Abstract
Introduction
Transcutaneous CO 2 (PtCO 2) is a continuous and non-invasive measure recommended by scientific societies in the management of respiratory distress. The objective of this study is to evaluate the correlation between PtCO 2 and blood pressure of CO 2 (PaCO 2) by blood gas analysis in emergency patients with dyspnoea and to determine the factors that interfere in this correlation.
Methods
From January to June 2014, all patients admitted to resuscitation room of the emergency department targeted for arterial blood gases were included prospectively. A sensor measuring the PtCO 2 was attached to the ear lobe of the patient before the gas analysis. Anamnesis, clinical and laboratory parameters were identified.
Results
90 patients with dyspnoea were included (with 104 pairs of measurements), the median age was 79 years [69-85]. The correlation between PtCO 2 and PaCO 2 was R 2= 0.83 (p <0.001) but became lower for values of PaCO 2>60 mm Hg. The mean bias (±SD) between the two methods of measurement (Bland-Altman analysis) was -1.4 mm Hg (±7.7) with limits of agreement of -16.4 to 13.7 mm Hg. In univariate analysis, PaO 2 interfered in this correlation. After multivariate analysis, the temperature (OR = 3.01, 95% CI = 1.16-7.09) and the PaO 2 (OR = 1.22, 95% CI = 1.02-1.47) were found to be significant.
Conclusions
In patients admitted in emergency unit for acute respiratory failure, there is a significant correlation between PaCO 2 and PtCO 2, mainly for values below 60 mm Hg. The two limiting factors of use are hyperthermia and users training.
Keywords: Emergency service, Blood gas monitoring, Transcutaneous, Carbon dioxide, Partial pressure
Introduction
In patients with respiratory failure admitted to resuscitation room (RR), the monitoring of arterial blood gases is crucial for diagnosis and therapeutic guidance [1]. The gold standard remains the analysis of arterial blood gases. This implies an arterial puncture that it is invasive, time consuming and giving only punctual results [2,3]. In addition, pending the results of blood gas analysis does not allow for real-time adaptation of oxygen therapy and/or mechanical ventilation. Oxygen saturation by pulse oxymetry (SpO 2) is widely used as a surrogate of arterial oxygen saturation (SaO 2) [4]. In mechanically ventilated patients, end tidal CO 2 (EtCO 2) allows an indirect reliable continuous assessment of arterial PCO 2. In non-ventilated patients, assessment of EtCO 2 is more complex, less accurate and often impossible. The transcutaneous monitoring of the carbon dioxide (PtCO 2) could represent a good alternative for immediate and continuous assessment of PCO 2 in RR, especially in non-ventilated patients. The transcutaneous continuous monitoring of the carbon dioxide has been recently recommended [5,6]. In the specific setting of RR, PtCO 2 has been poorly studied. Numerous studies in infants [7,8] and adults [9-11] have found a good correlation between PaCO 2 and PtCO 2. The main objective of this study was to investigate the relationship between measures of PtCO 2 and PaCO 2 in resuscitation room patients admitted. The secondary objective was to determine the factors that may disrupt the link between these two parameters.
Patients and methods
Setting and study population
This single-center prospective observational study was conducted from January to June 2014 at the emergency department (ED) of Nîmes University Hospital. According to the French Law (Law 88-1138 relative to Biomedical Research of 20 December 1988 modified on 9 August 2004), this non-interventional study did not require approval by an ethics committee nor informed signed consent from patients. It was reviewed and approved by our Institutional Review Board (number: 13/06-02). Moreover, the present study was declared to and approved by the national commission for data processing and civil liberties. All patients provided written informed consent. All adult patients oriented in the RR and with an arterial blood gas during laboratory tests were likely to be included in the study. Exclusion criteria were the realization of venous blood gases and non-compliance of the study protocol (incorrect installation of the sensor or signal abnormality of the monitor or backup).
