Abstract
Background:
The main objective of this study was to determine the incidence, time to event, and risk factors for posttraumatic seizures (PTS) following traumatic brain injury (TBI) in a five-year follow-up survival design.
Materials and Methods:
In a cohort study, between September 2008 and October 2013, 411 traumatic brain injury patients referring to the Emergency Units (EUs) of the Isfahan University Hospitals, who met the inclusion criteria, entered the study. Follow-up evaluations were conducted by telephone conversation or clinical examination, if needed. The patients were followed for up to five years after TBI or until a first seizure event if it occurred prior to the five-year anniversary. The survival rate data were collected and measured for all patients under follow-up. Survival analysis on PTS and its related predictors was done using the Kaplan-Meier curves and the Cox proportional hazards regression. All analyses were done using STATA and SPSS statistical software, and P-values smaller than 0.05 were considered to be statistically significant.
Results:
The median duration of follow-up was 36 months (Interquartile range: 23-50). A significantly greater number of first seizures occurred in the first year after injury than all other years (57.7%). The overall incidence of posttraumatic seizures, in this study population, was 6.33% (95% CI: 3.96-8.69). Among the participants, the incidence rates for early and late posttraumatic seizures were 1.95 and 4.38%, respectively. The result of the Cox regression analysis showed that the Glasgow Coma Scale (GCS) score and trauma severity were associated with PTS.
Conclusion:
All in all, the present study highlighted the role of the trauma severity and GCS as effective factors in the incidence of seizure in patients with TBI. Particular care is advised for patients with these risk factors during the primary handling in the Emergency Units.
Keywords: Cohort design, emergency units, follow-up study, posttraumatic seizures, traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) is a major public health problem, with a generic difficulty in emergency properties, particularly in urban trauma centers.[1,2] On account of its serious complications such as changes affecting thinking, language, sensation or emotions, which may not be easily apparent, and lack of knowledge among the public, it is referred to as the ‘silent epidemic’.[3] Posttraumatic seizures (PTS) are the types of seizures that arise from traumatic brain injury and brain harm due to physical trauma.[4] A seizure is ‘the physical response to abnormal electrical activity in the brain’[5,6] It has been estimated that seizures would occur in 5 to 10% of the cases after an acute stroke.[7] Posttraumatic seizures are commonly derived into three classes: ‘immediate seizures’, ‘early seizures’, and ‘late seizures’. Immediate seizures refer to those that happen at or minutes after impact; seizures that occur one week after head injury are called early seizures, and late posttraumatic seizures are defined as those occurring >1 week after injury.[8,9,10] The proper choice for TBI therapy depends on the specific injuries that the patient has sustained, timely diagnosis, clinical data, and imaging results.[1,11] In a study performed for identifying the specs of brain injuries associated with the development of seizures; it has been shown that the enhanced risk of seizures after TBI generally depends on the severity of the injury and the time since the injury.[12] The age of 65 years or older, a skull fracture, brain contusion with subdural hematoma, and lacking consciousness or more than one day amnesia, have been shown as the major risk factors for later seizures.[12,13,14] The risk factors and the time course of the risk are significant for designing seizure-prophylaxis studies.[15] Different ages have different outcomes in patients with TBI; Asikainen et al expressed that children are more susceptible to early seizures, while juveniles and adults are more prone to late seizures.[16,17] Also, investigation on different genders in outcomes after severe traumatic brain injury revealed that Female TBI patients have better predicted outcomes and most of the TBI patients are males.[18,19] Although many studies have been conducted on TBI, the exact distribution of early and late onset types of seizures among Iran emergencies, remains unclear. The objectives of the present study are to evaluate the exact distribution of the types of early and late onset seizures and factors affecting the occurrence of seizures over time in patients with TBI, who are referred to Emergency Units of the Isfahan University Hospital.
MATERIALS AND METHODS
This cohort study was conducted on 411 traumatic brain injury (TBI) patients referring to the Emergency Units of the Isfahan University Hospitals, between September 2008 and October 2013. The Krejcie and Morgan's table were used to determine the sample size.[20]
The non-probability consecutive sampling method was used. The study protocol was considered and approved by the Ethics Committee of the Vice-Chancellor for Research Affairs of the Isfahan University of Medical Sciences.
The inclusion criteria were:
Age over six years, male or female,
Diagnosis of acute traumatic brain injury, and
Provision of informed consent.
The patients were excluded if they had a previous history of seizures. Other exclusion criteria were:
A preceding history of brain injury or major mental disorder,
Pregnancy,
Death due to head trauma,
Evidence of metabolic disease other than obesity,
Predisposition to seizures (such as a history of brain tumor or stroke), and
Family history of seizure.
