Abstract
Objectives
To investigate the effect of Lawsonia inermis total methanolic extract (LIE) and octreotide (OC) on hepatocellular carcinoma (HCC) progression, depending on somatostatin receptor 2 (SSTR-2) and Alfa fetoprotein (AFP) perturbations.
Methods
Sixty albino mice, divided into five groups (12/each); all except control were injected with single diethyl nitrosamine (DENA) dose of 90 mg/kg body weight, intraperitoneally (IP). DENA group was killed at the last day of week 18. LIE group was given 200 mg/100 ml drinking water from first day of DENA injection until end of week 18. OC group received OC (0.1 mg/kg body weight, twice daily by subcutaneous injection, SC from the first day of week 17 till end of week 18. LIE + OC was given medications till the last day of week 18. Serum AFP, liver tissue SSTR-2 mRNA, its protein expression, reduced glutathione (GSH) and malondialdehyde (MDA) were analyzed.
Results
A significant increase in plasma AFP and hepatic mRNA, associated to liver tissue neoplastic changes, SSTR-2 expression and MDA with decreased hepatic GSH were observed in DENA group. These changes were significantly improved by LIE and/or OC.
Conclusions
LIE and/or OC treatment has effective chemopreventive action due to their ability to alleviate oxidative stress, desensitizing cellular growth receptor to SST.
Keywords: Hepatocarcinoma, SSTR-2, Lawsonia, Octreotide
Introduction
Hepatocellular carcinoma (HCC) ranks the fifth among malignancies worldwide, representing the third largest cause of cancer-related death, with an estimated mortality rate of about one million deaths annually and an incidence-to-mortality ratio very close to one [1]. Incidence of HCC has dramatically increased worldwide in both sexes and all races in the past two decades. Despite advances in its clinical study, the prognosis of HCC, which afflicts over 700,000 people worldwide annually, remains dismal. Liver cancer rapidly reduces quality of life and typically causes death 0.5–1 year from diagnosis [2].
Recently, research has focused on exploring many therapeutic trials for management of HCC. The discovery of chemotherapeutic agents for HCC is important to reduce the mortality caused by this affliction [3]. Significant efforts have focused on novel phytoceuticals in search of cancer inhibitors and cures. Extracts from natural products such as fruits, vegetables and medicinal herbs have positive effects against cancer compared with chemotherapy or recent hormonal treatments [4].
Somatostatin [also known as growth-inhibiting hormone (GIH) or somatotropin release-inhibiting factor (SRIF)] is a peptide hormone that regulates the endocrine system, and affects neurotransmission, cell proliferation via interaction with G-protein-coupled somatostatin receptors and inhibition of the release of numerous secondary hormones. The neuropeptide SST is widely distributed in the central and peripheral nervous system, and known to play important role in the endocrine, autocrine and paracrine functions in living organisms [5]. Basically, studies on SST metabolism have unified diverse concepts in intracellular signal transduction and eukaryotic gene expression [6, 7].
There are predominantly 2 biologically active forms of SST: SST-14 and SST-28.
SST acts on its multiple cell targets via a family of 6 receptors that originate from five genes: SSTR1, SSTR2a, SSTR2b, SSTR3, SSTR4, SSTR5. SSTR-2 is alternatively spliced at its C-terminus producing the SSTR2a and the SSTR2b variants that have a somewhat different tissue distribution [8].
The therapeutic potential of somatostatin remains unfulfilled due to its short half-life (plasma half-life = 1 min), though its tissue expression was recently pointed out in early HCC progression [9, 10]. However, a highly potent somatostatin analog was developed with increased stability [9, 11]. Some of these analogs like RC-160, OC and BIM23014 exhibit a marked increased stability in circulation (half-life = 2 h) and are at least 50 times more potent than somatostatin in inhibiting GH secretion in vivo. The antiproliferative activity of SST agonists like OC, lanreotide and RC-160 has been demonstrated in vitro in several breast, renal, lung, prostate, cervical, and colon cancer cell lines [12, 13].
Lawsonia inermis, also known as Henna or Mhendi, is abundantly available in tropical and subtropical areas. Ancient history of India describes its diverse uses and also plays appreciable role in natural herbal medicines [14, 15]. Main chemical components are lawsone, esculetin, fraxetin, isoplumbagin, scopoletin, betulin, betulinic acid, hennadiol, lupeol, lacoumarin, quinone and napthaquinone. Different solvents including methanol, ethanol, acetone, chloroform, hexane and water were used to prepare extracts of henna leaves [16]. Henna leaves, flowers, seeds, stem bark and roots are used in traditional medicine to treat a variety of ailments as rheumatoid arthritis, headache, ulcers, diarrhea, leprosy fever, leucorrhea, diabetes, cardiac disease, hepatoprotective and coloring agent [17].
The present work was conducted to look for a possible supplementary effect of Lawsonia inermis extract (LIE) with/or without octreotide (OC) on HCC progression. This was assessed by measuring the somatostatin receptor 2 (SSTR-2) expression along with serum Alfa fetoprotein (AFP) expression during hepatocellular carcinoma (HCC) development stages.
