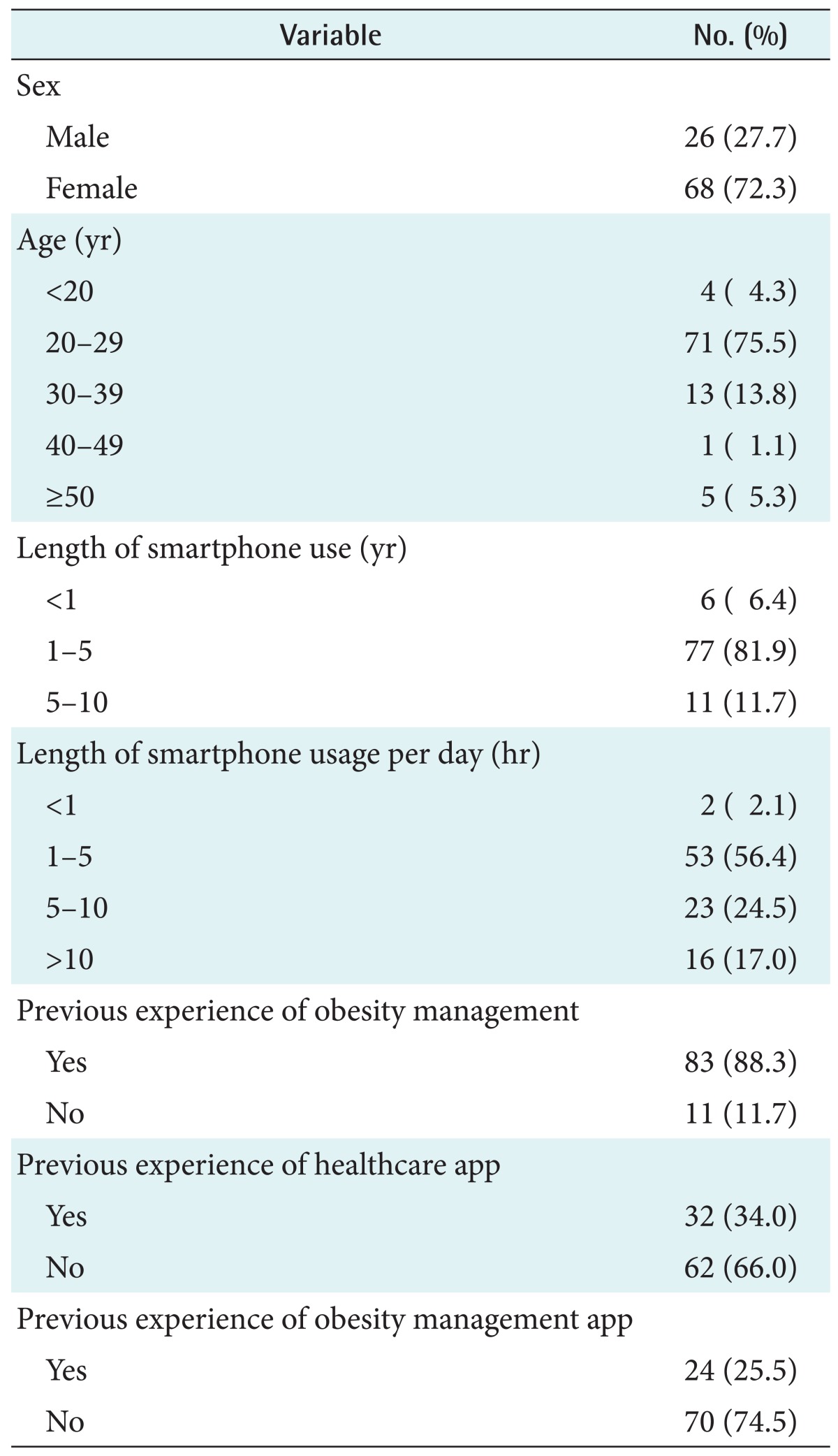
Table 1 gives the demographic information of the 94 respondents. The data show a higher proportion of female participants, with 68 females (72.3%) and 26 males (27.7%). Regarding age, the 20-29 years age group contained the largest number of participants (n = 71, 75.5%). Most of the subjects (n = 77, 81.9%) reported having used a smartphone for 1-5 years, and 53 (56.4%) reported using a mobile device for between 1 and 5 hours daily. More than 88% of the subjects answered having experienced obesity management, 32 (34.0%) responded that they had used a healthcare app, and 24 (25.5%) reported having used an obesity-management app before participating in this study.