The PtCO 2 measurement was performed by a Stow-Severinghaus sensor (tc Sensor 92 by Radiometer™, Copenhagen, Denmark). The sensor was placed on the earlobe heating skin to a temperature of 44 ∘C resulting in a dilatation of capillary bed that allows a 20 times faster diffusion of gases (CO 2 and O 2) from the skin to the sensor [12]. On the sensor, carbon dioxide reacts with water to form carbonic acid which dissociates into H+ and HCO3 thereby changing pH values. These pH changes are translated into PtCO 2 value through the Henderson-Hasselbalch formula [13].
Before the study, medical and paramedical staff were trained in the operation and maintenance of the monitor PtCO 2 type TCM TOSCA monitor (Radiometer™, Copenhagen, Denmark). Patients in whom RR admission was required were included. The PtCO 2 sensor was attached to the ear lobe of the patient allowing continuous measurement of PtCO 2. Arterial blood gases and the usual additional assessments were performed at the same time. The medical team was blinded for the value of PtCO 2.
Medical patient data were collected and computerized after initial collection on paper case report form (CRF). Blood pressure, heart rate and respiratory rate, blood oxygen saturation, Glasgow coma scale, temperature, time for completion of the arterial blood gases, catecholamines use, NIV or tracheal intubation were recorded by the attending physician. Epidemiological characteristics of patients such as admission modalities, length of hospital stay and biological data were collected on the CRF. PtCO 2 values were automatically saved every ten seconds by the monitor PtCO 2. The primary outcome variable was concordance between the simultaneous PaCO 2 and PtCO 2 values. Sample size calculation was based on the anticipated variation in the differences between the measurements and the required precision. Using previous study [14] for an estimate of the variation between the differences, a sample size of 50 patients gives a precision of ± 0.19 kPa in the limits of agreement. The secondary outcome was to determine the factors that interfere in this correlation.
Statistical analysis
Patient characteristics are described using qualitative variables (using frequencies and percentages) and quantitative variables (using means and standard deviation or median with interquartile depending on type of distribution). The concordance between PtCO 2 and PaCO 2 was evaluated by linear regression (correlation coefficients) and Bland-Altman analysis, which determined bias, precision, and agreement of PtCO 2 and PaCO 2, taking the automated analysis in the laboratory as the reference. The Pearson correlation coefficient was used to demonstrate the presence or absence of a relationship between PtCO 2 and PaCO 2. Relationships between measurement differences (|PaCO2-PtCO 2|) and patient characteristics were investigated by regression analysis. Variables related to the difference between PtCO 2 and PaCO 2 in the univariable analysis (defined by p <0.10, forward selection) were further analysed in a multivariable model (analysis of covariance). We introduced in this model PaCO 2 but did not introduce pH and PtCO 2 to avoid a collinear bias. Overall model fit was assessed using the Hosmer-Lemeshow test. All statistical tests were 2-sided. A P value less than 0.05 was considered significant for all analyses.
Analyses were performed with the use of R 3.0.2 (R Core Team 2013, R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria). The authors had full access to and take full responsibility for the integrity of the data.
Results
Between January 2014 and June 2014, 102 patients were screened. Only 90 patients were analyzed with 104 PtCO 2 values (Figure 1). Table 1 shows the characteristics of the 104 measurements. After linear regression analysis of 104 couples, there was a significant correlation between PaCO 2 and PtCO 2 with R 2=0.83(P<0.001) (Figure 2). The linear regression equation between the two variables was PaCO 2= 0.81 × + 10.86 PtCO 2. The Bland-Altman (12) is shown in Figure 3. The mean bias was -1.4 mm Hg (±7.7) and limits of agreement (bias ±1.96 SD) between the two techniques were -16.4 mm Hg and 13.7 mm Hg. The Pearson’s correlation coefficient was 0.94 (95% CI = 0.87-0.94, P <0.001).
Figure 1.
