Abstract
A contextual review of models for chronic care was done to develop a context-adapted chronic care model-based service delivery model for chronic conditions including diabetes. The Philippines was used as the setting of a low-to-middle-income country. A context-based narrative review of existing models for chronic care was conducted. A situational analysis was done at the grassroots level, involving the leaders and members of the community, the patients, the local health system and the healthcare providers. A second analysis making use of certain organizational theories was done to explore on improving feasibility and acceptability of organizing care for chronic conditions. The analyses indicated that care for chronic conditions may be introduced, considering the needs of people with diabetes in particular and the community in general as recipients of care, and the issues and factors that may affect the healthcare workers and the health system as providers of this care. The context-adapted chronic care model-based service delivery model was constructed accordingly. Key features are: incorporation of chronic care in the health system’s services; assimilation of chronic care delivery with the other responsibilities of the healthcare workers but with redistribution of certain tasks; and ensuring that the recipients of care experience the whole spectrum of basic chronic care that includes education and promotion in the general population, risk identification, screening, counseling including self-care development, and clinical management of the chronic condition and any co-morbidities, regardless of level of control of the condition. This way, low-to-middle income countries can introduce and improve care for chronic conditions without entailing much additional demand on their limited resources.
Keywords: Chronic care models, Context adaptation, Diabetes mellitus type 2, Low-to-middle income countries, Service delivery model
Core tip: This paper introduces strategies that low-to-middle-income countries can employ to introduce feasible care and prevention for diabetes amidst problems of the double burden of disease and scarcity of resources, and presents a context-adapted service delivery model that integrates care for diabetes and similar chronic conditions in the current health services and assimilates the delivery of diabetes care with other responsibilities of the health system so that people under the care of health services and the health system can experience the whole spectrum of diabetes prevention and care.
INTRODUCTION
Chronic conditions are said to be a global crisis that threatens human development, especially in low-to-middle income countries (LMIC)[1,2]. A large number of people from LMICs live with chronic conditions. This includes around 291 million with diabetes[3].
The macroeconomic effects of chronic conditions including diabetes in LMICs are substantial. These disproportionately affect the poor[4] and the care for these conditions leads to continued and, as the condition worsens and complications develop, escalating expenditures while decreasing productivity. The costs of care and the disability or death of a household income earner may cause (further) poverty[5]. For every 10% rise in mortality from chronic conditions, the yearly economic growth of a country is estimated to be reduced by 0.5 percentage points[6]. Abegunde et al[7] computed projections of foregone national income due to heart disease, stroke and diabetes in 23 LMICs and showed that these countries combined are at risk of losing US$ 84 billion in economic output over the ten-year period 2006-2015.
Thus, LMICs should move towards strategies to deal with chronic conditions including the provision of good quality chronic care in order to address the evolution that is threatening their people. However, the acute disease-oriented health systems of LMICs may face a number of difficulties in adjusting health care delivery to accommodate the growing burden of chronic conditions in general and diabetes in particular. This could be attributed to various reasons including resource constraints, absence of programs directed towards chronic conditions, and difficulties in introducing and/or integrating care for chronic conditions.
An adequate approach to care for chronic conditions such as diabetes is very different from the acute disease-oriented approach practiced in most LMICs: in addition to the disease prevention and drug prescription activities usually done in acute disease care, chronic care also needs to focus on disability limitation and rehabilitation[8]; should give attention to the psychosocial aspects of the patient[9]; and should involve and enable the patient in caring for the condition[10]. Other features that make chronic care different from acute disease care include: (1) case finding for assessment of risk factors, detection of early disease, and identification of high risk status; and (2) long term follow-up with regular monitoring and promotion of adherence to pharmacological and psychological interventions[1].
Analyses have demonstrated that in spite of increased funding in LMICs, progress towards agreed Millennium Development Goals, including the health-related ones, remains slow[11]. This could be attributed to weak health systems, human resource constraints, and over-concentration of resources to specific programs. Introducing chronic disease care in toto as practiced in high income countries (HIC) or separately structured and resourced vertical programs to address specific chronic disease problems to LMIC health systems may prove detrimental if not fatal. A better approach could be to strengthen the first line and progressively integrate care for chronic conditions into primary care activities, taking into consideration the capabilities of the health system.
LMICs can take the initiative to undertake the first steps towards the provision of good quality chronic care. Adapting models for chronic care to fit the context of a country and selecting specific elements for implementation is likely to stand a better chance of improving chronic care. This way, specific problems such as resource constraints may be addressed; certain characteristics of the people, the health system and the country that could be capitalized on may be identified; and particular context-adapted strategies may be employed.