Materials and methods
Animals
N.B: The institutional and national guidelines for the care and use of laboratory animals were observed. The research protocol was approved by the institutional committee for animal research. Sixty male albino mice (6-week old) weighing from 20 to 25 g were used in this study; they were kept for 2 days to accommodate on laboratory conditions, under constant environmental and nutritional conditions. Mice were fed normal food and water all over the period of the experiment unless otherwise mentioned.
Chemicals
SSTR-2 antibody was obtained from Santa Cruz Technology, Inc, UK (cat No. sc-25676). Octreotide (Sandostatin) was obtained from Novartis Pharma Company, Egypt. Secondary antibody: peroxidase-labeled anti-rabbit antibody was obtained from Amersham™ company (cat No.NIF824). Detection kit: obtained from Amersham™ company (cat No. RPN2108). Diethyl nitrosamine (DEN) (cat. No. N0258-1E) was purchased from Sigma Chemical Company St Louis, MO, USA. Total methanolic extract of Lawsonia inermis was kindly provided by Associate Professor Ehab Al-Khayat, Department of Pharmacognosy, Faculty of Pharmacy Al-Azhar University, Egypt. The powdered plant leaves (10 g) were extracted with 100 ml of methanol (70 %) for 1 h on an ultrasonic bath. The extract was filtered; the filtrate was evaporated in vacuum at 45 °C and then lyophilized. The total methanolic extract of henna possesses 7 compounds, p-coumaric acid, lawsone, apigenin, luteolin, 2-methoxy-3-methyl-1,4-naphthoquinone as well as cosmosiin and apiin [18]. RNA extraction kit from Omega Bio-tek and RT-PCR kit using preMix kit (Bioron). All the other chemicals and solvents used in the study were of analytical grade and were obtained either from Sigma Chemical Company or commercial suppliers, unless otherwise mentioned.
Experimental design
It comprised five groups (12 mice per group). HCC was induced in all groups (except normal control) by subnecrotic dose of DENA 90 mg/kg body weight in 0.9 % normal saline, intraperitoneally (IP), according to Sharma et al. [19], then selected groups were either treated with octreotide and/or total methanolic extract of Lawsonia inermis as follows:
(1) Normal control group: served as untreated healthy group, it was killed after 18 weeks. (2) DENA control group: was given a single sub-necrogenic IP dose of DENA (90 mg/kg body weight). This group was killed at the end day of week 18. (3) Octreotide (OC)-treated group: they were given subcutaneous doses of octreotide, twice daily (0.1 mg/kg body weight), from the first day of week 17 till the last day of week 18 (i.e., for 2 weeks) [20]. (4) Lawsonia-treated group: it was given ethanolic extract of Lawsonia inermis (LIE) mixed with drinking water in a dose of 200 mg/100 ml drinking water from the second day of DENA injection until the last day of week 18 [21]. (5) Lawsonia + octreotide (LIE + OC)-treated group: it was given LIE mixed with drinking water in a dose of 200 mg/100 ml drinking water from the second day to DENA injection and also was given twice daily SC injection of OC (0.1 mg/kg body weight) from the first day of the week 17 till the last day of week 18.
Sample preparation
At the end of time point for each group, mice were anesthetized with diethyl ether and killed. The livers were excised rapidly and divided into three parts: the first part was subjected for RNA preparation, the second part was homogenized in 0.25 M sucrose solution and stored at −80 °C, and the last part was fixed in 10 % neutral buffered formalin for histology examination.
Liver histopathology
Histological examination was performed on liver samples, stained with hematoxylin and eosin.
RNA extraction
RNA extraction was done using E. Z. N. A. Total RNA kit (Omega bio-tek) according to the instructions of the manufacturer.
RT-PCR procedure
This process was done using RT/PCR Pre Mix kit (Bioron). The premix tubes contain all the components necessary for cDNA synthesis and PCR amplification.
Western blotting
Up on determination of individual protein concentrations of the samples prepared for loading, aliquots of extracted hepatic samples [22] were examined by SDS-PAGE followed by immunoblotting. Cross-reacting bands were visualized by enhanced chemiluminescence (ECL) and X-ray development.
Biochemical analysis
Liver contents of both malondialdehyde (MDA), in the form of thiobarbituric acid reactive oxygen species (TBARS) and reduced glutathione (GSH) were determined [23, 24], respectively. The concentration of lipid peroxidation product, MDA, was determined using the thiobarbituric acid. 2 ml thiobarbituric acid was added to the 200 μL supernatant and boiled for 10 min in water bath. Absorbance of the color was measured at λ 530 nm. Concentration of MDA in supernatant of liver homogenate was calculated using a series of standard solution (0, 0.625, 1.25, 2.5, 5.0 nmol/ml). MDA was expressed as µM/500 mg wet tissue liver tissue. The concentration of the tissue non-enzymatic antioxidant, GSH, was determined using the dithiobisnitrobenzoate (DTNB) solution. Two hundred and fifty microliter liver homogenate was added into 8.9 ml 0.1 M, phosphate buffer saline (pH 7). Then, 5 % TCA was added to precipitate the protein. After centrifugation, 50 μL DTNB was added to the supernatant of liver homogenate and incubated for an hour. The produced color of the substance was measured at λ 412 nm. GSH content was computed using a standard curve of GSH standard concentrations (0, 10, 20, 40, 50, 100 mg/ml). The concentration of GSH in liver tissue was expressed as µM/500 mg wet tissue.
