Abstract
Background:
This study aims to evaluate the impact of the Isfahan Healthy Heart Program (IHHP) interventions concerning healthy behavior, on the prevalence of the metabolic syndrome (MetS) and its components in the Iranian population.
Materials and Methods:
The IHHP targeted the population at large in three districts in central Iran from 2000 to 2007. Numerous interventional activities were performed to improve lifestyle. The main intervention strategies were public education through mass media, intersectional cooperation, health professional education, marketing and organizational development, legislation and policy development, as well as research and evaluation. MetS was defined based on the Adult Treatment Panel (ATP) III definition. The logistic regression method was applied to explore the relationship between lifestyle factors with components of metabolic risk factors.
Results:
The mean age of the participants was 44.68 ± 14.43 years in 2001. The mean values of the MetS components differed from 2001 to 2007. The mean of systolic blood pressure (SBP) decreased from 126.7 ± 22.31 to 124.21 ± 20.0 and from 129.47 ± 23.08 to 126.26 ± 21.88 among females in both the intervention and reference areas. Similar changes were observed among males. The mean diastolic blood pressure (DBP) and triglycerides decreased significantly in the intervention area and increased significantly in the reference area in both sexes. High density protein cholesterol (HDL-C) was decreased in both sexes, from 2001 to 2007, in both areas. A strong relationship between tobacco control with high SBP and hypertriglyceridemia was found (P < 0.01).
Conclusion:
Lifestyle improvement programs could be useful to improve the MetS status among men and women.
Keywords: Iranian adults, lifestyle modification, metabolic syndrome
INTRODUCTION
Epidemiological studies confirmed a high prevalence of cardiovascular disease (CVD) and metabolic syndrome (MetS) among the Iranian population.[1,2] In the last decade there was an increase in the prevalence of obesity, hypertension, and other risk factors in this population.[3] This epidemic should be controlled to prevent further morbidity and mortality owing to diabetes and CVD.[4,5] Previous studies reported that individuals with MetS might benefit from extensive lifestyle modification.[6]
Although pharmacological therapy is a critical step in the management of patients with MetS, lifestyle modifications are the first step to achieve these goals.[7,8] Lifestyle modification is a multifactorial process and consists of changes in behavioral factors such as diet and physical activity, weight reduction, and tobacco control.[8] Several intervention trials have reported the effects of lifestyle intervention programs among high-risk populations.[9] However, the pooled effects suggest that multiple risk factor interventions have no effect on mortality. In spite of the recent meta-analyses there is doubt on whether lifestyle interventions actually assist the primary prevention of CVD.[10] However, the Isfahan Healthy Heart Program (IHHP), a comprehensive community-based intervention program that was designed to improve behavior lifestyles and control CVD and its risk factors has shown positive results.[11,12,13,14,15] This study aimed to evaluate the impact of IHHP interventions concerning healthy behaviors on the prevalence of MetS and its components in the Iranian population.
MATERIALS AND METHODS
Two cross-sectional surveys were conducted in three counties (Arak, Isfahan, and Najafabad) in the central part of Iran, as baseline (2001) and post-intervention (2007) phases of the IHHP, to assess its effects. The IHHP design and interventions have been previously reported in detail.[11,12] Multistage random sampling was used to select participants aged ≥19 years in the three counties. The intervention phase was then implemented in Isfahan and Najafabad, with populations of 1.895.856 and 275,084, respectively. Arak, with a population of 668,531, was considered as the reference area. The IHHP's primary prevention activities were healthy nutrition, increased physical activity, tobacco control, and coping with stress.[12,13] The secondary prevention activities were performed on CVD patients and their families as well as patients with diabetes, hypertension, and MetS. The main intervention strategies were public education through mass media, intersectoral cooperation, health professional education, marketing and organizational development, legislation and policy development, as well as research and evaluation.[12] Data on the demographics and lifestyle behaviors, including their nutritional habits, smoking, physical activity, and coping with stress were collected by trained interviewers and questionnaires were administered to each participant in the intervention and reference areas, in 2001 and 2007. Additional questions on medical history and medication use were completed. Written informed consent was obtained from the subjects after a full explanation of the whole study. The study was approved by the Ethics Committee of the Isfahan University of Medical Sciences.
