Abstract
Background:
Varicose veins are extremely common disease which is due to elevated superficial venous pressures. We aimed to know that if joint hypermobility causes the venous insufficiency following the prolonged standing.
Materials and Methods:
This prospective cohort study conducted on the soldiers of training periods in a military base of Iran Army in Isfahan in 2013. The active-duty soldiers were first examined by a physician and their Beighton scores (BSs) were obtained. At the onset of the training period, the presence of chronic venous insufficiency was clinically evaluated according to the C class of clinical, etiological, anatomical, and pathological classification. After 3 months, soldiers with and without joint hypermobility were reexamined for manifestations of venous insufficiency based on clinical examination.
Results:
Of 718 soldiers, 211 subjects were diagnosed for joint hypermobility syndrome (29.3%). The mean BS was significantly higher in hypermobility soldiers (5.5 ± 1.5) than the healthy ones (1.2 ± 1.1). Before the training period, the prevalence of spider and varicose veins in soldiers with joint hypermobility was significantly higher than healthy subjects (P > 0.001). After the training period, the prevalence of venous insufficiency significantly increased in soldiers with joint hypermobility (P > 0.001) while there was no significant difference in healthy group before and after the period of training (P = 0.25).
Conclusion:
Hypermobility could be considered as a risk factor for the development of venous insufficiency, so it seems necessary to evaluate the population who need to be standing for a long time for evidence of joint hypermobility.
Keywords: Joint hypermobility, prolonged standing, venous insufficiency
INTRODUCTION
Varicose veins and telangiectasia (spider veins) are the visible surface manifestations of an underlying problem with reverse venous flow, which is also termed venous insufficiency syndrome. Venous insufficiency syndromes describe venous blood deviating from a normal flow path and flow in a retrograde direction so that fluid accumulates, causing a “congested” leg.[1,2] The incidence and prevalence of venous insufficiency disease are depended on the age and sex of the population. Varicosities were observed in 72% of women aged 60–69 years but in only 1% of men aged 20–29 years.[3,4] In United State, one branch of the Framingham study found that the annual incidence was 2.6% in women and 2.0% in men.[5] Prevalence studies are rare and the range reported is wide (2–56% in men and 1–60% in women) due to variations of study population, selection criteria, methods of measurement and disease definition.[6] One Finnish study reported an incidence rate of 13.5/1000 person-years (8.5 for men and 19.2 for women).[7]
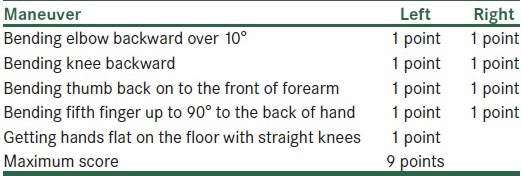
Intrinsic pathological conditions and extrinsic environmental factors combine to produce a wide spectrum of varicose disease. Most varicose disease is due to elevated superficial venous pressures, but some people have an inborn weakness of vein walls and can develop varicosities even in the absence of elevated venous pressures. Some patients with varicose veins of legs also have abnormally distensible veins in the forearm and hand veins.[8] Heredity is important in determining susceptibility to primary valvular failure, but the specific genetic factors responsible for varicosities have not yet been elucidated.[9] Prolonged standing leads to increased hydrostatic pressures that can cause chronic venous distention and secondary valvular incompetence anywhere within the superficial venous system. People with joint hypermobility syndrome (JHS), typically known with excessive joint range of motion based on Beighton criteria, have several related disorders such as low blood pressure, lightheadedness on standing, migraine headaches, and hemorrhoids.[10] JHS is more prevalent in adolescents with a wide range of frequency of 11.2–64.6% and formally diagnosed by using the Beighton scoring system consists of quintuplet examinations shown in Table 1.[11] Although there is no consensus on the minimum score needed to make a diagnosis for JHS, most researchers use a score of 4 out of 9.[12,13] There are many studies on the incidence of venous insufficiency in normal population and also about its risk factors but as we know there are no studies about the incidence of venous insufficiency in hypermobility patients especially after a period of prolonged standing. The aim of this study was to evaluate the role of hypermobility syndrome as a risk factor for venous insufficiency in persons who stand for long time. For this propose, we have chosen the duty soldiers as target population because of long-standing time in the training period.