Table 1. Demographic characteristics of the respondents.
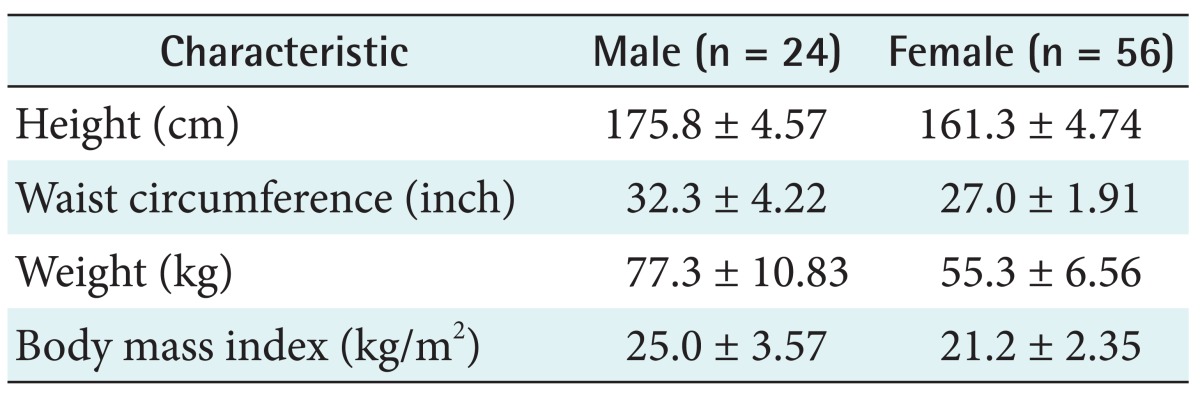
Of the 94 participants, 80 returned their usage record. For the 56 female participants who returned their data, the bodyweight was 55.3 ± 6.56 kg (mean ± SD), and the BMI was 21.2 ± 2.35 kg/m2. For the 24 male participants, the bodyweight was 77.3 ± 10.83 kg, and the BMI was 25.0 ± 3.57 kg/m2 (Table 2).
Table 2. Mean and standard deviation of obesity management app user's physical data (n = 80).
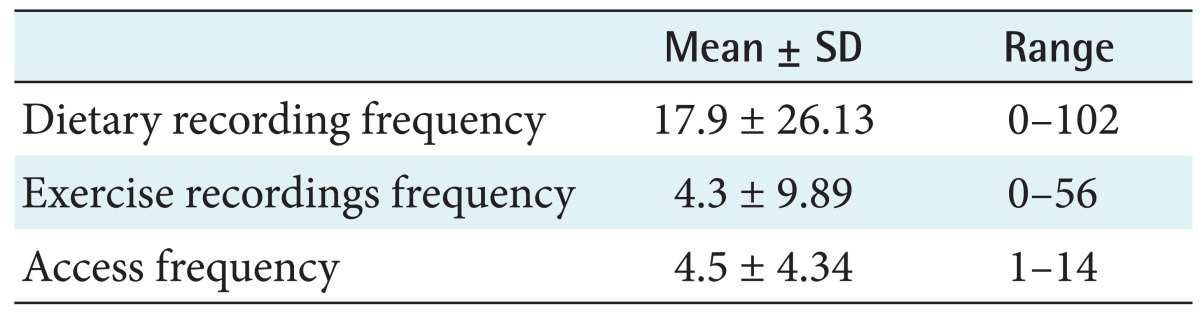
The usage logs (access and recording frequencies) of the 80 subjects who returned their data via the obesity-management app are summarized in Table 3. The frequency was highest for diet recordings, at 17.9 ± 26.13 (range, 0-102), and lowest for exercise recordings, at 4.3 ± 9.89.
