Prescribing of antidepressants has increased greatly in England and elsewhere in recent years.1-3 This increase has coincided with a fall in rates of suicide, leading some researchers to suggest a causal association.2,4-6 Meanwhile, others are concerned that antidepressants may precipitate suicidal behaviour.7,8 A recent review of evidence from paediatric trials by the Committee on Safety of Medicines in Britain led to most selective serotonin re-uptake inhibitors (SSRIs) being contraindicated in people aged younger than 18.9 So how safe are they? In this article, we assess the data on the risks and benefits.
Is increased prescribing linked to reduced suicide rates?
SSRIs and tricyclic antidepressants account for over 90% of antidepressant prescribing in Britain. Systematic reviews confirm that both these classes of antidepressant are effective in adults,10 although SSRIs are better tolerated by patients.11 The effectiveness of antidepressants in childhood and adolescence is less clear.12
As depression is the main psychiatric condition leading to suicide, it seems reasonable to infer that rises in antidepressant prescribing, which indicate improved management of depression, should have a beneficial effect on suicide rates. Indeed, an intervention to improve general practitioners' management of depression in a Swedish community resulted in increased antidepressant prescribing and a short term reduction in suicide.13
Summary points
Concern is growing that serotonin reuptake inhibitors (SSRIs) may precipitate suicidal behaviour, especially in children
Reassuringly, although antidepressant prescribing in Britain has more than doubled in the past 15 years, population suicide rates have fallen.
If the risks of SSRI associated suicidal behaviour seen in children were to apply to suicide in adults, the number of “antidepressant induced” suicides would be small enough to be masked by currently favourable suicide trends
Long term studies are required to assess the risks and benefits to population health of recent large scale rises in antidepressant prescribing.
Surprisingly, direct evidence that antidepressants prevent suicide is hard to find. A meta-analysis of data on the SSRI fluoxetine, funded by its manufacturer, found no evidence that suicidal acts were less frequent among adults taking antidepressants; the pooled incidences were 0.3% for fluoxetine, 0.2% for placebo, and 0.4% for tricyclics.14 In the most comprehensive synthesis of data from randomised trials, Khan and colleagues found no evidence of a beneficial effect of antidepressants on suicide.15 These findings are difficult to interpret as this was not a formal meta-analysis and relative risks were not derived separately for each trial on an intention to treat basis.
Suicide is rare, even among people with depression.16 Thus, most clinical trials have insufficient power to provide clear evidence on the effect of antidepressants on suicide.
Time trends
In the absence of clear evidence from clinical trials, researchers have investigated whether rises in antidepressant prescribing are associated with reductions in population suicide rates.2-6,17-19 With some exceptions,3,17,18 such studies conclude that recent rises in prescribing have contributed to falls in suicides. Interpretation of these findings is not straightforward. A range of factors influence population suicide rates.19 It is therefore challenging to distinguish the discrete effects of increased antidepressant prescribing from changes in other risk factors.