Statistical analysis
This was performed using Graph pad Prism 5 statistical software.
Results
Histopathological examination of hepatic tissues
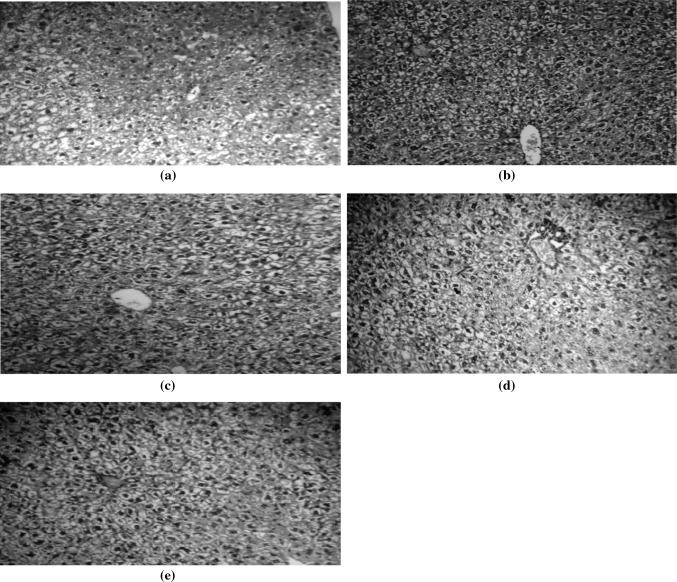
Control hepatic tissues showed normal cellular morphology (Fig. 1a). Cancer control group (DENA) showed increased cellular and nuclear pleomorphism with multi-nucleated giant cells and increased nuclear/cytoplasm (N/C) ratio (Fig. 1b). Octreotide-treated group showed marked decrease in the N/C ratio compared to cancer control (Fig. 1c). Lawsonia-treated group also showed a marked decrease in the N/C ratio, with less prominent nuclei compared to cancer control (Fig. 1d). (Lawsonia and Octreotide)-treated group: mild pleomorphism, low-grade mono-nucleated giant cells, less prominent nuclei, and marked decrease in N/C ratio in comparison to the cancer control (Fig. 1e).
Fig. 1.
Histopathological examination of hepatic tissues. a Normal hepatic tissue sections showing normal cellular architecture with no sinusoidal growth pattern, or increased nuclear/cytoplasmic ratio (H&E × 100). b Hepatic tissue section of cancer control animals showing cellular and nuclear pleomorphism, multi-nucleated giant cells and increased nuclear/cytoplasm (N/C) ratio (H&E × 100). c Hepatic tissue section of Lawsonia-treated animals showing marked decrease in the N/C ratio, and less prominent nuclei (H&E × 100). d Hepatic tissue section of Octreotide-treated group showing marked decrease in the N/C ratio (H&E × 100). e Hepatic tissue section of (Lawsonia and octreotide)-treated animals showing marked decrease in cellular & nuclear pleomorphism and N/C ratio, and less prominent nuclei (H & E × 100)
RT-PCR analysis
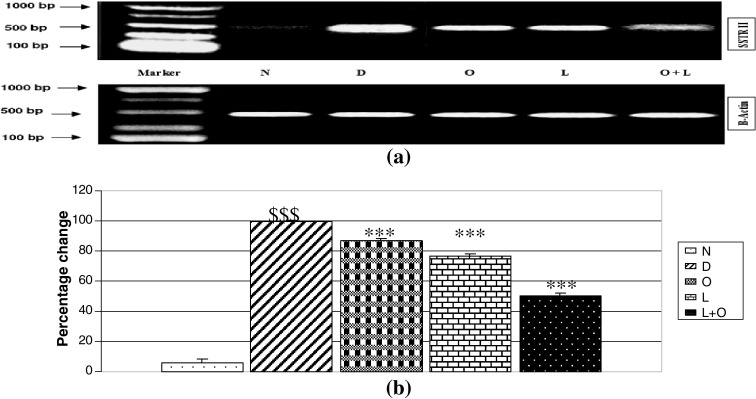
Evaluation of SSTR-2 mRNA expression
Expression of SSTR-2 mRNA was significantly (p < 0.05) increased in DENA-treated group (≈17-fold) compared to normal control. On the other hand, the level of SSTR-2 mRNA was significantly (p < 0.05) decreased about 13, 23 and 49 % in Lawsonia-treated group, octreotide-treated group and (Lawsonia and octreotide)-treated group respectively compared to DENA control group as shown in (Fig. 2a, b).
Fig. 2.