Weight and height were measured with calibrated instruments, under the standard protocol. Waist circumference (WC) and hip circumference were measured and recorded in centimeters, using the standard methods.[11] Blood pressure (BP) was measured twice from the right hand.[11]
Fasting (>12 hours) venous blood samples were collected from all the participants. Standard laboratory kits (Pars Azmoun Co., Tehran, Iran) and the enzymatic method were used to measure serum total cholesterol (TC), triglycerides (TG), HDL-C, and fasting blood glucose (FBG). A two-hour post-load plasma glucose level (2-hpp) was done for non-diabetic participants. All blood samples in both the 2001 and 2007 surveys were frozen at -20°C until assayed within 72 hours in the central laboratory of the Isfahan Cardiovascular Research Institute, with adherence to external national and international quality control. The global dietary index (GDI) was calculated representing the general dietary behavior. In addition, two consumption indices were calculated for specific food groups, that is, meat products and major sources of fat.[14] The usual dietary intake was assessed using a 49-item food frequency questionnaire (FFQ), listing foods commonly consumed by Iranians, and administered by trained technicians. For each food item, the participants were asked to report common portion sizes and consumption frequency during the previous year. The latter was recorded in terms of daily (e.g., bread), weekly (e.g., rice, meat) and monthly (e.g., fish) consumption, and the daily intake of each food was derived by dividing the weekly consumption by seven and the monthly consumption by 30.
Data on physical activity, expressed as metabolic equivalent task (METS) in minutes per week, were obtained through an oral questionnaire. Several questions on smoking behaviors and the frequency of smoking in a day, week or month were asked.[13] Smoking was defined as current smoking for those who smoked at least one cigarette per day and non-smokers were ones who did not actually smoke, but had a history of previous regular tobacco use.[13]
Metabolic syndrome definition
The updated ATP-III definition of MetS was met when three or more of the following criteria were present: Waist circumference ≥102 cm in men and 88 cm in women; HDL >40 mg/dl in men and, 50 mg/dl in women or specific treatment for this lipid abnormality; triglycerides ≥150 mg/dl in men and women or specific treatment for this lipid abnormality; systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥85 mmHg in men and women or treatment of previously diagnosed hypertension; and fasting glucose ≥100 mg/dl in men and women.[16]
Statistical analysis
All data were analyzed by SPSS (SPSS Inc, Chicago, IL, USA; Version 15). The averages are reported as Mean ± SD. For all analyses, statistical significance was assessed at a level of 0.05. The two-tailed t-test was used as appropriate to compare the mean ± SD of continuous variables in 2001 and 2007 and in the reference and intervention areas. The logistic regression method was applied to explore the relationship between lifestyle factors and components of metabolic risk factors.
RESULTS
The baseline sample included 15,705 participants (55.8% male) in the intervention area, and 1245 (40.2% male) in the reference area. In 2007, the sample included 1955 (54.6% male) in the intervention area and 973 (45.4% male) in the reference area. The mean age of the participants was significantly different across years (44.68 ± 14.43 years in 2001 vs. 49.106 ± 0.34 years in 2007).
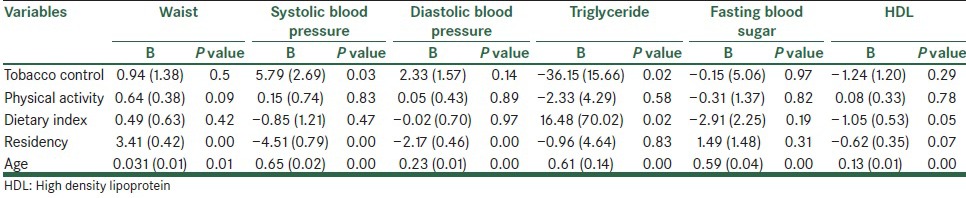
The mean values of the MetS components in 2001 and 2007 are presented in Table 1. The mean of WC declined significantly from 103.8 ± 10.48 to 100.23 ± 9.83 among females in the intervention area, whereas, it increased from 99.32 ± 10.48 to 100.82 ± 10.54 among females in the reference area. The mean of SBP decreased from 126.7 ± 22.31 to 124.21 ± 20.0 and from 129.47 ± 23.08 to 126.26 ± 21.88 among females in both the intervention and reference areas. Similar changes were observed among males. However, the mean of DBP and triglycerides decreased significantly in the intervention area and increased significantly in the reference area in both sexes. HDL-C was decreased in both sexes from 2001 to 2007 in the intervention and reference areas. Table 2 shows the correlation between the lifestyle factors and components of MetS in females. In this group, we found a strong relationship between tobacco control, with high SBP and hypertriglyceridemia (P < 0.01). In addition, having adequate physical activity has a significant relationship with abdominal obesity and hypertriglyceridemia (P < 0.05), even as, the dietary index has a significant correlation with hypertriglyceridemia and low HDL-C (P = 0.05). Age has a significant correlation with all MetS components, whereas, residency follows the same pattern except in relation to hypertriglyceridemia and elevated fasting blood sugar (P < 0.0001).