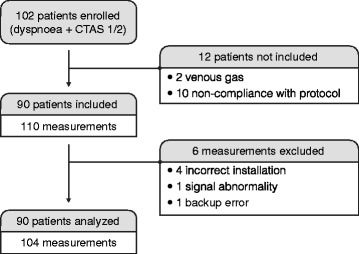
Flow diagram.
Table 1.
Patient characteristics
| Male sex, no. (%) | 51 (57) |
|---|---|
| Age, mean (± SD) - year | 76 (15) |
| Past medical history, no. (%) | |
| Acute pulmonary edema | 27 (29) |
| Chronic obstructive pulmonary disease | 27 (29) |
| Ischemic heart disease | 21 (23) |
| Home oxygen | 16 (17) |
| Clinical data at admission, median (IQR) | |
| Heart rate - beats/min. | 94 (80-110) |
| Systolic blood pressure - mm Hg | 122 (106-144) |
| Diastolic blood pressure - mm Hg | 69 (60-78) |
| Respiratory rate - breaths/min. | 24 (19-28) |
| Glasgow coma scale | 15 (14-15) |
| Temperature - ∘C | 37.0 (36.2-37.6) |
| Laboratory values, median (IQR) | |
| PaCO 2 - mm Hg | 46.2 (37.6-66.8) |
| PtCO 2 - mm Hg | 47.2 (42.1-60.0) |
| PaO 2 - mm Hg | 73.5 (63.0-89.0) |
| pH | 7.37 (7.30-7.43) |
| HCO 3 - mEq/L | 26.0 (22.8-29.7) |
| Base excess - mmol/L | 1.9 (-1.9-5.8) |
| Lactate - mmol/L | 1.3 (0.7-2.2) |
| Hemoglobin - g/dL | 12.3 (10.9-13.8) |
| White blood cells - G/L | 12.4 (7.9-15.5) |
| C-reactive protein | 41 (8-122) |
| Glycemia - g/L | 1.4 (1.2-1.7) |
| Brain natriuretic peptide - ng/L | 1704 (579-6200) |
| Diagnosis, no. (%) | |
| Heart failure | 25 (27) |
| COPD | 14 (15) |
| Pneumonia | 42 (46) |
| Pulmonary embolism | 5 (5) |
| Outcome, no. (%) | |
| Noninvasive ventilation required | 41 (45) |
| Intubation required | 4 (4) |
| Admitted to hospital | 61 (66) |
| Admitted to ICU | 19 (21) |
| Discharged from ED | 10 (11) |
| Death at the ED | 2 (2) |
| Inpatient mortality | 9 (10) |
COPD: Chronic obstructive pulmonary disease; ED: Emergency department; ICU: Intensive care unit; IQR: Interquartile range; PaCO 2: Partial pressure of carbon dioxide in the blood; PtCO 2: Transcutaneous partial pressure of carbon dioxide in the blood; PaO 2: Partial pressure of dioxygen in the blood.
Figure 2.
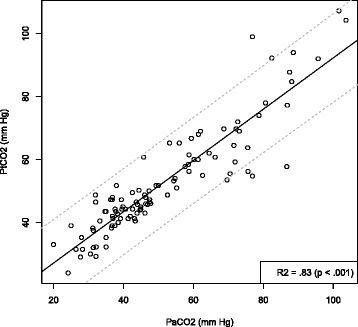
Linear regression between transcutaneous PtcCO 2 and PaCO 2. Regression line is the continuous line, the dotted lines show the 95% confidence interval.
Figure 3.
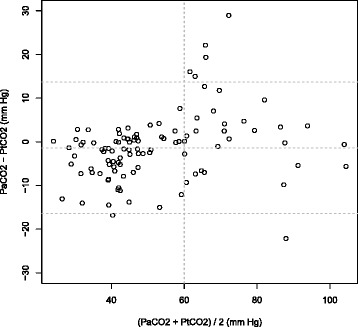
Bland-Altman representation of comparison analysis between PaCO 2 and PtcCO 2 vs means of paired measurements.