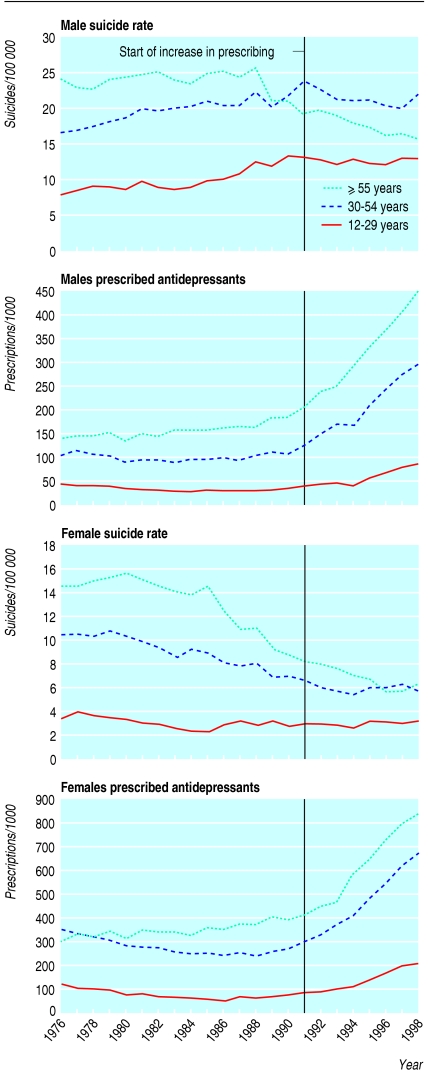
Furthermore, declining overall suicide trends may mask rises in some age and sex groups.19 In Australia, recent rises in antidepressant prescribing were associated with falls in suicide among some age and sex groups but increases in others.4 In Britain, declines in suicide preceded increases in prescribing (see fig A on bmj.com) and rises in antidepressant prescribing since 1991 in different age and sex groups do not consistently coincide with clear changes in previous suicide trends (fig 1). The levelling out of suicide trends in young men is probably due to a fall in suicide by self poisoning with car exhaust because of reductions in the carbon monoxide content of exhaust gases.20
Fig 1.
Trends in suicide and undetermined death rates (England and Wales) and prescribing of antidepressants (United Kingdom) by age and sex
Toxicity
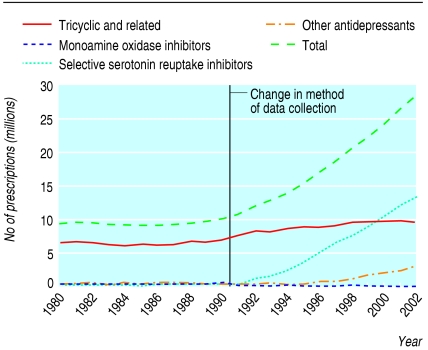
The possible benefits of increases in SSRI prescribing are not limited to their effect on depression. Self poisoning accounts for around a quarter of suicides in England; 20% of these deaths are antidepressant overdoses.21 Tricyclic antidepressants are considerably more toxic in overdose than SSRIs.21 Consequently, it has been estimated that a switch from tricyclics to SSRIs as first line treatment for depression could prevent 300-450 overdose deaths a year through restricting access to the more toxic antidepressants.22 Of note, increased SSRI prescribing has not been accompanied by a fall in use of tricyclics (fig 2).
Fig 2.
Trends in the number of antidepressant prescriptions issued 1980-2002, England
Do antidepressants increase the risk of suicide?
Soon after the launch of fluoxetine, the most commonly prescribed SSRI, a series of reports were published suggesting worsening of depression and emergence of suicidal thoughts in some people.23,24 The issue has been hotly debated.7,8 Disentangling the evidence is problematic as much of the research is sponsored by the pharmaceutical industry.25 Review of data from paediatric trials of SSRIs shows that published findings present a more favourable risk-benefit profile than unpublished trials sponsored by industry.12
Table 1 summarises the evidence from clinical trials on the adverse effects of SSRIs on suicidal behaviour in children, abstracted from information recently released by the Medicines and Healthcare Products Regulatory Agency.26 No suicides occurred in these trials. The pooled estimate of increased risk of suicidal thoughts or behaviour from these data is 1.66 (95% credibility interval 0.83 to 3.50). Interpretation of this apparent increase in risk is problematic as people taking SSRIs may be more likely to report adverse effects, perhaps because the drugs could have a disinhibiting effect. In addition, response to treatment may lead to reactivation among people whose depression previously prevented them from acting on suicidal impulses.27 Furthermore, any increased risk may be counterbalanced by a longer term reduction in suicidal behaviour; such benefits would not detected in the trials as they generally lasted 10 weeks or less, whereas the mean duration of treatment in clinical practice is three to four months.28
Table 1.
