Abstract
A 56-year-old woman visited her general practitioner 12 months prior with eczema. Blood samples showed anaemia, a haemoglobin level of 105 g/L and a high erythrocyte sedimentation rate (ESR) of 80 mm. Her eczema was diagnosed as discoid lupus erythaematosus but there were no signs of systemic lupus erythaematosus. Extensive investigations were made including testing of serial blood samples, repeated examinations by specialists in dermatology, rheumatology and gynaecology, and several X-rays including CT of the chest and the abdomen, all without finding a reasonable underlying diagnosis. One year later, the patient presented with dyspnoea associated with effort and body position; she was sent for echocardiography, which showed an atrial myxoma filling almost the whole left atrium and affecting the mitral valve. She was treated with urgent surgical removal and now, 6 weeks postsurgery, has fully recovered. She no longer has dyspnoea, her haemoglobin level and ESR have normalised, and the eczema has almost disappeared.
Background
Clinical signs and symptoms such as fatigue, dyspnoea, anaemia and increased erythrocyte sedimentation rate (ESR) are common in the middle-aged patient population. These signs, all part of a paraneoplastic syndrome, are often a reason for further investigation at a general practitioner’s (GP) office. In this case, the GP made a thorough investigation including serial physical examinations, blood samples, several X-rays such as pulmonary X-ray, and CT of the chest and abdomen, and asked for expert opinions from specialists in dermatology, rheumatology and gynaecology—all without finding a reasonable underlying cause of anaemia and chronic inflammation. Subsequently, the patient presented with dyspnoea during effort; she was sent for an echocardiography examination, which led to the correct diagnosis. After surgical treatment, the patient recovered very well, and 6 weeks postsurgery her haemoglobin level has normalised from 105 to 127 g/L and her ESR has decreased from 80 to 24 mm. She no longer has dyspnoea on effort and even her dermatological symptoms, for which she had visited her GP in the first place, have improved.
Case presentation
A 56-year-old woman, a former smoker, without any known medical history or medication, visited her GP 12 months prior for eczema on her face and forehead. Physical examination showed dermatitis and blood samples showed anaemia with a haemoglobin level of 105 g/L and increased ESR of 80 mm. The anaemia was characterised as hypochromic with small erythrocytes together with iron deficiency, but there were no signs of gastrointestinal bleeding. An examination by a specialist in gynaecology did not show any signs of bleeding either. Repeated plasma protein fraction samples only showed signs of inflammation, with no M-component. The patient was put on oral iron substitution and sent to a specialist in dermatology, due to the dermatitis. The examination showed signs of cutaneous lupus erythaematosus and a biopsy verified discoid lupus erythaematosus (DLE), which was treated with local corticosteroids with modest effect. However, a visit to a specialist in rheumatology showed no signs of systemic lupus erythaematosus or other systemic disease. Furthermore, a thorough X-ray examination including pulmonary X-ray, and CT of the chest and abdomen, did not show anything that could explain the anaemia or the high ESR. The GP wanted to try an ex juvantibus treatment with a high dose of oral corticosteroids, but the patient refused treatment. One year later, she again visited her GP because of dyspnoea on effort for the past couple of weeks. Her symptoms worsened while she waited for an echocardiography examination. Moreover, the last couple of months she had also presented with dyspnoea associated to body position. She could not lie face up without several pillows. An echocardiography examination showed a large 7.4×4.6 cm cardiac tumour in the left atrium, affecting the mitral valve and the blood flow to the left chamber. She was sent directly to the department of cardiology at the University hospital, which confirmed the finding.
Investigations
Transthoracic echocardiography showed a large 7.4×4.6 cm cardiac tumour in the left atrium, affecting the mitral valve and the blood flow to the left chamber. The left and right chambers had normal systolic function. There was significant 80 mL/m2 dilation of the left atrium, but the right atrium and both chambers were of normal size. There was significant 75 mm Hg systolic pulmonary hypertension (figure 1A, B).
Figure 1.
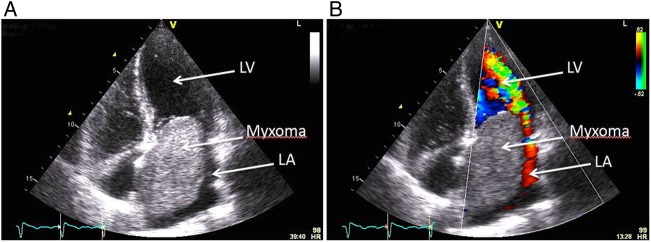
Transthoracic echocardiography showing an apical four-chamber view. (A) A large LA myxoma filling almost the whole LA and affecting the mitral valve. (B) A colour Doppler is added. The big atrial myxoma is affecting the blood flow from the LA to the chamber. The myxoma allows only limited blood flow through the mitral valve. LA, left atrium; LV, left ventricle.