RT-PCR analysis. a SSTR-2 mRNA expression. b Percentage change in SSTR-2 mRNA expression. Data were expressed as X ± SD of three separate experiments. Dollar compared to normal control (N). Asterisk compared to DENA control. Significant difference between groups is analyzed by one-way ANOVA test, where $$$, ***P < 0.001 highly significant, **P < 0.01 significant, *P < 0.05 mildly significant, ns P > 0.05 non significant. D DENA, L LIE, O OC, L + O LIE + OC
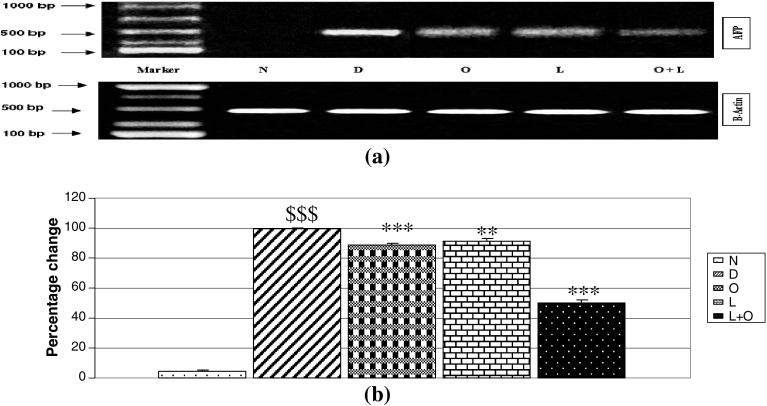
Measurement of AFP mRNA expression
Expression of AFP mRNA was significantly (p < 0.05) increased in DENA-treated group (≈22 folds) compared to normal control. On the other hand, the level of AFP mRNA was significantly decreased (p < 0.05) about 11, 9 and 49 % in Lawsonia-treated group, octreotide-treated group and (Lawsonia and octreotide)-treated group respectively compared to DENA control group as shown in (Fig. 3a, b).
Fig. 3.
Analysis of AFP mRNA expression. a AFP mRNA expression. b Percentage change in AFP mRNA expression. Data were expressed as X ± SD of three separate experiments. Dollar compared to normal control (N). Asterisk compared to DENA control. Significant difference between groups is analyzed by one-way ANOVA test, where $$$, ***P < 0.001 highly significant, **P < 0.01 significant, *P < 0.05 mildly significant, ns P > 0.0 non significant. D DENA, L LIE, O OC, L + O LIE + OC
Western blotting
Measurement of SSTR-2 protein expression in liver tissue
Expression of SSTR-2 protein was significantly (p < 0.05) increased in DENA-treated group (≈16-fold) compared to normal control. On the other hand, the level of SSTR-2 protein was significantly (p < 0.05) decreased about 26, 38 and 45 % in Lawsonia-treated group, octreotide-treated group and (Lawsonia and octreotide)-treated group respectively compared to DENA control group as shown in (Fig. 4a, b).
Fig. 4.
Biochemical analysis. a Protein expression of SSTR-2 in liver tissue. b Percentage change in SSTR-2 protein expression. Data were expressed as X ± SD of three separate experiments. Dollar compared to normal control (N). Asterisk compared to DENA control. Significant difference between groups is analyzed by one-way ANOVA test, where $$$, ***P < 0.001 highly significant, **P < 0.01 significant, *P < 0.05 mildly significant, ns P > 0.05 non significant. N control, D DENA, L LIE, O OC, L + O LIE + OC
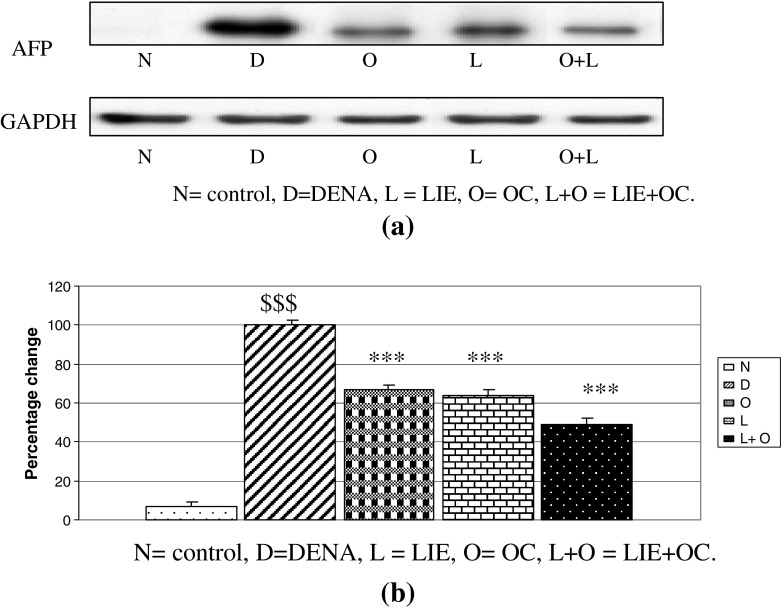
Measurement of AFP protein expression in liver tissue
Expression of AFP protein was significantly (p < 0.05) increased in DENA-treated group (≈15-fold) compared to normal control. On the other hand, the level of AFP protein was significantly (p < 0.05) decreased about 33, 36 and 51 % in Lawsonia-treated group, octreotide-treated group and (Lawsonia and octreotide)-treated group respectively compared to DENA control group as shown in Fig. 5a, b.
