Abstract
Objective
To determine the rate and trend of attrition from a surgical residency programme and to identify the reasons for attrition.
Methods
A questionnaire-based survey was conducted at a university hospital. Separate questionnaires were designed for residents and programme directors (PDs). The residents who left the training voluntarily from one of the five surgical residency programmes (i.e., general surgery, orthopaedics, neurosurgery, otorhinolaryngology and urology) during the academic years 2005–2011 were identified from a departmental database. The residents who did not respond after three attempts at contact, or those who refused to participate, were excluded.
Results
During the last 6 years, 106 residents were recruited; 84 (78%) were men, of whom 34.5% left the programme voluntarily. Of 22 women, half (54%) left the programme voluntarily (P = 0.07). The overall 6-year attrition rate was 39%. The reasons identified for attrition, in descending order, were personal reasons, attitude of senior residents or faculty, and change of specialty. None of the residents cited an excess workload as a reason for their leaving the programme. About 40% rejoined the same specialty after leaving, while 35% chose a different specialty (80% chose a different surgical subspecialty and 20% chose medicine). There was a significant discrepancy in the perspective of residents and PDs about the reasons for attrition.
Conclusion
Attrition among surgical residents, in particular woman residents, is high. Personal reasons and interpersonal relations were the most commonly cited reasons. Programme managers and residents have significantly different perspectives, again an indication of a communication gap.
Keywords: Residency, Urology, Attrition, Resident, Programme director
Introduction
Surgical training was once considered as an apprenticeship; Sir William Halsted advocated the idea of structured training, and he was instrumental in bringing a change in the training of surgeons from a disorganised apprenticeship to the modern appraisal-based training system. Early in the nineteenth century he introduced the German residency system of graded responsibility to North America [1,2].
Once a surgical career was considered the dream of every medical graduate, but with changing times there has been a decline in the interest in pursuing a career in surgery. In an interesting review Wanzel et al. [3] analysed the recent trend of declining interest in a surgical career, and noted that lifestyle changes, gender issues, and changes in governmental and medical school priorities are some of the major reasons. In another report [4] authors noted that the interest in general surgery actually peaked in the early 1980s and since then the number of applicants has been declining; only recently has this decline passed the threshold of available positions.
With the changing face of surgical training the trainers faced many challenges [5], attrition being one of them. Morris et al. [6] analysed the scope of and reasons for attrition in general surgery residents, noting that attrition occurs early in the residency and is mostly for quality of life reasons. Not only is there a decline in the number of applications, but also the retention of existing residents in the training programme has become a challenge. It is crucial to identify the factors resulting in attrition, as loss of a resident not only has a significant negative impact on the programme, but it also disturbs the career pathway of the resident [7].
Attrition in surgical residency is of continued concern for surgical educators globally. It is disruptive to the continued process of training a surgical resident. Attrition results in loss of morale and resources, and often leaves the programme struggling to find replacements for these residents. There has been an increase in the resident attrition rate over the years, but due to a paucity of data, the actual magnitude and factors associated with it are unclear.
The present study was designed to assess the perspective of both residents and programme directors (PDs) for the attrition in the surgical residency programme at a University Hospital.
Methods
We conducted a questionnaire-based survey at a University Hospital. Residents recruited during the academic years 2005–2011 in surgery and allied surgical specialties (general surgery; orthopaedics, neurosurgery, otorhinolaryngology and urology) were included in the study. There were no inductions in 2010, as the starting month of the academic year was changed from November to January at our institute. Only those surgical specialties were included in the study in which the residency programme started before 2005.
Residents who left the programme voluntarily were identified from the departmental database. Two separate questionnaires were designed for PDs and residents (Appendix 1). Residents were contacted by e-mail or telephone to complete the questionnaire. PDs were contacted either personally, by e-mail or telephone to complete the questionnaire. Residents who did not respond after three attempts, or those who refuse to participate, were excluded (Fig. 1). The attrition rate was defined as ‘the number of residents who left the programme voluntarily, divided by the total number of residents enrolled in that specific year’.
Figure 1.
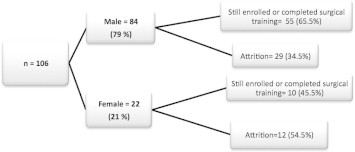
An algorithm of gender differences, showing the course from induction onwards.