For this research, the investigators reviewed existing models for chronic care considering the results of a situational analysis of a low middle-income country, the Philippines, to come up with a model for diabetes care delivery that could be adapted in low-to-middle-income countries with similar characteristics.
BACKGROUND ON THE PHILIPPINES: HEALTH SYSTEMS, CHRONIC CONDITIONS AND DM TYPE 2
Public health care in the Philippines was devolved in 1992 and the responsibility of providing basic health care services for the people was handed down to the local government units, specifically municipalities and cities, through their respective local government health units (LGHU)[12]. A decade before this health care devolution, the country implemented a primary health care policy which led to the creation of a large cadre of community-based health care workers locally called barangay health workers (BHW)[13]. The barangay (village) is the smallest unit of government; a city or a municipality would be composed of a number of barangays. Organizationally, the BHW fall under the governance of the barangay and are selected to work in their respective areas of residence; functionally, they are under the LGHU. A BHW is assigned approximately 10-20 families and is responsible for dissemination of health information and health promotion activities, and conducts other health-related undertakings to any member of the families being attended to.
The Philippines is among the 23 low-and-middle-income countries where 80% of the LMIC mortality due to chronic conditions is accounted for[7]. It is likewise predicted to be among the 10 countries worldwide with the highest numbers of people with DM type 2 by 2030[14]. For the past decade, eight of the 10 leading causes of mortality in the Philippines are chronic conditions and DM type 2 has been consistently among these[15]. Furthermore, the complications and consequences of DM type 2 in the Philippines are on the rise and have become alarming. For renal complications alone, it is seen that 55% of Filipino diabetics will eventually develop kidney disease; in 2007 there was an increase of more than 2800 diabetic nephropathy patients requiring dialysis[16]. Aside from these, the International Diabetes Federation estimated undetected type 2 diabetes (UDD) in the Philippines at 58.8% in 2011[3]. It seems that the current screening strategies in routine conditions cannot adequately identify previously undetected cases of DM type 2 in the Philippines. The high rate of UDD, the rapidly increasing prevalence of DM type 2, and the poor control of disease progression and emergence of complications only show that current case management of diabetes mellitus in the Philippines is below optimum, and the burden will only escalate if no measures are employed to address these problems. On the macroeconomic level, the Philippines lost US$60 million in 2006 from coronary heart disease, stroke, and diabetes alone[7].
METHODS OF REVIEW AND CONTEXTUAL ANALYSIS
Narratives on models for chronic care and their elements, records of implementation and outcomes of implementation, if any, were analyzed and adapted to the context of the Philippines, an LMIC where the health system is still acute disease-oriented, there is limited organized care for chronic conditions, if at all, and healthcare expenditures are mostly out-of-pocket. The investigators focused on the two main models for chronic care, which have been used by HIC health systems as bases for the organization of chronic care. For the situational analyses, they considered a number of organizational theories: on how an organization may respond to pressure to change and what factors could influence an organization’s response; and the factors that may facilitate or hinder adoption of innovations introduced to an organization. Key factors affecting the adaptation of chronic care models and the development of a context-adapted chronic care model-derived service delivery model were explored making use of theories presented by Oliver[17] in her analysis of organizational responses to pressures towards conformity and Greenhalgh et al[18]’s theories on diffusion of innovation, taking into consideration the background of the country and its health system and the profiles of the healthcare workers, the people with chronic conditions, and the community. The Philippine context was used and informal interviews with representatives of the community (the government and the people), the healthcare system/service and people with diabetes were conducted.
MODELS FOR CHRONIC CARE
In HICs, models and frameworks for chronic care and its delivery have been implemented, most of which were derived from Wagner’s Chronic Care Model (CCM)[19]. The CCM was conceptualized from a primary care perspective and advocates improvements in six essential elements: self-management support, clinical information systems, delivery system redesign, decision support, health care organization, and community resources[20]. The basic idea of the CCM is quite sound: to optimize “productive interactions” between “informed, activated patients” on one hand, and “prepared, pro-active practice teams” on the other, resulting in “functional and clinical outcomes” (Figure 1). However, the CCM appears to be grounded in a preponderantly clinic-based perspective with a background of abundant resources and a highly technological environment such as can be found in HICs. Its focus seems to be on optimizing clinical interaction for more effect in dealing with chronic conditions.
Figure 1.