In this study, we used the classification of head injury severity as defined by Annegers et al. Mild injuries were those in which no skull fracture was found and the period of posttraumatic amnesia or loss of consciousness was ≤30 minutes. The moderately injured group of patients included those with skull fractures or other injuries with > 30 minutes of posttraumatic amnesia or loss of consciousness, who did not otherwise meet the criteria for a severe injury. Severe injuries were those with a documented brain contusion, an intracerebral hematoma (ICH) or > 24 hours of posttraumatic amnesia or loss of consciousness.[12]
Follow-up evaluations were conducted by recording data (during hospitalization) and telephone conversations or clinical examinations, if needed (after discharging from the hospital). The patients were followed for up to five years.
The endpoint of the study was defined as ‘early and late posttraumatic seizures’ during follow-up. Early seizures were attacks that occurred one week after trauma. Late onset seizure were attacks that occurred more than a week after the trauma. Other predictive variables were age, sex, trauma severity, GCS, onset of PTS, and neuroradiological findings.
Data are presented as Mean ± SD or Median (twenty-fifth and seventy-fifth percentile) for continuous variables and Number (percent) for categorical ones. The Kolmogorov-Smirnov test was performed to check for normal distribution of the continuous variables.
We used descriptive statistics to define patient characteristics and used parametric and nonparametric tests, such as, the Independent-Samples T-test, Mann-Whitney, Chi-square, and Fisher's Exact test for statistical inference. Multivariate Cox proportional hazards regression analysis was used to examine the association between potential prognostic factors and the occurrence of posttraumatic seizures after traumatic brain injury. Hazard ratios (HRs) were presented with their 95% confidence interval.
All analyses were done using Statistical Package for Social Sciences Version 20 (SPSS Inc., Chicago, IL, USA) and Stata version 10.1 (StataCorp LP, College Station, USA). P-values less than 0.05 were considered significant.
RESULTS
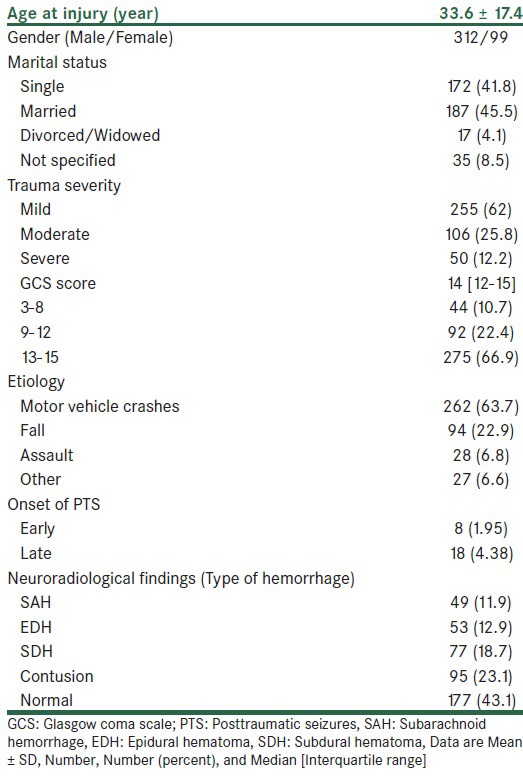
Four hundred and eleven patients (312 men and 99 women) entered the study. The mean of patients was 33.6 ± 17.4 years, with an age range of eight to 79 years and a median age of 27 years. Table 1 contains the details of the study population.
Table 1.
Demographic and clinical characteristics of 411 traumatic brain injury patients
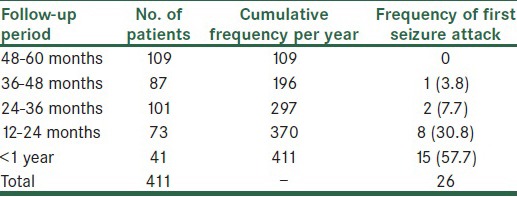
All the patients were followed for a median of 36 months. One hundred and ninety-six patients (47.7%) were followed for more than three years [Table 2]. Also, the total number of first seizure events in the specified period is shown in this table.
Table 2.
Duration of follow-up in the present cohort and occurrence of the first seizure attack
The overall incidence of posttraumatic seizure in this study population was 6.33%, with a 95% CI: 3.96-8.69), with higher frequency in severe head injuries. As shown in Table 1, the number of subjects who experienced early posttraumatic seizure (EPTS) was eight (1.95%). Also, the incidence rate of late posttraumatic seizure (LPTS) was 18 (4.38%).