Results
During the last six years, in all 106 residents were enrolled, of whom 84 were men and 22 were women; their course after enrolment is shown in Fig. 1. Twelve residents were excluded from further analysis as they either refused to participate or failed to respond to reminders. Forty-one residents (29 men and 12 women; mean age 29 years, SD 1.5) left the programme voluntarily during the study period. The women had a significantly higher rate of attrition than the men (54.5% vs. 34.5%), although this gender-related difference was not statistically significant (P = 0.07).
The 6-year overall attrition rate was 41/106 (38.6%) and the highest rate (nine of 13) was among inductees of 2008 (Fig. 2). The total number of residents leaving the programme was the highest in 2007 and 2008, i.e. 11/20 (55%) and nine of 13, respectively. For the other years it was variable, at 9/24 (38%) in 2005, one of 11 in 2006, six of 17 (35%) in 2009 and five of 21 (25%) in 2010. This trend of ‘rise in attrition’ was also apparent in the different specialties (Fig. 2). Not only the overall trend but also the rising rate of attrition in certain specialties (up to 100%) was a finding of concern (Table 1).
Figure 2.
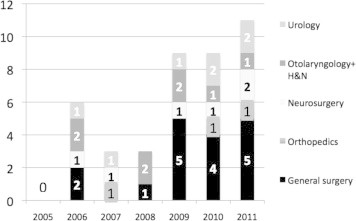
The number of residents leaving the programme in different specialties.
Table 1.
Trend of induction and attrition over the span of study period in different specialties.
| Specialty | Attrition/ inducted⁎ in year |
|||||
|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | 2011 | |
| General Surgery | 2/6 | 1/5 | 5/8 | 5/6 | 4/8 | 0/6 |
| Orthopedics | 0/6 | – | 2/3 | 0/1 | 0/2 | 1/4 |
| Neuro-surgery | 0/1 | 0/2 | 2/4 | 2/2 | 0/2 | 2/4 |
| ENT | 4/4 | 0/3 | 2/3 | 2/3 | 0/2 | 0/2 |
| Urology | 3/7 | 0/1 | 0/2 | 0/1 | 2/3 | 2/5 |
No of resident leaving the program/total number of resident inducted.
Most residents mentioned personal reasons (76%), while the remainder mentioned lifestyle (10%), expected financial return (8%) and workload (6%) as a reason to choose surgery. The quality of the academics (70%) and reputation (60%) were two major reasons cited by the residents for joining this surgical training programme.
Among the residents who left, half (51%) did so in the first 2 years of residency, 25% of whom did not continue beyond 3 months. Fourteen (34%) residents were in year 3 when they left the programme, of whom 10 were those who were inducted in a surgical subspecialty as year 3, while four residents left the programme after completing 2 years of residency (P < 0.04). There was only one chief resident who voluntarily left the programme just 2 months before graduation.
The reasons for attrition mentioned by residents were: personal (34.5%), attitude of senior residents (24%), attitude of faculty (13.7%), change of specialty (17%), nature of surgical training (10%) and the longer duration of training (5%). However, none of the residents cited the workload or low remuneration as factors for leaving the programme. For the seven female residents the most common personal reason for leaving the residency was reported as marriage (four), followed by personal health (one), health of spouse or family member (one), and migration (one). Women were more likely to leave for personal reasons.
The PDs of five subspecialties also mentioned personal issues as the main reason for attrition (44.8%), followed by a change of specialty (20.5%), performance (13.7%), and the attitude of faculty and senior residents (10.3%), workload (6.9%) and financial returns (3.4%). Except for personal reasons, there was a major discrepancy between the perspective of residents and PDs.
After leaving their specific residency programme, 39% of residents rejoined same surgical subspecialty elsewhere, while 39.5% joined some other specialty either within the same institute (18%) or elsewhere (21.5%). Of the residents who changed their specialty, 80% rejoined a surgical subspecialty, while 20% joined the emergency medicine department. However, none of the residents left medicine, although 21.4% of residents remained indecisive at the time of conducting the survey. Most residents (93%) had no regrets about the decision to leave the residency programme.
Discussion
Surgical training worldwide is undergoing unique changes and unfortunately attrition in residency programmes is one of them. Rising public expectations and dissatisfaction with the current service, concern for patient safety, increased use of technology, changing lifestyle preferences among medical students and globalisation of education and services are a few of the important factors identified affecting the surgical training programmes [2].
