Abstract
Objective To evaluate the incidence and consequences of uterine rupture in women who have had a delivery by caesarean section.
Design Systematic review.
Data sources Medline, HealthSTAR, Cochrane Database of Systematic Reviews, Cochrane Controlled Trials Register, National Centre for Reviews and Dissemination, reference lists, and national experts. Studies in all languages were eligible if published in full.
Review methods Methodological quality was evaluated for each study by using criteria from the United States Preventive Services Task Force and the National Health Service Centre for Reviews and Dissemination. Uterine rupture was categorised as asymptomatic or symptomatic.
Results We reviewed 568 full text articles to identify 71 potentially eligible studies, 21 of which were rated at least fair in quality. Compared with elective repeat caesarean delivery, trial of labour increased the risk of uterine rupture by 2.7 (95% confidence interval 0.73 to 4.73) per 1000 cases. No maternal deaths were related to rupture. For women attempting vaginal delivery, the additional risk of perinatal death from rupture of a uterine scar was 1.4 (0 to 9.8) per 10 000 and the additional risk of hysterectomy was 3.4 (0 to 12.6) per 10 000. The rates of asymptomatic uterine rupture in trial of labour and elective repeat caesarean did not differ significantly.
Conclusions Although the literature on uterine rupture is imprecise and inconsistent, existing studies indicate that 370 (213 to 1370) elective caesarean deliveries would need to be performed to prevent one symptomatic uterine rupture.
Introduction
Since at least 1916, the time of Edward Cragin's famous statement, “Once a caesarean always a caesarean,”1 the medical profession has been concerned about the risk of catastrophic uterine rupture for women whose previous deliveries were by caesarean section. In the past 20 years, trial of labour has been encouraged for women who have had a caesarean delivery. Recent studies reporting that mother and fetus may be at greater risk than previously thought, largely because of uterine rupture,2,3 have stirred controversy about the safety of vaginal birth after caesarean section.4-6
We sought to determine the incidence and consequences of uterine rupture for women with a low transverse caesarean section scar or unclassified scar (for which the direction of incision on the uterus is uncertain). We also searched for evidence about the effect of expanding the criteria for eligibility and of medical induction, and augmentation on maternal and infant morbidity and mortality. This review derives from an evidence based report conducted for the US Agency for Healthcare Research and Quality.7
Methods
Searching
The primary investigator and a medical librarian searched both Medline and HealthSTAR (1980 to 2002), using “vaginal birth after cesarean/caesarean”, “trial of labor/labour”, “trial of scar”, “labor/labour”, “delivery”, “vaginal birth”, “vaginal delivery”, “cesarean/caesarean”, “home childbirth”, “natural childbirth”, “obstetrical extraction”, and “uterine rupture” as search terms. We searched the Cochrane Database of Systematic Reviews, Cochrane Controlled Trials Register, the Database of Abstracts of Reviews of Effectiveness, reference lists of pertinent studies, reviews, and expert recommendations. The search was limited to 1980 or later, as in 1980 a National Institutes of Health consensus conference established vaginal birth after caesarean as an acceptable choice.8
Selection
We considered controlled trials, cohort studies, case-control studies, and case series with at least 10 cases. We sought studies comparing uterine rupture rates and sequelae in women with low transverse caesarean scar or unclassified scar who chose trial of labour or elective repeat caesarean delivery (ERCD), and if these were not available, non-comparative studies reporting uterine rupture rates and subsequent morbidity or mortality. A study was considered relevant if it was in full manuscript form, included women with low transverse caesarean or unclassified scar, provided data regarding uterine rupture, and had been conducted in a developed country. We excluded studies focusing on particular medical or obstetric conditions (for example, gestational diabetes or pre-eclampsia). Non-English articles with English abstracts were included if they provided information not found in English-language literature.
Two investigators independently reviewed random titles and abstracts to establish reliable, reproducible inclusion criteria. Once reliability was established (κ of ≥ 0.80), the primary investigator reviewed the remaining titles and abstracts.
Validity assessment
Two investigators independently rated the quality of the study, using criteria from the US Preventive Services Task Force and the NHS Centre for Reviews and Dissemination.9,10 Studies received a poor rating if the groups assembled were not comparable (for example, elective repeat caesarean patients were not eligible for trial of labour); if classification of uterine rupture was unreliable or invalid, or classification was not applied equally among groups; if key confounders, such as number of caesarean deliveries or direction of prior caesarean (vertical or transverse) were given little or no attention; if there was differential attrition or, for randomised control trials, if intention to treat analysis was lacking.
All studies needed to define uterine rupture, or to provide enough information about rupture events to allow for classification and determination of likely association to prior caesarean section. We excluded studies that had used ICD-9 codes to identify uterine rupture because ICD-9 codes are inaccurate: in one study, only 480 (39.8%) of 1244 suspected ruptures identified from ICD-9 codes were confirmed as true ruptures after records were reviewed.11
Data abstraction and study characteristics
From each study, two reviewers independently abstracted study design and setting; patients' characteristics; definition, rates, and predictors of uterine rupture; maternal and fetal outcomes; and methods of assessing or adjusting for confounders. When reviewers disagreed, agreement was reached by consensus.7
Terminology for rupture was inconsistent among studies, yet was crucial for understanding the incidence and consequences of the condition. We used “symptomatic uterine rupture” when uterine separation was diagnosed at laparotomy performed for maternal or fetal signs or symptoms associated with uterine rupture, such as fetal heart rate disturbances or maternal bleeding, and “asymptomatic uterine rupture” for uterine separation without signs or symptoms.
