Abstract
Background:
Onychomycosis is one of the most common clinical forms of fungal infections due to both filamentous fungi and yeasts. The genus of Candida is one of the most prominent causes of onychomycosis in all around the world. Although Candida albicans is still the most frequent cause of nail infections, use of broad-spectrum antifungal agents has led to a shift in the etiology of C. albicans to non-albicans species. The aim of the present study is rapid and precise identification of candida species isolated from nail infection by using of PCR-RFLP technique.
Materials and Methods:
A total of 360 clinical yeast strains were collected from nail infections in Iran. Genomic DNA was extracted using FTA; cards. ITS1-5.8SrDNA-ITS2 region was amplified using universal primers and subsequently products were digested with the restriction enzyme MspI. For identification of newly described species (C. parapsilosis complex), the SADH gene was amplified, followed by digestion with Nla III restriction enzyme.
Results:
Candida albicans was the most commonly isolated species (41.1%), followed by C. parapsilosis (21.4%), C. tropicalis (12.8%), C. kefyr (9.4%), C. krusei (5.5%), C. orthopsilosis (4.1%), C. glabrata (2.8%), C. guilliermondii (1.4%), C. rugosa (0.8%), and C. lusitaniae (0.5%). Patients in the age groups of 51-60 and 81-90 years had the highest and lowest distribution of positive specimens, respectively.
Conclusion:
Rapid and precise identification of Candida species from clinical specimens lead to appropriate therapeutic plans.
Keywords: Candida species, onychomycosis, PCR-RFLP
INTRODUCTION
Onychomycosis encloses all fungal infections of the nail due to filamentous and yeast fungi, accounted for up to 50% of all nail disorders which ranging from distal and lateral subungual, superficial, proximal subungual and dystrophic onychomycosis; however, in immunocompromised hosts can present a more significant health problem.[1,2] Studies have shown that the prevalence of onychomycosis increases with age and reasons for the age-related raise in onychomycosis may contain deficient circumferential circulation, repeated nail trauma, longer exposure to pathogenic fungi, diabetes, dysfunction of immune system, incompetence to cut the toenails or keep good foot considerations.[3,4] Moreover, numerous factors exist for increasing the prevalence of onychomycosis in modern life such as wearing of shoes especially high-heeled shoes, high moisture areas (gymnasium and wrestling mattresses by great numbers of people), use of broad-spectrum antibiotics, and corticosteroid therapy.[5] Although dermatophyte species cause 90% of toenails onychomycosis, Candida specie is considered as one of the most important causes of fingernail onychomycosis.[6,7] Candida albicans is the most prevalent species that can cause Candida nail infections and invades the entire nail plate, but onycholysis and paronychia may occur.[7] In cases of the nail Candida infections, accurate identification of causative agents at the species level is crucially important due to rapid development of resistance of some species to antifungal drugs, for instance C. krusei is innately resistant to fluconazole, and C. glabrata is able to be resistant.[8] Therefore, due to the high degree of phenotypic similarity between Candida species, identification problems are imminent. Conventional approaches for identification down to the species level in the diagnostic laboratory are based on morphological and physiological criteria, need several days or weeks to be concluded, and are frequently unspecific. However, today molecular identification methods are well established, e.g., restriction fragment length polymorphisms (RFLP), RFLP with hybridization probes, randomly amplified polymorphic DNA (RAPD) analysis, electrophoretic karyotyping, and sequencing. The latter method is relatively expensive, [9] therefore, alternative molecular tools with sufficient specificity, reproducibility and sensitivity are necessary.[9,10] Thus, in the present study, we used polymerase chain reaction (PCR) to amplify the entire internal transcribed spacer (ITS)-rDNA region and secondary alcohol dehydrogenase (SADH) gene, followed by RFLP analysis for identification of Candida species were obtained from onychomycosis.
MATERIALS AND METHODS
Fungal strains
A total of 360 clinical yeast strains were obtained from nail infections of patients at Tehran, Isfahan, Alborz, Kashan, and Mazandaran provinces of Iran, from April 2009 to June 2011. All strains were cultured on sabouraud glucose agar (Difco, Detroit, MI, USA) and incubated at 28-30°C for 48 h. A loopful of single and fresh colonies of each strain was transferred to glycerol 20% and stored at –20°C prior to use.
