Abstract
Intestinal malrotation is an anomaly of fetal intestinal rotation that can present with symptoms after birth or in early childhood, but is rarely diagnosed in adults. Patients who have symptomatic presentations require surgery. Other entities may mimic intestinal malrotation and respond to non-surgical management. We present 2 adult cases with the radiological diagnosis of intestinal malrotation: one with true malrotation presenting as a duodenal mass, and another with “pseudo-malrotation” due to altered anatomy. These cases illustrate the importance of recognizing and differentiating these rare adult presentations of true malrotation from “pseudo-malrotation” in regards to their acute management.
Introduction
Intestinal malrotation is a congenital anomaly referring to either the lack of or incomplete rotation of the fetal intestine around the axis of the superior mesenteric artery (SMA). Symptoms usually present soon after birth or in early childhood, but are rarely seen in adults. We present 2 adult cases with the suspected radiological diagnosis of intestinal malrotation: one with true malrotation requiring immediate surgical management, and another of “pseudo-malrotation” due to altered abdominal anatomy, which required only conservative management.
Case Report 1
True Malrotation: A 48-year-old Caucasian male with history of hypertension and hypercholesterolemia presented to his local hospital with complaints of nausea and vomiting for 1 week. On admission, he was found to be dehydrated and was managed with intravenous fluids. A CT scan of his abdomen was read to suggest a 3-cm duodenal mass, and he was transferred to our hospital for further evaluation. Upon admission to our hospital, the patient reported that he had been having intermittent problems with nausea and vomiting throughout his adult life, but they were much milder than his current episode. The patient's vital signs and physical exam were normal, except for mild epigastric abdominal tenderness. Laboratory analyses were within normal limits.
An abdominal X-ray only showed a mild ileus. An esophagogastroduodenoscopy (EGD) was normal. A CT scan of his abdomen showed gastrointestinal (GI) malrotation with the duodenum looping into the right abdomen rather than crossing the midline. The duodenal mass-like appearance was due to the duodenum folding upon itself. A superior mesenteric vein (SMV) rotation sign was positive, with classic inverse relationship of the SMV to the SMA(Figure 1A). An upper Gl with small bowel series showed an intestinal malrotation, with the small bowel loops spiraling into the right abdomen (Figure 2A).
Figure 1.
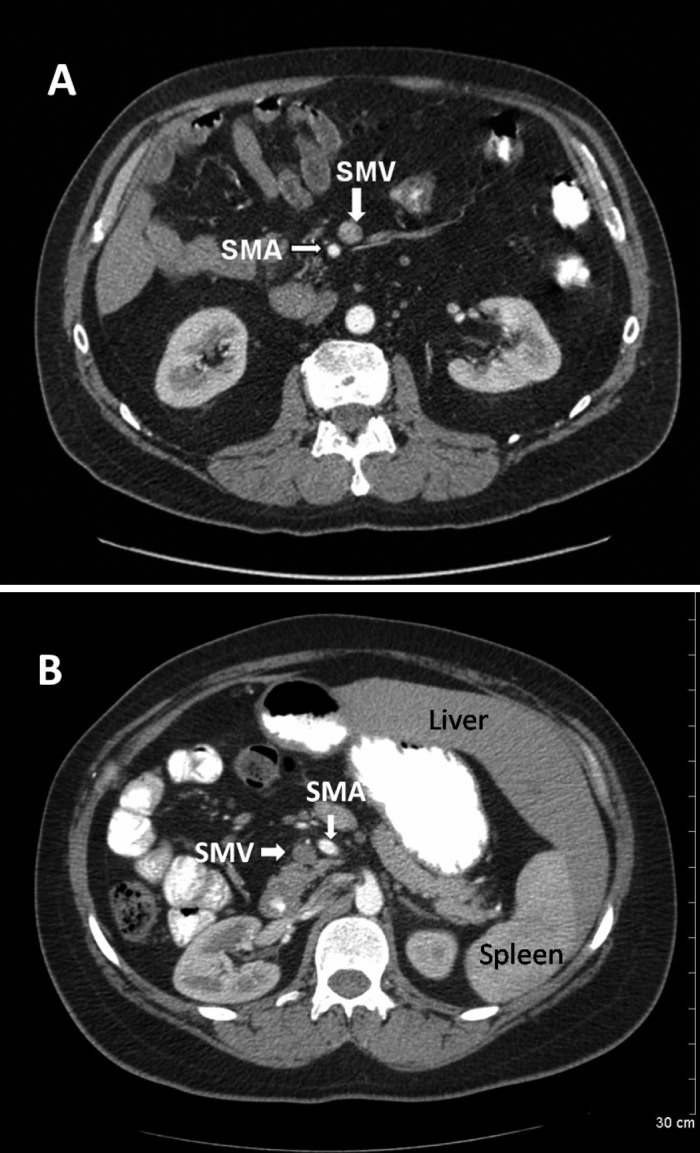
CAT scan of abdomen. (A) True malrotation with positive superior mesenteric vein (SMV) rotation sign showing classic inverse relationship of the SMV to the superior mesenteric artery (SMA). (B) Pseudo-malrotation with small bowel pushed to the right; not due to malrotation but from right liver lobe resection with compensatory hypertrophy of the left lobe. SMV rotation sign is negative.
