Abstract
We discuss a rare presentation of malignant teratoma in a 63-year-old woman who was admitted to accident and emergency with abdominal distension, bloody diarrhoea and peritonitis. CT of the abdomen and pelvis showed free air in the abdomen and a gas-fluid filled cavity measuring 12×6 cm in the mid-pelvis with possible fistulation that was suspicious for malignancy. A 10×12 cm ruptured dermoid cyst was found intraoperatively, which was adherent to the bowel wall. Bulky lymph nodes were also appreciated. The surgeon suspected a metastatic malignant teratoma, and a Hartmann's procedure, total abdominal hysterectomy and bilateral salpingoopherectomy were performed with clearance of the para-aortic lymph nodes. Subsequent histological analysis revealed a squamous cell carcinoma arising from an ovarian malignant teratoma. The patient went on to have carboplatin and paclitaxel chemotherapy and is alive at 6 months follow-up.
Background
Mature cystic teratoma is a common, benign germ cell tumour of the ovary and comprises 20% of all ovarian tumours.1 Malignant transformation of such tumours is rare and occurs in only 1–2% of all cases. The most common of these is squamous cell carcinoma (SCC), which represents 80–90% of all malignant transformations.2 Frequent presenting symptoms include an increase in abdominal size, presence of a mass and abdominal or pelvic pain.3 4 Invasion of a malignant teratoma into the sigmoid colon is rarely reported in the literature. In this case report, we describe a patient who presented unusually with peritonitis, diarrhoea with rectal bleeding secondary to ovarian cyst perforation and invasion of SCC into the sigmoid colon.
Case presentation
A 63-year-old woman presented with acute abdominal pain and distention. She described three episodes of vomiting and explosive bloody diarrhoea. On examination, there was clinical evidence of peritonitis, and the patient was particularly tender in the left iliac fossa.
A working diagnosis of bowel perforation was made, and CT of the abdomen and pelvis was requested. This revealed free gas in the abdomen and under the right hemidiaphragm. Free fluid in the abdomen and pelvis and a gas-fluid filled cavity measuring 12×6 cm in the mid-pelvis was also appreciated. The radiologist raised the possibility of a malignant dermoid cyst within this cavity with possible fistulisation to the sigmoid colon (figure 1).
Figure 1.
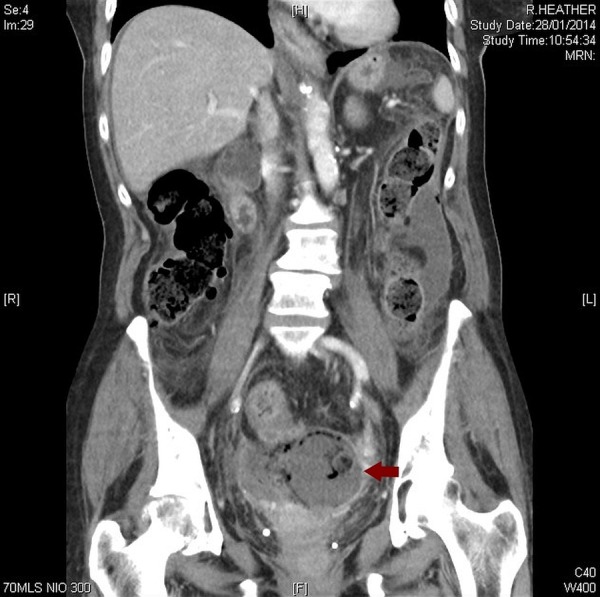
Dermoid cyst present within the mid-pelvis.
A ruptured left ovarian cyst measuring 10×12 cm was found intraoperatively. The cyst contained hair, and part of the wall was thickened to form a 40×20×20 mm mass that was adherent to the rectosigmoid junction. Multiple enlarged lymph nodes were identified along the left internal iliac artery and inferior mesenteric artery. A Hartmann's procedure, total abdominal hysterectomy and bilateral salpingoopherectomy were performed. Radical pelvic lymphadenectomy was accomplished with clearance of the para-aortic lymph nodes up to the origin of the inferior mesenteric artery.