Differential diagnosis
Connective tissue disease, vasculitis, myeloma or other form of cancer, and chronic infection or polymyalgia rheumatica.
Treatment
Urgent thoracic surgery for removal of the tumour was performed due to the risk of embolisation and intracardiac obstruction.
Pathological examination of the tumour verified the diagnosis of an atrial myxoma (figure 2).
Figure 2.

A left atrial myxoma with a smooth, glistening surface and a size of 7.5×5×4.5 cm.
Outcome and follow-up
Six weeks postsurgery, the patient's haemoglobin level normalised from 105 to 128 g/L and her ESR decreased from 80 to 24 mm. The patient no longer has symptoms of dyspnoea on effort or associated with body position. She has recovered very well after surgery and even her eczema, for which she had visited her GP in the first place, has improved and almost disappeared.
Discussion
Primary cardiac tumours are very rare, with an incidence of less than 0.03%. Most are benign tumours, mainly myxomas, and more than 75% of myxomas are located in the left atrium.1 The mean age at diagnosis is 56 years and the majority of patients are women.2 Half of the patients present with symptoms due to intracardiac obstruction or central or peripheral embolism, but constitutional signs such as fatigue, weight loss, muscle weakness and fever, are common as well. A wide range of non-specific cutaneous manifestations has also been reported.3 4 Echocardiography is the diagnostic method of choice. Transthoracic echocardiography has a very good sensitivity, up to 95%, but transoesophageal echocardiography is even better, reaching a sensitivity of 100%.5 Once a cardiac myxoma has been diagnosed, urgent surgical excision is required due to the risk of embolisation.4 The long-term prognosis is very good; cardiac myxomas most often occur only sporadically and surgery is usually curative with a low recurrence rate of 0–3%.2 6
Despite the fact that the present clinical case, a middle-aged woman, represents a typical patient with myxoma, we still have to remember that cardiac myxoma is a very rare diagnosis. Therefore, we have to investigate for more common causes of high ESR and anaemia. Her first symptom was eczema, which was diagnosed as dermal lupus erythaematosus (DLE) but without any signs of systemic disease. A wide range of cutaneous manifestations have been found associated with cardiac myxoma and most likely related to abnormal cytokine production from the tumour itself.4 This may also be the cause of the clinical picture with chronic inflammation and anaemia. The classic triad of a cardiac myxoma consists of (1) symptoms due to cardiac obstruction, (2) symptoms due to cerebral or peripheral embolism and (3) constitutional symptoms such as fever, weight loss or symptoms resembling inflammatory connective tissue disease. The present patient did follow the classic triad but started with the last arm and presented with a clinical picture of chronic inflammation and DLE. It was not until she started suffering from dyspnoea associated with effort and later also body position, the first arm of the classic triad, that she was sent for an echocardiography, which ultimately gave the correct diagnosis.
Fortunately, the present clinical case had no history of cerebral or peripheral embolism, which is one of the further clinical presentations to be expected of myxoma. Furthermore, when the myxoma grows and fills the atrium, it may impair the mitral valve function and obstruct the blood flow from the left atrium to the chamber. Therefore, another typical clinical presentation to be expected in myxoma could be breathlessness, or even presyncope or syncope attacks associated to body position, for example, when the patient bends forward to tie his or her shoelaces.
The patient in the present case was accepted for and went through surgical removal of the atrial myxoma the same day the echocardiography was made. At the follow-up visit, 6 weeks postsurgery, she has fully recovered and no longer has dyspnoea. Her haemoglobin level and ESR have normalised and the eczema has almost disappeared.
Patient's perspective.
I want to describe myself as an average physical active person, participating in work out classes twice a week and walking with walking sticks. The last year before I got my diagnosis I felt that my physical condition decreased and slowly worsened. I was no longer able to bicycle to work. Instead, I had to go by car and it was impossible to join a work out class. I tried to continue walking but had to stop to rest in uphill slopes. Furthermore, I easily contracted upper airway infections and had more or less a chronic cough, which I thought was the main reason for my decreased physical condition.