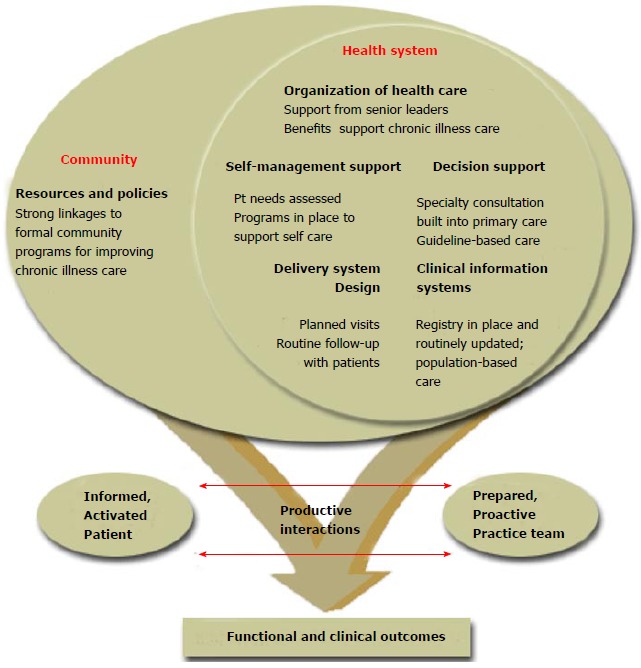
The chronic care model.
To adapt the basic principles and elements of the CCM to something actionable in developing countries, the World Health Organization[21] introduced the Innovative Care for Chronic Conditions framework (ICCCF) (Figure 2). The same essential chronic care elements specified in Wagner’s model were retained. The guiding principles of the ICCCF are evidence-based decision making, population focus, prevention focus, quality focus, integration, and adaptability. It has the following essential elements for taking action: supporting a paradigm shift, managing the political environment, building integrated health care, aligning sectoral policies for health, using health care personnel more effectively, centering care on the patient and family, supporting patients in their communities, and emphasizing prevention. The ICCCF seeks to improve health care at the macro, meso, and micro levels. However, essential components for the policy environment (macro level) are needed (leadership and advocacy, integrated policies that span different disease types and prevention strategies, consistent financing, developing human resources, legislative frameworks and partnership working), requirements that many low-to-middle-income countries, especially those encountering scarcity in human resources for health, economic crisis, and instabilities in leadership, may be unable to fulfill.
Figure 2.
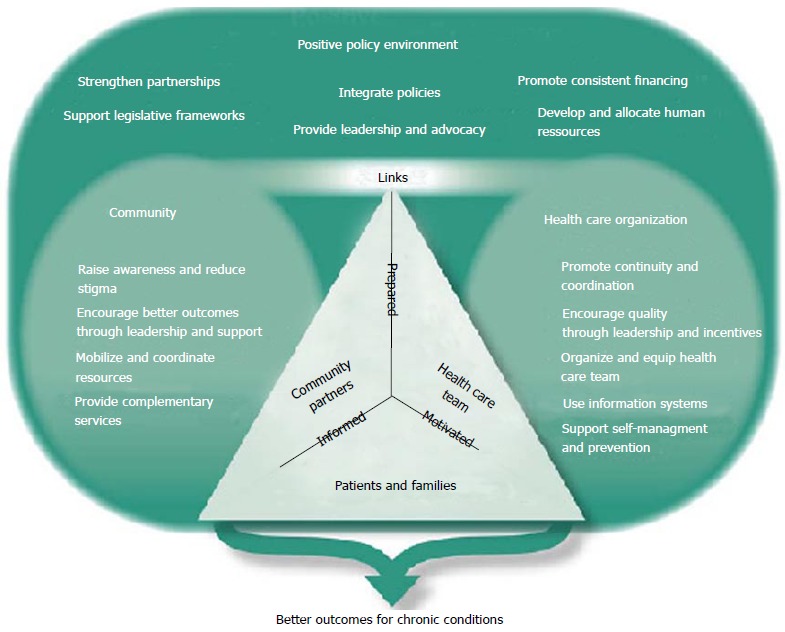
The innovative care for chronic conditions framework.
In Canada, the Province of British Columbia formulated the Expanded Chronic Care Model (Figure 3) integrating population health promotion and prevention with the existing elements of the CCM to address the social, environmental and cultural factors that affect health[22]. This way, the role of the community has become well delineated and added to the clinically focused initial CCM.
Figure 3.