Table 1.
Beighton criteria for diagnosis of joint hypermobility
MATERIALS AND METHODS
The present study is a prospective cohort study conducted on the soldiers of training periods in a military base of Iran Army in Isfahan during 12 months from April 2013 to April 2014. Inclusion criteria were: Soldiers of training period with standing time for at least 12 h a day who were deployed to the military service during 2013 and not affected by any rheumatologic and connective tissue disorders leading to joint laxity with participant consent. Exclusion criteria were the presence of any mental or physical disorders or any history of drug dependency causing joint weakness or severe disability that would have disrupted the examination. This study was approved in the Ethics Committee of AJA University of Medical Sciences and after being justified on the study objectives, soldiers were consciously entered in the study. Initially, individuals eligible for including to study distinguished by the history taking, specific neurologic and rheumatologic examinations and reviewing the documents of previous diseases of each soldier by a physician. Then soldiers were examined for the 5 tests of JHS by the physician and their Beighton scores (BSs) were obtained. Based on giving minimum score of 4, the enrolled soldiers were divided into two groups: Who have hypermobile joints and healthy soldiers.
At the beginning of the training period, the presence of chronic venous insufficiency (CVI) was clinically evaluated according to the C class of clinical, etiological, anatomical, and pathological classification. Based on this classification, participants classified into six categories; normal subjects with no visible or palpable signs of venous disease (C0), telangiectasies or reticular veins (C1), varicose veins (C2), edema (C3), pigmentation and eczema (C4a), lipodermatosclerosis and atrophie blanche (C4b), healed venous ulcer (C5), active venous ulcer (C6).[18] Subjects in class C0 considered as normal and those with class C1 or higher named as a group with venous insufficiency. Then, after passing 3 months of training, soldiers of two groups of with and without joint hypermobility were reexamined in terms of the new occurrence of manifestations of venous insufficiency based on clinical manifestations [Figure 1].
Figure 1.

Examples of telangiectasia and varicose veins in soldiers with joint hypermobility after passing 3-month course of military training
The collected data were analyzed in SPSS software for windows version 20.0. The obtained results from analyzing variables have been reported as mean ± standard deviation and frequency (percentage) based on the type of variables. To compare the mean age and BS in individuals having JHS with the healthy subjects and the frequency of venous insufficiency manifestations, independent-T and Chi-square and Mc-Nemar tests were applied, respectively. In all cases, the level of significance has been considered as <0.05.
RESULTS
Among 721 studied soldiers, 3 cases were excluded; because of exemption and discharge from service before completing the training period. Of 718 soldiers, 211 subjects were diagnosed for JHS based on achieving the minimum score of 4 from Beighton criteria (29.3%).
There was no significant difference in case of the mean age between Benign JHS and healthy soldiers, 19.58 ± 1.53 in suffered versus 19.64 ± 1.86 in a healthy group (P = 0.69). The mean BS was significantly higher (P > 0.001) in hypermobility soldiers (5.5 ± 1.5) than the healthy ones (1.2 ± 1.1).
Before training period, 74 and finally after training 89 soldiers, (all in class C1) diagnosed as venous insufficient cases (15 new cases). Higher classes were not found in studied soldiers. Before the training period, the prevalence of spider and varicose veins in soldiers with joint hypermobility was significantly higher than healthy subjects (P > 0.001) [Figure 2].
Figure 2.