DNA extraction and amplification of the ITS rDNA regions
Genomic DNA was extracted using FTA® Elute Micro Cards (Whatman Inc., Clifton, NJ, USA) according to the manufacturer's instructions.[11] Briefly, fresh colony was suspended in 100 μl of sterile water, then 4 μl of the suspension was dribbled on a disc of FTA card (3 mm in diameter), subsequently incubated at room temperature for at least 3 hours. The dried papers were eluted in 500 μl distilled water for a few seconds. FTA card was transferred to a new tube containing 30 μl distilled water and incubated at 95°C for 25 minutes. At last the paper discs were taken away and the water containing DNA was kept at –20°C. The internal transcribed spacer region (ITS1-5.8SrDNA-ITS2) region was amplified by using two universal ITS1 (5Ͳ-TCCGTAGGTGAACCTGCG G-3Ͳ) and ITS4 (5Ͳ-TCCTCC GCT TATTGATATGC-3Ͳ) primers.[12] PCR reactions were performed on a Gene Amp PCR System 9700 (Applied Biosystems, Foster City, CA) in 25 μl volumes containing 25 ng of template DNA, 2.5 μl reaction buffer (0.1 M Tris-HCl, pH 8.0, 0.5 M KCl, 15 mM MgCl2, 0.1% gelatine, 1% Triton X-100), 0.1 mM of each dNTP and 1.0 U Taq DNA polymerase. Amplification was performed with cycles of 2 min at 94°C for primary denaturation, followed by 35 cycles at 95°C (30 s), 55°C (45 s) and 72°C (60 s), with a final 7 min extension step at 72°C.
Digestion with the restriction enzyme MspI and NlaIII
PCR products were digested in a final reaction volume of 15 μl containing 3 μl water, 1.5 μl buffer, 1U of restriction enzyme MspI (Fermentas, Vilnius, Lithuania)[13] and 10 μl PCR product at 37°C for 2 hours. For identification of newly described species in the C. parapsilosis complex including C. parapsilosis, C. orthopsilosis, and C. methapsilosis, the SADH gene was amplified using the SADHF (5Ͳ-GTT GAT GCT GTT GGA TTG T-3Ͳ) and SADHR (5Ͳ-CAA TGC CAA ATC TCC CAA-3Ͳ) primers, [14] followed by digestion with NlaIII (Hin1II) restriction enzyme (Fermentas, Vilnius, Lithuania).[15,16] Finally, 5 μl of PCR amplicons and 10 μl of RFLP products were loaded on 1.5 and 2% agarose gel, respectively, in TBE buffer (Tris 0.09 M, Boric acid 0.09 M, EDTA 2 mM) and stained with 0.5 μg/ml ethidium bromide. The bands patterns were visualized using the gel documentation system (UVITEC, Cambridge, UK) and photographed.
Culture on CHROMagar Candida
A total of 80 isolates containing C. albicans, C. tropicalis, C. krusei, and C. glabrata (n = 20 for each species) were sub-cultured on CHROMagar Candida (CHROMagar Microbiology, Paris, France), and incubated at 35° C for 2 days observing for color differences for each species [17,18] for confirmation and the reliability of the PCR-RFLP method.