Quantitative data synthesis
We conducted several meta-analyses to estimate the risks associated with trial of labour and clinical factors that influence risk. Our primary outcomes of interest were the additional absolute risks of symptomatic uterine rupture, and of maternal or perinatal death, or hysterectomy, related to rupture, when trial of labour rather than repeat caesarean delivery was chosen. We were also interested in risks associated with management techniques such as induction or augmentation of labour, as well as signs or symptoms predicting poor outcomes from uterine rupture. Absolute risk differences and rates were calculated and pooled by random effects and fixed effects models, which weighted studies by the inverse of their variances, giving more weight to precise studies. To reduce bias, we included only studies of fair to good quality. Two investigators independently rated the quality of the study, using criteria from the US Preventive Services Task Force and the NHS Centre for Reviews and Dissemination.9,10 Studies received a poor rating if the groups assembled were not comparable (for example, elective repeat caesarean patients were not eligible for trial of labour); if classification of uterine rupture was unreliable or invalid, or classification was not applied equally among groups; if key confounders, such as number of caesarean deliveries or direction of prior caesarean (vertical or transverse) were given little or no attention; if there was differential attrition or, for randomised control trials, if intention to treat analysis was lacking. A study received a fair rating if generally comparable groups were assembled but some question remained whether minor differences occurred in follow up; if measurement of uterine rupture was acceptable (for example, no definition but study details allowed for classification) and generally applied equally; if some, but not all, potential confounders were accounted for; and for randomised controlled trials, if intention to treat analysis was performed. As results from fixed effects and random effects models did not differ, we present the results from the random effects models.
Results
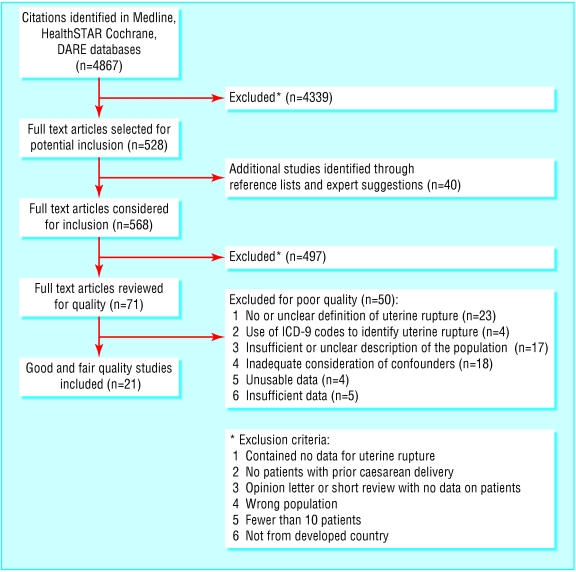
We identified 4867 citations, reviewed 568 full text articles, and identified 21 studies of fair to good quality (fig 1). We excluded 497 studies because they did not meet inclusion criteria. No articles written in languages other than English met the inclusion criteria. Of the 71 studies considered potentially eligible, 50 received a poor rating (16 for two or more reasons).
Fig 1.
Eligibility of studies for inclusion in systematic review
Study characteristics
The included studies consisted of two large, population based retrospective studies,2,12 15 prospective cohort studies,13-27 two case-control studies,28,29 and two case series30,31 (table 1). Cohort studies defined the trial of labour group as women who had had a caesarean delivery (sometimes including women with scar of unclassified origin or low vertical scar) who had a trial of labour ending in vaginal or caesarean delivery. Often the repeat caesarean group was defined as women without a trial of labour (sometimes including women for whom caesarean section was indicated). Terms describing severity of rupture were used inconsistently; the term “dehiscence” usually signified incidental findings of a scar defect at caesarean or uterine exploration after vaginal delivery, but in three studies14,21,28 it also included symptomatic ruptures. Thirteen studies used the terms “complete uterine rupture” or “true uterine rupture,”2,12,13,15-19,22,23,29-31 but these gave inconsistent definitions: separation requiring operative intervention (for example, emergent caesarean for maternal bleeding or fetal heart rate abnormality with scar separation); extrusion of fetus at caesarean for failure to progress; scar with bleeding, haematoma formation, or extrusion of fetus; or exclusively for separations with serious maternal or infant consequences (hysterectomy or death).
Table 1.