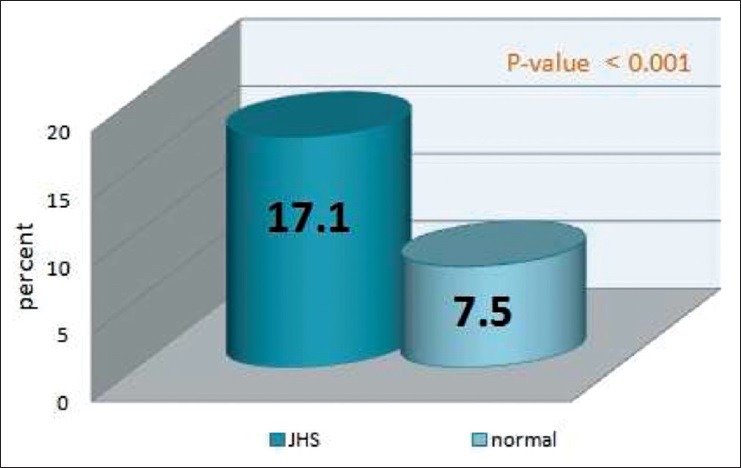
Comparison of the prevalence of abnormal visible tortuous veins of lower limb predisposing varicose veins in suffered and healthy soldiers before military training (JHS: Joint hypermobility syndrome, P values calculated by Chi-square test)
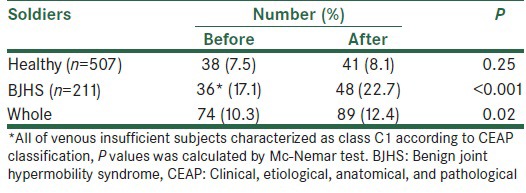
The prevalence of venous insufficiency syndrome in each group of JHS and healthy soldiers before beginning and after the end of the training period are shown in Table 2. As it shown, in the JHS group, the prevalence of venous insufficiency after the training period was significantly higher than before (P > 0.001) while there was no significant difference in healthy group before and after the period (P = 0.25).
Table 2.
Comparison of the prevalence of venous insufficiency syndrome before and after military training
When we compared the incidence of varicose veins based on BS of 5 and 6, the incidences of spider and varicose veins in suffered group were more significantly increased (P < 0.001). The differences became more obvious in higher BSs [Figure 3].
Figure 3.
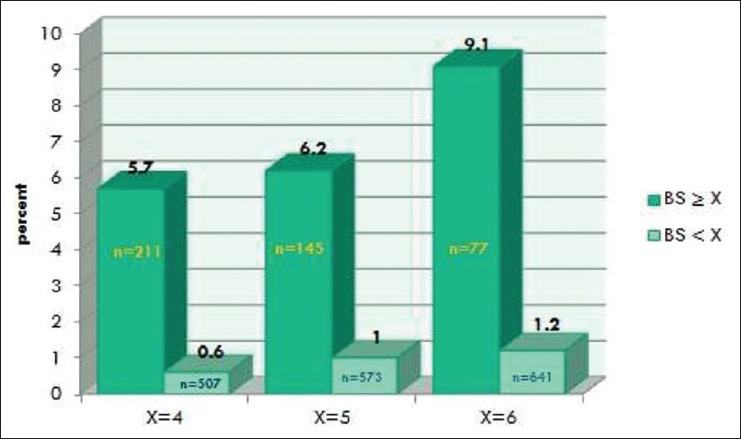
Comparison of the incidence of venous insufficiency during training period in two groups of soldiers based on BS limit of 4, 5 and 6 (BS: Beighton score, n: Number of subjects, P values calculated by Chi-square test)
DISCUSSION
Varicose veins have a significant impact on healthcare resources, and in this study, we aimed to evaluate the effect of prolonged standing on venous insufficiency incidence in hypermobility patients. Based on numerous studies on CVI, the main risk factors found to be associated with CVI include age, sex, and positive family history of varicose veins, obesity, pregnancy, phlebitis, and previous leg injury. There are also environmental or behavioral factors may be associated with CVI such as long-standing time and perhaps a special sitting posture at work.[2] Moreover, diseases like hypermobility showed variable associations with venous disease.[3] Based on several studies, patients with joint hypermobility are at a higher risk of connective tissue disorders such as varicose veins, hernia, or uterine or rectal prolapses.[3,5,9,10,12,13] In one study in Iranian adolescents, a significant relationship found between joint hypermobility and recurrent dislocations of temporomandibular, shoulder and ankle joints indicating the role of connective tissues defects in both.[11] There are many studies about the effect of long-standing effect on venous insufficiency and it has been approved as a strong risk factor for this disease but in our study, the possible effect of another risk factor means joint hypermobility has been evaluated in people who were obliged to standing for a long time in day. According to our knowledge, there is no study which has been investigated the hypermobility as a factor increasing the risk of venous insufficiency in long-standing people. As the joint hypermobility patients suffer from the weakness of supporting tissue structures [2,3] and, on the other hand, the weakness of venous walls connective tissues has role in varicose physiopathology; [14] it may suppose that joint hypermobility predisposed to the venous insufficiency following the prolonged standing.