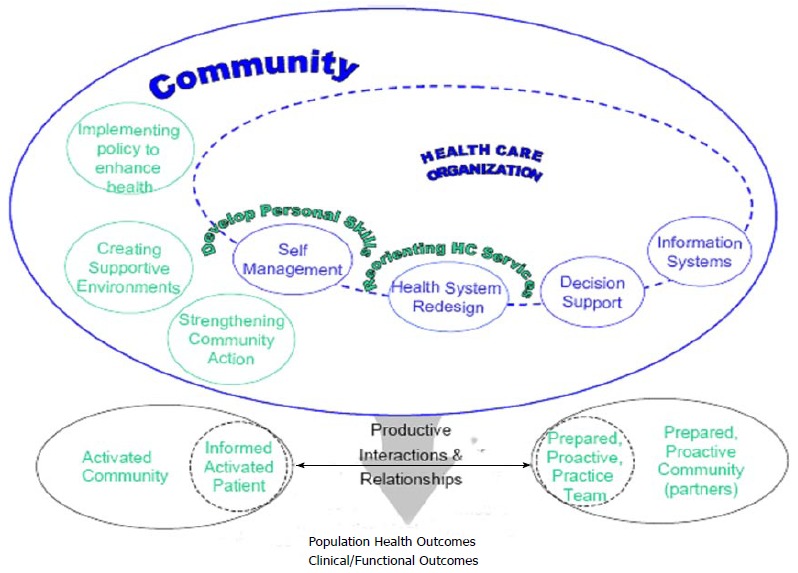
The expanded chronic care model.
Some countries chose to implement selected elements of these models. In Scotland, key principles in chronic care have been established, namely: pathways of care focused on individuals with chronic conditions; partnership between health care professionals and people with chronic conditions; partnership between primary care, social care, and other agencies; integrated solutions that respond to the needs of people with chronic conditions; focus on providing care in primary care and community settings; and focus on self-care[23].
Certain LMICs have made use of the CCM or the ICCCF to design systems of care for chronic conditions. The CCM-based Vera-Cruz Initiative for Diabetes Awareness in Mexico reports improved glycemia among its study participants 18 mo after implementation[24] while Rwanda made use of ICCCF elements to strengthen its health system and design a system of care for HIV/AIDS, with impressive results[25,26]. However, such implementations of elements of the CCM/ICCCF in LMICs are exceptions rather than the rule. The health systems response in many LMICs is still characterized by a public health system focused on prevention programs; little consideration for the organization, coordination and regulation of health care services; routine medical practice without attention to the opportunities and resources for the specific aspects of chronic care; and large out-of-pocket expenses for patients[27].
Studies conducted on the implementation of the CCM in HICs demonstrated significant correlations between specific elements of the CCM and better health outcomes[28,29]. The number of elements of the CCM and the type and intensity of implementation may vary, depending on many contextual and organizational factors[30].
THE ORGANIZATIONAL THEORIES USED
Oliver’s typology of strategic responses to institutional processes[17] lists five behaviors that organizations may enact in response to pressures toward conformity with the institutional environment: acquiescence and its alternative forms of habit, imitation, and compliance; compromise including pacifying tactics and bargaining; avoidance, concealment, buffering and escape; defiance, dismissal, challenge and attack; and manipulation including use of co-opting, influencing and controlling tactics. Oliver further states the following antecedents of strategic response: (1) the cause - why the organization is being pressured to conform to institutional norms or expectations; (2) the constituents - who are exerting institutional pressures on the organization; (3) the content - to what norms or requirements is the organization being pressured to conform; (4) the means of control - how or by what means are the institutional pressures being exerted; and (5) the context - what is the environmental context within which institutional pressures are being exerted. Ten predictive dimensions on which the response of the organization will depend are theorized from these antecedents. The investigators considered seven of these theoretical dimensions: social legitimacy; economic efficiency; external dependence on institutional constituents; consistency with organizational goals; constraints on decision-making imposed on the organization; voluntary diffusion of norms; and environmental interconnectedness. The other three dimensions namely multiplicity of constituents demands, legal coercion and environmental uncertainty, although necessary for implementation of top-down policies, were deemed to be less relevant for the present purpose, the perspective of which is rather how institutions would react to bottom-up innovations.
Greenhalgh et al[18] theorized that adoption of any intervention by an organization is variable - some interventions may be fully adopted, partially or not at all, while some may be eventually abandoned in time - and presented a unifying conceptual model for considering the different aspects of a complex situation and their many interactions. Certain attributes influence the (non)adoption of interventions based on the characteristics of the innovation, the individuals who will adopt the intervention and the system where the innovation will be assimilated. For this research, the investigators considered the following characteristics of an innovation in designing the context-adapted chronic care model-based service delivery model: relative advantage; compatibility; simplicity; trialability; observability; reinvention; risk; consideration of task issues; knowledge required; and augmentation/support. In constructing the model, the investigators envisioned a care model that could be applied in the context of an LMIC such as the Philippines, and that would engage the two main groups of stakeholders: those who are involved in the provision of care and prevention activities (the care providers, the health service/health system, and the policy makers); and the intended recipients of these activities (the person with the condition and the community members).
A 2-step situational analysis was conducted to help determine what specific interventions for chronic care could be feasibly applied to successfully organize care for chronic conditions, particularly type 2 diabetes mellitus (DM type 2), in the Philippines.
