Abstract
Lung involvement in primary Sjögren syndrome occurs in approximately 10–20% of patients. Tocilizumab, an anti-interleukin-6 receptor antibody, has demonstrated efficacy and safety in small series of systemic sclerosis, and systemic lupus erythematosus, but its effect on interstitial lung manifestations of connective tissue diseases is not well known. We report the use of tocilizumab in a refractory organising pneumonia associated with Sjögren's disease. Our observation suggests that tocilizumab could be an alternative therapeutic in refractory organising pneumonia.
Background
Lung involvement in primary Sjögren's syndrome (pSS), as defined by symptoms and either pulmonary function testing or radiographic abnormalities, is seen in between 0% and 20% of patients.1 Among the histopathological patterns described in pSS, organising pneumonia (OP) is infrequently observed.2 The optimal treatment for patients with pSS-associated interstitial lung disease (ILD) is not known but likely depends on the specific underlying pathology. Prednisone therapy in the range of 0.5–1 mg/kg/day is favoured as the initial treatment for OP. Although OP is considered to have a good prognosis and to be corticosteroid responsive, some patients with OP treated with corticosteroids relapse, especially those patients with connective tissue disease (CTD).3 Tocilizumab, an anti-interleukin 6 (IL-6) receptor antibody, has demonstrated efficacy and safety in a small series of rheumatoid arthritis, systemic sclerosis and systemic lupus erythematosus,4 but its effect on interstitial lung manifestations of these CTDs is not well known. We report the first case of steroid refractory pSS-associated OP successfully treated by tocilizumab.
Case presentation
A 55-year-old Caucasian non-smoking man was referred for an acute bilateral pneumonia (figure 1A). He also had associated diffuse bilateral arthritis of the hands and knees for 1 month and fever persisting after several antibiotic treatments. His medical history was unremarkable. He denied recent travel or relevant exposures. He never had any gastroesophageal reflux disease symptoms or a proton pump inhibitor. The patient described Raynaud phenomenon: persistent troublesome dry eyes and feeling of dry mouth. Schirmer's test was positive. Labial salivary gland biopsy showed a focal sialadenitis with a focus score of 3/4 mm2. Laboratory evaluations showed elevated C reactive protein levels (296 mg/L) and positive antinuclear antibodies (1:320). No Sjögren's syndrome type A antigen (SSA)/Ro or SSB/La antibodies were detected. Serum protein electrophoresis revealed a polyclonal hypergammaglobulinemia with a γ-globulin level of 33 g/dL. X-rays and CT scans showed diffuse, migrating, bilateral subpleural alveolar consolidations (figure 2). Bronchoalveolar lavage analysis revealed a mildly elevated lymphocyte count (20%, CD4/CD8 0.25). Microbial cultures for bacteria, fungus and mycobacteria were all negative. [18F]-Fluorodeoxyglucose positron emission tomography revealed a mild uptake in the area of consolidation. According to the consensus of classification criteria,5 pSS-associated OP was diagnosed.
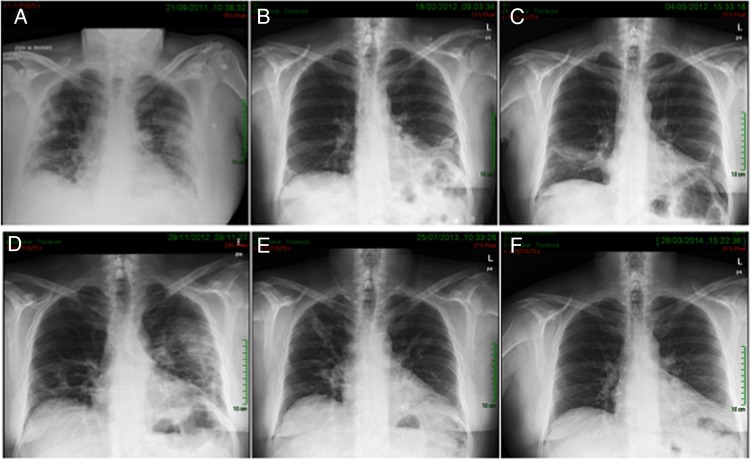
Figure 1.
Evolution of chest X-rays: (A) at diagnosis, (B) improvement after receiving prednisone 30 mg/day, (C) first relapse, with a daily dose of 12.5 mg/day of prednisone, (D) after 6 months of treatment with methotrexate (25 mg/week) and prednisone 25 mg/day, (E) after two rituximab infusions, methotrexate and prednisone 25 mg/day and (F) after two infusions of tocilizumab plus methotrexate, prednisone can be tapered to 5 mg/day without any relapse of organising pneumonia or arthritis.
