Abstract
Recently, indications for endoscopic clips have expanded to include closure of gastrointestinal fistulae and perforations. A 62-year-old man with remote history of surgery for peptic ulcer underwent right hemicolectomy for a large hepatic flexure mass with proximal colonic dilatation. During surgery, inadvertent pinpoint duodenotomy of the afferent Billroth II limb resulted in a duodeno-cutaneous fistula. Despite total parental nutrition, cutaneous bile drainage persisted. The duodenal fistula was closed during upper endoscopy using three endoclips. Cutaneous bile drainage stopped, and the abdominal wall defect healed. This is the first published case of endoclip closure of an iatrogenic duodenal fistula from a Billroth II afferent limb.
Introduction
Use of endoscopic clips was first described in 1975 as a novel method for management of gastrointestinal bleeding.1 Over the next 2 decades, endoclips were extensively employed in Europe and Japan, and they are now widely used in the United States.2,3 No consensus guidelines exist for the use of endoclips for other indications. Recent case reports describe more expanded utility to include closure of gastrocutaneous fistulae and viscus perforations.4–7 The ability to treat such breaches in intestinal continuity endoscopically and avoid surgery has great potential for shortening hospital stays and decreasing patient morbidity and mortality. We report a patient with prior Billroth II surgery who developed a duodeno-cutaneous fistula following laparotomy to resect a hepatic flexure colon mass. Spontaneous closure of the fistula did not occur after several months of conservative treatment including total parenteral nutrition. Another surgery for fistula closure was contemplated. Prior to operation, upper endoscopy to assess the duodenum was requested by the surgical service.
Case Report
A 62-year-old man was first seen in the gastroenterology clinic complaining of abdominal pain and weight loss. He had a history of partial gastrectomy and vagotomy performed 25 years earlier for treatment of peptic ulcer disease. He reported 6 months of mild postprandial epigastric pain and 15 pounds of unintentional weight loss. He denied nausea, vomiting, melena, hematochezia, and change in bowel habits. Five years earlier, upper endoscopy revealed Billroth II anatomy consistent with his reported ulcer surgery. Colonoscopy performed at that time was significant for a 30-mm tubulovillous adenoma in the descending colon, which was completely resected via snare polypectomy.
Physical examination revealed evidence of prior abdominal surgery and mild tenderness to palpation in the right upper quadrant without guarding or rebound. On colonoscopy, there was an obstructing, near circumferential mass at the hepatic flexure (Figure 1A and Figure 1B) preventing further advancement of the colonoscope. Multiple biopsies of the mass were taken. CT scan of the abdomen performed on the same day reported a 4.9 × 2.9-cm hepatic flexure mass with circumferential narrowing and a dilated, air-filled colon proximal to the lesion. Endoscopic biopsies of the mass showed normal colonic mucosa. Repeat colonoscopy 3 weeks after the initial procedure showed a similar endoscopic appearance, and biopsies of the mass were again negative for neoplasia.
Figure 1.
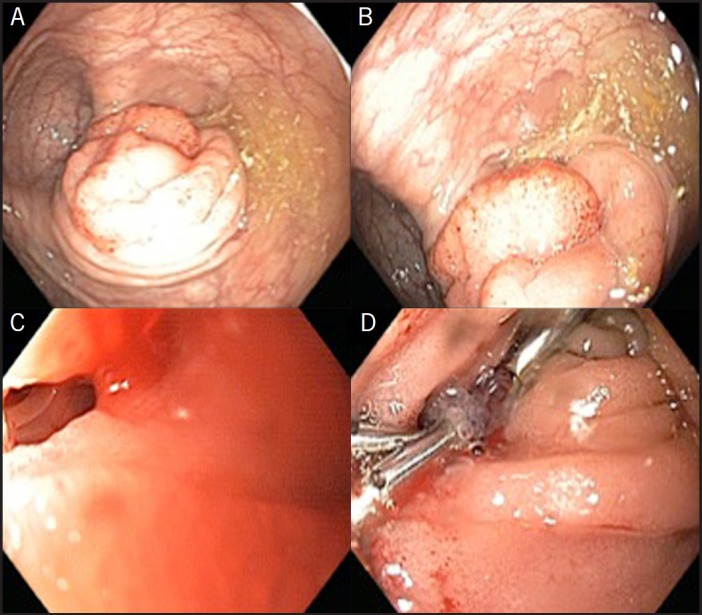
(A and B) Large polypoid appearing mass at the hepatic flexure. (C) Fistula orifice originating from afferent Billroth II duodenal limb. (D) Three standard endoclips deployed with successful closure of fistula orifice.