Table 1.
Characteristics of the studied population in both the intervention and reference areas from 2001 to 2007
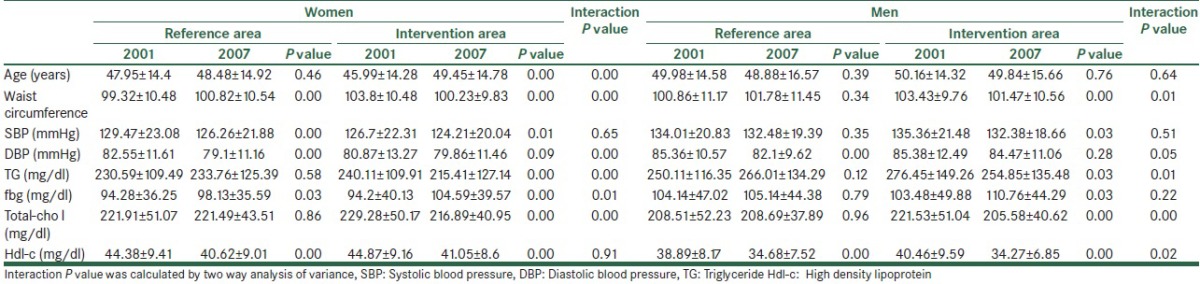
Table 2.
Relationship between lifestyle factors and components of metabolic risk factors in females in both intervention and reference areas from 2001 to 2007
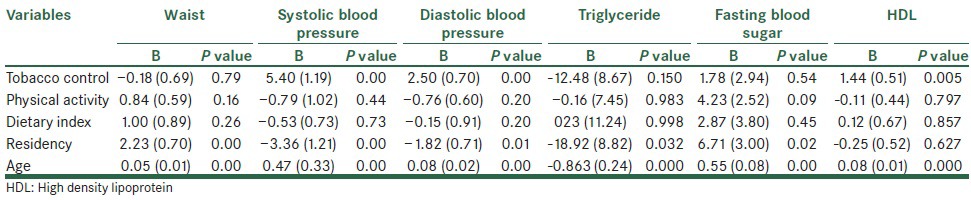
In males, there was a significant relationship between tobacco control and elevated systolic and diastolic blood pressures and also low HDL-C. Physical activity had a significant relationship with elevated fasting blood glucose (P < 0.01). The dietary index had a non-significant relationship with the MetS components among the subjects of our study. Residency had a significant relationship with all MetS components except low HDL-C (P < 0.01). We have seen a significant relationship between age and all the considered risk factors [Table 3].
Table 3.
Relationship between lifestyle factors and components of metabolic risk factors in male in both intervention and reference area from 2001 to 2007
DISCUSSION
The results of this study showed that the community-based lifestyle intervention program could improve lifestyle habits. We found a strong association between tobacco control, being physically active, and healthy nutrition on some components of MetS, especially in women. In this study, the prevalence of MetS and its components was significantly reduced after lifestyle modification during the six-year follow up. Similar improvements have been achieved throughout by quitting tobacco; and having enough physical activity and a healthy diet could improve the metabolic parameters.
Comprehensive lifestyle intervention programs have generally focused on changing high-risk behaviors by persuading at-risk people to quit smoking, have a lower fat intake, and be more physically active. Adopting healthy lifestyle behaviors in middle age can result in lower cardiovascular disease (CVD) and mortality.[17] However, the modern lifestyle modification therapy combines specific recommendations on diet and exercise with behavioral and cognitive strategies. It is suggested to consider weight loss as a core of treating MetS and its components.[18] Thus, developing ethnically relevant interventions that are successful in helping people with MetS are needed to reduce long-term negative outcomes. After IHHP interventions, the items on Mets were improved, even when the abdominal circumference was greater than the normal value in women, which was similar with another study among the Japanese population.[19] Lifestyle changes are important in the treatment of obesity, although, they are usually unlikely to provide a permanent effect. The main challenge of treatment is helping patients maintain healthy behavior changes in the long term[20]. New strategies demonstrated the effectiveness of goal setting for nutrition and physical activity behavior changes in combination with pharmacotherapy in subject with MetS.[21] In-line with our study, Moran et al., did not find any relationship between lifestyle intervention on improving glucose tolerance or lipid profiles.[22]
Ilanne-Parikka and colleagues assessed the effects of leisure time physical activity and resistance training on MetS and its components in a Finnish population.[23] They found increased moderate-to-vigorous leisure time physical activity was associated with a decreased probability of developing MetS and an increased likelihood of its resolution in individuals at high-risk for type 2 diabetes.[23] Similarly, our results showed that being physically active had an inverse association with some risk factors such as abdominal obesity and hypertriglyceridemia (P < 0.05).