Figure 2.

Chest CT scan at admission: diffuse bilateral migrating subpleural consolidations are observed.
Treatment
Oral prednisone (1 mg/kg/day) was started. Respiratory symptoms and arthritis rapidly improved, and the alveolar infiltrates diminished on the CT scan (figure 1B). Steroids were tapered, however, 8 months after treatment initiation, the first relapse of OP and arthritis was observed at a dose of 12.5 mg/day (figure 1C). Methotrexate was added (25 mg/week), but was ineffective in controlling the arthritic and pulmonary symptoms after 6 months of treatment (figure 1D). The patient received two injections of rituximab (1000 mg each). The prednisone dose was kept above 25 mg/day after treatment initiation, because of persistent arthritic and OP activity (figure 1E). Nearly 2 years after the diagnosis was made, we decided to give tocilizumab (8 mg/kg, ie, 785 mg/month), in combination with prednisone and methotrexate (25 mg/week).
Outcome and follow-up
After two infusions, the patient significantly improved (figure 1F). Prednisone was progressively tapered to 5 mg/day. Eight months after initiating tocilizumab, the EULAR Sjögrens Syndrome Disease Activity Index was stable at 4. CT scan and pulmonary function tests were normalised (figure 3). To this point, the treatment was well tolerated.
Figure 3.

CT scan after two perfusion of tocilizumab: dramatic improvement is observed. No relapse was observed when prednisone was tapered to 5 mg/day.
Discussion
The pathophysiology of OP is unclear and the role of IL-6 in the disease has never been investigated. However, in a murine model of virus-induced OP, high IL-6 messenger RNA levels in the lungs have been observed.6 Lymphocytes and neutrophils, regulated by IL-6, are increased in alveolar spaces and bronchiolar lumens, especially during early stages of the process.7 These data could be the beginning of an explanation for the effect of IL-6 blockade observed in our case.
Oral prednisone is the recommended treatment regardless of the aetiology. However, responsiveness seems to be poorer in OP in patients with CTD.2 5 In a small series of 18 pSS-associated ILD, OP was observed in 4 of 18 patients, and all improved after steroid therapy.8 One case of steroid refractory fatal OP has been reported.9 For refractory cases, immunosuppressive agents such as cyclophosphamide, azathioprine, cyclosporine10 and recently, infliximab and rituximab, have been used.10
The effect of tocilizumab on pSS has not been investigated except in one short report.11 The treatment effect on CTD ILD has not been well established; concerning systemic sclerosis, no effect has been observed on lung fibrosis,12 but some cases of ILD improved after tocilizumab in rheumatoid arthritis (RA),13 and no effects on undifferentiated autoinflammatory disorder have been reported.14 However, concerns have been raised about pulmonary toxicity of tocilizumab in RA, since there have been several cases of exacerbation of ILD,15 16 and the appearance of ILD,17 including a case of OP,18 after this treatment. Further investigations are required to assess the role of tocilizumab as an alternative therapeutic in refractory OP.
Learning points.
Lung involvement in primary Sjögren's syndrome (pSS), as defined by symptoms and either pulmonary function testing or radiographic abnormalities, is seen in between 0% and 20% of patients.1
To the best of our knowledge, this is the first reported case of successful use of tocilizumab in refractory organising pneumonia (OP) associated with pSS.