Quality of study, definitions used, and predictors of uterine rupture
| Study, location | Quality | Terms and definitions | Potential predictors of uterine rupture reported (No with predictor/total cases of uterine rupture) |
|---|---|---|---|
| McMahon 1996,2 Canada | Good | Uterine rupture: symptomatic defect of entire uterine wall requiring operative intervention | Not reported |
| Smith 2002,12 Scotland | Fair | Uterine rupture: not reported | Not applicable |
| Duff 1988,14 USA | Good | Uterine scar dehiscence: disruption of any portion of lower segment incision (used to describe a patient with vaginal bleeding and fetal bradycardia who delivered by repeat CD; Apgars 4, 8; 60% of scar disrupted) | 1/1 vaginal bleeding and fetal bradycardia |
| Flamm 1988,15 USA | Fair | Asymptomatic uterine window: small defects visualised at CD or palpated at VD | No sign: 1/3 CD for failure to progress |
| Fetal distress: 1/3 | |||
| Abdominal pain: 1/3 | |||
| Cowan 1994,13 USA | Fair | Bloodless uterine scar dehiscence: any defect in the pre-existing caesarean scar with no maternal or fetal compromise
|
Abnormal fetal tracing (immediate and prolonged fetal bradycardia): 5/5 |
| True uterine rupture: Scott's definition - “a complete separation of the wall of the pregnant uterus, with or without expulsion of the fetus, endangering the life of the mother or fetus” (one rupture occurred at fundus with an intact uterine scar) | Oxytocin: 3/5 UR (1 vertical, 1-2 prior CD) | ||
| Epidural: 1/5 UR | |||
| Flamm 1994,16 USA | Fair | Uterine rupture: any defect that involved the entire uterine wall or was symptomatic or required operative intervention | Not reported |
| Flamm 1990,17 USA | Fair | Uterine rupture: any defect that involved the entire uterine wall or was symptomatic or required operative intervention. (2/10 UR occurred after VD) | Abnormal EFM: 7/10 “variable or prolonged bradycardia most common warning sign” |
| Oxytocin: 6/10 UR; NS v non-rupture | |||
| Martin 1983,18 USA | Fair | Dehiscence: non-traumatic separation of the uterine scar without bleeding or extrusion of fetus into wound
|
Not reported |
| Uterine rupture: scar separation with bleeding, haematoma formation, or extrusion of the fetus | |||
| Meehan 1989,19 Ireland | Fair | Bloodless dehiscence: dehiscence of uterine scar not associated with bleeding; it includes small “window” defects and larger defects in which bleeding was not a feature
|
Fetal distress: 1/1 UR |
| True rupture: rupture of the uterine scar accompanied by intra-abdominal or vaginal bleeding | Oxytocin: NS | ||
| Epidural: NS | |||
| Meier 1982,20 USA | Fair | Scar dehiscence: uterine scar separation (incidentally noted at caesarean delivery) | No sign reported: 2/2 dehiscences found at CD |
| Paul 1985,21 USA | Fair | Uterine dehiscence: any palpable and/or visualised uterine defect (further subgrouped into dehiscences that required no intervention and those that did require intervention, which were termed uterine rupture) | Abdominal pain: 2/5 UR |
| Postpartum bleeding: 1/5 UR | |||
| No sign reported: arrest of dilation found UR | |||
| Partial extrusion of fetus: 1/5 UR | |||
| Abnormal fetal tracing: 1/5 UR | |||
| Note: 25 CD for “fetal distress” (18/751 TOL v 7/458 repeat CD) (7/18 TOL emergent CD, 2/7 ERCD emergent CD) | |||
| Phelan 1987,22 USA | Fair | Uterine dehiscence: scar separation not requiring operative intervention | Fetal distress such as severe variable decelerations or prolonged fetal bradycardia most frequent sign, no cases of UR with maternal pain and changes in uterine tone |
| Stovall 1987,23 USA | Fair | Dehiscence: palpable or visualised defect in previous uterine scar
|
Pain, vaginal bleeding, loss of uterine tone in the one case of UR, NR difference between UR and non-UR |
| Uterine window: dehiscence not requiring surgical intervention or blood component replacement
|
|||
| Uterine rupture: dehiscence requiring intervention | |||