RESULTS
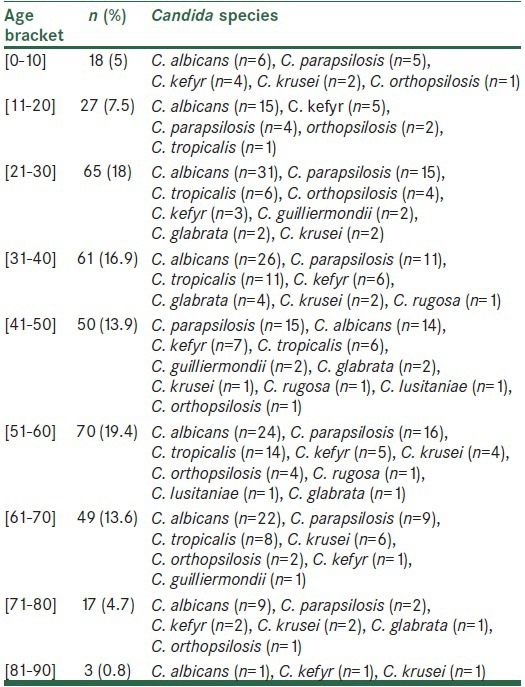
Since April 2009 to June 2011, 360 clinical isolates were obtained from patients in different geographical locations. According to the size of ITS rDNA region [Figure 1] and MspI-RFLP fragments of strains [Figure 2], the isolates were identified. A total of 77 C. parapsilosis complex were screened by amplification of the SADH gene and digested with NlaIII restriction enzyme [Figure 3]. In this stage, 15 isolates of C. orthopsilosis were identified. The most prevalent species was C. albicans (41.1%), followed by C. parapsilosis (21.4%), C. tropicalis (12.8%), C. kefyr (9.4%), C. krusei (5.5%), C. orthopsilosis (4.1%), C. glabrata (2.8%), C. guilliermondii (1.4%), C. rugosa (0.8%), and C. lusitaniae (0.5%) [Table 1]. Sixty-nine (19.2%) patients were males and 291 (80.1%) were females. The age range of patients was between 7 and 88 years. The majority numbers of patients were between 51 and 60 years [Table 2]. Sixteen (4.4%) strains were obtained from toenails, and 344 (95.5%) strains from fingernails. C. tropicalis, C. guilliermondii, and C. lusitaniae strains were not isolated from male patients. The results of the identification based on species level observed on CHROMagar Candida for 80 selected Candida isolates was 100% in agreement with the species delineation in PCR-RFLP method utilized in the present study (data not shown).
Figure 1.
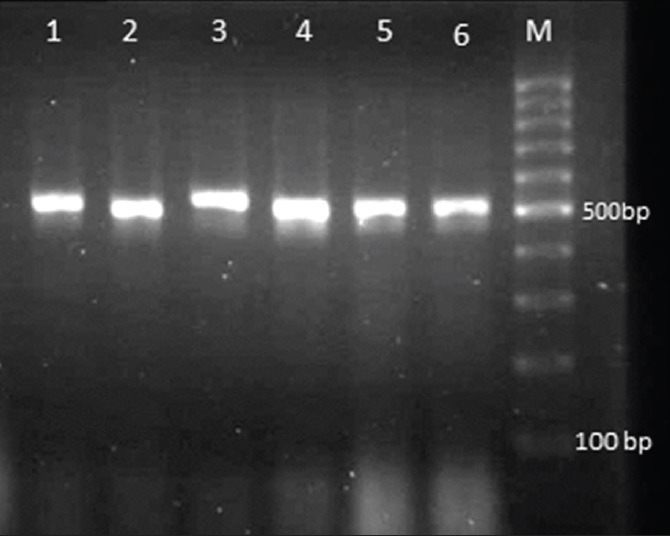
Gel electrophoresis of ITS-PCR products of clinical Candida species. Lane 1: C. tropicalis, Lane 2,4: C. krusei, Lane 3: C. albicans, Lane 5,6: C. parapsilosis
Figure 2.
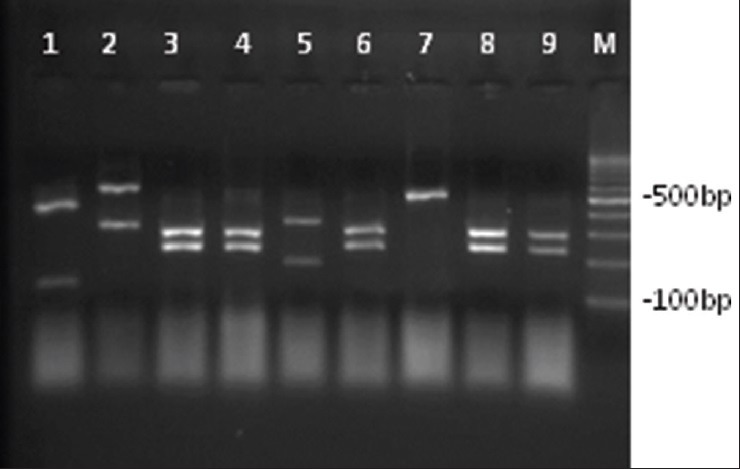
Agarose gel electrophoresis of ITS-PCR products of clinical yeast strains after digestion with Msp I. Lane 1: C. guilliermondii, lane 2: C. glabrata, lane 3,4,6,8,9: C. albicans, lane 5: C. tropicalis, lane 7: C. parapsilosis, and lane M: 100 bp Ladder
Figure 3.