Fig. 5.
a Protein expression of AFP in liver tissue. b Percentage change in AFP protein expression. Data were expressed as X ± SD of three separate experiments. Dollar compared to normal control (N), Asterisk compared to DENA control, Significant difference between groups is analyzed by one-way ANOVA test, where $$$, ***P < 0.001 highly significant, **P < 0.01 significant, *P < 0.05 mildly significant, ns P > 0.05 non significant. N control, D DENA, L LIE, O OC, L + O LIE + OC
Biochemical parameters
Hepatic content of reduced glutathione
The hepatic tissue content of GSH was significantly decreased in DENA control group (≈39 %) compared to normal control. On the other hand, hepatic tissue content of GSH was significantly increased by 1.7-, 1.4- and 2.1-fold in Lawsonia, Octreotide, and (Lawsonia and octreotide)-treated group respectively compared to DENA control as shown in Table 1.
Table 1.
Hepatic content of reduced glutathione (GSH) and malondialdehyde (MDA)
| Parameter | Group | ||||
|---|---|---|---|---|---|
| Normal control (N) | DENA control (D) | Lawsonia (L) | Octreotide (O) | Octreotide + lawsonia (L + O) | |
| GSH content (µM/500 mg) wet tissue | 3.3 ± 0.2 | 1.311 ± 0.08727a | 2.188 ± 0.0999a | 1.804 ± 0.1309b | 2.758 ± 0.1033a |
| MDA content (µM/500 mg) wet tissue | 29.1 ± 1.7 | 148.6 ± 9.8a | 92.85 ± 8.9a | 113.6 ± 8.6b | 54.08 ± 5a |
Data are presented as mean ± SE, n = 10, multiple comparisons were done using one-way ANOVA followed by Tukey–Karmer as post ANOVA test
D DENA, L LIE, O OC, L + O LIE + OC
aHighly significantly different from corresponding control at P < 0.001
bSignificantly different from control group at P < 0.05, D group was compared to normal control, L, O and L + O groups were compared to DENA control
Hepatic content of malondialdehyde (MDA) (measured as TBARS)
The hepatic tissue content of MDA was significantly increased in DENA control group (≈5-fold) compared to normal control. On the other hand, hepatic tissue content of MDA was significantly decreased by 42, 23 and 64 % in Lawsonia-, Octreotide-, and (Lawsonia and octreotide)-treated group respectively compared to DENA control as shown in Table 1.
Discussion
Hepatocellular carcinoma is one of the most misdiagnosed and resistant cancers, that is why recent research focus on the discovery of specific and sensitive markers and alternative medications. In this study, we tried to investigate the probable curative effect of Lawsonia inermis extract and/or octreotide on experimental HCC progression depending on SSTR-2, in parallel to AFP expression as follow-up tools.
In the present study, DENA-treated groups showed significant premalignant morphological abnormalities manifested by histological examination. DENA was known to induce damage in many enzymes involved in DNA repair and induce liver cancer in experimental animals [25, 26]. Our study also exhibited marked increase in the RNA and protein expression of AFP in DENA-treated group in accordance with many previous studies [27, 28].
Somatostatin receptors are not expressed in normal hepatocytes, in contrast to the HCC hepatocyte, where these receptors are frequently expressed, with the SSTR-2 subtype being predominant [29]. Our results showed marked increase in the mRNA expression and protein synthesis of SSTR-2 prior to HCC development. Up-regulation of SSTRs during liver disease is in agreement with previous findings reported that SSTRs are expressed in diseased, not normal liver [30]. The reason why SSTRs are up-regulated during liver injury remains to be elucidated but it has been demonstrated that cytokines, growth factors, and somatostatin regulate SSTR gene expression [31].
The main question is: Does activation of these receptors have antitumor effects and, if so, through which receptor(s)? It has been shown previously that antitumor effects of somatostatin in other tumors are mediated directly by receptors present on the tumor cells resulting in growth arrest, apoptosis, or inhibition of migration and indirectly via inhibition of release of growth factors or cytokines, modulation of immune cells, and inhibition of neoangiogenesis [32]. It has been shown that octreotide competes with insulin-like growth factor in human hepatoma cells, decreasing bioactivity of insulin-like growth factor, a well-recognized mitogen for hepatoma cells [33].
Damage due to oxidative stress and free radicals is one of the important factors in hepatocarcinogenesis. GSH is a very important factor in detoxification, while MDA is a sign of lipid peroxidation [34]. Our work revealed that DENA significantly increased TBARS and decreased GSH in liver tissues. These actions had been reported in many models of DENA-induced HCC [35, 36].
In this study, octreotide showed significant anti-cancer properties by reversing most of the histological and biochemical perturbations observed in DENA-treated groups. It is believed that octreotide can inhibit the growth of a variety of tumors, either directly, through binding on the SSTRs of tumor cells, or indirectly, through an immunomodulatory or an antiangiogenic effect [37, 38]. Several reports indicate that octreotide inhibits the proliferation and induces apoptosis in HepG2 cell line [39–41]. Similarly, clinical trials have demonstrated a survival benefit of patients with inoperable HCC treated with OC [29, 42], although some negative studies have been published [43]. This contradiction may be due to failure of selective criteria for patients recruited to OC treatment program, Yuen et al. in this study, selected patients with short expected survival. So, our study will certainly help newly discovered subjects with moderate or higher expected survival. This was confirmed by Kouroumalis et al. [44].