Table 3. Record of obesity management app usage (n = 80).
2. Validity and Reliability of the Instrument
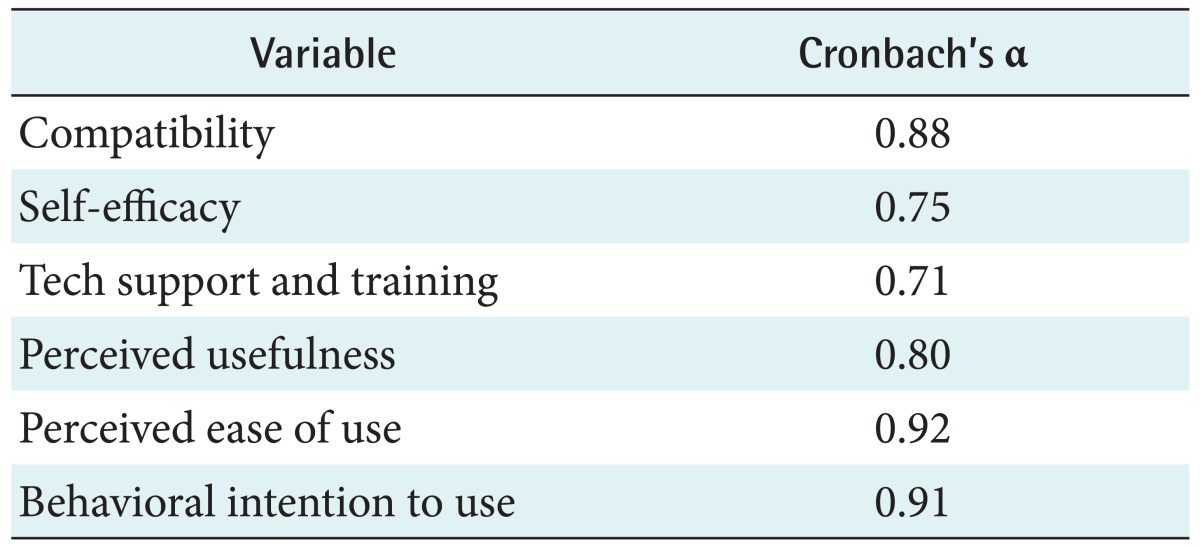
The internal consistency of the instrument used in this study was evaluated by calculating Cronbach's alpha (Table 4). Cronbach's alpha for all constructs ranged from 0.71 to 0.92, which are above the minimum acceptable threshold value of 0.60-0.70 suggested by Hair et al. [27].
Table 4. Reliability of measurement tools.
3. Descriptive Statistics for the MHS Acceptance Model Variables
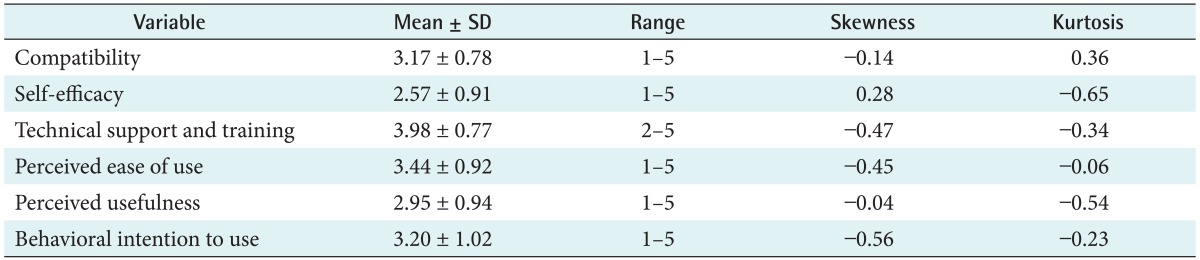
Among the observed variables of the MHS acceptance model, the mean values for compatibility, self-efficacy, and technical support and training were 3.17, 2.57, and 3.98, respectively. The mean values for PEOU and PU were 3.44 and 2.95, respectively, and the mean BI for the mobile obesity-management app was 3.20. Since the Z scores for skewness and kurtosis for all variables measured in this study did not exceed the critical value (±1.96) at the statistical significance level of 0.05 set by Hair et al. [27], it can be concluded that all of the variables were normally distributed (Table 5).