RESULTS OF THE CONTEXTUAL ANALYSIS
Results of analysis of key factors on the proposed organization of care for chronic conditions considering the current situation including awareness and level of knowledge on chronic conditions in general and on DM type 2 in particular, and skills for its care among the leaders and members of the community, the patients, the health system and the healthcare providers are listed in Table 1.
Table 1.
Key contextual factors that is expected to affect chronic care model adaptations for the development of a service delivery model for chronic conditions including type 2 diabetes mellitus
| Key factors | Analysis based on context |
| Community-related | |
| Policy | No specific policies on chronic care delivery exist at both national and local levels |
| Politics | Informal interviews with government officials suggested some awareness of chronic conditions such as DM type 2 and the needs that must be addressed for the care of chronic conditions in general and DM type 2 in particular in the political environment |
| Support | National support is limited mostly to prevention and one-day health promotion campaigns on specific chronic conditions |
| Support from private organizations and civil societies is currently untapped | |
| Awareness | Informal interviews with local government officials and community members suggested a low level of awareness of DM type 2, the care for DM type 2 and other associated factors, and the prevalence and burden of DM type 2 in the locality |
| Patient-related | |
| Support | Informal interview with healthcare staff and people with diabetes gave an impression of low level of support given to people with diabetes by the community and health services |
| Awareness | Informal interview with healthcare staff and people with diabetes gave an impression of low level of knowledge on the condition and care for the condition |
| Perceived need | Informal interview with people with diabetes revealed a moderate level of perceived need to improve care delivery for their condition |
| Perceived benefits | Informal interview with people with diabetes revealed a moderate level of perceived benefits of improving care delivery for their condition |
| Self-efficacy | Informal interview with healthcare staff and people with diabetes suggested a low level of self-efficacy in managing the condition |
| Provider-related | |
| Perceived need | Informal interview with healthcare staff revealed a high level of perceived need to improve primary care for chronic conditions |
| Perceived benefits | Informal interview with healthcare staff revealed a high level of perceived benefits of delivering good quality chronic care |
| Self-efficacy | Informal interview with healthcare staff suggested an impression of low level of self-efficacy in the provision of good quality chronic/diabetes care |
| Skill proficiency | Informal interview with healthcare staff suggested an impression of a need for skills and knowledge development regarding delivery of good quality chronic/diabetes care |
| Health service-related | |
| Leadership | The (local) government leaders and health officers are supportive of project implementation |
| Shared vision | The health system has a shared vision in improving the quality of care for chronic conditions |
| Organizational norms regarding change | The healthcare workers may be open to small, incremental changes as long as these do not lead to a drastic increase in demands on resources and workload |
| Administrative support | Administrative support for the project is limited |
DM: Diabetes mellitus.
The community, the patients, the health system and the healthcare providers were taken into consideration as these would be the key potential players in implementing any of Wagner’s six essential chronic care elements (self-management support, clinical information systems, delivery system redesign, decision support, health care organization, and community resources). The patient is central to all of these chronic care elements; the community, separately as an organized group and as a unit of government, would be responsible for the community resources; and the healthcare provider and the health service would be involved in at least five if not all of the elements.
This first analysis would indicate that there are no insurmountable barriers to the introduction of at least basic interventions for the care of chronic conditions.
The analysis of these factors was taken a step further by applying Oliver’s typology and the theories of Greenhalgh et al[18] (Table 2), which explored aspects that could affect adaptation of chronic care models towards the development of a chronic care service delivery model.
Table 2.