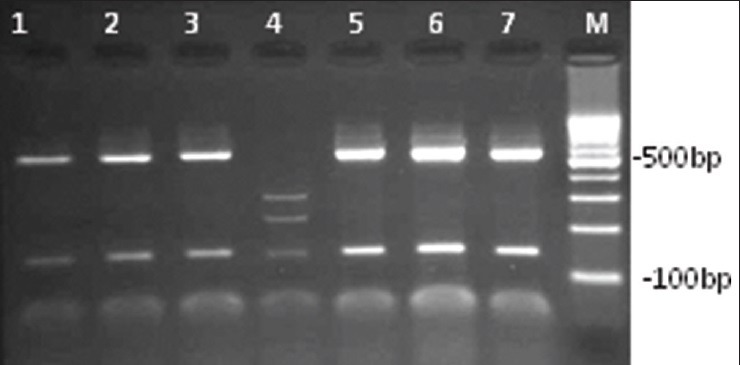
Electrophoretic patterns of SADH-RFLP by NlaIII restriction enzyme in C. parapsilosis group, isolated from onychomycosis in Iran. Lane 1,2,3,5,6,7: C. parapsilosis, lane 4: C. orthopsilosis, and lane M: 100 bp Ladder
Table 1.
Candida species isolated from nail infections in Iran, from April 2009 to June 2011
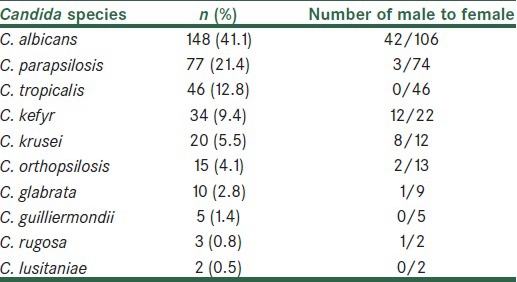
Table 2.
Age bracket of patients with onychomycosis in Iran during 2009-2011
DISCUSSION
“Onychomycosis” conventionally referred to non-dermatophytic infection of the nail; however, it is nowadays applied as a common term to designate any fungal nail infection.[19] Candida nail infections occur in patients with chronic mucocutaneous candidiasis which are caused by C. albicans and non-albicans species. Candida onychomycosis occur more frequently in female rather than male and often affect the middle finger which probably due to contact with Candida strains that are in the intestine or vagina.[7,20] Laboratory diagnosis of onychomycosis consists of direct microscopic examination to see fungal elements in nail specimens and culture to identify the species involved. In addition, conventional approaches for identification down to the species level in the diagnostic laboratory are based on morphological and physiological criteria, need several days or weeks to be concluded, and are frequently unspecific. Therefore, discrimination between isolated organisms as pathogens, saprophytes, colonizers, and contamination of the culture plate is a big challenge. Owing to the fact that typically the treatment phase of the onychomycosis is over a long period and takes much time for the nail to grow completely. furthermore non-albicans species like C. glabrata, C. parapsilosis, C. tropicalis, C. lusitaniae, and C. krusei have appeared as significant opportunistic pathogens [21] and show dissimilarities in levels of resistance to antifungal agents, [8,22] use of molecular approach to correctly identify the causative agent based on species level for appropriate antifungal regimen is crucially mandatory. Our study has documented that C. albicans caused (41.1%) of onychomycosis and non-albicans species connected with (58.9%) nail infections. Several studies have shown an increasing prevalence of onychomycosis with age, [21,23] but our study did not reveal any meaningful association between these parameters [Table 2]. Tainwala et al.[24] reported only one case of onychomycosis below 20 years, whereas we found 45 (12.5%) positive specimens in age range 0-20 years. Many investigations showed that onychomycosis was more common in males than females; [25,26] however, the ratio of male to female in our study was approximately 1:4. In the present survey, all fingernail infection caused by C. albicans, excluding two cases, had paronychia which is in conformity with different studies.[27,28] Amplification and digestion of the ITS rDNA region with MspI produced a two-band pattern for C. albicans, C. glabrata, C. tropicalis, C. krusei, C. lusitaniae and C. rugosa, in contrast a three-band pattern for C. guilliermondii.[29] Some species like C. parapsilosis and C. kefyr have no cutting site for restriction enzyme MspI; nevertheless, we confirmed our results by amplification of the SADH gene of the C. parapsilosis group, following digestion of PCR products with NlaIII restriction enzyme.[15] Since 2005, C. parapsilosis complex reclassified to C. parapsilosis, C. orthopsilosis, and C. methapsilosis.