Table 5. Descriptive statistics of observed variables (n = 94).
4. Correlations among the MHS Acceptance Model Variables
The correlation coefficients among the MHS acceptance model variables are listed in Table 6. All of the correlation coefficients were statistically significant at the significance level at α = 0.05.
Table 6. Correlations among the measurement variables.
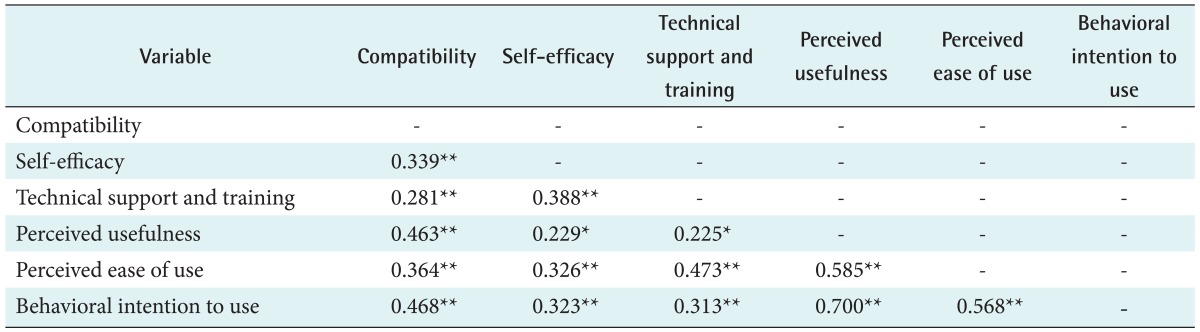
*Correlation is significant at the 0.05 level (two-tailed). **Correlation is significant at the 0.01 level (two-tailed).
5. Model Evaluation
1) Goodness of fit of the MHS acceptance model
The model included six latent constructs: technical support and training, compatibility, self-efficacy, PU, PEOU, and BI. Table 7 presents the goodness-of-fit statistics between the data and the proposed model.
Table 7. Model evaluation overall fit measurement.
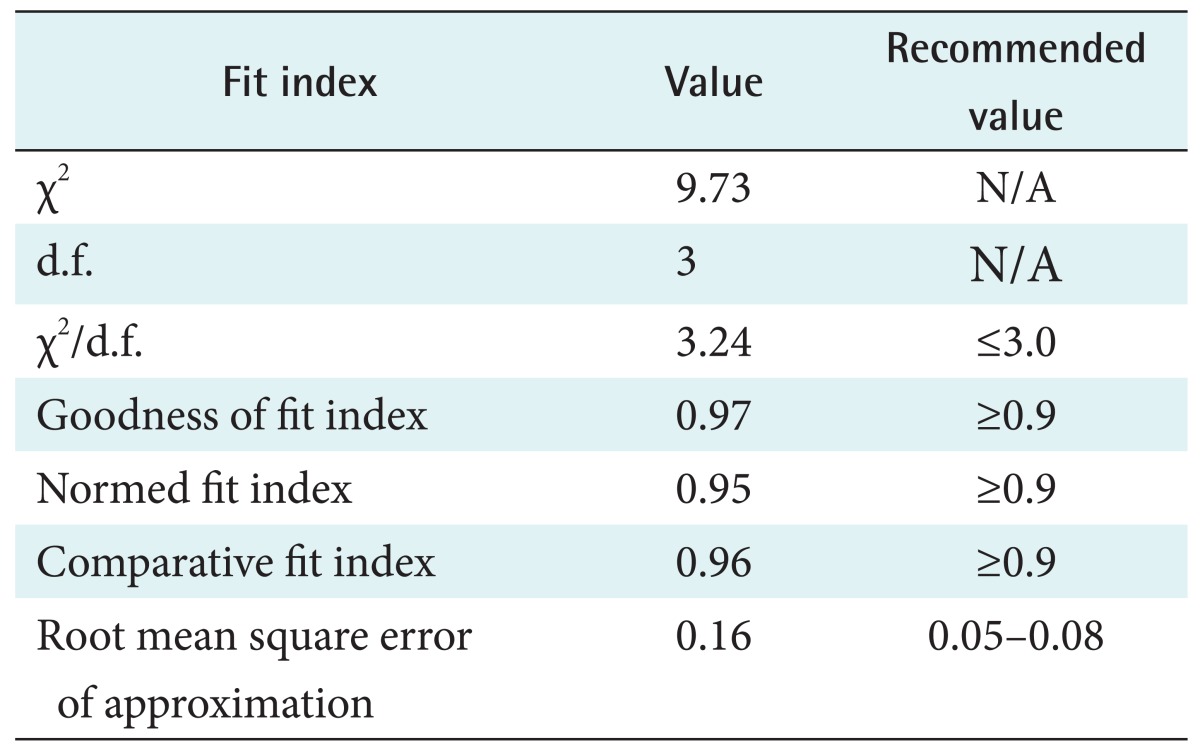