Kirkendoll and his co-workers claimed that generally MetS subjects were unfamiliar with Mets as a diagnosis. Most were uninformed of the term and had not been told by their doctors that their combination of health problems was referred to as ‘MetS’. Based on their individual risk factors, participants should be aware of the need to change lifestyle behaviors to improve their health. In addition, they should have sufficient knowledge of the appropriate behaviors in which they should be engaged. However, they expressed skill building to successfully change behaviors.[24,25]
Limitation
Several limitations must be considered in this study. The type of intervention may have been one of our limitations. Although community-based intervention is accepted for intervention, direct intervention may have been more consequential. Moreover, there may be some confounders that affect our results. In future studies the possible confounders must be considered. In spite of these drawbacks, the main strength of this study is a large population-based sample that has been followed for six years, which is very significant.
CONCLUSION
In conclusion, lifestyle improvement programs could be useful to improve the MetS status among men and women. Physical activity, healthy diet, and quitting smoking, more specifically, had benefits with respect to hyperglycemia and dyslipidemia.
ACKNOWLEDGMENT
The Isfahan Healthy Heart Program is supported by a Grant (No. 31309304) from the Iranian budget and programming organization, the Deputy of Health, of the Ministry of Health and Medical Education in the Islamic Republic of IRAN, Isfahan Cardiovascular Research Center, and Isfahan Provincial Health Center, both affiliated to the Isfahan University of Medical Sciences. It is indexed as code No. 86 in the Canadian Heart Health Promotion Projects: www.med.mun.com
Footnotes
Source of Support: The Isfahan Healthy Heart Program is supported by a Grant (No. 31309304) from the Iranian budget and programming organization, the Deputy of Health, of the Ministry of Health and Medical Education in the Islamic Republic of IRAN, Isfahan Cardiovascular Research Center, and Isfahan Provincial Health Center, both affiliated to the Isfahan University of Medical Sciences. It is indexed as code No. 86 in the Canadian Heart Health Promotion Projects: www.med.mun.com
Conflict of Interest: None declared.
REFERENCES
- 1.Sarrafzadegan N, Sayed-Tabatabaei FA, Bashardoost N, Maleki A, Totonchi M, Habibi HR, et al. The prevalence of coronary artery disease in an urban population in Isfahan, Iran. Acta Cardiol. 1999;54:257–63. [PubMed] [Google Scholar]
- 2.Gharipour M, Sarrafzadegan N, Sadeghi M, Andalib E, Talaie M, Shafie D, et al. Predictors of metabolic syndrome in the Iranian population: waist circumference, body mass index, or waist to hip ratio? Cholesterol 2013. 2013 doi: 10.1155/2013/198384. 198384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tavassoli AA, Gharipour M, Khosravi A, Kelishadi R, Siadat ZD, Bahonar A, et al. Gender differences in obesogenic behaviour, socioeconomic and metabolic factors in a population-based sample of Iranians: The IHHP Study. J Health Popul Nutr. 2010;28:602–9. doi: 10.3329/jhpn.v28i6.6609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gharipour M, Sarrafzadegan N, Sadeghi M, Andalib E, Talaie M, et al. Predictors of metabolic syndrome in the Iranian population: waist circumference, body mass index, or waist to hip ratio? Cholesterol 2013. 2013 doi: 10.1155/2013/198384. 198384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giri M. Medical management of obesity. Acta Clin Belg. 2006;61:286–94. doi: 10.1179/acb.2006.048. [DOI] [PubMed] [Google Scholar]
- 6.Panagiotakos DB, Pitsavos C, Chrysohoou C, Skoumas J, Tousoulis D, Toutouza M, et al. Impact of lifestyle habits on the prevalence of the metabolic syndrome among Greek adults from the ATTICA study. Am Heart J. 2004;147:106–12. doi: 10.1016/s0002-8703(03)00442-3. [DOI] [PubMed] [Google Scholar]
- 7.Gharipour M, Kelishadi R, Khosravi A, Shirani S, Masjedi M, Sarrafzadegan N. The impact of a community trial on the pharmacological treatment in the individuals with the metabolic syndrome: Findings from the Isfahan Healthy Heart Program, 2001-2007. Arch Med Sci. 2012;8:1009–17. doi: 10.5114/aoms.2012.32407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iseki K. Metabolic syndrome and chronic kidney disease: A Japanese perspective on a worldwide problem. J Nephrol. 2008;21:305–12. [PubMed] [Google Scholar]