[14] It is considerable that we isolated C. orthopsilosis (n = 15) from onychomycosis for the first time in Iran. There was not any C. methapsilosis strain among these isolates. C. kefyr generated an approximately 720 bp band and were discriminated from the C. parapsilosis complex, which presented a 520 bp band. In agreement to our study, Feng et al.[30] reported C. parapsilosis was the most prevalent strain of Candida onychomycosis among non-albicans species. Infections caused by C. glabrata are increasing in all clinical forms of candidiasis.[31] Candida glabrata is a complex of species too, comprising two new species C. nivariensis [32] and C. bracarensis.[33] According to the size of variation of ITS-amplicons, [34] neither C. bracarensis nor C. nivariensis were identified among our strains. Contrary to our findings, Chai et al.[35] showed that nail infections in consequence of C. tropicalis are infrequently seen, whereas we isolated 46 strains from clinical samples. Similar to the current study, Chadeganipour et al.[36] described that C. albicans was the most prevalent (84%) species among yeasts, and females were affected more frequently than males. Khosravi et al.[37] reported Candida albicans and C. parapsilosis as predominant species of the Genus Candida that were isolated from onychomycosis. Hashemi et al.[38] revealed 25.5% of onychomycosis cases related to yeast strains and C. albicans was the main candida species in their study. Rising of non-albicans strains among clinical specimens and differences in levels of resistance to the antifungal drugs among Candida species are important subjects in medicine. Therefore, molecular techniques are suitable and reliable methods for precise and correct identification of clinical pathogens at the species level which would be useful in clinical laboratories and lead to a perfect control of infections.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Baran R, Hay RJ, Tosti A, Haneke E. A new classification of onychomycosis. Br J Dermatol. 1998;139:567–71. doi: 10.1046/j.1365-2133.1998.02449.x. [DOI] [PubMed] [Google Scholar]
- 2.Scher RK. Onychomycosis: A significant medical disorder. J Am Acad Dermatol. 1996;35:S2–5. doi: 10.1016/s0190-9622(96)90061-4. [DOI] [PubMed] [Google Scholar]
- 3.Drake LA, Dinehart SM, Farmer ER, Goltz RW, Graham GF, Hordinsky MK, et al. Guidelines/Outcomes Committee. Guidelines of care for superficial mycotic infections of the skin: Onychomycosis. J Am Acad Dermatol. 1996;34:116–21. doi: 10.1016/s0190-9622(96)80136-8. [DOI] [PubMed] [Google Scholar]
- 4.Elewski BE, Charif MA. Prevalence of onychomycosis in patients attending a dermatology clinic in northeastern Ohio for other conditions. Arch Dermatol. 1997;133:1172–3. [PubMed] [Google Scholar]
- 5.Lohoué Petmy J, Lando AJ, Kaptue L, Tchinda V, Folefack M. Superficial mycoses and HIV infection in Yaounde. J Eur Acad Deramtol Venereol. 2004;18:301–4. doi: 10.1111/j.1468-3083.2004.00924.x. [DOI] [PubMed] [Google Scholar]
- 6.Zomorodian K, Rahimi MJ, Pakshir K, Motamedi M, Ghiasi MR, Rezashah H. Determination of antifungal susceptibility patterns among the clinical isolates of Candida species. J Glob Infect Dis. 2011;3:357–60. doi: 10.4103/0974-777X.91059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.André J, Achten G. Onychomycosis. Int J Dermatol. 1987;26:481–90. doi: 10.1111/j.1365-4362.1987.tb02287.x. [DOI] [PubMed] [Google Scholar]