The ratio of χ2 to its degrees of freedom, 3.24, was greater than the recommended less than 3.0, and the root mean square error of approximation of 0.16 was not within the acceptable range of 0.05-0.08 set by Hair et al. [27]. However, the measurement model had a good fit with the data based on other indices of fit, such as the GFI (0.97) and NFI (0.95).
2) The structural model
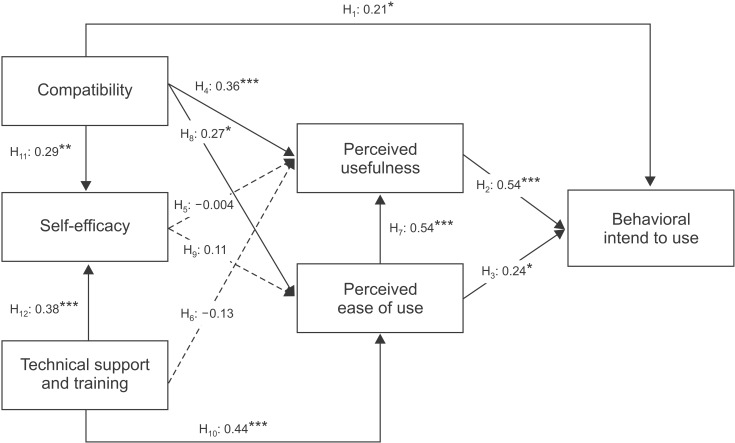
Table 8 lists the direct and indirect effects estimates of the MHS acceptance model variables for BI, PU, PEOU, and selfefficacy, and Figure 2 shows the standardized path coefficients of the hypothesized relationships among the variables. The hypotheses were strongly supported except for H5, H9, and H6. The data strongly support a very strong direct effect of PU on BI for the mobile obesity-management app (H2: β = 0.54, p < 0.001). The PEOU had a significant direct effect on BI for the mobile obesity-management app (H3: β = 0.24, p < 0.05), and an indirect effect on BI through the mediating variable of PU; meanwhile, PEOU had a very strong effect on PU (H7: β = 0.54, p < 0.001).
Table 8. Path analysis result - direct and indirect effects.