For group with PaC02 < 60 mmH, R 2=0.70 (P <0.001) and the mean bias was -3.5 mm Hg (±5.0). For group with PaC02 > 60 mmH, R 2 = 0.57 (P <0.001) and the mean bias was 4.1 mm Hg (±10.2).
In univariate analysis, the only factor associated with a difference between PaCO 2 and PtCO 2 was PaO 2 (Table 2). In multivariate analysis with three explanatory variables (PaCO 2, PaO 2, temperature), we found the temperature and the PaO 2 to be significantly associated with a high difference between PaCO 2 and PtCO 2 (Table 2). In this model, 11 observations were deleted because of missing data. This model has a nonsignificant Hosmer-Lemeshow chi-square goodness-of-fit statistic. The higher the temperature of the patient, the higher the difference between PaCO 2 and PtCO 2 was significant (Figure 4).
Table 2.
Relationships between measurement differences (|PaCO 2 -PtCO 2 |) and patient characteristics, univariate and multivariate analysis (ANCOVA)
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Variable | OR [95% CI] | P-value | OR [95% CI] | P-value |
| Sex | 1.61 [0.18-14.25] | 0.66 | ||
| Past medical history | ||||
| Acute pulmonary edema | 0.29 [0.03-2.96] | 0.29 | ||
| COPD | 0.60 [0.06-6.18] | 0.67 | ||
| Ischemic heart disease | 0.75 [0.06-8.91] | 0.82 | ||
| Home oxygen | 1.01 [0.06-16.77] | 0.99 | ||
| Heart rate | 0.98 [0.94-1.03] | 0.40 | ||
| Systolic blood pressure | 1.01 [0.97-1.05] | 0.60 | ||
| Diastolic blood pressure | 0.97 [0.91-1.03] | 0.33 | ||
| Respiratory rate | 1.01 [0.88-1.18] | 0.85 | ||
| Temperature | 2.45 [0.93-6.49] | 0.07 | 3.01 [1.16-7.80] | 0.03 |
| PaCO 2 | 1.05 [1.00-1.12] | 0.06 | 1.06 [1.00-1.12] | 0.05 |
| PtCO 2 | 1.06 [1.00-1.13] | 0.06 | ||
| PaO 2 | 1.21 [1.01-1.45] | 0.04 | 1.22 [1.02-1.47] | 0.03 |
| HCO 3 | 0.96 [0.80-1.15] | 0.64 | ||
| Base excess | 0.96 [0.82-1.12] | 0.60 | ||
| Lactate | 1.44 [0.43-4.79] | 0.54 | ||
| Hemoglobin | 1.20 [0.74-1.95] | 0.45 | ||
| White blood cells | 0.91 [0.74-1.12] | 0.38 | ||
| C-reactive protein | 1.00 [0.99-1.01] | 0.72 | ||
| Glycemia | 4.70 [0.62-35.58] | 0.13 | ||
| Brain natriuretic peptide | 1.00 [1.00-1.00] | 0.82 | ||
ANCOVA: Analysis of covariance; COPD: Chronic obstructive pulmonary disease; CI: Confidence interval; PaCO 2: Partial pressure of carbon dioxide in the blood; PtCO 2: Transcutaneous partial pressure of carbon dioxide in the blood; PaO 2: Partial pressure of dioxygen in the blood.
Figure 4.
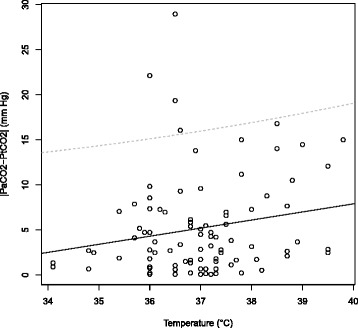
Linear regression between temperature and difference between PaCO 2 and PtCO 2 (|PaCO 2-PtCO 2|). Regression line is the continuous line, the dotted lines show the 95% confidence interval.