| Connolly 2001,28 Ireland | Fair | Scar dehiscence (further classified as partial and complete): not reported. (Life threatening complication, “common symptoms include fetal distress, abdominal pain, scar tenderness, vaginal bleeding; rarely massive hemorrhage and hypovolemic shock may be presenting symptom”) | Fetal distress: 9/13 cases v 2/13 controls (OR 12.3; 95% CI: 1.9 to 81) |
| Scar tenderness: 8/13 cases v 0/13 controls | |||
| Vaginal bleeding: 6/13 cases v 0/13 controls | |||
| Oxytocin: Induction: 0/13 cases v 2/13 controls; augmentation: 10/13 cases v 3/13 controls (OR 4.5; 95% CI 0.9313 to 42.8) | |||
| Epidural: 5/13 cases v 8/13 controls (OR 2.5; 95% CI 0.41 to 26.2) | |||
| Maternal age (mean): 31.5 cases v 27.5 controls (OR per 1 year in age 1.35; 95% CI 1.03 to 2.19) | |||
| Parity (mean): 3.15 cases v 2.85 controls (OR per 1-unit 1.59; 95% CI 0.17 to 18.9) | |||
| Prior VD (before or after CD): 7/13 cases v 5/13 controls (OR 1.29; 95% CI 0.2175 to 11.86) | |||
| GA (mean): 39.3 cases v 40.3 controls; NS | |||
| Leung 1993,29 USA | Fair | Uterine rupture: uterine scar separation and emergent laparotomy, acute fetal distress necessitating operative intervention, or acute maternal bleeding manifested by hypotension or shock | Not reported but included in case series data |
| Any oxytocin: 54/70 cases v 39/70 controls (OR 2.7; 95% CI 1.2 to 6.0) | |||
| Induction = 11/70 cases v 10/70 controls | |||
| Augmentation = 43/70 cases v 29/70 controls | |||
| Epidural: 29/70 cases v 19/70 controls (OR 1.9; 95% CI 0. to 4.1) | |||
| Maternal age and parity: Not reported | |||
| Prior VBAC: 11/70 cases v 16/70 controls (OR 0.5; 95% CI 0.1 to 1.6) | |||
| CD for CPD: 22/70 cases v 21/70 controls (OR 0.9; 95% CI 0. to 2.0) | |||
| Unclassified scar: 61/70 cases v 59/70 (OR 1.3; 95% CI 0. to 3.1) >1CD: 23/70 cases v 11/70 controls (OR 2.6; 95% CI 1. to 6.4) | |||
| Bujold 2002,31 Canada | Fair | Complete uterine rupture: “uterine scar separation with the overlying visceral peritoneum (uterine serosa) opened; all uterine ruptures had been confirmed at the time of emergency laparotomy; records with uterine dehiscences (not defined) were excluded” | Fetal tracing abnormality: 20/23 patients |
| Abdominal pain: 1/23 first symptom (3 with abnormal tracings also reported pain) | |||
| Vaginal bleeding: (1 of the patients with abnormal fetal tracing) | |||
| Haematuria: 2/23 first sign | |||
| Oxytocin: 5/9 metabolic acidosis v 9/14 without acidosis; NS | |||
| Induction of labour: 3/9 with acidosis v 5/14 without; NS | |||
| Epidural: 8/9 with acidosis v 12/14 without acidosis; NS | |||
| Leung 1993,30 USA | Fair | Uterine rupture: uterine scar separation and emergent laparotomy, acute fetal distress necessitating operative intervention, or acute maternal bleeding manifested by hypotension or shock | Fetal tracing abnormality: 91/99 |
| Pain: 13/99 | |||
| Vaginal bleeding: 11/99 | |||
| Oxytocin: NS in extrusion | |||
| Epidural: NS in extrusion | |||
| Maternal age: NS for extrusion | |||
| Parity: NS for extrusion | |||
| Prior VBAC: 16 patients with prior VBAC had rupture | |||
| CD for CPD: NS |
CD=caesarean delivery; CI=confidence interval; CPD=cephalopelvic disproportion; EFM=electrofetal monitor; ERCD=elective repeat caesarean delivery; GA=gestational age; NS=no significant difference; OR=odds ratio; UR=uterine rupture; VBAC=vaginal birth after caesarean ; VD=vaginal delivery.
Data synthesis
Symptomatic uterine rupture
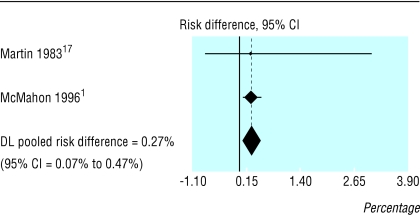
Ten of 11 observational studies provided the best evidence on the occurrence of symptomatic rupture (table 2).2,13-18,20,22,23 Symptomatic rupture rates in prospective cohort studies ranged from 0/1000 in a small study20 to 7.8/1000 in the largest,16 with a pooled rate of 3.8 (95% confidence interval 1.3 to 6.2) per 1000 trials of labour. Only one retrospective and one prospective study provided comparative data for symptomatic rupture in trial of labour versus elective repeat caesarean (fig 2).2,18 When combined, these data show an additional risk of 2.7 (0.73 to 4.73) symptomatic ruptures per 1000.
Table 2.