Contextual analysis of key factors affecting adaptation of chronic care models and subsequent selection of CACCM elements for implementation making use of Oliver’s typology and characteristics enumerated by Greenhalgh et al[18]
| CACCM- and project-related | |
| Oliver’s dimensions | |
| Social legitimacy | Improving care for chronic conditions and protection and promotion of the health and wellbeing of the LGU population enhances the social fitness of the LGHU and the local government |
| Economic efficiency | The introduction of additional activities in any organization entails additional expenses. Cost-effective or cost-saving innovations would be preferred |
| External dependence on institutional constituents | The LGHU are dependent on the LGU for funding; the LGU officials who decide on the allocation of these resources are dependent on the populace for their seats in office |
| Consistency with organizational goals | The primary goal of the LGHU is to provide good quality healthcare to the people |
| Discretionary constraints imposed on the organization | The LGHU expects full autonomy especially in substantive decision-making such as resource-allocation, resource acquisition, organizational administration, etc. |
| Voluntary diffusion of norms | A moderate to high degree of voluntary diffusion with some degree of pressure from the LGU officials to diffuse said norms may be most effective in promoting adoption of the intervention |
| Environmental interconnectedness | A certain degree of predictability of the environment is seen: the general population, especially the people with diabetes and their families will most likely appreciate the intervention. Such appreciation may be reflected on goodwill towards the LGU officials and consequently to the LGHU (for example additional budget allocated to health) |
| Greenhalgh’s characteristics | |
| Relative advantage | Implementing a diabetes-care project gives the advantage of improving the care for this condition and a number of its comorbidities, but without reduction of other health benefits |
| Compatibility | Compatibility of the intervention with current/pre-existing activities in the LGHU and with the current duties, responsibilities and workload of the LGHU staff is sought |
| Simplicity | Simplicity and ease of use of the intervention favors adoption of the intervention |
| Trialability | Flexibility in accomplishing a number of tasks, i.e., giving leeway to the healthcare staff regarding performance of activities related to the intervention will increase acceptability of the intervention |
| Observability | Providing information to the intended adopters of the benefits of the intervention, e.g., improvements of glycemia, favors adoption of the intervention |
| Reinvention | Flexibility of the intervention allowing adaptation and refinement to suit the context, the needs of the individual person with diabetes and the capabilities of the healthcare provider favors its adoption |
| Risk | Based on outcomes of previous studies conducted on implementation of chronic care models and provision of self-management education, it is certain that the benefits far outweigh the risks |
| Task issues | Workable and easy to use interventions favor adoption Relevance of the intervention to the work of the staff and tasks that may contribute to the relevance of the work of the individual health care worker is preferred However, the intervention may also be interpreted as an added workload to the LGHU staff |
| Knowledge required | Knowledge and skills required for full implementation of the intervention need to be supplied/supplemented |
| Augmentation/support | Provision of a training workshop prior to implementation increases the probability of adoption of the intervention |
LGHU: Local government health units; LGU: Local government units.
Based on these, a feasible service delivery model for DM type 2 and similar chronic conditions was constructed, taking into consideration the existing healthcare organization and design, the current duties and responsibilities of individual cadres of healthcare workers, and the chronic care activities that need to be and can be provided.
THE CONTEXT-ADAPTED SERVICE DELIVERY MODEL FOR DM TYPE 2 AND SIMILAR CHRONIC CONDITIONS
Health care reorganization to concentrate primarily on chronic care is neither feasible nor desirable for developing countries still dealing with the problems of acute diseases concurrently with the rising prevalence of chronic conditions. Gradual accommodation of care to include chronic conditions is a better choice as LMICs continue their battle against malaria, pneumonia, diarrheal diseases and other acute illnesses. With this double burden of disease, the health care system should address the care for both chronic and acute conditions in terms of a more inclusive priority setting.
As mentioned previously, creating more vertical programs with specialized structures, dedicated personnel and earmarked budget may prove more detrimental to an already-weak health system, and may inadvertently lead to inattention and cause neglect to other health issues that also need to be addressed. Primary care strengthening and capacity building of an existing health service may pave the way towards health care delivery to the people rather than prevention and care of a specific disease, moving health care towards a person-centered, comprehensive approach and veering away from being disease-centered.
LMICs can deliver prevention and care for chronic conditions such as DM type 2 by applying carefully thought-through implementation principles.
Although the care for acute and chronic diseases may seem contrasting, the people involved in health care delivery are basically not. The usual personnel complement of a health service can also be used for chronic care. Chronic care activities may range from simple, standardizable procedures that require low expertise to complex ones that require more expertise and more extensive training and education. These activities may be distributed to different types of health care personnel. A model for the delivery of chronic care services where the activities were stratified according to the level of expertise of health care personnel in LMIC was conceptualized (Figure 4). In this model, healthcare personnel may range from volunteers/community-based health workers and expert patients, constituting the health care personnel with lesser formal expertise, to paramedical personnel (midwives, nurses) to physicians (general practitioners, specialists) constituting health care personnel with more formal expertise, although the highest tier may only involve up to the nurses in certain settings. Chronic care activities may involve health promotion and prevention in the general population, among a population at risk, and a subpopulation with high risk of developing certain chronic conditions; clinical management, counseling and health education of those with good control of their chronic conditions and with stable co-morbidities; and clinical management, counseling and health education of those with poor control of their chronic conditions and/or with unstable co-morbidities.
Figure 4.
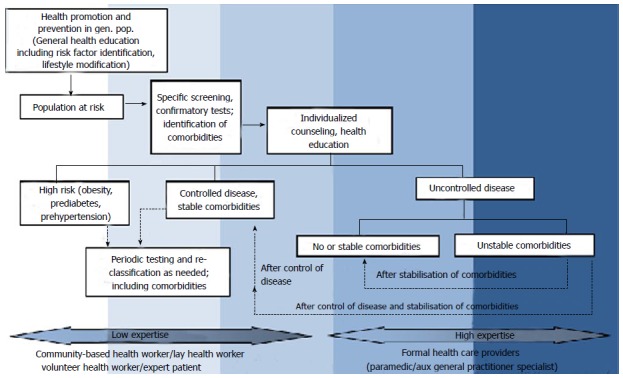
The context-adapted service delivery model for type 2 diabetes mellitus and similar chronic conditions.