Discussion
To our knowledge, this study is the largest cohort of PtCO 2 measurements in ED. The mean bias was -1.4 mm Hg (±7.7) and the limits of agreement (bias ±1.96 SD) between the two techniques were -16.4 mm Hg and 13.7 mm Hg. There was a significant correlation between PaCO 2 and PtCO 2 (R 2=0.83, p <0.001). This value is comparable to what was shown in intensive care (R 2=0.86, p <0.01) [9] while other studies have found better correlation (R 2 coefficient between 0.91 and 0.99 [15-17]). First, this difference can be explained by the recruitment of our patients, performed only in RR with acute respiratory failure. Because a majority of our patients were non-intubated, our results highlight the feasibility and the potential interest of PtCO2 as EtCO2 cannot easily be monitored in non-intubated patients. Indeed, the extreme values of PaCO 2 and high PaCO 2 values were reported as possibly interfering in the correlation-PtCO 2 PaCO 2 [9,18-20]. Second, this difference may result from the use of the device by a large number of doctors. Calibration, sensor placement and latency to reach the plateau value of PtCO 2 may differ from one doctor to another. This may lead to poorer reproducibility; some operators use the apparatus less frequently. However, this reflects our center daily practice and occurs when there is any change of material. Third, our population was more likely to have breathing disorders and therefore agitation and/or sweating leading to mobilization of the sensor which may disrupt the measurement. Our study found a value PtCO 2 generally greater than the value of PaCO 2 measured. Indeed, linear regression equation is PtCO 2 = 0.81 × + 10.86 PaCO 2. This overestimation is in accordance with available literature [9,21,22]. This overestimation may have implications for patients requiring non-invasive ventilation and with no blood gas reference. Thus, the recommendations highlight the need to conduct a gas analysis to verify the correlation between the PaCO 2 and PtCO 2 [5]. This parameter is particularly important to consider given that the analysis of Bland-Altman reveals a poorer correlation values PtCO 2>60 mm Hg. The value of the mean bias reported in our study corresponds to those found in the literature (-1.4 to 4.6 mm Hg) [15,23,24]. This dispersion of the correlation for high values of PaCO 2 was previously reported. The accuracy of PtCO 2 seems to be restricted to patients with PaCO 2 values of <56 mm Hg [25]. One explanation for this poor correlation with the clinical manifestations of hypercapnia (excessive sweating and vasodilatation) leading to a lower diffusion of carbon dioxide [25]. In our study, after multivariate analysis, only the temperature was associated with a poor correlation between PaCO 2 and PtCO 2 (HR = 1.15 [0.2-2.10], p = 0.018). The notion that the temperature can influence the correlation had been raised by Rodriguez et al. [26]. The linear regression analysis reveals that the higher is the body temperature, the greater the difference between the PaCO 2 and PtCO 2 is important. This poor correlation can be explained by the fact that the higher the patient’s temperature, the greater the difference between the temperature sensor (44 ∘C) is low, resulting in small changes in local perfusion and thus altering the local production of CO 2. This hypothesis follows directly from the operating principle of the sensor [5]. It could also be hypothesized that a high body temperature promotes sweating and vasodilatation making far more difficult sensor measurement. Finally, a low blood pressure can also be a cause a poor correlation [27]. This hypothesis cannot be confirmed by the present data, has few patients has shock criteria. Similarly, the assumption that the pH may explain poor correlation [20] is not confirmed in our study in the multivariate analysis.