Risk of suicidal behaviour associated with use of SSRIs to treat depression in children and adolescents26
| Drug | Duration of trial(s) (weeks) | Adverse outcomes (drugv placebo)* | Odds ratio (95% CI) |
|---|---|---|---|
| Fluoxetine | 8 | Suicide attempts: 2.4% (6/249) v 1.9% (4/209) | 1.3 (0.4 to 4.4) |
| Sertraline | 10 | Suicide related events (includes suicidal thoughts): 2.7% (5/189) v placebo: 1.1% (2/184) | 2.4 (0.5 to 12.4) |
| Citalopram | 8-10 | Self harm: 8.0% (17/213) v 4.9% (10/205) | 1.6 (0.8 to 3.5) |
| Paroxetine | 8-12 | “Possibly related to suicidality”: 3.7% (14/378) v 2.5% (7/285) | 1.5 (0.6 to 3.7) |
| Pooled estimate | — | — | 1.66 (0.83 to 3.5)† |
Risks in relation to specific drugs were pooled from up to three trials. When data were presented separately we focused on risk in relation to self harm rather than suicidal thoughts.
Pooled estimates derived from bayesian random effects model.
Reassuringly, time trends for suicide (England and Wales)29 and non-fatal self harm (Oxford)30 in children and adolescents provide no consistent evidence of adverse trends paralleling increased prescribing in the 1990s, although there is some evidence of a rise in non-fatal self harm in young females. Furthermore, in the United States, recent research suggests that areas with the largest increases in antidepressant prescribing to 10-19 year olds experienced the greatest falls in suicide.6
Modelling the effect
There are two reasons why an adverse effect of antidepressants on suicide risk may have been overlooked in adult clinical trials. Firstly, self harm, and fatal self harm in particular, is relatively rare, and most clinical trials lack power to detect any increased risk. Secondly, as it seems counterintuitive that treatments for depression might increase suicide risk, the possibility may not have been specifically investigated in the clinical trials. The increased risk in children may have been detected either because of the increased prevalence of suicidal thoughts and self harm in young people (giving greater power) or because the absence of beneficial effects12 meant that adverse effects dominated the clinical picture.
If rare adverse effects of antidepressants on suicide exist, recent large scale increases in prescribing might be expected to affect suicide trends. But, as detailed above, recent suicide trends have generally been favourable, and so it is likely either that benefits outweigh the risks in adults or that any excess risk is small. Nevertheless, antidepressants may have precipitated some suicides in susceptible individuals, and it is important to estimate the number of such deaths. Table 2 outlines a model to estimate the number of excess deaths that may have occurred in 2002 compared with 1991 as a result of their increased use in England.
Table 2.
Model of possible excess suicides in 2002 compared to 1991 as a result of increased antidepressant prescribing (assumes findings from paediatric trials apply to adults and additional assumptions listed in text)
| Total | Male | Female | |
|---|---|---|---|
| No of extra antidepressant prescriptions issued in England in 2002 compared with 1991 (Department of Health)* | 17 386 000 | 5 795 000 | 11 591 000 |
| Additional person years exposed to antidepresants in 2002 compared to 1991† | 1 381 000 | 460 000 | 921 000 |
| Suicide rate in primary care treated depression (based on mean one year follow up)16‡ | 85/100 000/year | 127.5/100 000/year | 42.5/100 000/year |
| No of suicides among people receiving antidepressants§ | 586 | 391 | |
| No of excess suicides¶ | 586−(586/1.66)=233 | 391−(391/1.66)=155 |
Figures for males and females based on assumption that ratio of males:females prescribed antidepressants is 1:2.1
Assumes mean duration of antidepressant prescription is 29 days31 and all dispensed prescriptions are taken in their entirety by patients (No of extra prescriptions×29/365).
Assuming ratio of male:female suicide rates among people taking antidepressants is the same as that for general population suicide rates: 3:1.w1 This is in keeping with the relative risk of suicide of 2.8 in males receiving antidepressants compared with females in Jick et al.16
Additional person years of prescriptions×annual suicide rate.
Assuming relative risk associated with antidepressant prescribing is 1.66 (see table 1).
