Abstract
An otherwise healthy young man was transferred to our hospital after a diving incident. He had made an uncontrolled ascent from 10 m. On arrival he appeared well. No hypotensive episodes occurred during the transfer. He denied having arthralgias, back pain, dyspnoea or neurological symptoms. Laboratory investigations revealed acutely elevated creatinine (170 µmol/L) and creatine kinase (909 U/L). Radiology was consistent with a focus of pulmonary barotrauma and intrinsic renal disease. Creatine kinase is a marker of arterial gas embolism (AGE). We determined that our patient suffered acute kidney injury as a result of gas embolisation to his renal vasculature from an area of pulmonary barotrauma. Creatinine fell the following day in response to aggressive intravenous fluids. This is the first reported case of acute kidney injury secondary to AGE. Biochemical studies should be part of the routine assessment of patients involved in diving incidents.
Background
Dive medicine is unfamiliar to most physicians. As deep-sea diving becomes increasingly popular, more doctors need to be aware of its associated maladies.1 Hyperbaric compression chambers offer an effective treatment, so knowing how to assess a diver and recognise a treatable condition is paramount.1 2
We present the case of a young man involved in a diving incident who, on initial assessment, appeared to have been unaffected. However, laboratory investigations revealed he had suffered an acute kidney injury. This is the first report of a diver with acute kidney injury secondary to arterial gas embolism (AGE).
Biochemical analysis is an important adjunct to history and physical examination when assessing patients after a diving incident.3 4
Case presentation
A 29-year-old man was air lifted to the National Hyperbaric Medicine Unit for assessment. Earlier that day he had been diving off the southern coast of Ireland with his ‘buddy’. During their ascent, our patient's air-supply became critically low at a 10 m safety stop; he panicked and shot straight to the surface. He had reached a maximum depth of 30 m, averaged 20 m and the dive had lasted 32 min using standard compressed air.
On the surface he was tachypnoeic and tachycardic, triggering an emergency call. Pneumothorax was out ruled by ultrasound before air transfer. He was conscious and maintained adequate blood pressure throughout.
On arrival the patient appeared well and denied any arthralgias, back pain, dyspnoea, chest pain, haemoptysis or neurological symptoms. A few hours later he vomited once, but denied abdominal pain. He reported having had a cough productive of green sputum over the 2 days prior to diving. Otherwise he had no significant medical or surgical history, and took no medications.
On examination, Glasgow Coma Scale (GCS) was 15/15, respiratory rate 16, oxygen saturation 97% on room air, pulse 90 bpm, blood pressure 122/77 mm Hg and temperature 36.5°C. There was no surgical emphysema. No deficit in motor, sensory, cerebellar or higher neurological function was detected. Urinalysis revealed trace protein and trace blood. Urine output was not compromised.
Investigations
Initial investigations showed raised creatinine suggestive of acute kidney injury and elevated creatine kinase (CK, table 1). On presentation, the creatinine to urea ratio was >10 (23.6 μmol/mmol). Arterial blood gas analysis was normal. Troponin T was slightly elevated (21 ng/L) but an ECG was normal. There was no eosinophilia on a differentiated blood count.
Table 1.
Trends of creatinine, urea and creatine kinase from day of admission until discharge, with follow-up creatinine
| Admission | +12 h | +16 h | +36 h | Follow-up day 21 | |
|---|---|---|---|---|---|
| Creatinine (µmol/L) | 170 | 232 | 228 | 216 | 80 |
| Urea (mmol/L) | 7.2 | 10.2 | 10.2 | 8.3 | – |
| Creatine kinase (U/L) | 909 | 1289 | – | 1050 | – |
An admission chest X-ray (figure 1) showed subtle opacification in the right upper zone and renal ultrasound (figure 2) showed increased parenchymal echogenicity bilaterally, right more than left, consistent with intrinsic renal disease.
Figure 1.