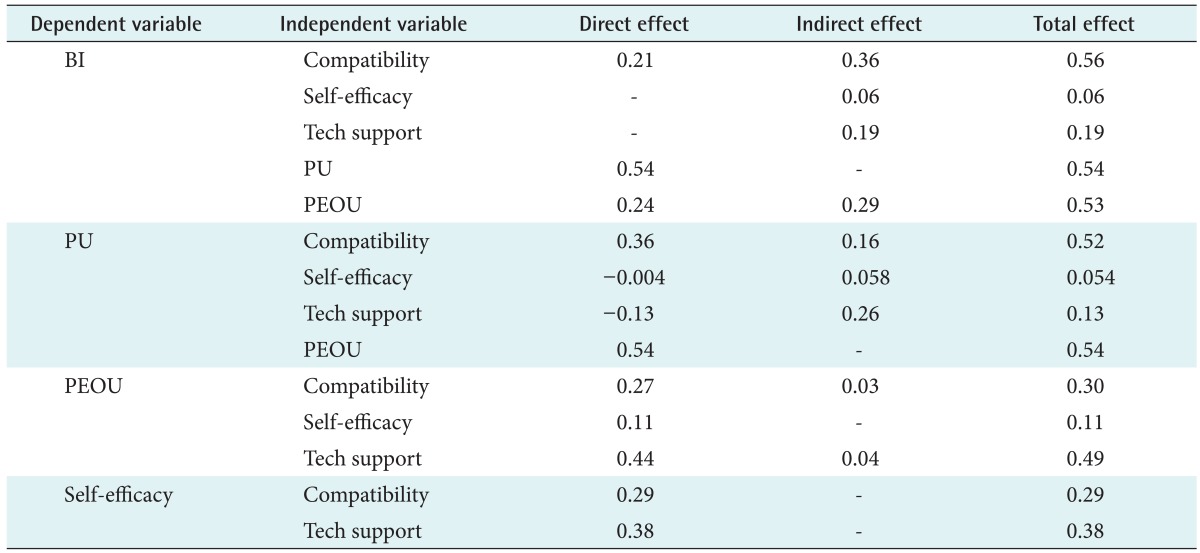
BI: behavioral intention, PU: perceived usefulness, PEOU: perceived ease of use.
Figure 2. Path diagram of mobile healthcare system (MHS) acceptance model for mobile obesitycare app (path coefficients are indicated in the path diagram). *p < 0.05, **p < 0.01, ***p < 0.001.
Compatibility had a direct effect on BI for the mobile obesity-management app (H1: β = 0.21, p < 0.05), a strong direct effect on PU (H4: β = 0.36, p < 0.001), and a significant effect on both PEOU (H8: β = 0.27, p < 0.05) and self-efficacy (H11: β = 0.29, p < 0.01). In addition, technical support and training had a strong direct effect on self-efficacy (H12: β = 0.38, p < 0.001) and on PEOU (H10: β = 0.44, p < 0.001). However, the data show that self-efficacy had no significant direct effects on PU (H5) or PEOU (H9), and that technical support and training had no significant effect on PU (H6).
IV. Discussion
The factors influencing the general public's acceptance of an obesity-management app were analyzed in this study using the MHS acceptance model, a composite model of TAM with and compatibility, self-efficacy, and technical support and training from the study of Wu et al. [6].
Descriptive statistics revealed that the age of the subjects who used the obesity-management app was 27.0 ± 8.46 years, most of whom (89.3%) fell into the age group of 20 to 39 years. This result is in line with that of Wu et al. [6] for mobile computing acceptance factors in hospitals, for which the subjects were aged 29.6 ± 6.34 years, 92.6% of whom were aged between 20 and 39 years. Finn found that most of the mHealth app consumers were aged between 35 and 44 years [28]. Thus, it appears that most mHealth app customers tend to be relatively young, in their 20s or 30s.
The results of the path analysis demonstrated that self-efficacy does not significantly affect PU or PEOU, which is the direct opposite of what Wu et al. [6] found. This discordance may be related to the tool used to measure self-efficacy when the obesity-management app is used. The concept of self-efficacy encompasses several different meanings, from self-efficacy in the use of a mobile device or obesity management in general to the specific use of a mobile obesity-management app. If we had measured self-efficacy at various levels, as did Hasan [29], who measured general mobile selfefficacy versus system-specific self-efficacy, the findings may have been different.