The antiproliferative effect of octreotide is thought to be mediated by SSTR-2 [32] and SSTR-5 [45]. Even when a significant amount of SSTR-2 binding in cellular membranes is not evident, it is possible that octreotide is internalized either along with SSTR-2 or alone [46, 47]. The antiproliferative effect of octreotide may be due to either cell necrosis or apoptosis [20]. Mediated by SSTR-2, octreotide upregulates tumor necrosis factor-related apoptosis-inducing ligand (TRAIL), death receptor 4 (DR4) and downregulates Bcl-2, which results in apoptosis [48, 49].
The effect of LIE is referred mainly to its flavonoid content and coloring p-coumaric acid, lawsone, apigenin, luteolin, 2-methoxy-3-methyl-1,4-naphthoquinone as well as cosmosiin and apiin in depressing cancer cell growth [50].
In conclusion, Lawsonia inermis and/or octreotide can be regarded as a beneficial chemopreventive combination therapy to unoperable HCC. LIE, by normalizing the peroxidative tendency, through elevating available GSH, depressing MDA production and SST expression, introduced a more suitable microenvironment to the cellular action of OC. This relied on their modulatory action on SSTR-2 mRNA and protein expression, along with efficient improvement of oxidative stress within the hepatocytes. This was proved by both histological improvement and retraction of AFP mRNA and protein overexpression up on hepatocarcinogenesis.
References
- 1.Abdel-Hamid NM. Recent insights on risk factors of hepatocellular carcinoma. World J Hepatol. 2009;1(1):3–7. doi: 10.4254/wjh.v1.i1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bosch FX, Ribes J, Cleries R, Diaz M. Epidemiology of hepatocellular carcinoma. Clin Liver Dis. 2005;9(2):191–211. doi: 10.1016/j.cld.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 3.Kaufmann SH, Earnshaw WC. Induction of apoptosis by cancer chemotherapy. Exp Cell Res. 2000;256(1):42–49. doi: 10.1006/excr.2000.4838. [DOI] [PubMed] [Google Scholar]
- 4.Abdel-Hamid NM, Abdel-Ghany MI, Nazmy MH, Amgad SW. Can methanolic extract of Nigella sativa seed affect glyco-regulatory enzymes in experimental hepatocellular carcinoma? Environ Health Prev Med. 2013;18(1):49–56. doi: 10.1007/s12199-012-0292-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferjoux G, Lopez F, Esteve JP, Ferrand A, Vivier E, Vely F, Saint-Laurent N, Pradayrol L, Buscail L, Susini C. Critical role of src and SHP-2 in sst2 somatostatin receptor-mediated activation of SHP-1 and inhibition of cell proliferation. Mol Biol Cell. 2003;14(9):3911–3928. doi: 10.1091/mbc.E03-02-0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weckbecker G, Raulf F, Stolz B, Bruns C. Somatostatin analogs for diagnosis and treatment of cancer. Pharmacol Ther. 1993;60(2):245–264. doi: 10.1016/0163-7258(93)90009-3. [DOI] [PubMed] [Google Scholar]
- 7.Weckbecker G, Lewis I, Albert R, Schmid HA, Hoyer D, Bruns C. Opportunities in somatostatin research: biological, chemical and therapeutic aspects. Nat Rev Drug Discov. 2003;2(12):999–1017. doi: 10.1038/nrd1255. [DOI] [PubMed] [Google Scholar]
- 8.Reubi JC, Waser B. Concomitant expression of several peptide receptors in neuroendocrine tumours: molecular basis for in vivo multireceptor tumour targeting. Eur J Nucl Med Mol Imaging. 2003;30(5):781–793. doi: 10.1007/s00259-003-1184-3. [DOI] [PubMed] [Google Scholar]
- 9.Abdel-Hamid NM, Mohafez OM, Zakaria S, Thabet K. Hepatic somatostatin receptor 2 expression during premalignant stages of hepatocellular carcinoma. Tumour Biol. 2014;35(3):2497–2502. doi: 10.1007/s13277-013-1330-x. [DOI] [PubMed] [Google Scholar]
- 10.Abdel-Hamid NM, Mohafez OM, Zakaria S, Thabet K. Hepatic somatostatin receptor 2 expression during premalignant stages of hepatocellular carcinoma. Tumour Biol. 2014;35(3):2497–2502. doi: 10.1007/s13277-013-1330-x. [DOI] [PubMed] [Google Scholar]
- 11.Hannon JP, Nunn C, Stolz B, Bruns C, Weckbecker G, Lewis I, Troxler T, Hurth K, Hoyer D. Drug design at peptide receptors: somatostatin receptor ligands. J Mol Neurosci. 2002;18(1–2):15–27. doi: 10.1385/JMN:18:1-2:15. [DOI] [PubMed] [Google Scholar]
- 12.Dasgupta P, Singh A, Mukherjee R. N-terminal acylation of somatostatin analog with long chain fatty acids enhances its stability and anti-proliferative activity in human breast adenocarcinoma cells. Biol Pharm Bull. 2002;25(1):29–36. doi: 10.1248/bpb.25.29. [DOI] [PubMed] [Google Scholar]