Results of studies comparing trial of labour and emergency repeat caesarean delivery
|
Sample size
|
Uterine exploration
|
No (%) of uterine ruptures
|
|||||
|---|---|---|---|---|---|---|---|
| Study | Characteristics of population | TOL | ERCD | Symptomatic | Asymptomatic | Reported associated major morbidity | |
| Cowan 199413 | All vertical scars excluded; unclassified scars and more than 1 previous caesarean allowed | 593 | Not reported | TOL - 5 (0.8) | Not reported | 1 fetus with severe neurological sequelae | |
| Flamm 199416 | All vertical scars excluded; unclassified scars allowed | 5022 | 2207 | Discretion | TOL - 39 (0.8) | Not reported | 0 maternal and neonatal deaths, 3/39 hysterectomies |
| Duff 198814 | One prior LTCD and unclassified scar not allowed | 227* | Yes | TOL - 1 (0.4) | Not reported | 0 maternal or perinatal deaths | |
| Flamm 198815 | LTCD, unclassified scar and more than 1 previous caesarean allowed | 1776† | Yes (discretion?) | TOL - 3 (0.2) | TOL - 11 (0.6) | Symptomatic UR: TOL - 0 maternal and neonatal deaths, 1 hysterectomy | |
| Flamm 199017 | LTCD, unclassified scars and more than 1 previous caesarean allowed | 3957 | Majority no longer did | TOL - 7 (0.2) | Not reported | 0 maternal deaths; 1 hysterectomy with infant born vaginally, Apgar 9; 3 infants with Apgar <7 (one cerebral palsy at 15 months); 1 perinatal death related to rupture | |
| Phelan 198722 | Low vertical scars, unclassified scars, LTCD during 2nd year and more than 1 previous caesarean allowed | 1796 | 314 | Yes | TOL - 5 (0.3) | TOL - 34 (1.9) ERCD - 7 (2.2) | Symptomatic UR: TOL - 1 neonatal death, post rupture, scar intact, fetal bradycardia (sign), 4600g Apgar 0,0,3; none in transverse scar |
| Stoval 198723 | More than 1 LTCD or LVCD allowed; not clear what was done with unclassified scars | 272 | Yes | TOL - 1 (0.4) | TOL - 6 (2.2) | Symptomatic UR: TOL - 0 maternal or fetal deaths | |
| Paul 198521 | Not more than 1 previous caesarean allowed; low vertical scars, unclassified scars and LTCD allowed | 751 | 157 | Yes | TOL - 5 (0.7)‡ | TOL - 11 (1.5)‡ ERCD - 4 (2.5)‡ | Symptomatic UR: TOL - 0 maternal deaths, 2 fetal deaths (classical incision 3 prior CD, fundal incision), 0 hysterectomies |
| Martin 198318 | 1 or more LTCD or LVCD allowed, no rupture occurred in the 76 with prior vertical scars | 162 | 555 | Yes | TOL - 1 failed (0.6) ERCD - 2 (0.4) | TOL - 1 successful, 3 failed (2.5) ERCD - 4 (0.7) | Symptomatic UR: TOL - 0 maternal or fetal deaths ERCD - 0 maternal or perinatal deaths, 0 hysterectomies |
| Meier 198220 | 1 or more LTCD allowed, no “obvious CPD” allowed | 207 | 62 | Not reported | Not reported | TOL - 1 (0.48) ERCD −1 (1.6) | Symptomatic UR: TOL - 0 maternal and fetal deaths |
| McMahon 19962 | 1 LTCD allowed; not clear what was done with unclassified scars | 3249 | 2889 | Not reported | TOL - 10 (0.3) ERCD - 1 (0.03) | Not reported | TOL - 0 maternal deaths, 2 perinatal deaths, 2 hysterectomies; ERCD - 0 maternal or perinatal deaths, 0 hysterectomies |
CPD=cephalopelvic disproportion; ERCD=elective repeat caesarean delivery; LTCD=low transverse caesarean delivery; LVCD=low vertical caesarean delivery; TOL=trial of labour; UR=uterine rupture.
Called dehiscence but symptomatic.
One third still had thin layer of peritoneum over scar.
Included in Phelan 198722
Fig 2.
Symptomatic uterine rupture: trial of labour versus elective repeat caesarean delivery
Perinatal deaths—Classification and reporting inconsistencies make it difficult to assess the risk of perinatal death due to rupture. Six cohort studies14-16,18,20,23 including from 162 to 5022 trials of labour reported no perinatal deaths related to rupture; three other cohort studies (3957,17 3249,2 and 1796 trials of labour22) reported rates of 14% (1/7), 20% (2/11), and 60% (3/5),2,17,22 and two case series reported rates of 6% and 4%.30,31 Overall, six deaths were reported in 74 symptomatic ruptures, corresponding to an additional 1.4 (0 to 9.8) perinatal deaths per 10 000 trials of labour.2,13-18,20-23,30,31 By contrast, an analysis of linked data from the Scottish Morbidity Record and Stillbirth and Neonatal Death Enquiry found 20 perinatal deaths among 15 515 trials of labour compared to none among 9014 planned caesareans.12 Their rate of 12.9 (7.9 to 19.9) per 10 000 is almost 10 times higher than our estimate. The death rate for trial of labour (20 perinatal deaths: 8 in vaginal deliveries and 12 in emergent caesarean deliveries) may be spuriously high—and that for repeat caesarean delivery spuriously low—because all emergent caesarean deliveries and vaginal deliveries were classified as trials of labour regardless of intended delivery route. In a separate study, two of nine (22%) emergent caesareans were in women who requested repeat caesarean.21 If this proportion were applied to the Scottish study, three of the 12 emergent perinatal deaths would have occurred in the planned repeat caesarean group, and the difference would no longer be statistically significant.
Hysterectomy—In the five cohort studies reporting on hysterectomies related to rupture, seven hysterectomies occurred in 60 symptomatic ruptures (13%; 4% to 27%).2,14-17 These data indicate that 3.4 (0 to 12.6) per 10 000 women choosing trial of labour sustain a rupture that would necessitate hysterectomy.