We also found that technical support and training had a significant effect on PEOU but not on PU. These findings contradict those of Wu et al. [6], who found that technical support and training had no significant effect on either PU or PEOU. Those authors explained that technical support and training did not affect PU and PEOU for two reasons: 1) the participating hospitals were all equipped with computerized healthcare IT/IS, and as such, all subjects were trained in basic computer skills, and 2) the participating hospitals provided MHS and relevant training to their staff [11]. However, the subjects of the present study were healthcare consumers, and unlike healthcare professionals, they lacked essential computing education or training, which may explain why technical support and training had a significant effect on PEOU.
The factors influencing the acceptance of an obesity-management mobile app, developed as a part of the Health Avatar project, were analyzed with a view to encouraging adoption of the app. Various mobile apps acting as health avatars were developed in the Health Avatar project. Mobile apps for the management of chronic diseases, such as diabetes, hypertension, and hyperlipidemia, are currently under development. These mobile apps will provide various healthcare interventions that are free from temporal and spatial limitations. Health avatars utilizing various health and disease management technologies are enabled by a variety of features, such as life-logging, self-tracking, and qualified-self. In fact, webbased programs and other smartphone apps that track, analyze, and provide feedback based on a person's diet, exercise, sleeping pattern, and activity are already popularly in use [30].
This study was subject to two main limitations. First, we did not analyze the relationship between obesity-management app usage (access frequency and diet/exercise recording frequency) and acceptance factors. This was due to the obesity management being used for a very short period of time and the low frequencies of access and data recording. Adding an alarm or reminder function to the app, as the users requested, would improve access and data recording frequencies, thus making it possible to study the relationship between app usage and acceptance factors. Second, snowball and convenient sampling methods, and a self-report survey were used in this study, which could have resulted in both selection bias and social desirability bias.
Notwithstanding these limitations, this study represents the first attempt to analyze mobile obesity-management app acceptance factors based on a TAM. Further studies are recommended to examine the effectiveness of the obesity-management app in terms of clinical outcomes, such as weight and BMI, and to confirm the findings of this study by repeating it with different study subjects using other mHealth apps or services for the management of various diseases.
Acknowledgments
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (No. 2010-0028631).
Footnotes
Conflict of Interest: The authors have no potential conflicts of interest relevant to this article.
References
- 1.Patrick K, Griswold WG, Raab F, Intille SS. Health and the mobile phone. Am J Prev Med. 2008;35(2):177–181. doi: 10.1016/j.amepre.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haux R. Health information systems - past, present, future. Int J Med Inform. 2006;75(3-4):268–281. doi: 10.1016/j.ijmedinf.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Berg M. Patient care information systems and health care work: a sociotechnical approach. Int J Med Inform. 1999;55(2):87–101. doi: 10.1016/s1386-5056(99)00011-8. [DOI] [PubMed] [Google Scholar]
- 4.Short D, Frischer M, Bashford J. Barriers to the adoption of computerised decision support systems in general practice consultations: a qualitative study of GPs perspectives. Int J Med Inform. 2004;73(4):357–362. doi: 10.1016/j.ijmedinf.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 5.Johnson JD, Meyer M, Woodworth M, Ethington C, Stengle W. Information technologies within the cancer information service: factors related to innovation adoption. Prev Med. 1998;27(5 Pt 2):S71–S83. doi: 10.1006/pmed.1998.0248. [DOI] [PubMed] [Google Scholar]