- 13.Lamberts SW, de Herder WW, Hofland LJ. Somatostatin analogs in the diagnosis and treatment of cancer. Trends Endocrinol Metab. 2002;13(10):451–457. doi: 10.1016/S1043-2760(02)00667-7. [DOI] [PubMed] [Google Scholar]
- 14.Gupta A. Quality standards of Indian medicinal plants. Indian Counc Med Res. 2003;1:123–129. [Google Scholar]
- 15.Lavhate MSMS. A review: nutritional and therapeutic potential of Ailanthus excelsa. Pharmacog Rev. 2007;1(1):105–113. [Google Scholar]
- 16.Khodaparast H. HMaZD: phenolic compounds and antioxidant activity of henna leaves extracts. Dairy Food Sci. 2007;2(1):38–41. [Google Scholar]
- 17.Madhava Chetty K, Sivaji K, Tulsi Rao K. Flowering plants of Chittoor district, Andhra Pradesh, India. 1. Tirupati: Students Offset printers; 2008. [Google Scholar]
- 18.Mikhaeil BR, Badria FA, Maatooq GT, Amer MM. Antioxidant and immunomodulatory constituents of henna leaves. Z Naturforsch C. 2004;59(7–8):468–476. doi: 10.1515/znc-2004-7-803. [DOI] [PubMed] [Google Scholar]
- 19.Sharma ASNaR. Studies on mode of action of hexaammine co(iii) chloride against diethylnitrosamine-induced hepatocarcinogenesis in mice. J Biochem Mol Toxicol. 2009;3(3):193–201. doi: 10.1002/jbt.20280. [DOI] [PubMed] [Google Scholar]
- 20.Hua YP, Yin XY, Peng BG, Li SQ, Lai JM, Liang HZ, Liang LJ. Mechanisms and influence of octreotide-induced regulation of somatostatin receptor 2 on hepatocellular carcinoma. Chemotherapy. 2009;55(5):312–320. doi: 10.1159/000227763. [DOI] [PubMed] [Google Scholar]
- 21.Dasgupta TRA, Yadava PK. Modulatory effect of Henna leaf (Lawsonia inermis) on drug metabolising phase I and phase II enzymes, antioxidant enzymes, lipid peroxidation and chemically induced skin and forestomach papillomagenesis in mice. Mol Cell Biochem. 2003;245:11–22. doi: 10.1023/A:1022853007710. [DOI] [PubMed] [Google Scholar]
- 22.Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein–dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 23.Mihara M, Uchiyama M. Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal Biochem. 1978;86(1):271–278. doi: 10.1016/0003-2697(78)90342-1. [DOI] [PubMed] [Google Scholar]
- 24.Ellman GL. Tissue sulfhydryl groups. Arch Biochem Biophys. 1959;82(1):70–77. doi: 10.1016/0003-9861(59)90090-6. [DOI] [PubMed] [Google Scholar]
- 25.Brown JL. N-Nitrosamines. Occup Med. 1999;14(4):839–848. [PubMed] [Google Scholar]
- 26.Bhosale PML, Ingle AD, Gadre RB, Rao KVK. Protective effect of Rhodotorula glutinis NCIM3353 on the development of hepatic preneoplastic lesions. Curr Sci. 2002;83:303–308. [Google Scholar]
- 27.Kew MC. Hepatocellular cancer. A century of progress. Clin Liver Dis. 2000;4(1):257–268. doi: 10.1016/S1089-3261(05)70107-0. [DOI] [PubMed] [Google Scholar]
- 28.Johnson PJ. The role of serum alpha-fetoprotein estimation in the diagnosis and management of hepatocellular carcinoma. Clin Liver Dis. 2001;5(1):145–159. doi: 10.1016/S1089-3261(05)70158-6. [DOI] [PubMed] [Google Scholar]
- 29.Kouroumalis E, Skordilis P, Thermos K, Vasilaki A, Moschandrea J, Manousos ON. Treatment of hepatocellular carcinoma with octreotide: a randomised controlled study. Gut. 1998;42(3):442–447. doi: 10.1136/gut.42.3.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reynaert H, Rombouts K, Jia Y, Urbain D, Chatterjee N, Uyama N, Geerts A. Somatostatin at nanomolar concentration reduces collagen I and III synthesis by, but not proliferation of activated rat hepatic stellate cells. Br J Pharmacol. 2005;146(1):77–88. doi: 10.1038/sj.bjp.0706298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel YC. Somatostatin and its receptor family. Front Neuroendocrinol. 1999;20(3):157–198. doi: 10.1006/frne.1999.0183. [DOI] [PubMed] [Google Scholar]
- 32.Ferjoux G, Bousquet C, Cordelier P, Benali N, Lopez F, Rochaix P, Buscail L, Susini C. Signal transduction of somatostatin receptors negatively controlling cell proliferation. J Physiol Paris. 2000;94(3–4):205–210. doi: 10.1016/S0928-4257(00)00206-0. [DOI] [PubMed] [Google Scholar]