For DM type 2 (and similar chronic conditions, i.e., hypertension, coronary artery disease, cerebrovascular accidents, some cancers, chronic obstructive pulmonary disease), health care workers with the least formal expertise may perform population-based health promotion and prevention activities, carry out pre-screening activities to identify a subpopulation at risk for developing DM type 2, and may follow-up on people noted to be at high risk or already identified to have prediabetes. These activities are standardizable; operating procedures and work flow diagrams/decision trees may be constructed to instruct the health care worker, and checklists may be prepared to serve as guides. On the next tier of health care workers, activities that may be assigned include specific screening or confirmatory testing for dysglycemia (DM type 2 and prediabetes), identification of co-morbidities, and counseling, health education and clinical management of patients in good glycemic control and with stable co-morbidities. Although certain guidelines and diagrams still make these activities standardizable, a higher level of expertise is expected to clinically manage optimally controlled DM type 2 and co-morbidities and to recognize and know when to refer impending instabilities; special skills also need to be developed to initiate effective communication and counseling/health education. At the higher end of the spectrum, activities are focused on those with poor glycemic control and/or unstable co-morbidities and complications, which would require clinical expertise and judgment for appropriate clinical management and counseling.
CONCLUSION
The context-adapted service delivery model for DM type 2 and similar chronic conditions may be far-removed from that in HICs, but it is designed to deliver prevention and care that encompasses the spectrum of diabetes from those at risk to those with poor glycemic control and/or unstable co-morbidities and includes counseling for self-management education and support. It is likewise designed for the general population to experience this service through general health (diabetes) education and healthy lifestyle promotion. The model incorporates care for diabetes into a current package health care activities making use of pre-existing human resources for health. It taps the potential of a workforce that may assume simple and standardizable diabetes prevention and care activities. In so doing, the additional burden on professional healthcare workers who are now required to focus attention on both acute and chronic conditions is decreased. This service delivery model, adapted to the Philippine context, may be applicable to other LMICs having a similar situation as the Philippines. The model, however, requires additional support in terms of preparing all cadres for the delivery of diabetes care. These include sustained decision support, and materials such as the flowcharts, decision trees and checklists.
Taking inspiration from models of chronic care and carefully selecting essential elements according to effectiveness potential and local feasibility can result in basic but efficient care strategies[31].
A low resource healthcare system with no specific attention at all for chronicity can be induced to include chronic/lifelong conditions among its priorities, even with minimal means. Well applied, however, such minimal means can make a lot of difference for increasing numbers of people.
Footnotes
Supported by The Belgian Directorate for Development Cooperation through the Institute of Tropical Medicine, Antwerp.
Conflict-of-interest: Neither of the authors has any financial competing interests regarding this research.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: August 29, 2014
First decision: November 27, 2014
Article in press: February 11, 2015
P- Reviewer: Nishio K S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
References
- 1.Beaglehole R, Epping-Jordan J, Patel V, Chopra M, Ebrahim S, Kidd M, Haines A. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet. 2008;372:940–949. doi: 10.1016/S0140-6736(08)61404-X. [DOI] [PubMed] [Google Scholar]
- 2.Beaglehole R, Bonita R, Alleyne G, Horton R, Li L, Lincoln P, Mbanya JC, McKee M, Moodie R, Nishtar S, et al. UN High-Level Meeting on Non-Communicable Diseases: addressing four questions. Lancet. 2011;378:449–455. doi: 10.1016/S0140-6736(11)60879-9. [DOI] [PubMed] [Google Scholar]
- 3.International Diabetes Federation. Diabetes Atlas, 5th ed, with 2012 updates. Internatonal Diabetes Federation, Brussels. 2011. [Google Scholar]
- 4.World Health Organization. Mortality and burden of disease estimates for WHO member states in 2008. Geneva: WHO; 2010. [Google Scholar]
- 5.Meessen B, Zhenzhong Z, Van Damme W, Devadasan N, Criel B, Bloom G. Iatrogenic poverty. Trop Med Int Health. 2003;8:581–584. doi: 10.1046/j.1365-3156.2003.01081.x. [DOI] [PubMed] [Google Scholar]