- 6.Wu JH, Wang SC, Lin LM. Mobile computing acceptance factors in the healthcare industry: a structural equation model. Int J Med Inform. 2007;76(1):66–77. doi: 10.1016/j.ijmedinf.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Zhang H, Cocosila M, Archer N. Factors of adoption of mobile information technology by homecare nurses: a technology acceptance model 2 approach. Comput Inform Nurs. 2010;28(1):49–56. doi: 10.1097/NCN.0b013e3181c0474a. [DOI] [PubMed] [Google Scholar]
- 8.Lee J, Rho MJ. Perception of influencing factors on acceptance of mobile health monitoring service: a comparison between users and non-users. Healthc Inform Res. 2013;19(3):167–176. doi: 10.4258/hir.2013.19.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korea Ministry of Health and Welfare. Korea National Health and Nutrition Examination. Seoul: Korea Ministry of Health and Welfare; 2011. [Google Scholar]
- 10.Goessens BM, Visseren FL, de Nooijer J, van den Borne HW, Algra A, Wierdsma J, et al. A pilot-study to identify the feasibility of an Internet-based coaching programme for changing the vascular risk profile of high-risk patients. Patient Educ Couns. 2008;73(1):67–72. doi: 10.1016/j.pec.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Jeon HO, Kim O. The effects of an internet based coaching program for obesity management in hypertensive patients. Korean J Adult Nurs. 2011;23(2):146–159. [Google Scholar]
- 12.Breton ER, Fuemmeler BF, Abroms LC. Weight loss-there is an app for that! But does it adhere to evidenceinformed practices? Transl Behav Med. 2011;1(4):523–529. doi: 10.1007/s13142-011-0076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeon E, Park HA, Min YH, Kim HY. Analysis of the information quality of Korean obesity-management smartphone applications. Healthc Inform Res. 2014;20(1):23–29. doi: 10.4258/hir.2014.20.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Research2guidance. Mobile health market report 2011-2016. Berlin: Research2guidance; 2012. [Google Scholar]
- 15.Jeon E, Park HA. Development of a smartphone application for clinical-guideline-based obesity management. Healthc Inform Res. 2015;21(1):10–20. doi: 10.4258/hir.2015.21.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venkatesh V, Davis FD. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manag Sci. 2000;46(2):186–204. [Google Scholar]
- 17.Rogers EM. Diffusion of innovations. 5th ed. New York(NY): Simon & Schuster Inc; 2003. [Google Scholar]
- 18.Compeau DR, Higgins CA. Computer self-efficacy: development of a measure and initial test. MIS Q. 1995;19(2):189–211. [Google Scholar]
- 19.Igbaria M, Zinatelli N, Cragg P, Cavaye AL. Personal computing acceptance factors in small firms: a structural equation model. MIS Q. 1997;21(3):279–305. [Google Scholar]
- 20.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989;13(3):319–340. [Google Scholar]
- 21.Van Slyke C, Lou H, Day J. The impact of perceived innovation characteristics on intention to use groupware. Inf Resour Manag J. 2002;15(1):1–12. [Google Scholar]
- 22.Jelekäinen P. GSM-PKI solution enabling secure mobile communications. Int J Med Inform. 2004;73(3):317–320. doi: 10.1016/j.ijmedinf.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 23.Kim K. AMOS 18.0 structural equation modeling analysis. Korean edition. Seoul, Korea: Hannarae Publishing; 2010. [Google Scholar]
- 24.Chau PY, Hu PJ. Investigating healthcare professionals' decisions to accept telemedicine technology: an empirical test of competing theories. Inf Manag. 2002;39(4):297–311. [Google Scholar]
- 25.Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q. 2003;27(3):425–478. [Google Scholar]
- 26.Chapman DW, Carter JF. Translation procedures for the cross cultural use of measurement instruments. Educ Eval Policy Anal. 1979;1(3):71–76. [Google Scholar]
- 27.Hair JF, Jr, Anderson RE, Tatham RL. Multivariate data analysis with readings. 2nd ed. New York (NY): Macmillan Publishing; 1986. [Google Scholar]
- 28.Ruder Finn Inc. mHealth report. New York (NY): Ruder Finn Inc.; 2012. [Google Scholar]
- 29.Hasan B. Delineating the effects of general and system-specific computer self-efficacy beliefs on IS acceptance. Inf Manag. 2006;43(5):565–571. [Google Scholar]
- 30.Kim J, Park HA. Development of a health information technology acceptance model using consumers' health behavior intention. J Med Internet Res. 2012;14(5):e133. doi: 10.2196/jmir.2143. [DOI] [PMC free article] [PubMed] [Google Scholar]