Because of the gradual worsening of my physical condition, I adapted my lifestyle. Maybe that's also why I didn't react as strongly as I would have if the change had been faster or more acute. During this period, about 12 months, I visited my general practitioner (GP) several times. First because of an irritating eczema and then we also tried to find out the cause of my shortness of breath, the anaemia and the increased ESR. I was treated with local corticosteroids for my eczema but we couldn’t find any explaining background or a cause of my other symptoms, which was really frustrating. Treatment with high-dose corticosteroids was discussed but I wasn't motivated enough for that.
Meantime, I worked full time and had, as far as I can remember, no days of sick leave. I managed to complete my duties at work, but nonetheless I was always tired after work and spent most of my spare time resting on the sofa.
Approximately 3 months before my surgical treatment, I went for a shorter hiking among the Swedish mountains and it was now that I really felt that something was wrong. I've made the same hiking tour several times earlier but this time it took twice as long. Uphill, I wasn't able to go more than 10 m before I had to stop to catch my breath and my legs felt like they were made of lead. Of course, my family was worried because of my worsening physical condition. At this time, even a few steps walking up the stairs at home made me breathless and it was impossible to lay down, face up during the nights without a couple of pillows under my head. Now, my GP sent me for an ultrasound examination of my heart and it was now that they discovered the myxoma in my heart.
I went through the examination early in the morning and got the surgical treatment later in the afternoon the same day. I felt relieved when I got the diagnosis that explained my symptoms but also a bit shocked when I heard that I had a tumor inside my heart. That day, everything went so fast that I had no time to get worried before the operation; but post surgery I had a couple of weeks of anxiety and discomfort when I realized what I had gone through. I felt depressed in some way but all these problems disappeared after a further week.
Now, only 8 weeks post surgery I find myself surprisingly well recovered. I've started regular walking tours and participate in work out classes and it's a huge difference compared to before surgery. Once again, I am able to go for jogging tours, walking uphill and in stairs without losing my breath and I really feel that my physical condition is improving every day. Additionally, my eczema is much better and has almost disappeared. Within a week, I'm planning to go back to work again, starting half time but hopefully full time soon.
I feel a great relief and gratitude for everything that has gone in the right direction so far, and I'm looking forward to go back to a normal life again.
Learning points.
Atrial myxoma is a rare disease but still a known cause of several paraneoplastic symptoms and clinical signs such as anaemia, fatigue, elevated erythrocyte sedimentation rate and dyspnoea.
In the present clinical case, the general practitioner made a thorough investigation, maybe even more extensive than many other colleagues would have done. But at last the correct diagnosis was made, which, in this particular case, was treatable with thoracic surgery and removal of the atrial myxoma, after which the patient was completely recovered.
Always listen to the patient, rely on your findings, and try to find a reasonable explanation for the symptoms and clinical signs.
Footnotes
Contributors: ME, the cardiologist in charge for the patient, initiated and drafted the manuscript. PS was responsible for the surgical treatment and follow-up of the patient, and revised the manuscript critically for important intellectual content and approved the final version of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ventura F, Landolfa MC, Leoncini A et al. . Sudden death due to primary atrial neoplasms: report of two cases and review of literature. Forensic Sci Int 2012;214:e30–3. 10.1016/j.forsciint.2011.07.042 [DOI] [PubMed] [Google Scholar]
- 2.Lee Percell RL Jr, Henning RJ, Siddique Patel M. Atrial myxoma: case report and a review of the literature. Heart Dis 2003;5:224–30. 10.1097/01.hdx.0000074515.95567.92 [DOI] [PubMed] [Google Scholar]
- 3.Pinede L, Duhaut P, Loire R. Clinical presentation of left atrial cardiac myxoma. A series of 112 consecutive cases. Medicine 2001;80:159–72. 10.1097/00005792-200105000-00002 [DOI] [PubMed] [Google Scholar]
- 4.Smith M, Chaudhry MA, Lozano P et al. . Cardiac myxoma induced paraneoplastic syndromes: a review of the literature. Eur J Int Med 2012;23:669–73. 10.1016/j.ejim.2012.05.015 [DOI] [PubMed] [Google Scholar]
- 5.Engberding R, Daniel WG, Erbel R et al. . Diagnosis of heart tumours by transoesophageal echocardiography: a multicentre study in 154 patients. European Cooperative Study Group. Eur Heart J 1993;14:1223–8. 10.1093/eurheartj/14.9.1223 [DOI] [PubMed] [Google Scholar]
- 6.Bjessmo S, Ivert T. Cardiac myxoma: 40 years’ experience in 63 patients. Ann Thorac Surg 1997;63:697–700. 10.1016/S0003-4975(96)01368-9 [DOI] [PubMed] [Google Scholar]