- 9.Baghaei A, Sarrafzadegan N, Rabiei K. How effective are strategies for non-communicable disease prevention and control on high risk population in a developing country Isfahan Healthy Program. Arch Med Sci. 2010;6:24–31. doi: 10.5114/aoms.2010.13503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ebrahim S, Beswick A, Burke M, Davey SG. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst Rev. 2006;4:CD001561. doi: 10.1002/14651858.CD001561.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarrafzadegan N, Sadri GH, Malek Afzali H, Baghaei M, Mohammadi Fard N, Shahrokhi S, et al. Isfahan Healthy Heart Programme: A comprehensive integrated community-based programme for cardiovascular disease prevention and control. Design, methods and initial experience. Acta Cardiol. 2003;58:309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 12.Sarrafzadegan N, Baghaei AM, Sadri GH, Kelishadi R, Malekafzali H, Boshtam M. Isfahan Healthy Heart Program: Evaluation of comprehensive, community-based interventions for non-communicable disease. Prev Control J. 2006;2:73–84. [Google Scholar]
- 13.Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, Mohammadifard N, Rabiei K, Roohafza H, et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bull World Health Organ. 2009;87:39–50. doi: 10.2471/BLT.07.049841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohammadifard N, Kelishadi R, Safavi M, Sarrafzadegan N, Sajadi F, Sadri GH. Effect of a community-based intervention on nutritional behavior in a developing country setting: The Isfahan Healthy Program. Public Health Nutr. 2009;17:1–9. doi: 10.1017/S1368980008004230. [DOI] [PubMed] [Google Scholar]
- 15.Sarrafzadegan N, Azadbakht L, Mohammadifard N, Esmaillzadeh A, Safavi M, Sajadi F, et al. Do lifestyle interventions affect dietary diversity score in the general population? Public Health Nutr. 2009;12:1924–30. doi: 10.1017/S1368980009004856. [DOI] [PubMed] [Google Scholar]
- 16.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 17.Liu K, Daviglus ML, Loria CM, Colangelo LA, Spring B, Moller AC, et al. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: The Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation. 2012;125:996–1004. doi: 10.1161/CIRCULATIONAHA.111.060681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cornier MA, Dabelea D, Hernandez TL, Lindstrom RC, Steig AJ, Stob NR, et al. The metabolic syndrome. Endocr Rev. 2008;29:777–822. doi: 10.1210/er.2008-0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miyatake N, Fujii M, Miyachi M, Tabata I, Takeshi S, Hirao T, et al. Changes in metabolic syndrome and its components with lifestyle modification in Japanese men. Intern Med. 2010;49:261–5. doi: 10.2169/internalmedicine.49.2900. [DOI] [PubMed] [Google Scholar]
- 20.Wagh A, Stone NJ. Treatment of metabolic syndrome. Expert Rev Cardiovasc Ther. 2004;2:213–28. doi: 10.1586/14779072.2.2.213. [DOI] [PubMed] [Google Scholar]
- 21.TPelikánova T. Treatment of diabetes in metabolic syndrome. Vnitr Lek. 2009;55:637–45. [PubMed] [Google Scholar]
- 22.Moran LJ, Hutchison SK, Norman RJ, Teede HJ. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2011;2:CD007506. doi: 10.1002/14651858.CD007506.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Ilanne-Parikka P, Laaksonen DE, Eriksson JG, Lakka TA, Lindstr J, Peltonen M, et al. Finnish Diabetes Prevention Study Group. Leisure-time physical activity and the metabolic syndrome in the Finnish diabetes prevention study. Diabetes Care. 2010;33:1610–7. doi: 10.2337/dc09-2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kirkendoll K, Clark PC, Grossniklaus D, Igho-Pemu P, Mullis R, Dunbar SB. Metabolic syndrome in African Americans: Views on making lifestyle changes. J Transcult Nurs. 2010;21:104–13. doi: 10.1177/1043659609357636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gulseth HL, Gjelstad IM, Tierney AC, Shaw DI, Helal O, Hees AM, et al. Dietary fat modifications and blood pressure in subjects with the metabolic syndrome in the LIPGENE dietary intervention study. Br J Nutr. 2010;104:160–3. doi: 10.1017/S0007114510000565. [DOI] [PubMed] [Google Scholar]