Asymptomatic uterine rupture
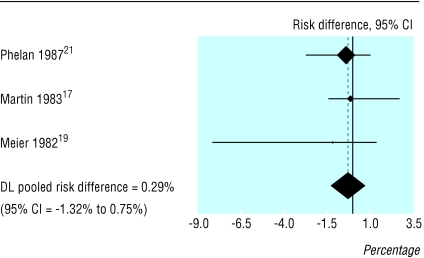
Eight prospective cohort studies reported performing uterine exploration after vaginal birth after a previous caesarean (table 2).14-18,21-23 Five reported routinely performing manual uterine exploration after vaginal birth. 14,15,18,22,23 In these studies, rates of asymptomatic uterine rupture, or dehiscence, ranged from 5/1000 to 20/1000,20,23 with a mean weighted average rate of 13 per 1000 trials of labour. In three comparative studies the rates for asymptomatic rupture in trial of labour and elective repeat caesarean were not significantly different (16 (5.4 to 28.4) per 1000 v 13 (4.3 to 26.2) per 1000; fig 3).18,20,22
Fig 3.
Asymptomatic uterine rupture: trial of labour versus elective repeat caesarean delivery
Increased incidence with induction
Oxytocin use was associated with a twofold to fourfold increased risk of uterine rupture in two case-control studies.28,29 This finding has not been confirmed in cohort studies or controlled trials. In prospective cohort studies, the use of oxytocin13,21,23-25 or prostaglandin26,27 was not associated with a higher risk of uterine rupture.
Predictors of major morbidity from rupture
Abnormalities in fetal heart rate were the most common sign of rupture, occurring in 55-87% of uterine rupture events. Other signs reported were vaginal bleeding, pain, and disturbances of uterine contractions.
No properly designed studies have directly evaluated whether fetal heart rate signs predict—or whether acting on them prevents—mortality and major morbidity related to uterine ruptures. Two case series that examined whether delays in delivery after fetal bradycardia were associated with infant morbidity had conflicting results.30,31 Leung et al found that fetal heart rate disturbances occurred in 91/99 uterine ruptures (92%), with 56 having prolonged deceleration only.30 No prolonged clinical morbidity (death, asphyxia, or intubation) occurred when delivery took place within 17 minutes of onset of deceleration, but four cases (1 asphyxia and 3 intubations) occurred in infants delivered after 17 minutes. The three neonates requiring intubation were extubated within 24 hours (range 1-24 hours) and were discharged from the hospital without adverse sequelae. If these three temporary neonatal intubations were excluded, one neonatal asphyxia and no deaths would remain. A more recent case series of 23 uterine ruptures included four cases of brain injury or death. The authors found no relation between outcome and interval between onset of fetal heart rate deceleration to delivery.31
Discussion
This report aimed to answer a question on the minds of patients, providers, and policy makers: what additional risks does a woman who has had a caesarean delivery assume if she chooses to attempt vaginal delivery rather than have a caesarean section? Most of the literature focuses on the risk of uterine rupture in the trial of labour group, with an implicit assumption that this risk would be eliminated by elective repeat caesarean delivery. If this assumption were true, it would take 263 elective repeat caesareans to prevent one uterine rupture due to trial of labour. However, elective repeat caesarean delivery is not guaranteed to prevent uterine rupture. In two comparative studies, trial of labour posed an additional risk of 0.27% (2.7/1000; 95% confidence interval 0.73 to 4.73)2,18; thus it would take 370 (213 to 1370) elective repeat caesareans to prevent one symptomatic uterine rupture due to trial of labour.
Morbidity
Patients are also concerned about additional morbidity. About 5% of symptomatic uterine ruptures were associated with perinatal mortality and 13% with hysterectomy. This translates to 7142 elective repeat caesareans to prevent one rupture related perinatal death and 2941 to prevent one rupture related hysterectomy. It would take only one misclassified case of symptomatic uterine rupture in the smaller study and five in the largest2 to entirely negate the observed difference in symptomatic uterine rupture between groups. Caution must be used in interpreting these results.
Serious morbidity or mortality due to uterine rupture is rare, making it difficult to study. As a result, studies have focused on the occurrence of uterine rupture rather than how often bad outcomes result from it. The existing evidence is sufficient to conclude there is an increased risk of symptomatic uterine rupture for trial of labour over elective repeat caesarean and that caesarean delivery is not completely protective. However, most uterine ruptures do not have serious consequences, and patients and clinicians may wish to base decisions on the likelihood of significant morbidity or mortality for the mother and baby rather than on the occurrence of uterine rupture itself.
Induction
We found insufficient evidence to make a reliable estimate of the risk of uterine rupture when oxytocin or prostaglandins are used during labour. There is a temptation to make a conclusion on the use of prostaglandins to induce trials of labour, especially with the large effect reported by Lydon-Rochelle et al (relative risk of uterine rupture 15.6; 8.1 to 30).3 We excluded this study because the use of ICD-9 codes to identify uterine rupture has been shown to be only about 40% accurate.11 If the Lydon-Rochelle study missed 60% of cases, we would still expect to find a significant increase in uterine rupture among women receiving prostaglandins: studies using better methods of identifying ruptures produce a relative risk of approximately 6. Prostaglandins did not increase the risk of uterine rupture in other observational studies. Although the studies we reviewed were much smaller, overall the number of women receiving prostaglandins was similar in the largest cohort study included and the Lydon-Rochelle study. Whether prostaglandins really increase the risk is still open to question.