- 8.Borst A, Theelen B, Reinders E, Boekhout T, Fluit AC, Savelkoul PH. Use of amplified fragment length polymorphism analysis to identify medically important Candida spp., including C. dubliniensis. J Clin Microbiol. 2003;41:1357–62. doi: 10.1128/JCM.41.4.1357-1362.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soll DR. The ins and outs of DNA fingerprinting the infectious fungi. Clin Microbiol Rev. 2000;13:332–70. doi: 10.1128/cmr.13.2.332-370.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Enger L, Joly S, Pujol C, Simonson P, Pfaller M, Soll DR. Cloning and characterization of a complex DNA fingerprinting probe for Candida parapsilosis. J Clin Microbiol. 2001;39:658–69. doi: 10.1128/JCM.39.2.658-669.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borman AM, Linton CJ, Miles SJ, Campbell CK, Johnson EM. Ultra-rapid preparation of total genomic DNA from isolates of yeast and mould using Whatman FTA filter paper technology-a reusable DNA archiving system. Med Mycol. 2006;44:389–98. doi: 10.1080/13693780600564613. [DOI] [PubMed] [Google Scholar]
- 12.White TJ, Bruns T, Taylor J. Innis MA, Gelfand DH, Sninsky JJ, White TJ. PCR Protocols: A Guide to Methods and Applications. London, UK: Academic Press; 1990. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics; pp. 315–22. [Google Scholar]
- 13.Mirhendi H, Makimura K, Khoramizadeh M, Yamaguchi H. A one-enzyme PCR-RFLP assay for identification of six medically important Candida species. Nihon Ishinkin Gakkai Zasshi. 2006;47:225–9. doi: 10.3314/jjmm.47.225. [DOI] [PubMed] [Google Scholar]
- 14.Tavanti A, Davidson AD, Gow NA, Maiden MC, Odds FC. Candida orthopsilosis and Candida metapsilosis spp. nov. to replace Candida parapsilosis groups II and III. J Clin Microbiol. 2005;43:284–92. doi: 10.1128/JCM.43.1.284-292.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mirhendi H, Bruun B, Schønheyder HC, Christensen JJ, Fuursted K, Gahrn-Hansen B, et al. Molecular screening for Candida orthopsilosis and Candida metapsilosis among Danish Candida parapsilosis group blood culture isolates: Proposal of a new RFLP profile for differentiation. J Med Microbiol. 2010;59:414–20. doi: 10.1099/jmm.0.017293-0. [DOI] [PubMed] [Google Scholar]
- 16.Mohammadi R, Mirhendi H, Yadegari MH, Ghahri M, Shadzi S, Jalalizand N, et al. Evaluation of prevalence of the new Candida Species (C. Orthopsilosis and C. Metapsilosis) among C. Parapsilosis Group isolated from patients by PCR-RFLP of SADH Gene in Iran. J Isfahan Med Sch. 2011;29:1–10. [Google Scholar]
- 17.Odds FC, Bernaerts R. CHROMagar Candida, a new differential isolation medium for presumptive identification of clinically important Candida species. J Clin Microbiol. 1994;32:1923–9. doi: 10.1128/jcm.32.8.1923-1929.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daef E, Moharram A, Eldin SS, Elsherbiny N, Mohammed M. Evaluation of chromogenic media and seminested PCR in the identification of Candida species. Braz J Microbiol. 2014;45:255–62. doi: 10.1590/S1517-83822014005000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weitzman I, Summerbell RC. The dermatophytes. Clin Microbiol Rev. 1995;8:240–59. doi: 10.1128/cmr.8.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zaias N, Glick B, Rebell G. Diagnosing and treating onychomycosis. J Fam Pract. 1996;42:513–8. [PubMed] [Google Scholar]
- 21.Nucci M, Marr KA. Emerging fungal diseases. Clin Infect Dis. 2005;41:521–6. doi: 10.1086/432060. [DOI] [PubMed] [Google Scholar]
- 22.Gumbo T, Isada CM, Hall G, Karafa MT, Gordon SM. Candida glabrata Fungemia. Clinical features of 139 patients. Medicine (Baltimore) 1999;78:220–7. doi: 10.1097/00005792-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Kaur R, Kashyap B, Bhalla P. Onychomycosis--epidemiology, diagnosis and management. Indian J Med Microbiol. 2008;26:108–16. doi: 10.4103/0255-0857.40522. [DOI] [PubMed] [Google Scholar]