Limitations
First, our study has few patients with hemodynamic instability requiring the establishment of intravenous fluids or vasopressor support. It is therefore difficult to conclude to any contribution from the low-speed on the correlation between PaCO 2 and PtCO 2. Several studies have shown that the correlation between the PtCO 2 PaCO 2 and is not affected by the use of catecholamine but by dermal vasoconstriction secondary to a state of shock [9,22,26]. Secondly, body mass index (BMI) has not been measured over the study. Several studies reported conflicting conclusions regarding the influence of the thickness of the skin, indirectly estimated by BMI, on the diffusion of CO 2 to the skin and therefore the values of PcCO 2 [9,22,24,25]. Third, the majority of patients had received only blood gases during the treatment, not for obtaining intra-individual correlations between different values PtCO 2 and PaCO 2. This analysis was important to be able to easily predict PaCO 2 values from continuous measurement of PtCO 2 in patients requiring several hours of surveillance [26,28].
Conclusions
In patients admitted in emergency unit for acute respiratory failure, there is a significant correlation between PaCO 2 and PtCO 2, mainly for values below 60 mm Hg. The two limiting factors of use are hyperthermia and users training.
Key messages
In patients admitted in emergency unit for acute respiratory failure, there is a significant correlation between PaCO 2 and PtCO 2.
This correlation is comparable to what was shown in intensive care.
The two limiting factors of use are hyperthermia and users training.
Acknowledgements
The authors acknowledge all the emergency physicians at Nîmes University Hospital who recruited the patients, the residents who helped in this process, and other members of our research team for their help.
Abbreviations
- ANCOVA
Analysis of covariance
- BMI
Body mass index
- CI
Confidence interval
- COPD
Chronic obstructive pulmonary disease
- CRF
Case report form
- ED
Emergency department
- EtCO 2
End tidal CO 2
- ICU
Intensive care unit
- IQR
Interquartile range
- OR
Odds ratio
- RR
Resuscitation room
- PaCO 2
Partial pressure of carbon dioxide in the blood
- PtCO 2
Transcutaneous partial pressure of carbon dioxide in the blood
- PaO 2
Partial pressure of dioxygen in the blood
- SaO 2
Arterial oxygen saturation
- SpO 2
Oxygen saturation by pulse oxymetry
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
XB, PGC, LP and MR conceived the study and wrote the manuscript. JELC was the director of this research project and participated to the writing of this manuscript. LP and MR performed the exams. PGC was the responsible of the statistical analysis. XB, PGC, LP, MR, RGG, CR, PR, MS, LM and JELC have been involved in drafting the manuscript or revising it critically for important intellectual content. XB, PGC, LP, MR, RGG, CR, PR, MS, LM and JELC have given final approval of the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Contributor Information
Xavier Bobbia, Email: xavier.bobbia@gmail.com.
Pierre-Géraud Claret, Email: pierre.geraud.claret@gmail.com.
Ludovic Palmier, Email: lpalmier@hotmail.fr.
Michaël Robert, Email: robertmichael34000@gmail.com.
Romain Genre Grandpierre, Email: romainsbs@hotmail.com.
Claire Roger, Email: clairepenetrat@hotmail.com.
Patrick Ray, Email: patrick.ray@tnn.aphp.fr.
Mustapha Sebbane, Email: m-sebbane@chu-montpellier.fr.
Laurent Muller, Email: laurent.muller27@orange.fr.
Jean-Emmanuel de La Coussaye, Email: jean.emmanuel.delacoussaye@chu-nimes.fr.