Women comprise more than half of medical school classes and only a small percentage of women opt for a surgical career [8]. Women are much less likely to undertake a surgical elective and are considerably less likely to choose a career in surgery [3]. However, the number of surgical residents far exceeds the female surgical faculty, indicating a positive trend. In the present study woman residents were more likely to leave surgical training. Although this has been reported from another series [5], the issue is particularly disturbing in the current study, 54.5% vs. 32% [6] and 43% [7]. Although the residents do not cite sexual harassment as a reason, it is known that it is grossly under-reported. Sexual harassment among the surgery residency programme was reported by Komaromy et al. [9] and later by Daugherty et al. [10], but attrition resulting from this has not been reported before. This phenomenon might not be unique to one institute, but due to a paucity of local literature this is a new but worrisome addition to the list of factors related to attrition. None of our residents, from either gender, cited this as a reason. One of the reasons for attrition for women residents, particularly in a more traditional society, is for marriage, family and other personal factors, like raising children. To accommodate parenting and other family roles, women in many professions, including surgery, are more likely to have part-time or intermittent participation in the work force [11,12].
Generally the factors noted that contribute to the attrition in the present study are in general consensus with what has been reported previously in international data [4], with the exception of the attitude of senior residents and faculty. This has not been cited as an independent reason in contemporary reports. Perhaps when the resident notes that the working environment was not conducive they are referring to this reason.
It is difficult to understand how enthusiastic surgical trainees work their way through many hurdles to enter a surgical residency programme, and then suddenly decide to quit. Richardson [13] used a triangle of professional satisfaction to illustrate three factors that are important in the determination of the level of career fulfilment. This might help to understand how certain attitudes can affect the growth, level of professional satisfaction and eventually the discontinuation of a career path that a trainee had chosen with great enthusiasm. The effect of long working hours on lifestyle, and the financial burden, remained issues of constant debate [5], but none of the residents in the present survey mentioned them as a reason for leaving. A change of specialty is another identified reason, but interestingly most residents who left then rejoined the same or a different surgical specialty. This result differs from those in previous studies, where residents left the surgical training programme to pursue a career with a more controlled lifestyle [5,14,15]. Residents are more likely to leave the programme in the earlier years of residency [5,16,17], but our study shows that attrition occurred even at a senior level, although the causes between the groups were different.
There is a significant discrepancy between the perspective of residents and PDs; this reflects the lack of communication between them. This might be one reason for the increasing trend of attrition, as the problems faced by the residents remained unidentified by the PDs and therefore were not addressed.
Within this study the need to identify the most suitable resident for surgical training has been re-emphasised, as there was a substantial percentage of residents who remained indecisive even after leaving the programme. Some novel selection strategies might need to be adopted to avoid or at least reduce attrition [18].
In conclusion, attrition in surgical residency programmes is a major challenge to the programmes. Woman residents are more likely to leave. Identifying the factors responsible might help to tailor the programme to minimise the attrition and its effect on disrupting the residency programmes. There are some generic causes, but the order of these issues might have a significant local influence.
Conflict of interest
None.
Source of funding
None.
Footnotes
Peer review under responsibility of Arab Association of Urology.
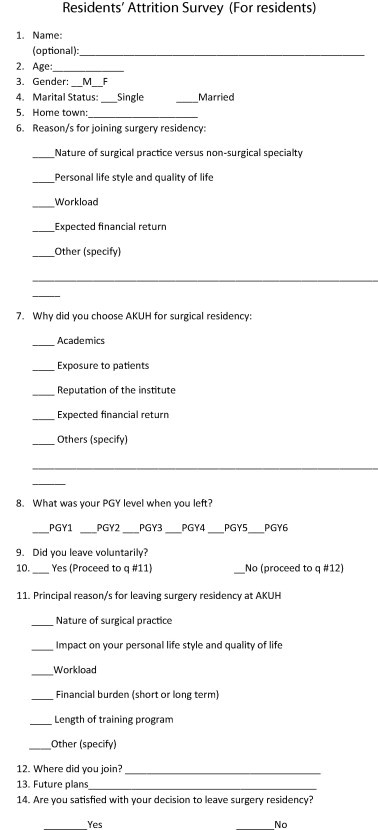
Appendix 1.
The survey proforma used in the study for assessing the perspective of PDs (a) and residents (b).