- 24.Tainwala R, Sharma YK. Current clinico-mycological trends of onychomycosis in Pune. Indian J Dermatol. 2012;57:242–3. doi: 10.4103/0019-5154.96220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bramono K, Budimulja U. Epidemiology of onychomycosis in Indonesia: Data obtained from three individual studies. Nihon Ishinkin Gakkai Zasshi. 2005;46:171–6. doi: 10.3314/jjmm.46.171. [DOI] [PubMed] [Google Scholar]
- 26.Banerjee U, Sethi M, Pasricha JS. Study of onychomycosis in India. Mycoses. 1990;33:411–5. doi: 10.1111/myc.1990.33.7-8.411. [DOI] [PubMed] [Google Scholar]
- 27.Haneke E. Fungal infections of the nail. Semin Dermatol. 1991;10:41–53. [PubMed] [Google Scholar]
- 28.Williams HC. The epidemiology of onychomycosis in Britain. Br J Dermatol. 1993;129:101–9. doi: 10.1111/j.1365-2133.1993.tb03510.x. [DOI] [PubMed] [Google Scholar]
- 29.Mohammadi R, Mirhendi H, Rezaei-Matehkolaei H, Ghahri M, Shidfar MR, Jalalizand N, et al. Molecular identification and distribution profile of Candida species isolated from Iranian patients. Med Mycol. 2013;51:657–63. doi: 10.3109/13693786.2013.770603. [DOI] [PubMed] [Google Scholar]
- 30.Feng X, Ling B, Yang G, Yu X, Ren D, Yao Z. Prevalence and distribution profiles of Candida parapsilosis, Candida orthopsilosis and Candida metapsilosis responsible for superficial candidiasis in a Chinese university hospital. Mycopathologia. 2012;173:229–34. doi: 10.1007/s11046-011-9496-5. [DOI] [PubMed] [Google Scholar]
- 31.Silva S, Negri M, Henriques M, Oliveira R, Williams DW, Azeredo J. Candida glabrata, Candida parapsilosis and Candida tropicalis: Biology, epidemiology, pathogenicity and antifungal resistance. FEMS Microbiol Rev. 2012;36:288–305. doi: 10.1111/j.1574-6976.2011.00278.x. [DOI] [PubMed] [Google Scholar]
- 32.Alcoba-Flórez J, Méndez-Alvarez S, Cano J, Guarro J, Pérez-Roth E, del Pilar Arévalo M. Phenotypic and molecular characterization of Candida nivariensis sp. nov., a possible new opportunistic fungus. J Clin Microbiol. 2005;43:4107–11. doi: 10.1128/JCM.43.8.4107-4111.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Correia A, Sampaio P, James S, Pais C. Candida bracarensis sp. nov., a novel anamorphic yeast species phenotypically similar to Candida glabrata. Int J Syst Evol Microbiol. 2006;56:313–7. doi: 10.1099/ijs.0.64076-0. [DOI] [PubMed] [Google Scholar]
- 34.Mirhendi H, Bruun B, Schønheyder HC, Christensen JJ, Fuursted K, Gahrn-Hansen B, et al. Differentiation of Candida glabrata, C. nivariensis and C. bracarensis based on fragment length polymorphism of ITS1 and ITS2 and restriction fragment length polymorphism of ITS and D1/D2 regions in rDNA. Eur J Clin Microbiol Infect Dis. 2011;30:1409–16. doi: 10.1007/s10096-011-1235-9. [DOI] [PubMed] [Google Scholar]
- 35.Chai LY, Denning DW, Warn P. Candida tropicalis in human disease. Crit Rev Microbiol. 2010;36:282–98. doi: 10.3109/1040841X.2010.489506. [DOI] [PubMed] [Google Scholar]
- 36.Chadeganipour M, Nilipour S, Ahmadi G. Study of onychomycosis in Isfahan, Iran. Mycoses. 2010;53:153–7. doi: 10.1111/j.1439-0507.2008.01679.x. [DOI] [PubMed] [Google Scholar]
- 37.Khosravi AR, Mansouri P. Onychomycosis in Tehran, Iran: Prevailing fungi and treatment with itraconazole. Mycopathologia. 2006;150:9–13. doi: 10.1023/a:1011028730323. [DOI] [PubMed] [Google Scholar]
- 38.Hashemi SJ, Gerami M, Zibafar E, Daei M, Moazeni M, Nasrollahi A. Onychomycosis in Tehran: Mycological study of 504 patients. Mycoses. 2010;53:251–5. doi: 10.1111/j.1439-0507.2009.01703.x. [DOI] [PubMed] [Google Scholar]