References
- 1.Rady MY. Bench-to-bedside review: Resuscitation in the emergency department. Crit Care. 2005;9(2):170–6. doi: 10.1186/cc2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burri E, Potocki M, Drexler B, Schuetz P, Mebazaa A, Ahlfeld U, et al. Value of arterial blood gas analysis in patients with acute dyspnea: an observational study. Crit Care. 2011;15(3):R145. doi: 10.1186/cc10268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bobbia X, Grandpierre RG, Claret PG, Moreau A, Pommet S, Bonnec JM, et al. Ultrasound guidance for radial arterial puncture: a randomized controlled trial. Am J Emerg Med. 2013;31(5):810–5. doi: 10.1016/j.ajem.2013.01.029. [DOI] [PubMed] [Google Scholar]
- 4.Silversides JA, Ferguson ND. Clinical review: Acute respiratory distress syndrome - clinical ventilator management and adjunct therapy. Crit Care. 2013;17(2):225. doi: 10.1186/cc11867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Restrepo RD, Hirst KR, Wittnebel L, Wettstein R. AARC clinical practice guideline: transcutaneous monitoring of carbon dioxide and oxygen: 2012. Respir Care. 2012;57(11):1955–62. doi: 10.4187/respcare.02011. [DOI] [PubMed] [Google Scholar]
- 6.Brochard L, Martin GS, Blanch L, Pelosi P, Belda FJ, Jubran A et al. Clinical review: Respiratory monitoring in the ICU - a consensus of 16. Crit Care. 2012;16(2):219. doi: 10.1186/cc11146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monaco F, Nickerson BG, McQuitty JC. Continuous transcutaneous oxygen and carbon dioxide monitoring in the pediatric ICU. Crit Care Med. 1982;10(11):765–6. doi: 10.1097/00003246-198211000-00014. [DOI] [PubMed] [Google Scholar]
- 8.O’Connor TA, Grueber R. Transcutaneous measurement of carbon dioxide tension during long-distance transport of neonates receiving mechanical ventilation. J Perinatol. 1998;18(3):189–92. [PubMed] [Google Scholar]
- 9.Bendjelid K, Schütz N, Stotz M, Gerard I, Suter PM, Romand JA. Transcutaneous PCO2 monitoring in critically ill adults: clinical evaluation of a new sensor. Crit Care Med. 2005;33(10):2203–6. doi: 10.1097/01.CCM.0000181734.26070.26. [DOI] [PubMed] [Google Scholar]
- 10.Delerme S, Montout V, Goulet H, Arhan A, Le Saché F. Devilliers C, et al. Concordance between transcutaneous and arterial measurements of carbon dioxide in an ED. Am J Emerg Med. 2012;30(9):1872–6. doi: 10.1016/j.ajem.2012.03.033. [DOI] [PubMed] [Google Scholar]
- 11.Gancel PE, Roupie E, Guittet L, Laplume S, Terzi N. Accuracy of a transcutaneous carbon dioxide pressure monitoring device in emergency room patients with acute respiratory failure. Intensive Care Med. 2011;37(2):348–51. doi: 10.1007/s00134-010-2076-1. [DOI] [PubMed] [Google Scholar]
- 12.Severinghaus JW, Astrup P, Murray JF. Blood gas analysis and critical care medicine. Am J Respir Crit Care Med. 1998;157(4 Pt 2):S114–22. doi: 10.1164/ajrccm.157.4.nhlb1-9. [DOI] [PubMed] [Google Scholar]
- 13.Kellum JA. Determinants of blood pH in health and disease. Crit Care. 2000;4(1):6–14. doi: 10.1186/cc644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heuss LT, Chhajed PN, Schnieper P, Hirt T, Beglinger C. Combined pulse oximetry/cutaneous carbon dioxide tension monitoring during colonoscopies: pilot study with a smart ear clip. Digestion. 2004;70(3):152–8. doi: 10.1159/000081515. [DOI] [PubMed] [Google Scholar]