The demographic and clinical characteristics of the patients with early and late posttraumatic seizures are shown in detail in Table 3.
Table 3.
The comparison of demographic and clinical features of 26 patients with early and late posttraumatic seizures
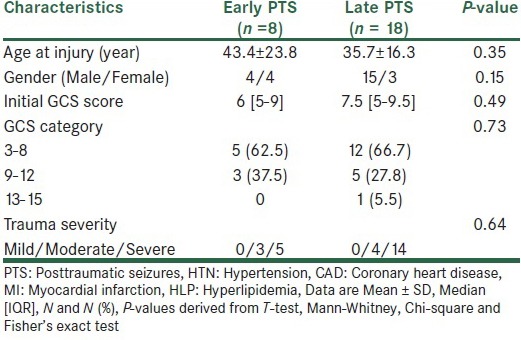
As it is shown by the analysis of the statistics, there were statistically no significant differences between the two groups with respect to the mean of age, sex, GCS score, and trauma severity. The other non-significant associations were not present in the bivariate analysis.
We constructed Kaplan-Meier plots and Cox proportional hazard ratios for prediction of time to posttraumatic seizures. The univariate and adjusted hazard ratio, 95% CI, and P-value for each variable in the Cox's proportional hazard model for risk of PTS in all 411 patients are shown in Table 4.
Table 4.
The univariate and multivariable Cox regression analyses of time to posttraumatic seizures
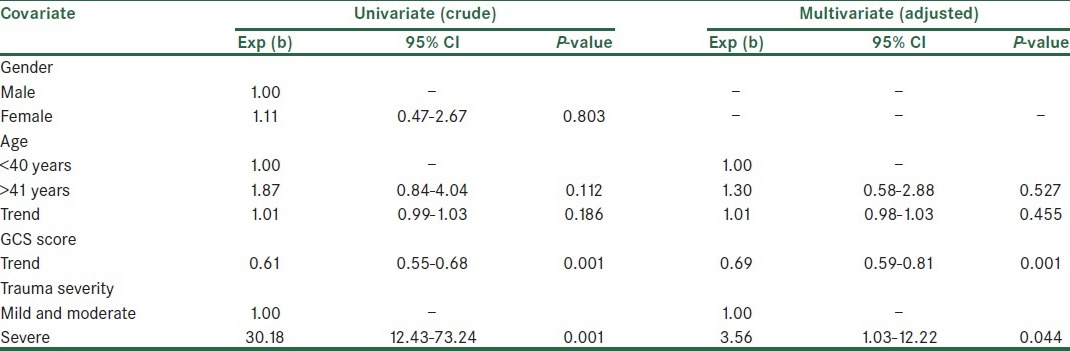
The log rank analysis showed that the female patients had 1.11 times more hazards of PTS, as compared to males, however, it was not statistically significant (P = 0.803) [Figure 1].
Figure 1.
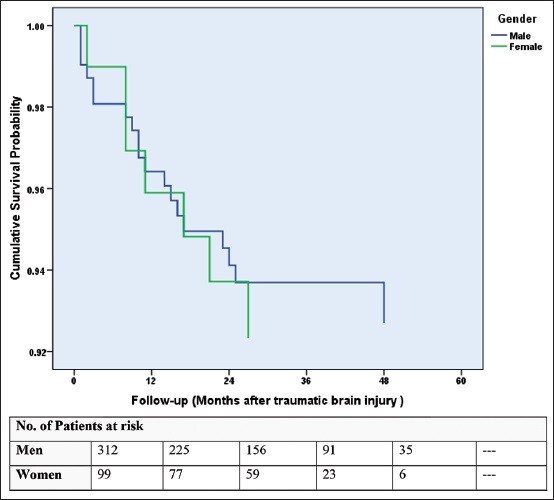
The Kaplan–Meier product limits estimates for probability of survival, by gender, The hazard ratio for posttraumatic seizures among female patients as compared to males, was 1.11 (95% confidence interval, 0.47 to 2.67; P = 0.8).
The log-rank analysis showed that the patients with severe traumatic brain injury had 30 times more hazards of PTS as compared to the patients with mild-to-moderate traumatic brain injury (P = 0.001) [Figure 2]. Variables, including age, sex, trauma severity, and GCS score were entered into a Cox proportional-hazards model, to identify the predictors of PTS. Variables with a probability value of <0.2 were retained.
Figure 2.