The model is based on the worst case scenario that the findings in relation to non-fatal self harm in paediatric trials are applicable to suicide deaths in adults. Under the model's assumptions (see bmj.com) an excess of 388 suicides (95% credibility interval-202 to 704) (233 men and 155 women) may have occurred in 2002 compared with 1991 as a result of increased anti-depressant prescribing. This is equivalent to an annual increase of around 35 suicides since 1991 (0.8% of the roughly 4500 annual suicides in England). Such a small increase may have been masked by other favourable influences on suicide.
The credibility intervals of our estimated increase in suicides (-202 to 704) include the possibility of a null or beneficial effect of SSRIs. Furthermore, some of our model assumptions are likely to result in us overestimating possible SSRI associated suicides. Firstly, there is no evidence that the findings from the paediatric trials can be extrapolated to adults, nor indeed that the strength of associations are the same for fatal and non-fatal self harm. Furthermore, the relative risk we used in our main model is based on findings from trials generally lasting 10 weeks or less, whereas the recommended duration of treatment is six months or more.32 Any increased suicide risk early in treatment may be offset by longer term improvements in suicide risk.
Secondly, we will have overestimated person time at risk because not all dispensed prescriptions are used and we have not taken account of the fact that (any) antidepressant associated increased risk of suicide may be concentrated in the early weeks of treatment. A sizeable proportion of people prescribed the drugs are long term users or have been taking antidepressants for two months or more and may therefore not be at risk of side effects.
Lastly, we assumed that suicide rates among those receiving antidepressants in 2002 are similar to those in the late 1980s and early 1990s.16 Recent increases in prescribing are likely to have occurred among people with less severe depressive illness and therefore a lower absolute suicide risk. The balance of risk and benefits may be different in this patient group. Our estimate of suicide rates among those treated with antidepressants is, however, some five times lower than that reported in one study.15 A sensitivity analysis of our model assumptions is presented on bmj.com.
Conclusions
There is no strong evidence that increases in antidepressant prescribing lie behind recent reductions in population suicides. Furthermore, data from paediatric trials suggest that SSRIs are associated with an increased risk of suicidal behaviour and most SSRIs seem to be ineffective for childhood depression. However, current concerns about the safety of SSRIs come from clinical trials both of too short duration (< 10 weeks) to identify longer term beneficial effects and are carried out in children and adolescents, among whom suicide is rare.
From the population perspective, the balance sheet of risks and benefits of SSRIs is unclear. Any antidepressant induced suicides may be offset by the beneficial effects of antidepressants on depression and long term suicide risk associated with untreated depression. The low toxicity of SSRIs in overdose will have prevented some suicides. The balance of risks and benefits may vary depending on an individual's underlying suicide risk. For patients with conditions that have a high risk of suicide, such as severe depression,33 the risk-benefit balance may be more favourable than for patients with conditions such as anxiety and mild depression, in which suicide is rare. It is in these lower risk conditions, however, that much of the recent rise in prescribing has probably occurred.
Depression is a common and disabling condition, and so the safety of drugs used in its management is crucial. Future trials of antidepressants should be of sufficient duration to detect longer term benefits of this class of drug and balance these against possible risks. They should also systematically collect data on suicidal thoughts and behaviour. Long term studies are required to assess the effect on population health of recent rises in antidepressant prescribing.
Supplementary Material
 A figure showing trends in suicide and prescribing plus further data on the model are on bmj.com
A figure showing trends in suicide and prescribing plus further data on the model are on bmj.com
We thank Ian Weller and George Davey Smith for critical comments on the paper, IMS Health for the age specific prescribing data, the Department of Health for prescribing data, Lesley Wise for critical comments and helpful discussions on our model, and Shahrul Mt Isa, for help with calculating the confidence intervals.
Contributors and sources: DG has a longstanding research interest in the epidemiology and prevention of suicide. DA has a longstanding research interest in drug safety and bayesian modelling. The idea for the paper arose from their joint work on the Medicines and Healthcare Products Regulatory Agency's Expert Working Group on SSRIs. DG wrote the first draft of the article and undertook literature reviews; DA performed the statistical modelling. Both authors contributed to the final content of the paper and will act as guarantors.