- 15.Storre JH, Steurer B, Kabitz HJ, Dreher M, Windisch W. Transcutaneous PCO2 monitoring during initiation of noninvasive ventilation. Chest. 2007;132(6):1810–6. doi: 10.1378/chest.07-1173. [DOI] [PubMed] [Google Scholar]
- 16.McVicar J, Eager R. Validation study of a transcutaneous carbon dioxide monitor in patients in the emergency department. Emerg Med J. 2009;26(5):344–6. doi: 10.1136/emj.2007.055715. [DOI] [PubMed] [Google Scholar]
- 17.Cox M, Kemp R, Anwar S, Athey V, Aung T, Moloney ED. Non-invasive monitoring of CO2 levels in patients using NIV for AECOPD. Thorax. 2006;61(4):363–4. doi: 10.1136/thx.2005.051664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McLellan PA, Goldstein RS, Ramcharan V, Rebuck AS. Transcutaneous carbon dioxide monitoring. Am Rev Respir Dis. 1981;124(2):199–201. doi: 10.1164/arrd.1981.124.2.199. [DOI] [PubMed] [Google Scholar]
- 19.Tobias JD. Transcutaneous carbon dioxide monitoring in infants and children. Paediatr Anaesth. 2009;19(5):434–44. doi: 10.1111/j.1460-9592.2009.02930.x. [DOI] [PubMed] [Google Scholar]
- 20.Versmold HT, Linderkamp O, Holzmann M, Strohhacker I, Riegel K. Transcutaneous monitoring of PO2 in newborn infants: where are the limits? Influence of blood pressure, blood volume, blood flow, viscosity, and acid base state. Birth Defects Orig Artic Ser. 1979;15(4):285–94. [PubMed] [Google Scholar]
- 21.Rosner V, Hannhart B, Chabot F, Polu JM. Validity of transcutaneous oxygen/carbon dioxide pressure measurement in the monitoring of mechanical ventilation in stable chronic respiratory failure. Eur Respir J. 1999;13(5):1044–7. doi: 10.1034/j.1399-3003.1999.13e18.x. [DOI] [PubMed] [Google Scholar]
- 22.Janssens JP, Howarth-Frey C, Chevrolet JC, Abajo B, Rochat T. Transcutaneous PCO2 to monitor noninvasive mechanical ventilation in adults: assessment of a new transcutaneous PCO2 device. Chest. 1998;113(3):768–73. doi: 10.1378/chest.113.3.768. [DOI] [PubMed] [Google Scholar]
- 23.Lang CJ. Apnea testing guided by continuous transcutaneous monitoring of partial pressure of carbon dioxide. Crit Care Med. 1998;26(5):868–72. doi: 10.1097/00003246-199805000-00020. [DOI] [PubMed] [Google Scholar]
- 24.Maniscalco M, Zedda A, Faraone S, Carratù P. Sofia M. Evaluation of a transcutaneous carbon dioxide monitor in severe obesity. Intensive Care Med. 2008;34(7):1340–4. doi: 10.1007/s00134-008-1078-8. [DOI] [PubMed] [Google Scholar]
- 25.Cuvelier A, Grigoriu B, Molano LC, Muir JF. Limitations of transcutaneous carbon dioxide measurements for assessing long-term mechanical ventilation. Chest. 2005;127(5):1744–8. doi: 10.1378/chest.127.5.1744. [DOI] [PubMed] [Google Scholar]
- 26.Rodriguez P, Lellouche F, Aboab J, Buisson CB, Brochard L. Transcutaneous arterial carbon dioxide pressure monitoring in critically ill adult patients. Intensive Care Med. 2006;32(2):309–12. doi: 10.1007/s00134-005-0006-4. [DOI] [PubMed] [Google Scholar]
- 27.Belenkiy S, Ivey KM, Batchinsky AI, Langer T, Necsoiu C, Baker W, et al. Noninvasive carbon dioxide monitoring in a porcine model of acute lung injury due to smoke inhalation and burns. Shock. 2013;39(6):495–500. doi: 10.1097/SHK.0b013e318292c331. [DOI] [PubMed] [Google Scholar]
- 28.Randerath WJ, Stieglitz S, Galetke W, Anduleit N, Treml M, Schäfer T. Evaluation of a system for transcutaneous long-term capnometry. Respiration. 2010;80(2):139–45. doi: 10.1159/000295904. [DOI] [PubMed] [Google Scholar]