Figure 2.

Upper Gl with small bowel series. (A) True malrotation: Intestinal malrotation with the duodenum not crossing midline and the small bowel loops spiraling into the right abdomen. (B) Pseudo-malrotation: The duodenum did not appear to cross past the midline and the jejunal small bowel was located in the right upper quadrant, suggestive of intestinal malrotation.
The patient was taken for an operative repair with a Ladd's procedure. Congenital bands across the second and third portions of the duodenum were lysed. The small bowel was repositioned and an appendectomy and cecopexy were performed. The patient recovered uneventfully and was doing well on his follow-up visit 1 month after discharge.
Case Report 2
Pseudo-Malrotation: A 36-year-old Caucasian female presented to the outpatient clinic with complaints of intermittent upper abdominal pain for the past year. She had a history of a hepatoblastoma as an infant and had undergone a tri-segmentectomy of her liver, followed by radiation and chemotherapy. She had been asymptomatic until this new onset of intermittent abdominal pain, which used to occur infrequently but now occurred several times a week. She had no associated nausea or vomiting.
Her vital signs and physical exam were normal, except for her abdominal exam. She had multiple well-healed scars across her mid-abdomen, without any evidence of a hernia. There was mild epigastric abdominal tenderness. Her bowel sounds were normal. The right lobe of her liver was not palpable. Further evaluation included a normal EGD. An upper Gl series showed no evidence of gastric outlet obstruction or strictures. The duodenum did not appear to cross past the vertebral bodies, and the entire jejunal small bowel was located in the right upper quadrant, suggestive of an intestinal malrotation (Figure 2B). A subsequent CT scan of her abdomen showed her small bowel pushed to the right; not due to malrotation, but due to her right hepatic lobe resection, with compensatory hypertrophy of the left lobe, which completely filled the left upper quadrant and displaced the spleen below it. A SMV rotation sign was negative (Figure 1B). Her abdominal pain was attributed to her altered intraabdominal anatomy as well as dyspepsia, which improved with antacid therapy. She continued to do well on medical therapy on follow-up.
Discussion
Malrotation is estimated to occur in between 1 in 200–500 live births, and symptomatic malrotation is estimated to occur in 1 in 6,000 live births.1 Male predominance is observed in neonatal presentations at a ratio of 2:1. In infants, the mortality ranges between 2–24%, and it increases tremendously with the presence of necrotic bowel at the time of surgery. However, the true incidence in adults is difficult to estimate, as most patients remain asymptomatic until they are picked up incidentally during diagnosis of other unrelated abdominal complaints.
Normal intestinal embryology was first described by Meckel in 1817.2 However, it was not until 80 years later that Mall explained the embryology of malrotation in 1898.3 In 1923, Dott described the relationship between the anatomy and clinical outcomes for malrotation.4 Dr. William Ladd wrote the classic article on treatment of malrotation, and his surgical approach—the Ladd procedure—remains the cornerstone of practice.5
The process of midgut rotation can be described in 3 stages. Stage I comprises of physiological umbilical herniation and rotation of the midgut loop, extending from the fifth to the 10th week of gestation. Failure of return to the abdomen during Stage I results in the development of omphaloceles. Stage II comprises further rotation of the midgut loop followed by reduction of the midgut hernia into the abdominal cavity, occurring during the 10th to the 12th week of gestation. Stage II anomalies result in nonrotation, mixed rotation, and reversed rotation. Nonrotation is the most common rotational anomaly resulting in midgut volvulus and duodenal obstruction. Stage III involves the fixation of the mesentery to the posterior abdominal wall extending from the 12th week of gestation up until term. Normal rotation and fixation results in a wide-based mesentery extending from the ligament of Treitz in the left upper quadrant to the ileocecal valve in the right lower quadrant. Stage III anomalies result in internal hernias, midgut volvulus, unattached duodenum, mobile cecum, incomplete fixation of hepatic flexure of the colon, and intermittent duodenal obstruction by Ladd bands.6
Rotational anomalies can lead to a wide variety of clinical symptoms and atypical anatomic positioning. In newborns, the most common presenting sign is bilious vomiting. It can also manifest as bloody vomitus due to intestinal necrosis, abdominal pain, peritonitis, dehydration, and shock.5 In older children and adults, the presentation could be intermittent vomiting, abdominal pain, and duodenal obstruction due to Ladd's bands. Less commonly, they can also present with enteropathy, pancreatitis, peritonitis, biliary obstruction, motility disorders, and chylous ascites.7 Volvulus can be caused due to the twisting of bowel around the SMA pedicle, and it could result in a life-threatening vascular insufficiency to the SMA distribution.