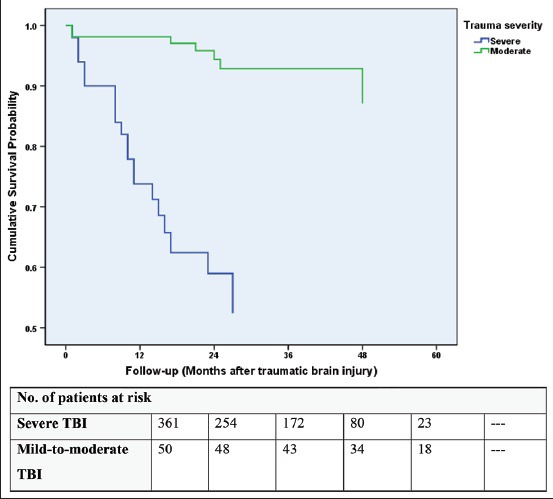
Kaplan–Meier product limits estimates for probability of survival, by trauma severity
The adjusted hazard ratio for posttraumatic seizures among patients with severe TBI, as compared to those with mild-to-moderate TBI, was 3.56 (95% confidence interval, 1.03 to 12.22; P < 0.044).
DISCUSSION
Posttraumatic seizures, as sequelae of traumatic brain injury, have been fairly well-documented; Meanwhile, the distribution of early and late seizures is not clearly understood. The present investigation as a five-year follow-up survival analysis tries to identify the early and late posttraumatic seizures following traumatic brain injury in patients referring to Emergency Units of the Isfahan University Hospitals.
As our results indicate, there were no statistically significant differences between early and late seizure groups, with respect to the mean of age, sex, GCS score, and trauma severity.
According to the study conducted by Asikainen et al., children are more susceptible to early seizures, while juveniles and adults are more prone to late seizures,[16,17] Unlike the findings in the present study, there were no statistically significant differences between the two groups of early and late seizures, with respect to the mean of age and sex. It should also not be ignored that although the sex is not statistically significant, female patients had 1.11 times more hazards of posttraumatic seizure as compared to males (P = 0.803).
Saadat et al., have expressed that age, GCS, Injury Severity Score (ISS), arterial blood pressure (BP), and respiratory rate (RR) are prognostic factors in patients with TBI. Our results confirmed their findings for the GCS score (P < 0.001) and trauma severity (P = 0.044), but in contrast to their study we could not find statistically significant differences regarding the age.[17]
The total incidence of posttraumatic seizure in this study population was 6.33%, with a higher frequency in severe head injury, while in former studies the incidence of seizures has been expressed to be from 2 to 25%.[21,22,23]
One of the important factors for the incidence of seizures after trauma is prophylaxis with common anti-seizure medications such as Dilantin. It seems that the medication of an antiepileptic drug for every brain injury (including not severe trauma) or in other words, over prophylaxis, has been affecting the low rate of seizures in the present study.
One of the major limitations of our study is that the patients underwent different types of management prior to arriving at our Emergency Units. Blood pressure (BP), respiratory rate (RR), alcohol utilization, hypoxia, and hyperthermia were significant risk factors in other studies, and hence, we did not name these factors in our investigation.
Another major limitation of the present study was the absence of length of hospital stay, which should be considered in future studies, because this shortage could change the real incidence of seizures.
In conclusion, our results indicated that trauma severity and the Glasgow Coma Scale (GCS) were effective risk factors in the incidence of seizures in patients with TBI. Particular care is advocated for patients with regard to these risk factors during the primary handling in Emergency Units.
ACKNOWLEDGMENTS
The authors appreciate the financial support given by the Vice Chancellor for Research (School of Medicine, Isfahan University of Medical Sciences, Isfahan, IRAN) [Project number: 390531].
Footnotes
Source of Support: Vice Chancellor for Research (School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran)
Conflict of Interest: None declared.