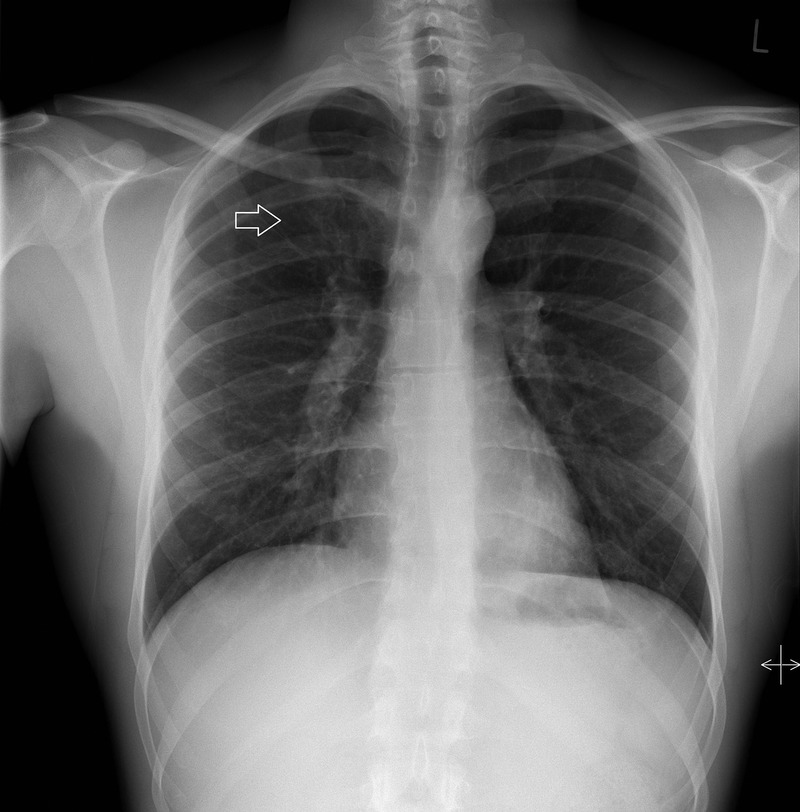
The admission chest X-ray, taken while the patient was still wearing his wet suit, demonstrates an area of increased opacity in the right upper zone (white arrow) caused by pulmonary barotrauma.
Figure 2.
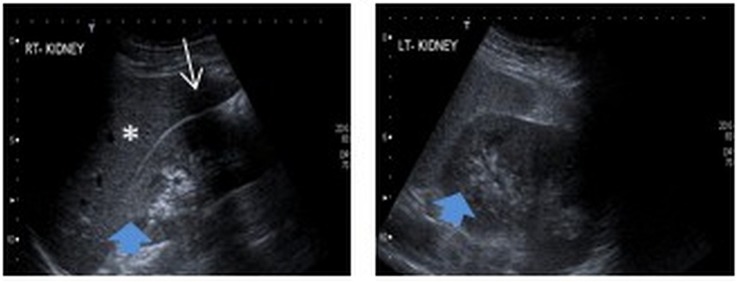
Renal ultrasonography showed hyper-echoic renal parenchyma bilaterally (blue arrows). A rib shadow (white arrow) and adjacent liver (asterisk) can be seen. Renal parenchyma should be less echoic than liver parenchyma.
By the second hospital day creatinine peaked at 232 µmol/L (estimated glomerular filtration rate not applicable in acute setting) and urea rose to 10.2 mmol/L. CK peaked at 1289 U/L. Potassium and bicarbonate remained within normal limits.
Differential diagnosis
There are two cardinal pathophysiological processes that can complicate uncontrolled ascent in divers: decompression sickness (the bends) and pulmonary barotrauma.2 Knowing that SCUBA equipment allows the diver to breathe air at a variable pressure, directly proportional to the ambient pressure at a given depth, is key to understanding the mechanism of injury in these conditions.2
Decompression sickness is caused by the dissolution of nitrogen gas during rapid ascent, as per Henry's law, forming bubbles in tissue and vasculature. Given the dive profile, and without the classic musculoskeletal symptoms (which affect 70% of cases), neurological symptoms, or other more subtle features such as cutaneous lesions or general fatigue, this diagnosis seemed unlikely.2
Pulmonary barotrauma occurs when air inhaled under pressure at depth is not exhaled during an uncontrolled ascent, and expands in the lungs, as per Boyle's law, leading to direct alveolar rupture. This can result in pneumothorax, pneumomediastinum or arterial gas embolism. In AGE, air passes from a ruptured alveolus through the pulmonary venous system to the left ventricle and then embolises systemically.2
AGE can occur after sudden ascent from shallow depths because the alveolus is more prone to rupture, as is a balloon, while it is more expanded.1 The volume of air in our patient's lungs would have doubled in volume after travelling from 10 m deep (2 ATA) to the surface (1 ATA).2 CK is a diagnostic and prognostic marker of AGE,3 and any organ can be affected by AGE.4
The peak CK level in this case fell well short of the values seen in renal failure caused by myoglobin toxicity in rhabdomyolysis.5
Given the clinical, biochemical and radiological evidence, we determined that the patient suffered acute tubular injury as a result of AGE involving his renal vasculature. The raised CK and troponin T indicate that air also embolised to his skeletal and cardiac muscles.