In women, increased time standing was positively associated with more severe disease and increased sitting time inversely associated with moderate disease. For men, increased daily walking was associated with moderate disease, and men who worked as laborers were more likely to have severe disease than those in positions which typically require more desk time. Regular movement when sitting for long periods was related to lower rates of moderate disease in men.[10] Fowkes et al. similarly found that sitting was associated with lower rates of venous insufficiency for women and not for men.[19] They also found that walking was a risk factor for women with venous insufficiency when age-adjusted, but less so when multiply adjusted. They found walking to be related to lessened risk of venous insufficiency in men. Our data indicate that standing was a strong risk factor for venous insufficiency. This is concordant with a number of studies.[15,16,17,18,19] In a representative cross-section study on hospital employees in a university hospital, the prevalence of cardiovascular disease (CVD) was highest in women, especially in those working in a standing position or under conditions of high temperature and humidity. The results warrant regular evaluation of standing for a long-time risk factor with subsequent primary prophylaxis of CVD.[20]
The main limitation of our study was the duration of follow-up. Although participants were followed up for 3 months, many of signs and symptoms of venous insufficiency may gradually progress in a long time. Therefore, it is recommended for future studies to consider a longer time of follow-up.
CONCLUSION
Joint hypermobility, as a presentation for generalized connective tissue disorder, can be considered as a risk factor for venous insufficiency. In addition, standing for a long time has been found as a risk factor for the development of varicose veins among patients with joint hypermobility. It seems necessary to evaluate the population who need to be standing for a long time at work in order to detect hypermobility and manifestation of venous insufficiency syndrome.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Khan AF, Chaudhri R, Ashraf MA, Mazaffar MS, Zawar-ul-Imam S, Tanveer M. Prevalence and presentation of chronic venous disease in Pakistan: A multicentre study. Phlebology. 2013;28:74–9. doi: 10.1258/phleb.2012.011122. [DOI] [PubMed] [Google Scholar]
- 2.Carpentier PH, Maricq HR, Biro C, Ponçot-Makinen CO, Franco A. Prevalence, risk factors, and clinical patterns of chronic venous disorders of lower limbs: A population-based study in France. J Vasc Surg. 2004;40:650–9. doi: 10.1016/j.jvs.2004.07.025. [DOI] [PubMed] [Google Scholar]
- 3.Vlajinac HD, Radak DJ, Marinkovic JM, Maksimovic MZ. Risk factors for chronic venous disease. Phlebology. 2012;27:416–22. doi: 10.1258/phleb.2011.011091. [DOI] [PubMed] [Google Scholar]
- 4.Zahariev T, Anastassov V, Girov K, Goranova E, Grozdinski L, Kniajev V, et al. Prevalence of primary chronic venous disease: The Bulgarian experience. Int Angiol. 2009;28:303–10. [PubMed] [Google Scholar]
- 5.Brand FN, Dannenberg AL, Abbott RD, Kannel WB. The epidemiology of varicose veins: The Framingham Study. Am J Prev Med. 1988;4:96–101. [PubMed] [Google Scholar]