The relation between fetal heart rate disturbances and uterine rupture is unclear. Studies examining the relation between duration of fetal heart rate disturbance, particularly prolonged bradycardia and adverse perinatal outcomes, report conflicting results. Because the definition of uterine rupture often includes uterine ruptures that are discovered when a caesarean section is done because of fetal heart rate disturbances, it is impossible to determine the accuracy of fetal heart rate as a premonitory sign. Finding a uterine wall defect in this context does not necessarily signify that the defect was the cause of the fetal heart rate abnormality or that morbidity in the infant would be attributable directly to rupture.
Methodological issues
Existing studies do not permit a precise estimate of the frequency of serious events, which occur once in every 1000-10 000 deliveries. A randomised trial of this question would have to be huge and might fail if women preferred to make their own decision rather than accept a random assignment to trial of labour or elective repeat caesarean. For an observational study, the major challenges are to accurately classify exposures (trial of labour, elective repeat caesarean, induction, and augmentation) and outcomes (rupture related events). Attempts have been made to classify a labour after delivery as a trial of labour or elective repeat caesarean, but these are fraught with bias. For example, women who intend to have a trial of labour but undergo early labour and decide on caesarean section are difficult to distinguish from women who “fail” trial of labour. Accounting for differences in the time of exposure is important, since women who choose elective repeat caesarean commonly deliver before 40 weeks whereas women choosing trial of labour may deliver up to 43 weeks.
Although degrees of measurement bias and misclassification are unavoidable, a multicentre prospective cohort study or national registry would offer the best opportunity to guide the design of effective preventive strategies. Meanwhile, this review indicates that there is less than a 1% chance that a woman with a low transverse caesarean scar or scar of unclassified origin will sustain a uterine rupture as a consequence of attempting vaginal delivery; that elective repeat caesarean does not always prevent uterine rupture; and that for more than two thirds of women who experience a uterine rupture, neither they nor their infant will have severe health consequences related to uterine rupture.
What is already known
Perceptions of high risk for uterine rupture cause many patients and practitioners to avoid vaginal birth after caesarean delivery
Epidemiological studies show an association between previous caesarean section and uterine rupture
What this study adds
Symptoms of uterine rupture were more common in women undergoing trial of labour than planned repeat caesarean delivery, but the additional risk is less than previously thought
For every 10 000 women attempting trial of labour there would be 27 additional symptomatic uterine ruptures, 1.4 perinatal deaths related to rupture, and 3.4 hysterectomies related to rupture
Studies need to use standard and precise definitions for uterine rupture and related outcomes
Supplementary Material
 A table with details of included studies is on bmj.com
A table with details of included studies is on bmj.com
Contributors: J-MG and MSMcD contributed to the conception and design and analysis of data and drafting and revising of the article. PO contributed to the design and assembly of data, drafting and revising of the article, technical support. PN contributed to the design, revising of the article, and technical support. BKSC contributed to analysis of data, drafting and revising of the article, and statistical expertise. MH contributed to conception and design, interpretation of data, drafting and revising of the article. J-MG, MSMcD, PO, and MH approved the final version. J-MG is guarantor.
Funding: This study was conducted by the Oregon Health & Science University Evidence-based Practice Center under contract to the Agency for Healthcare Research and Quality, Rockville, MD (contract 290-97-0018, task order No 9). Support for J-MG was also provided by the Agency for Healthcare Research and Quality grant No 1 K08 HS11338-01.
Competing interests: None declared.
Ethical approval: Not required.
References
- 1.Cragin EB. Conservatism in obstetrics. N Y Med J 1916;104: 1-3. [Google Scholar]
- 2.McMahon MJ, Luther ER, Bowes WA, Olshan AF. Comparison of a trial of labor with an elective second cesarean section. N Engl J Med 1996;335: 689-95. [DOI] [PubMed] [Google Scholar]
- 3.Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP. Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med 2001;345: 3-8. [DOI] [PubMed] [Google Scholar]
- 4.Greene MF. Vaginal delivery after cesarean section—is the risk acceptable? [letter; comment]. N Engl J Med 2001;345: 54-5. [DOI] [PubMed] [Google Scholar]
- 5.Flamm BL. Once a cesarean, always a controversy. Obstet Gynecol 1997;90: 312-5. [DOI] [PubMed] [Google Scholar]
- 6.Scott JR. Putting elective cesarean into perspective [comment]. Obstet Gynecol 2002;99: 967-8. [DOI] [PubMed] [Google Scholar]
- 7.Guise J, McDonagh M, Hashima J, Kraemer D, Eden K, Berlin M, et al. Vaginal birth after cesarean (VBAC). Evidence report/technology assessment (prepared by the Oregon Health & Science University Evidence-based Practice Center under contract N. 290-97-0018). Rockville, MD: Agency for Healthcare Research and Quality Publication, 2003.
- 8.Cesarean childbirth: report of a consensus development conference sponsored by the NICHHD in Conjunction with the National Center for Health Care Technology and assisted by the Office for Medical Applications of Research. NIH Publication. 1981; 82-2067.
- 9.Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Preventive Med 2001;20(suppl): 21-35. [DOI] [PubMed] [Google Scholar]
- 10.Khan K, Riet G, Popay J, Nixon J, Kleijnen J. Study quality assessment. Undertaking systematic reviews of research effectiveness: CRD's guidance for those carrying out or commissioning reviews. York: NHS Centre for Reviews and Dissemination, 2001.