Analysis of the resected material identified a 40 mm circumferential tumour within the sigmoid colon, which invaded through the muscularis propria. The ovarian capsule was ruptured, and the ovarian cyst measured 80×50×40 mm (figure 2). The histology showed a poorly differentiated SCC arising from an ovarian malignant teratoma (figure 3) that had invaded into the colon. The colon was found to be extensively infiltrated with SCC (figures 4 and 5), which undermined the colonic mucosa and caused mucosal ulceration in areas. Lymphovascular infiltration was also identified in 14 of the 22 resected lymph nodes. The cancer was staged at a minimum of International Federation of Gynecology and Obstetrics (FIGO) stage 2B.
Figure 2.
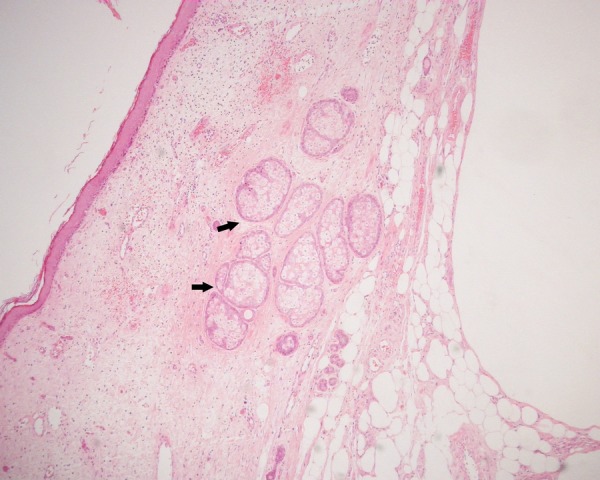
Ovary with area of mature cystic teratoma (×4).
Figure 3.
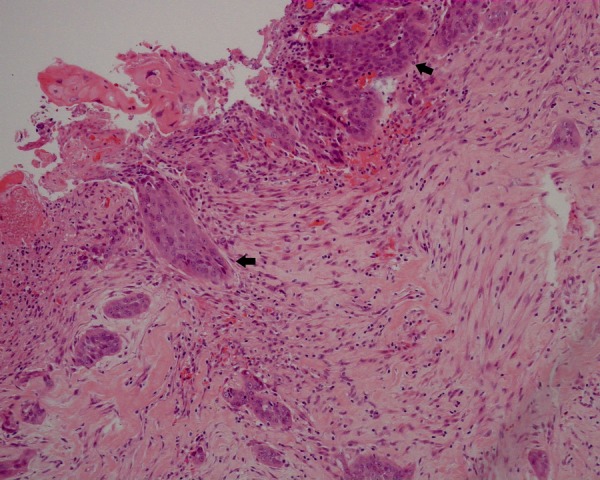
Ovary with squamous cell carcinoma arising from squamous dysplasia.
Figure 4.
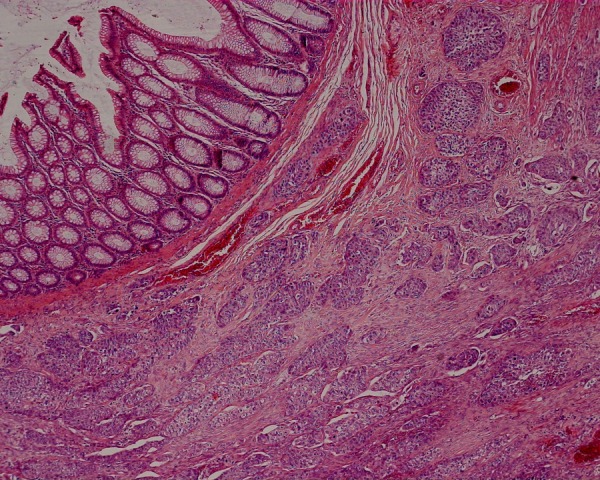
Colon with underlying squamous cell carcinoma (×4).
Figure 5.