- 6.Kuhlmann A, Prenzler A, Hacker J, Graf von der Schulenburg JM. Impact of radiofrequency ablation for patients with varicose veins on the budget of the German statutory health insurance system. Health Econ Rev. 2013;3:9. doi: 10.1186/2191-1991-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mäkivaara LA, Jukkola TM, Sisto T, Luukkaala T, Hakama M, Laurikka JO. Incidence of varicose veins in Finland. Vasa. 2004;33:159–63. doi: 10.1024/0301-1526.33.3.159. [DOI] [PubMed] [Google Scholar]
- 8.Evans CJ, Fowkes FG, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. J Epidemiol Community Health. 1999;53:149–53. doi: 10.1136/jech.53.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anwar MA, Georgiadis KA, Shalhoub J, Lim CS, Gohel MS, Davies AH. A review of familial, genetic, and congenital aspects of primary varicose vein disease. Circ Cardiovasc Genet. 2012;5:460–6. doi: 10.1161/CIRCGENETICS.112.963439. [DOI] [PubMed] [Google Scholar]
- 10.Criqui MH, Denenberg JO, Bergan J, Langer RD, Fronek A. Risk factors for chronic venous disease: The San Diego Population Study. J Vasc Surg. 2007;46:331–7. doi: 10.1016/j.jvs.2007.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azma K, Mottaghi P, Hosseini A, Abadi HH, Nouraei MH. Benign joint hypermobility syndrome in soldiers; what is the effect of military training courses on associated joint instabilities? J Res Med Sci. 2014;19:639–43. [PMC free article] [PubMed] [Google Scholar]
- 12.Nazem M, Mottaghi P, Hoseini A, Khodadadi HA. Benign joint hypermobility syndrome among children with inguinal hernia. J Res Med Sci. 2013;18:904–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Knight I, Bird HA. Joint hypermobility syndrome. BMJ. 2010;341:c3044. doi: 10.1136/bmj.c3044. [DOI] [PubMed] [Google Scholar]
- 14.Rabe E, Pannier F. Clinical, aetiological, anatomical and pathological classification (CEAP): Gold standard and limits. Phlebology. 2012;27(Suppl 1):114–8. doi: 10.1258/phleb.2012.012s19. [DOI] [PubMed] [Google Scholar]
- 15.Criqui MH, Jamosmos M, Fronek A, Denenberg JO, Langer RD, Bergan J, et al. Chronic venous disease in an ethnically diverse population: The San Diego Population Study. Am J Epidemiol. 2003;158:448–56. doi: 10.1093/aje/kwg166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiesa R, Marone EM, Limoni C, Volonté M, Schaefer E, Petrini O. Effect of chronic venous insufficiency on activities of daily living and quality of life: Correlation of demographic factors with duplex ultrasonography findings. Angiology. 2007;58:440–9. doi: 10.1177/0003319706292012. [DOI] [PubMed] [Google Scholar]
- 17.Ruckley CV, Evans CJ, Allan PL, Lee AJ, Fowkes FG. Chronic venous insufficiency: Clinical and duplex correlations. The Edinburgh Vein Study of venous disorders in the general population. J Vasc Surg. 2002;36:520–5. doi: 10.1067/mva.2002.126547. [DOI] [PubMed] [Google Scholar]
- 18.Jawien A. The influence of environmental factors in chronic venous insufficiency. Angiology. 2003;54(Suppl 1):S19–31. doi: 10.1177/0003319703054001S04. [DOI] [PubMed] [Google Scholar]
- 19.Fowkes FG, Lee AJ, Evans CJ, Allan PL, Bradbury AW, Ruckley CV. Lifestyle risk factors for lower limb venous reflux in the general population: Edinburgh Vein Study. Int J Epidemiol. 2001;30:846–52. doi: 10.1093/ije/30.4.846. [DOI] [PubMed] [Google Scholar]
- 20.Ziegler S, Eckhardt G, Stöger R, Machula J, Rüdiger HW. High prevalence of chronic venous disease in hospital employees. Wien Klin Wochenschr. 2003;115:575–9. doi: 10.1007/BF03040451. [DOI] [PubMed] [Google Scholar]