REFERENCES
- 1.Barkley JM, Morales D, Hayman LA, Diaz-Marchan PJ. Static neuroimaging in the evaluation of TBI. Brain injury medicine: Principles and practice. 2007:129–48. [Google Scholar]
- 2.Shukla D, Devi BI, Agrawal A. Outcome measures for traumatic brain injury. Clin Neurol Neurosurg. 2011;113:435–41. doi: 10.1016/j.clineuro.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Coronado VG, Faul M, Wald MM, Xu L. Traumatic brain injury in the United States: Emergency department visits, hospitalizations, and deaths, 2002-2006: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. 2010 [Google Scholar]
- 4.Wagner AK, Miller MA, Scanlon J, Ren D, Kochanek PM, Conley YP. Adenosine A1 receptor gene variants associated with post-traumatic seizures after severe TBI. Epilepsy Res. 2010;90:259–72. doi: 10.1016/j.eplepsyres.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajendra Acharya U, Vinitha Sree S, Swapna G, Martis RJ, Suri JS. Automated EEG analysis of epilepsy: A review. Knowledge-Based Systems. 2013 [Google Scholar]
- 6.Labate D, Inuso G, Occhiuto G, La Foresta F, Morabito FC. Neural Nets and Surroundings. Springer; 2013. Measures of brain connectivity through permutation entropy in epileptic disorders; pp. 59–67. [Google Scholar]
- 7.Asconape J, Penry J. Poststroke seizures in the elderly. Clinics in Geriatric Medicine. 1991;7:483–92. [PubMed] [Google Scholar]
- 8.Frey LC. Epidemiology of posttraumatic epilepsy: A critical review. Epilepsia. 2003;44:11–7. doi: 10.1046/j.1528-1157.44.s10.4.x. [DOI] [PubMed] [Google Scholar]
- 9.Jennett B. United Kingdom: Heinemann Medical; 1975. Epilepsy after non-missile head injuries. [DOI] [PubMed] [Google Scholar]
- 10.Annegers JF, Grabow JD, Groover RV, Laws ER, Elveback LR, Kurland LT. Seizures after head trauma A population study. Neurology. 1980;30:683–9. doi: 10.1212/wnl.30.7.683. [DOI] [PubMed] [Google Scholar]
- 11.Najafi MR, Abrishamkar S, Sonbolestan SA, Hamrah H. The effects of gabapentin on improvement of consciousness level in patients with traumatic brain injury: A randomized clinical trial. 2012 [Google Scholar]
- 12.Annegers JF, Hauser WA, Coan SP, Rocca WA. A population-based study of seizures after traumatic brain injuries. N Engl J Med. 1998;338:20–4. doi: 10.1056/NEJM199801013380104. [DOI] [PubMed] [Google Scholar]
- 13.Annegers JF, Grabow JD, Kurland LT, Laws ER., Jr The incidence, causes, and secular trends of head trauma in Olmsted County, Minnesota, 1935-1974. Neurology. 1980;30:912–9. doi: 10.1212/wnl.30.9.912. [DOI] [PubMed] [Google Scholar]
- 14.Annegers JF, Coan SP. The risks of epilepsy after traumatic brain injury. Seizure. 2000;9:453–7. doi: 10.1053/seiz.2000.0458. [DOI] [PubMed] [Google Scholar]
- 15.Temkin NR. Risk factors for posttraumatic seizures in adults. Epilepsia. 2003;44:18–20. doi: 10.1046/j.1528-1157.44.s10.6.x. [DOI] [PubMed] [Google Scholar]
- 16.Asikainen I, Kaste M, Sarna S. Early and late posttraumatic seizures in traumatic brain injury rehabilitation patients: Brain injury factors causing late seizures and influence of seizures on long-term outcome. Epilepsia. 1999;40:584–9. doi: 10.1111/j.1528-1157.1999.tb05560.x. [DOI] [PubMed] [Google Scholar]
- 17.Saadat S, Akbari H, Khorramirouz R, Mofid R, Rahimi-Movaghar V. Determinants of mortality in patients with traumatic brain injury. Ulus Travma Acil Cerrahi Derg. 2012;18:219–24. [PubMed] [Google Scholar]
- 18.Groswasser Z, Cohen M, Keren O. Female TBI patients recover better than males. Brain Inj. 1998;12:805–8. doi: 10.1080/026990598122197. [DOI] [PubMed] [Google Scholar]
- 19.Aghakhani N, Azami M, Jasemi M, Khoshsima M, Eghtedar S, Rahbar N. Epidemiology of traumatic brain injury in Urmia, Iran. Iran Red Crescent Med J. 2013;15:173–4. doi: 10.5812/ircmj.2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970 [Google Scholar]
- 21.Garga N, Lowenstein DH. Posttraumatic epilepsy: A major problem in desperate need of major advances. Epilepsy Curr. 2006;6:1–5. doi: 10.1111/j.1535-7511.2005.00083.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Englander J, Bushnik T, Duong TT, Cifu DX, Zafonte R, Wright J, et al. Analyzing risk factors for late posttraumatic seizures: A prospective, multicenter investigation. Arch Phys Med Rehabil. 2003;84:365–73. doi: 10.1053/apmr.2003.50022. [DOI] [PubMed] [Google Scholar]
- 23.Angeleri F, Majkowski J, Cacchio G, Sobieszek A, D’Acunto S, Gesuita R, et al. Posttraumatic epilepsy risk factors: One-year prospective study after head injury. Epilepsia. 1999;40:1222–30. doi: 10.1111/j.1528-1157.1999.tb00850.x. [DOI] [PubMed] [Google Scholar]