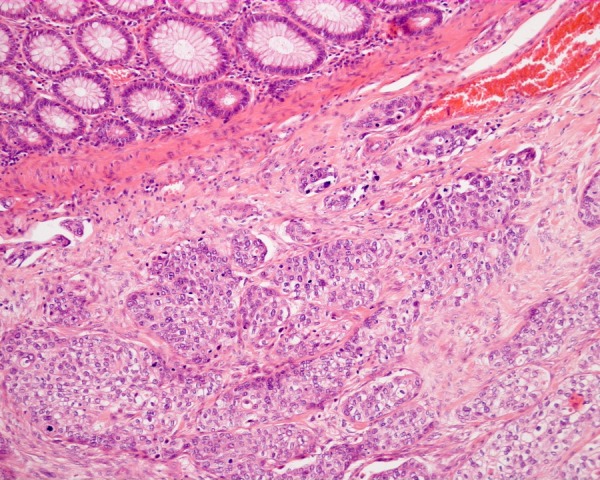
Colon with underlying squamous cell carcinoma (×10).
Our patient returned to theatre 4 weeks postoperatively with features of bowel obstruction. The gynaecological team recommended omentectomy. This was not possible as dense adhesions precluded satisfactory progress and the risk of bowel perforation outweighed any benefit derived from adhesiolysis and omentectomy. The patient started adjuvant chemotherapy with carboplatin and paclitaxel 2 months following her index operation. She tolerated chemotherapy very well. The only significant side effect was thrombocytopaenia, which required reducing the carboplatin dose on her third cycle. She is alive 6 months postoperatively.
Discussion
Malignant transformation is a rare complication of benign cystic teratoma of the ovary, representing 1–2% of cases.5 As was the case in our patient, it typically presents in postmenopausal women (mean age 55).3 It is posited that this may relate to long-term presence of benign disease.6
While benign disease is readily identified radiologically with pathognomonic signs such as hair and teeth, preoperative diagnosis of malignancy is challenging. Distinguishing benign from malignant disease on CT images is often impossible, and clinical presentation varies widely and is often indistinguishable from benign disease.5 7 In addition, the literature suggests that tumour markers in preoperative diagnosis have limitations and their role in diagnosis is controversial.3 8
A systematic review of 277 patients described the most common symptoms of pain (54%), mass and constipation (31%).3 This case is unusual in its presentation of rectal bleeding, diarrhoea and peritonitis. Sigmoid infiltration is also rare and was the most likely cause for rectal bleeding in this patient. This case, therefore, illustrates the need for clinical suspicion of invasive ovarian malignancy when rectal bleeding in association with an ovarian mass is identified.
The current literature indicates that malignant teratoma is larger than benign disease, with a mean malignant diameter of 148 mm.3 Kikkawa et al4 report that cyst dimension >99 mm is 86% sensitive for malignancy. Our pathological measurements are not in accordance with this observation. This may indicate that cyst size in the case of ovarian cyst rupture may not be reliable as a diagnostic tool.
Tumour markers such as CA125, CA19-9, CEA and SCC, are often elevated in malignant teratoma.3 However, a high concentration of CA125 and CA19-9 can also be seen in benign disease, and, equally, studies have seen patients with normal serum CA125 in malignancy.7 9 CA125 and CA19-9, therefore, offer little diagnostic benefit. However, raised CA125 has been associated with poor prognosis in malignant transformation.3 There is evidence to suggest raised serum CEA and SCC are associated with malignant transformation and it is recommended that patients are tested for these markers where there is suspicion of malignant transformation of a benign cystic teratoma.4 Our patient had a marginally raised CEA (5 µg/L) and an elevated CA-125 of 355 U/mL. Serum SCC was not tested.
Preoperative CT imaging in our patient indicated presence of a dermoid cyst, but was unable to diagnose malignancy. This is consistent with the literature, which illustrates the difficulties in diagnosing malignancy of a dermoid cyst on ultrasound and CT.7 10 It has been suggested that MRI has a greater diagnostic value in differentiating between benign and malignant disease.7 This is because features of malignancy (such as necrosis and direct invasion) are better appreciated in MRI.7 11 Further radiological assessment through MRI may have assisted diagnosis and surgical planning in this patient.
Few case reports draw an association between adherence observed intraoperatively and malignancy. A malignant cystic teratoma that was found to be adherent to the bladder wall was not recognised and treated appropriately as malignancy in a case report by Badmos et al.6 Surgeons should be alerted to the possibility of malignancy in patients with malignant teratoma, under which circumstances radical resection is recommended.3 7
Learning points.