- 11.Weiss J, Nannini A, Fogerty S, Sachs B. Use of hospital discharge data to monitor uterine rupture—Massachusetts, 1990-1997; US Department of Health & Human Services. MMWR Morbid Mortal Wkly Rep 2000;49: 245-8. [PubMed] [Google Scholar]
- 12.Smith GCS, Pell JP, Cameron AD, Dobbie R. Risk of perinatal death associated with labor after previous cesarean delivery in uncomplicated term pregnancies. JAMA 2002;287: 2684-90. [DOI] [PubMed] [Google Scholar]
- 13.Cowan RK, Kinch RA, Ellis B, Anderson R. Trial of labor following cesarean delivery. Obstet Gynecol 1994;83: 933-6. [DOI] [PubMed] [Google Scholar]
- 14.Duff P, Southmayd K, Read JA. Outcome of trial of labor in patients with a single previous low transverse cesarean section for dystocia. Obstet Gynecol 1988;71: 380-4. [PubMed] [Google Scholar]
- 15.Flamm BL, Lim OW, Jones C, Fallon D, Newman LA, Mantis JK. Vaginal birth after cesarean section: results of a multicenter study. Am J Obstet Gynecol 1988;158: 1079-84. [DOI] [PubMed] [Google Scholar]
- 16.Flamm BL, Goings JR, Liu Y, Wolde-Tsadik G. Elective repeat cesarean delivery versus trial of labor: a prospective multicenter study. Obstet Gynecol 1994;83: 927-32. [DOI] [PubMed] [Google Scholar]
- 17.Flamm BL, Newman LA, Thomas SJ, Fallon D, Yoshida MM. Vaginal birth after cesarean delivery: results of a 5-year multicenter collaborative study. Obstet Gynecol 1990;76: 750-4. [DOI] [PubMed] [Google Scholar]
- 18.Martin JN, Harris BA, Huddleston JF, Morrison JC, Propst MG, Wiser WL, et al. Vaginal delivery following previous cesarean birth. Am J Obstet Gynecol 1983;146: 255-63. [DOI] [PubMed] [Google Scholar]
- 19.Meehan FP, Burke G. Trial of labour following prior section: a 5 year prospective study (1982-1987). Eur J Obstet, Gynecol Reprod Bio 1989;31: 109-17. [DOI] [PubMed] [Google Scholar]
- 20.Meier PR, Porreco RP. Trial of labor following cesarean section: a two-year experience. Am J Obstet Gynecol 1982;144: 671-8. [DOI] [PubMed] [Google Scholar]
- 21.Paul RH, Phelan JP, Yeh SY. Trial of labor in the patient with a prior cesarean birth. Am J Obstet Gynecol 1985;151: 297-304. [DOI] [PubMed] [Google Scholar]
- 22.Phelan JP, Clark SL, Diaz F, Paul RH. Vaginal birth after cesarean. Am J Obstet Gynecol 1987;157: 1510-5. [DOI] [PubMed] [Google Scholar]
- 23.Stovall TG, Shaver DC, Solomon SK, Anderson GD. Trial of labor in previous cesarean section patients, excluding classical cesarean sections. Obstet Gynecol 1987;70: 713-7. [PubMed] [Google Scholar]
- 24.Blanchette H, Blanchette M, McCabe J, Vincent S. Is vaginal birth after cesarean safe? Experience at a community hospital. Am J Obstet Gynecol 2001;184: 1478-87. [DOI] [PubMed] [Google Scholar]
- 25.Flamm BL, Goings JR, Fuelberth NJ, Fischermann E, Jones C, Hersh E. Oxytocin during labor after previous cesarean section: results of a multicenter study. Obstet Gynecol 1987;70: 709-12. [PubMed] [Google Scholar]
- 26.Flamm BL, Anton D, Goings JR, Newman J. Prostaglandin E2 for cervical ripening: a multicenter study of patients with prior cesarean delivery. Am J Perinatol 1997;14: 157-60. [DOI] [PubMed] [Google Scholar]
- 27.Blanco JD, Collins M, Willis D, Prien S. Prostaglandin E2 gel induction of patients with a prior low transverse cesarean section. Am J Perinatol 1992;9: 80-3. [DOI] [PubMed] [Google Scholar]
- 28.Connolly GA, Razak ARA, Conroy R, Harrison RFH, McKenna PF. A five year review of scar dehiscence in the Rotunda Hospital Dublin. Irish Med J 2001;94: 176-8. [PubMed] [Google Scholar]
- 29.Leung AS, Farmer RM, Leung EK, Medearis AL, Paul RH. Risk factors associated with uterine rupture during trial of labor after cesarean delivery: a case-control study. Am J Obstet Gynecol 1993;168: 1358-63. [DOI] [PubMed] [Google Scholar]
- 30.Leung AS, Leung EK, Paul RH. Uterine rupture after previous cesarean delivery: maternal and fetal consequences. Am J Obstet Gynecol 1993;169: 945-50. [DOI] [PubMed] [Google Scholar]
- 31.Bujold E, Gauthier RJ. Neonatal morbidity associated with uterine rupture: what are the risk factors? Am J Obstet Gynecol 2002;186: 311-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.