References
- 1.Osborne M.P. William Stewart Halsted. His life and contributions to surgery. Lancet Oncol. 2007;8:256–265. doi: 10.1016/S1470-2045(07)70076-1. [DOI] [PubMed] [Google Scholar]
- 2.Halsted W.S. Johns Hopkins Hospital; Baltimore, MD: 1904. The Training of the Surgeon. [15: 267–75] [Google Scholar]
- 3.Wanzel K.R., Ward M., Reznick R.K. Teaching the surgical craft: from selection to certification. Curr Probl Surg. 2002;39:573–659. doi: 10.1067/mog.2002.123481. [DOI] [PubMed] [Google Scholar]
- 4.Bland K.I., Isaacs G. Contemporary trends in student selection of medical specialties: the potential impact on general surgery. Arch Surg. 2002;137:259–267. doi: 10.1001/archsurg.137.3.259. [DOI] [PubMed] [Google Scholar]
- 5.Lum S.K., Crisostomo A.C. A comparative study of surgical training in South East Asia, Australia and the United Kingdom. Asian J Surg. 2009;32:137–142. doi: 10.1016/S1015-9584(09)60384-5. [DOI] [PubMed] [Google Scholar]
- 6.Morris J.B., Leibrandt T.J., Rhodes R.S. Voluntary changes in surgery career paths. A survey of the program directors in surgery. J Am Coll Surg. 2003;196:611–616. doi: 10.1016/S1072-7515(02)01832-X. [DOI] [PubMed] [Google Scholar]
- 7.Naylor R.A., Reisch J.S., Valentine R.J. Factors related to attrition in surgery residency based on application data. Arch Surg. 2008;143:647–651. doi: 10.1001/archsurg.143.7.647. [DOI] [PubMed] [Google Scholar]
- 8.American Association of Medical Colleges. Women in US Academic medicine Statistics 2000–1, Washington DC. American Association of Medical Colleges, 2001.
- 9.Komaromy M., Bindman A.B., Haber R.J., Sande M.A. Sexual harassment in medical training. N Engl J Med. 1993;328:322–326. doi: 10.1056/NEJM199302043280507. [DOI] [PubMed] [Google Scholar]
- 10.Daugherty S.R., Baldwin D.C., Jr., Rowley B.D. Learning, satisfaction, and mistreatment during medical internship: a national survey of working conditions. JAMA. 1998;279:1194–1199. doi: 10.1001/jama.279.15.1194. [DOI] [PubMed] [Google Scholar]
- 11.Bass B.L., Napolitano L.M. Gender and diversity considerations in surgical training. Surg Clin N Am. 2004;84:1537–1555. doi: 10.1016/j.suc.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Bergen P.C., Turnage R.H., Carrico C.J. Gender-related attrition in a general surgery training program. J Surg Res. 1998;77:59–62. doi: 10.1006/jsre.1998.5335. [DOI] [PubMed] [Google Scholar]
- 13.Richardson J.D. Workforce and lifestyle issues in general surgery training and practice. Arch Surg. 2002;137:515–520. doi: 10.1001/archsurg.137.5.515. [DOI] [PubMed] [Google Scholar]
- 14.Dodson T.F., Webb A.L. Why do residents leave general surgery? The hidden problem in today’s programs. Curr Surg. 2005;62:128–131. doi: 10.1016/j.cursur.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 15.Kwakwa F., Jonasson O. Attrition in graduate surgical education. An analysis of the 1993 entering cohort of surgical residents. J Am Coll Surg. 1993;1999(189):602–610. doi: 10.1016/s1072-7515(99)00198-2. [DOI] [PubMed] [Google Scholar]
- 16.Everett C.B., Helmer S.D., Osland J.S., Smith R.S. General surgery resident attrition and the 80-hour workweek. Am J Surg. 2007;194:751–756. doi: 10.1016/j.amjsurg.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 17.Yeo H., Bucholz E., Ann Sosa J., Curry L., Lewis F.R., Jr, Jones A.T. A national study of attrition in general surgery training: which residents leave and where do they go? Ann Surg. 2010;252:529–534. doi: 10.1097/SLA.0b013e3181f2789c. [DOI] [PubMed] [Google Scholar]
- 18.Kelz R.R., Mullen J.L., Kaiser L.R., Pray L.A., Shea G.P., Drebin J.A. Prevention of surgical resident attrition by a novel selection strategy. Ann Surg. 2010;252:537. doi: 10.1097/SLA.0b013e3181f27a50. [DOI] [PubMed] [Google Scholar]