- 33.Reynaert H, Rombouts K, Vandermonde A, Urbain D, Kumar U, Bioulac-Sage P, Pinzani M, Rosenbaum J, Geerts A. Expression of somatostatin receptors in normal and cirrhotic human liver and in hepatocellular carcinoma. Gut. 2004;53(8):1180–1189. doi: 10.1136/gut.2003.036053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reed JC. Mechanisms of apoptosis. Am J Pathol. 2000;157(5):1415–1430. doi: 10.1016/S0002-9440(10)64779-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sivaramakrishnan V, Shilpa PN, Praveen Kumar VR, Niranjali Devaraj S. Attenuation of N-nitrosodiethylamine-induced hepatocellular carcinogenesis by a novel flavonol–Morin. Chem Biol Interact. 2008;171(1):79–88. doi: 10.1016/j.cbi.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 36.Yadav AS, Bhatnagar D. Chemo-preventive effect of Star anise in N-nitrosodiethylamine initiated and phenobarbital promoted hepato-carcinogenesis. Chem Biol Interact. 2007;169(3):207–214. doi: 10.1016/j.cbi.2007.06.032. [DOI] [PubMed] [Google Scholar]
- 37.Susini C, Buscail L. Rationale for the use of somatostatin analogs as antitumor agents. Ann Oncol. 2006;17(12):1733–1742. doi: 10.1093/annonc/mdl105. [DOI] [PubMed] [Google Scholar]
- 38.Kvols LK, Woltering EA. Role of somatostatin analogs in the clinical management of non-neuroendocrine solid tumors. Anticancer Drugs. 2006;17(6):601–608. doi: 10.1097/01.cad.0000210335.95828.ed. [DOI] [PubMed] [Google Scholar]
- 39.Liu HL, Huo L, Wang L. Octreotide inhibits proliferation and induces apoptosis of hepatocellular carcinoma cells. Acta Pharmacol Sin. 2004;25(10):1380–1386. [PubMed] [Google Scholar]
- 40.Xie Y, Tang CW, Wang CH. Effect of HBV X gene transfection on octreotide-inhibited growth of hepatocellular carcinoma cell line HepG2. Ai Zheng. 2005;24(8):965–969. [PubMed] [Google Scholar]
- 41.Ma Q, Meng LQ, Liu JC, Hu JP, Ge J, Wan YL, Jiang S. Octreotide induces apoptosis of human hepatoma cells by the mechanism of facilitating the Fas/FasL gene expression therein. Zhonghua Yi Xue Za Zhi. 2008;88(10):716–718. [PubMed] [Google Scholar]
- 42.Samonakis DN, Moschandreas J, Arnaoutis T, Skordilis P, Leontidis C, Vafiades I, Kouroumalis E. Treatment of hepatocellular carcinoma with long acting somatostatin analogues. Oncol Rep. 2002;9(4):903–907. [PubMed] [Google Scholar]
- 43.Yuen MF, Poon RT, Lai CL, Fan ST, Lo CM, Wong KW, Wong WM, Wong BC. A randomized placebo-controlled study of long-acting octreotide for the treatment of advanced hepatocellular carcinoma. Hepatology. 2002;36(3):687–691. doi: 10.1053/jhep.2002.35071. [DOI] [PubMed] [Google Scholar]
- 44.Kouroumalis E, Samonakis D, Skordilis P. Octreotide treatment of hepatocellular carcinoma. Hepatology. 2003;37(2):477. doi: 10.1053/jhep.2003.50026. [DOI] [PubMed] [Google Scholar]
- 45.Ballare E, Persani L, Lania AG, Filopanti M, Giammona E, Corbetta S, Mantovani S, Arosio M, Beck-Peccoz P, Faglia G, et al. Mutation of somatostatin receptor type 5 in an acromegalic patient resistant to somatostatin analog treatment. J Clin Endocrinol Metab. 2001;86(8):3809–3814. doi: 10.1210/jcem.86.8.7787. [DOI] [PubMed] [Google Scholar]
- 46.Dournaud P, Boudin H, Schonbrunn A, Tannenbaum GS, Beaudet A. Interrelationships between somatostatin sst2A receptors and somatostatin-containing axons in rat brain: evidence for regulation of cell surface receptors by endogenous somatostatin. J Neurosci. 1998;18(3):1056–1071. doi: 10.1523/JNEUROSCI.18-03-01056.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hornick CA, Anthony CT, Hughey S, Gebhardt BM, Espenan GD, Woltering EA. Progressive nuclear translocation of somatostatin analogs. J Nucl Med. 2000;41(7):1256–1263. [PubMed] [Google Scholar]
- 48.Guillermet J, Saint-Laurent N, Rochaix P, Cuvillier O, Levade T, Schally AV, Pradayrol L, Buscail L, Susini C, Bousquet C. Somatostatin receptor subtype 2 sensitizes human pancreatic cancer cells to death ligand-induced apoptosis. Proc Natl Acad Sci U S A. 2003;100(1):155–160. doi: 10.1073/pnas.0136771100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guillermet-Guibert J, Saint-Laurent N, Davenne L, Rochaix P, Cuvillier O, Culler MD, Pradayrol L, Buscail L, Susini C, Bousquet C. Novel synergistic mechanism for sst2 somatostatin and TNFalpha receptors to induce apoptosis: crosstalk between NF-kappaB and JNK pathways. Cell Death Differ. 2007;14(2):197–208. doi: 10.1038/sj.cdd.4401939. [DOI] [PubMed] [Google Scholar]
- 50.Priya R, Ilavenil S, Kaleeswaran B, Srigopalram S, Ravikumar S. Effect of Lawsonia inermis on tumor expression induced by Dalton’s lymphoma ascites in Swiss albino mice. Saudi J Biol Sci. 2011;18(4):353–359. doi: 10.1016/j.sjbs.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]