- 6.Stuckler D, Basu S, McKee M. Drivers of inequality in Millennium Development Goal progress: a statistical analysis. PLoS Med. 2010;7:e1000241. doi: 10.1371/journal.pmed.1000241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370:1929–1938. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 8.Longino CF, Pardeck JT, Murphy JW. Reason and rationality in health service delivery. New York: Haworth Press; 1998. [DOI] [PubMed] [Google Scholar]
- 9.de Ridder D, Geenen R, Kuijer R, van Middendorp H. Psychological adjustment to chronic disease. Lancet. 2008;372:246–255. doi: 10.1016/S0140-6736(08)61078-8. [DOI] [PubMed] [Google Scholar]
- 10.The Ljubljana Charter on reforming health care. BMJ. 1996;312:1664–1665. [PMC free article] [PubMed] [Google Scholar]
- 11.Travis P, Bennett S, Haines A, Pang T, Bhutta Z, Hyder AA, Pielemeier NR, Mills A, Evans T. Overcoming health-systems constraints to achieve the Millennium Development Goals. Lancet. 2004;364:900–906. doi: 10.1016/S0140-6736(04)16987-0. [DOI] [PubMed] [Google Scholar]
- 12.Grundy J, Healy V, Gorgolon L, Sandig E. Overview of devolution of health services in the Philippines. The International Journal of Rural and Remote Health Research, Education, Practice and Policy, online 2003-7-1, cited 2013-9-4. Available from: http://www.rrh.org.au/articles/subviewnew.asp?ArticleID=220. [PubMed]
- 13.Phillips DR. Primary health care in the Philippines: banking on the barangays? Soc Sci Med. 1986;23:1105–1117. doi: 10.1016/0277-9536(86)90269-8. [DOI] [PubMed] [Google Scholar]
- 14.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 15.Department of Health. Annual calendar of activities 2013, cited 2013-2-7. Available from: http://www.doh.gov.ph/annual_calendar.html.
- 16.Philippine Society of Nephrologists. Philippine Renal Disease Registry 2007 Annual Report. Quezon City: National Kidney Transplant & Institute; 2008. [Google Scholar]
- 17.Oliver C. Strategic responses to institutional processes. AMR. 1991:16: 145–179. [Google Scholar]
- 18.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1:2–4. [PubMed] [Google Scholar]
- 20.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organisation. Innovative care for chronic conditions: building blocks for action: global report. Geneva: WHO; 2007. [Google Scholar]
- 22.Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D, Salivaras S. The expanded Chronic Care Model: an integration of concepts and strategies from population health promotion and the Chronic Care Model. Hosp Q. 2003;7:73–82. doi: 10.12927/hcq.2003.16763. [DOI] [PubMed] [Google Scholar]
- 23.Singh D, Ham D. Improving care for people with long-term conditions: a review of UK and international frameworks. Birmingham: University of Birmingham Health Services Management Center and the National Health Systems Institute on Innovation and Improvement; 2006. [Google Scholar]
- 24.Pan American Health Organization. Innovative care for chronic conditions: Organizing and delivering high quality care for chronic non-communicable diseases in the Americas. Washington, DC: PAHO; 2013. [Google Scholar]
- 25.Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the quality of health care for chronic conditions. Qual Saf Health Care. 2004;13:299–305. doi: 10.1136/qshc.2004.010744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Farmer PE, Nutt CT, Wagner CM, Sekabaraga C, Nuthulaganti T, Weigel JL, Farmer DB, Habinshuti A, Mugeni SD, Karasi JC, et al. Reduced premature mortality in Rwanda: lessons from success. BMJ. 2013;346:f65. doi: 10.1136/bmj.f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ku GM, Idrissi A, Bhojani U, Kifle A, Chenge F. Analyzing health systems to make them stronger: Organisation of Health (Care) Systems for Chronic Diseases [Accessed 15 November 2013] Available from: http: //www.strengtheninghealthsystems.be/topic5_2.html.
- 28.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009;28:75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nutting PA, Dickinson WP, Dickinson LM, Nelson CC, King DK, Crabtree BF, Glasgow RE. Use of chronic care model elements is associated with higher-quality care for diabetes. Ann Fam Med. 2007;5:14–20. doi: 10.1370/afm.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cretin S, Shortell SM, Keeler EB. An evaluation of collaborative interventions to improve chronic illness care. Framework and study design. Eval Rev. 2004;28:28–51. doi: 10.1177/0193841X03256298. [DOI] [PubMed] [Google Scholar]
- 31.Ku GMV, Kegels G. Changes in knowledge, attitudes, self-management practices and glycemic control: effects of the First Line Diabetes Care (FiLDCare) diabetes self-management education and support project in the Northern Philippines. BMJ Open, online publication 2014-8-12, cited 2014-8-25. Available from: http://bmjopen.bmj.com/content/4/8/e005317.full. [DOI] [PMC free article] [PubMed]