Further investigations are required to assess the role of tocilizumab as an alternative therapeutic in refractory OP.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Nannini C, Jebakumar AJ, Crowson CS et al. Primary Sjogren's syndrome 1976–2005 and associated interstitial lung disease: a population-based study of incidence and mortality. BMJ Open 2013;3:e003569 10.1136/bmjopen-2013-003569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henriet AC, Diot E, Marchand-Adam S et al. Organising pneumonia can be the inaugural manifestation in connective tissue diseases, including Sjogren's syndrome. Eur Respir Rev Off J Eur Respir Soc 2010;19:161–3. 10.1183/09059180.00002410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yoo JW, Song JW, Jang SJ et al. Comparison between cryptogenic organizing pneumonia and connective tissue disease-related organizing pneumonia. Rheumatol Oxf Engl 2011;50:932–8. 10.1093/rheumatology/keq410 [DOI] [PubMed] [Google Scholar]
- 4.Murakami M, Nishimoto N. The value of blocking IL-6 outside of rheumatoid arthritis: current perspective. Curr Opin Rheumatol 2011;23:273–7. 10.1097/BOR.0b013e3283456797 [DOI] [PubMed] [Google Scholar]
- 5.Shiboski SC, Shiboski CH, Criswell LA et al. Sjögren's International Collaborative Clinical Alliance (SICCA) Research Groups. American College of Rheumatology classification criteria for Sjögren's syndrome: a data-driven, expert consensus approach in the Sjögren's International Collaborative Clinical Alliance cohort. Arthritis Care Res 2012;64:475–87. 10.1002/acr.21591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Majeski EI, Paintlia MK, Lopez AD et al. Respiratory reovirus 1/L induction of intraluminal fibrosis, a model of bronchiolitis obliterans organizing pneumonia, is dependent on T lymphocytes. Am J Pathol 2003;163:1467–79. 10.1016/S0002-9440(10)63504-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cordier JF. Organising pneumonia. Thorax 2000;55:318–28. 10.1136/thorax.55.4.318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parambil JG, Myers JL, Lindell RM et al. Interstitial lung disease in primary Sjögren syndrome. Chest 2006;130:1489–95. 10.1378/chest.130.5.1489 [DOI] [PubMed] [Google Scholar]
- 9.Schlesinger C, Koss MN. The organizing pneumonias: a critical review of current concepts and treatment. Treat Respir Med 2006;5:193–206. 10.2165/00151829-200605030-00005 [DOI] [PubMed] [Google Scholar]
- 10.Ramos-Casals M, Brito-Zerón P, Sisó-Almirall A et al. Topical and systemic medications for the treatment of primary Sjögren's syndrome. Nat Rev Rheumatol 2012;8:399–411. 10.1038/nrrheum.2012.53 [DOI] [PubMed] [Google Scholar]
- 11.Komai T, Shoda H, Yamaguchi K et al. Neuromyelitis optica spectrum disorder complicated with Sjogren syndrome successfully treated with tocilizumab: a case report. Mod Rheumatol 2013. [DOI] [PubMed] [Google Scholar]
- 12.Elhai M, Meunier M, Matucci-Cerinic M et al. EUSTAR (EULAR Scleroderma Trials and Research group). Outcomes of patients with systemic sclerosis-associated polyarthritis and myopathy treated with tocilizumab or abatacept: a EUSTAR observational study. Ann Rheum Dis 2013;72:1217–20. 10.1136/annrheumdis-2012-202657 [DOI] [PubMed] [Google Scholar]
- 13.Andres M, Vela P, Romera C. Marked improvement of lung rheumatoid nodules after treatment with tocilizumab. Rheumatol Oxf Engl 2012; 51:1132–4. 10.1093/rheumatology/ker455 [DOI] [PubMed] [Google Scholar]
- 14.Keidel SM, Hoyles RK, Wilkinson NM. Efficacy of tocilizumab for interstitial lung disease in an undifferentiated autoinflammatory disorder partially responsive to anakinra. Rheumatol Oxf Engl 2014;53:573–4. 10.1093/rheumatology/ket211 [DOI] [PubMed] [Google Scholar]
- 15.Kawashiri SY, Kawakami A, Sakamoto N et al. A fatal case of acute exacerbation of interstitial lung disease in a patient with rheumatoid arthritis during treatment with tocilizumab. Rheumatol Int 2012;32:4023–6. 10.1007/s00296-010-1525-z [DOI] [PubMed] [Google Scholar]
- 16.Wendling D, Vidon C, Godfrin-Valnet M et al. Exacerbation of combined pulmonary fibrosis and emphysema syndrome during tocilizumab therapy for rheumatoid arthritis. Joint Bone Spine 2013;80:670–1. 10.1016/j.jbspin.2013.03.009 [DOI] [PubMed] [Google Scholar]
- 17.Hadjinicolaou AV, Nisar MK, Bhagat S et al. Non-infectious pulmonary complications of newer biological agents for rheumatic diseases—a systematic literature review. Rheumatology (Oxford) 2011;50:2297–305. 10.1093/rheumatology/ker289 [DOI] [PubMed] [Google Scholar]
- 18.Ikegawa K, Hanaoka M, Ushiki A et al. A case of organizing pneumonia induced by tocilizumab. Intern Med 2011;50:2191–3. 10.2169/internalmedicine.50.5497 [DOI] [PubMed] [Google Scholar]