Treatment
High-rate (125–200 mL/h) intravenous 0.9% sodium chloride was administered for 24 h. Hyperbaric oxygen therapy was considered, however, due to the atypical presentation, minor degree of injury and rapid clinical improvement, it was not initiated.
Outcome and follow-up
The patient's renal function improved the day after admission, and he was discharged home. His creatinine had returned to baseline (80 µmol/L) at follow-up 3 weeks later.
Discussion
Acute kidney injury associated with SCUBA diving is extremely rare. One case reported from New Zealand involved a diver who had a near-drowning experience; findings on urinalysis and renal ultrasound were different to the present case, and the authors attributed the insult to hypoxia and hypotension.6 Another diver was reported to have developed minimal change disease after exposure to fire coral in the Caribbean Sea, which was felt to represent an atopic reaction.7
The effect of intra-arterial bubbles on end organs in AGE is more complicated than distal ischaemia. Disruption of endothelial function and an inflammatory response against the air-bubbles themselves could also have contributed to the disturbance of renal function seen in our patient.2 8 Bubble contact with endothelial cells results in calcium influx, mitochondrial dysfunction and cell death.9
The usefulness of CK as a marker of embolism burden in AGE is well documented. The peak level of CK has even been shown to correlate with the severity of residual neurological deficit.3 Our patient's peak CK level corresponded with ‘no deficit’, in keeping with his clinical course.
Recompression with hyperbaric oxygen therapy should always be considered as first-line treatment when AGE is suspected. Intravenous fluids to improve perfusion are also advocated.1 2 8
Learning points.
Arterial gas embolism (AGE) affects divers who ascend quicker than gas can escape their lungs (even from shallow depths), as a result of either rapid ascent or compromised air flow, and any organ can be affected.1 2 4
Creatine kinase is a particularly useful marker in the diagnosis and prognosis of AGE.3
Recompression hyperbaric oxygen therapy is first-line treatment for divers with AGE.1 2 8
Footnotes
Contributors: PJG, YK, ENS and DL took part in the management of the patient’s care. PJG and YK wrote the first draught of the manuscript. ENS and DL contributed to the finalisation of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lynch JH, Bove AA. Diving medicine: a review of current evidence. J Am Board Fam Med 2009;22:399–407. 10.3122/jabfm.2009.04.080099 [DOI] [PubMed] [Google Scholar]
- 2.Auerbach P. Wilderness medicine. 5th edn Mosby, 2007. [Google Scholar]
- 3.Smith RM, Neuman TS. Elevation of serum creatine kinase in divers with arterial gas embolization. N Engl J Med 1994;330:19–24. 10.1056/NEJM199401063300104 [DOI] [PubMed] [Google Scholar]
- 4.Smith RM, Neuman TS. Abnormal serum biochemistries in association with arterial gas embolism. J Emerg Med 1997;15:285–9. 10.1016/S0736-4679(97)00007-3 [DOI] [PubMed] [Google Scholar]
- 5.Clarkson PM, Kearns AK, Rouzier P et al. Serum creatine kinase levels and renal function measures in exertional muscle damage. Med Sci Sports Exerc 2006;38:623–7. 10.1249/01.mss.0000210192.49210.fc [DOI] [PubMed] [Google Scholar]
- 6.Neale TJ, Dewar JM, Parr R et al. Acute renal failure following near drowning in salt water. N Z Med J 1984;97:319–22. [PubMed] [Google Scholar]
- 7.Prasad GV, Vincent L, Hamilton R et al. Minimal change disease in association with fire coral (Millepora species) exposure. Am J Kidney Dis 2006;47:e15–6. 10.1053/j.ajkd.2005.09.025 [DOI] [PubMed] [Google Scholar]
- 8.Muth CM, Shank ES. Gas embolism. N Engl J Med 2000;342:476–82. 10.1056/NEJM200002173420706 [DOI] [PubMed] [Google Scholar]
- 9.Sobolewski P, Kandel J, Eckmann DM. Air bubble contact with endothelial cells causes a calcium-independent loss in mitochondrial membrane potential. PLoS ONE 2012;7:e47254 10.1371/journal.pone.0047254 [DOI] [PMC free article] [PubMed] [Google Scholar]