Competing interests: DG and DA are members of the Medicines and Healthcare Products Regulatory Agency's expert working group on the safety of SSRIs and DA is a member of the Committee on Safety of Medicines. We act as independent advisers, receiving travel expenses and a small fee for attending meetings and reading materials in preparation for the meeting. DA has spoken on the methodology of adverse drugs reactions in HIV at a scientific meeting attended by several pharmaceutical companies, and sponsored by GlaxoSmithKline. An honorarium was paid to her department.
References
- 1.Middleton N, Gunnell D, Whitley E, Dorling D, Frankel S. Secular trends in antidepressant prescribing in the UK, 1975-1998. J Public Health Med 2001;23: 262-7. [DOI] [PubMed] [Google Scholar]
- 2.Isacsson G. Suicide prevention—a medical breakthrough? Acta Psychiatr Scand 2000;102: 113-7. [DOI] [PubMed] [Google Scholar]
- 3.Barbui C, Campomori A, D'Avanzo B, Negri E, Garattini S. Antidepressant drug use in Italy since the introduction of SSRIs: national trends, regional differences and impact on suicide rates. Soc Psychiatry Psychiatr Epidemiol 1999;34: 152-6. [DOI] [PubMed] [Google Scholar]
- 4.Hall WD, Mant A, Mitchell PB, Rendle VA, Hickie IB, McManus P. Association between antidepressant prescribing and suicide in Australia, 1991-2000: trend analysis. BMJ 2003;326: 1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rihmer Z, Belso N, Kalmar S. Antidepressants and suicide prevention in Hungary. Acta Psychiatr Scand 2001;103: 238-9. [DOI] [PubMed] [Google Scholar]
- 6.Olfson M, Shaffer D, Marcus SC, Greenberg T. Relationship between antidepressant medication treatment and suicide in adolescents. Arch Gen Psychiatry 2003;60: 978-82. [DOI] [PubMed] [Google Scholar]
- 7.Healy D. Lines of evidence on the risks of suicide with selective serotonin reuptake inhibitors. Psychother Psychosom 2003;72: 71-9. [DOI] [PubMed] [Google Scholar]
- 8.Medawar C, Herxheimer A, Bell A, Jofre S. Paroxetine, Panorama and user reporting of ADRs: Consumer intelligence matters in clinical practice and post-marketing drug surveillance. Int J Risk Saf Med 2002;15: 161-9. [Google Scholar]
- 9.SSRI and venlafaxine use in children. Curr Prob Pharmacovig 2003;29: 4. [Google Scholar]
- 10.Freemantle N, Long A, Mason J, Sheldon T, Song F, Watson P, et al. Effective health care: the treatment of depression in primary care. Leeds: University of Leeds; Department of Health, 1993.