Malignant transformation of teratoma is an important differential in women presenting with abdominal pain and a palpable mass.
The patient group affected by malignant teratoma is predominantly postmenopausal and radiological evidence of an ovarian cyst >99 mm should prompt further investigation to exclude malignancy.
CEA and squamous cell carcinoma biochemical markers have been shown to assist preoperative diagnosis of malignant teratoma.
It is difficult to diagnose malignant teratoma from CT imaging, and clinicians may find MRI useful in reaching a diagnosis and for the purposes of surgical planning.
Adherence noted intraoperatively should alert clinicians to the possibility of malignant teratoma. Under these circumstances, radical resection is advocated to optimise long-term outcome.
Acknowledgments
The authors acknowledge the contribution of Mr M Willcox for performing the gynaecological surgery.
Footnotes
Contributors: ATG, AOJ, JG and YA all contributed to conception and design, acquisition of data and drafting the manuscript or critically evaluating the intellectual content.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Tseng C, Chou H, Huang K et al. Squamous cell carcinoma arising in mature cystic teratoma of the ovary. Gynecol Oncol 1996;63:364–70. 10.1006/gyno.1996.0337 [DOI] [PubMed] [Google Scholar]
- 2.Powell J, Stonson J, Connor G et al. Squamous cell carcinoma arising in a dermoid cyst of the ovary. Gynecol Oncol 2003;89:526–8. 10.1016/S0090-8258(03)00135-5 [DOI] [PubMed] [Google Scholar]
- 3.Hackethal A, Brueggmann D, Bohlmann M et al. Squamous-cell carcinoma in mature cystic teratoma of the ovary: systematic review and analysis of published data. Lancet Oncol 2008;9:1173–80. 10.1016/S1470-2045(08)70306-1 [DOI] [PubMed] [Google Scholar]
- 4.Kikkawa F, Nawa A, Tanakishi K et al. Diagnosis of squamous cell carcinoma arising from mature cystic teratoma of the ovary. Cancer 1998;82:2249–55. [DOI] [PubMed] [Google Scholar]
- 5.Chaudry S, Hussain R. Squamous cell carcinoma arising in mature cystic teratoma (dermoid cyst)–a rare presentation. J Pak Med Assoc 2013;63:521–3. [PubMed] [Google Scholar]
- 6.Badmos K, Ibrahim O, Aboyeji A et al. Squamous cell carcinoma arising in a mature cystic ovarian teratoma with bladder invasion: a case report. Afr Health Sci 2011;11:285–7. [PMC free article] [PubMed] [Google Scholar]
- 7.Hurwitz J, Fenton A, McCluggage W et al. Squamous cell carcinoma arising in a dermoid cyst of the ovary: a case series. BJOG 2007;114:1283–7. 10.1111/j.1471-0528.2007.01478.x [DOI] [PubMed] [Google Scholar]
- 8.Tangjitgamol S, Manusirivithaya S, Sheanakul C et al. Squamous cell carcinoma arising from dermoid cyst: case reports and review of literature. Int J Gynaecol Cancer 2003;13:558–63. 10.1046/j.1525-1438.2003.13312.x [DOI] [PubMed] [Google Scholar]
- 9.Nagata H, Takahashi K, Yamane Y et al. Abnormally high values of CA 125 and CA 19-9 in women with benign tumors. Gynecol Obstet Invest 1989;28:165–8. 10.1159/000293559 [DOI] [PubMed] [Google Scholar]
- 10.Lee Y, Abulafia O, Montalto N et al. Malignant transformation of an ovarian mature cystic teratoma presenting as a rectal mass. Gynecol Oncol 1999;75:499–503. 10.1006/gyno.1999.5602 [DOI] [PubMed] [Google Scholar]
- 11.Hosokawa T, Sato Y, Seki T et al. Malignant transformation of mature cystic teratoma of the ovary with rupture. Jpn J Radiol 2010;28:372–5. 10.1007/s11604-010-0434-0 [DOI] [PubMed] [Google Scholar]