Plain radiographs are not very helpful for diagnosis, but may show a “double-bubble” sign due to partial obstruction of the duodenum causing distension of the stomach and the first part of the duodenum.8 Upper GI series can show the abnormal position of the duodenum with a “corkscrew” appearance due to duodenal obstruction or a volvulus.9 Barium enema can be used as an adjunct to upper GI series for a volvulus involving the transverse colon. CT scan is very useful in revealing abnormal small bowel location and for looking for the SMV rotation sign, which results from the inverse relationship of the SMV to the SMA.10 Ultrasound can also show a “whirlpool” sign suggesting a midgut volvulus.11
Ladd's procedure remains the mainstay of surgical treatment regardless of the age of presentation. This procedure involves detorsion of the midgut volvulus, if present, followed by lysis of adhesive Ladd's bands, widening of the mesenteric base, and a prophylactic appendectomy and cecopexy. Ladd's procedure can also be performed laparoscopically as long as there is no midgut volvulus.12
The management in adults differs depending upon clinical presentation. If there is a symptomatic malrotation, then prompt exploration of the acute abdomen along with Ladd's procedure and resection of the nonviable bowel should be performed. If malrotation is discovered during evaluation of an unrelated complaint, then the malrotation should only be addressed if it does not add undue risk to the current planned procedure. It can be repaired electively at a later date, if possible. If malrotation is asymptomatic with incidental discovery on a radiologic examination, then intervention is only indicated if the patient is at risk for a midgut volvulus.13
Our cases illustrate the importance of identifying and differentiating a true small bowel malrotation in an adult patient versus a pseudo-malrotation. Rarely, true malrotation can present in adult patients with a variety of abdominal signs and symptoms, such as the duodenal mass in our first patient; that said, initial imaging may be misleading in patients with a pseudo-malrotation due to altered abdominal anatomy from prior surgeries such as a tri-segmentectomy, as in our second patient. Fortunately, we can now confirm our suspicions with advanced imaging technology in a noninvasive manner, alerting us to the need for immediate surgical management for true malrotation versus conservative management for pseudo-malrotation.
Disclosures
Author contributions: All authors had significant contribution to the conception and design; analysis and interpretation of the data; drafting of the article; critical revision of the article for important intellectual content; final approval of the article; and meet criteria for authorship. H.S. Khara is the article guarantor.
Financial disclosure: No funding resources were involved in our study. No conflicts of interest exist for any authors.
References
- 1.Warner BW. Malrotation In: Oldham KT, Colombani PM, Foglia RP, eds. Surgery of Infants and Children: Scientific Principles and Practice. Philadelphia, PA: Lippincott Williams & Wilkins; 1997: 1229–40. [Google Scholar]
- 2.Skandalakis JE, Gray SW, Ricketts R, Richardson DD. The small intestines In: Skandalakis JE, Gray SW, eds. Embryology for Surgeons: The Embryological Basis for the Treatment of Congenital Anomalies. 2nd ed.Baltimore, MD: Williams & Wilkins; 1994:184–236. [Google Scholar]
- 3.Mall FT. Development of the human intestine and its position in the adult. Bull Johns Hopkins Hosp. 1898;9:197–208. [Google Scholar]
- 4.Dott NM. Anomalies of intestinal rotation: Their embryology and surgical aspects: With report of five cases. Br J Surg. 1923;11(42):251–86. [Google Scholar]
- 5.Ladd WE. Surgical diseases of the alimentary tract in infants. N Engl J Med. 1936;215:705–8. [Google Scholar]
- 6.Amaral L, Quintanilha R, Bernardo L, et al. Intestinal malrotation in the elderly. Am Surg. 2009;75:631–3. [PubMed] [Google Scholar]
- 7.Spigland N, Brandt ML, Yazbeck S. Malrotation presenting beyond the neonatal period. J Pediatr Surg. 1990;25(11):1139–42. [DOI] [PubMed] [Google Scholar]
- 8.Poki HO, Holland AJ, Pitkin J. Double bubble, double trouble. Pediatr Surg Int. 2005;21(6):428–31. [DOI] [PubMed] [Google Scholar]
- 9.Ortiz-Neira CL. The corkscrew sign: Midgut volvulus. Radiology. 2007;242(1):315–6. [DOI] [PubMed] [Google Scholar]