- 11.MacGillivray S, Arroll B, Hatcher S, Ogston S, Reid I, Sullivan F et al. Efficacy and tolerability of selective serotonin reuptake inhibitors compared with tricyclic antidepressants in depression treated in primary care: systematic review and meta-analysis. BMJ 2003;326: 1014-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whittington CJ, Kendall T, Fonagy P, Cottrell D, Cotgrove A, Boddington E. Selective serotonin reuptake inhibitors in childhood depression: systematic review of published versus unpublished data. Lancet 2004;363: 1341-5. [DOI] [PubMed] [Google Scholar]
- 13.Rutz W, von Knorring L, Walinder J. Long-term effects of an educational program for general practitioners given by the Swedish committee for the prevention and treatment of depression. Acta Psychiatr Scand 1992;85: 83-8. [DOI] [PubMed] [Google Scholar]
- 14.Beasley CM Jr, Dornseif BE, Bosomworth JC, Sayler ME, Rampey AH, Heiligenstein JH. Fluoxetine and suicide: a meta-analysis of controlled trials of treatment for depression. BMJ 1991;303: 685-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khan A, Khan S, Kolts R, Brown WA. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry 2003;160: 790-2. [DOI] [PubMed] [Google Scholar]
- 16.Jick SS, Dean AD, Jick H. Antidepressants and suicide. BMJ 1995;310: 215-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oravecz R, Czigler B, Leskosek F. Correlation between suicide rate and antidepressant use in Slovenia. Arch Suicide Res 2003;7: 279-85. [Google Scholar]
- 18.Helgason T, Tomasson H, Zoega T. Antidepressants and public health in Iceland. Time series analysis of national data. Br J Psychiatry 2004;184: 157-62. [DOI] [PubMed] [Google Scholar]
- 19.Gunnell D, Middleton N, Whitley E, Dorling D, Frankel S. Why are suicide rates rising in young men but falling in the elderly?—a time-series analysis of trends in England and Wales 1950-1998. Soc Sci Med 2003;57: 595-611. [DOI] [PubMed] [Google Scholar]
- 20.Amos T, Appleby L, Kiernan K. Changes in rates of suicide by car exhaust asphyxiation in England and Wales. Psychol Med 2001;31: 935-9. [DOI] [PubMed] [Google Scholar]
- 21.Shah R, Uren Z, Baker A, Majeed A. Deaths from antidepressants in England and Wales 1993-1997: analysis of a new national database. Psychol Med 2001;31: 1203-10. [DOI] [PubMed] [Google Scholar]
- 22.Freemantle N, House A, Song F, Mason JM, Sheldon TA. Prescribing selective serotonin reuptake inhibitors as strategy for prevention of suicide. BMJ 1994;309: 249-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Teicher MH, Glod C, Cole JO. Emergence of intense suicidal preoccupation during fluoxetine treatment. Am J Psychiatry 1990;147: 207-10. [DOI] [PubMed] [Google Scholar]
- 24.Masand P, Gupta S, Dewan M. Suicidal ideation related to fluoxetine treatment. N Engl J Med 1991;324: 420. [DOI] [PubMed] [Google Scholar]
- 25.Als-Nielsen B, Chen W, Gluud C, Kjaergard LL. Association of funding and conclusions in randomized drug trials. JAMA 2003;290: 921-6. [DOI] [PubMed] [Google Scholar]
- 26.Medicines and Healthcare Products Regulatory Agency. Selective serotonin reuptake inhibitors (SSRIs): overview of regulatory status and CSM advice relating to major depressive disorder (MDD) in children and adolescents including a summary of available safety and efficacy data. http://medicines.mhra.gov.uk/ourwork/monitorsafequalmed/safetymessages/ssrioverview_101203.htm (accessed 16 May 2004).
- 27.Nutt D. Death and dependence: current controversies over the selective serotonin reuptake inhibitors. J Psychopharmacol 2003;17: 355-64. [DOI] [PubMed] [Google Scholar]
- 28.MacKay FR, Dunn NR, Martin RM, Pearce GL, Freemantle SN, Mann RD. Newer antidepressants: a comparison of tolerability in general practice. Br J Gen Pract 1999;49: 892-6. [PMC free article] [PubMed] [Google Scholar]
- 29.McClure GMG. Suicide in children and adolescents in England and Wales 1970-1998. Br J Psychiatry 2001;178: 469-74. [DOI] [PubMed] [Google Scholar]
- 30.Hawton K, Hall S, Simkin S, Bale L, Bond A, Codd S, et al. Deliberate selfharm in adolescents: a study of characteristics and trends in Oxford, 1990-2000. J Child Psychol Psychiatry 2003;44: 1191-8. [DOI] [PubMed] [Google Scholar]
- 31.Donoghue JM, Tylee A. The treatment of depression: prescribing patterns of antidepressants in primary care in the UK. Br J Psychiatry 1996;168: 164-8. [DOI] [PubMed] [Google Scholar]
- 32.Paykel ES, Priest RG. Recognition and management of depression in general practice: consensus statement. BMJ 1992;305: 1198-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry 1998;173: 11-53. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.