The case was presented at the institution's tumor board, and a collective decision was made to perform an open right hemicolectomy, given radiologic and endoscopic appearance suggesting a hepatic flexure colon cancer. At surgery, both the afferent limb of the duodenum and the gallbladder were tightly adherent to the colon in the area of the hepatic flexure, and the gallbladder contained multiple gallstones. During the right hemicolectomy and cholecystectomy procedure, a pinpoint duodenotomy occurred. The duodenal perforation was sutured, and a percutaneous drain was placed in the gallbladder fossa adjacent to the duodenotomy site. Pathology of the resected colon showed marked acute and chronic serositis with associated fibrosis, but no malignancy or neoplasia was evident.
Significant percutaneous drainage of bile occurred in the immediate postoperative period and persisted over the next 2 months, despite a trial of total parenteral nutrition. Fistulogram revealed an enterocutaneous fistula arising from the afferent limb of the Billroth II anastomosis with contrast entering the stomach via the gastojejunostomy. Upper endoscopy was performed in anticipation of surgery to close the fistula, and the duodenal opening of the fistula was easily identified in the afferent limb of the Billroth II anastomosis (Figure 1C). Three standard endoclips were used to approximate the fistula opening (Figure 1D), resulting in immediate and lasting cessation of percutaneous bile drainage. The patient was discharged from the hospital 2 days after endoscopic clipping. At 1 month follow-up, the patient reported no leakage of intestinal contents, and the abdominal wall fistulous site had closed.
Discussion
Postoperative enterocutaneous fistulae present a therapeutic challenge. Traditionally a complication requiring surgical intervention, development of a number of endoscopic devices/therapeutics, including fibrin tissue sealant/adhesive and endoclips, has led to several non-surgical methods for management of enterocutaneous fistulae.
Endoscopically-placed endoclips for management of small gastrointestinal perforations was initially described in 1995 when Wewalka et al successfully closed a small esophageal perforation that developed after pneumatic dilatation for achalasia.4 In 2003, Familiari et al described endoclip closure of a colocutaneous fistula, which occurred following an episode of necrotizing pancreatitis.5 Gastrocutaneous fistula, which occasionally occurs after removal of a percutaneous gastrostomy tube, also lends itself to endoclip closure.8,9 In our case, extensive adhesions secondary to the patient's prior Billroth II surgery and chronic cholecystitis resulted in a complex mass involving the hepatic flexure of the colon, the gallbladder, and the duodenal portion of the Billroth II afferent limb. Extensive dissection to free these organs resulted in an injury to the duodenum, which was not successfully repaired and continued to drain bile externally for 2 months through a surgical drain placed in the gallbladder fossa. Successful endoscopic closure of our patient's duodenal fistula with endoclips obviated the need for additional surgery. To our knowledge, this is the first report of endoclip closure of an iatrogenic duodenal fistula in a Billroth II afferent limb. Use of endoscopically-placed endoclips should be considered as a non-surgical therapeutic option when dealing with small breaches in upper gastrointestinal viscus integrity.
Disclosures
Author contributions: All authors contributed significantly to the creation and review of all parts of the manuscript. All take full responsibility for the work presented in the paper. MT Voellinger is the article guarantor.
Financial disclosure: The authors report no financial, consultant, institutional, or other relationship that may lead to bias or conflict of interest. There was no source of funding.
Informed consent was obtained for this case report.
References
- 1.Hayashi T, Yonezawa M, Kawabara T. The study on staunch clip for the treatment by endoscopy. Gastroenterol Endosc. 1975;17:355–64. [Google Scholar]
- 2.Grupka MJ, Benson J. Endoscopic clipping. J Dig Dis. 2008;9(22):72–8. [DOI] [PubMed] [Google Scholar]
- 3.Raju GS, Gajula L. Endoclips for GI endoscopy. Gastrointest Endosc. 2004;59:267–79. [DOI] [PubMed] [Google Scholar]
- 4.Wewalka FW, Clodi PH, Haidinger D. Endoscopic clipping of esophageal perforation after pneumatic dilation for achalasia. Endoscopy. 1995;27(8):608–11. [DOI] [PubMed] [Google Scholar]
- 5.Familiari P, Macri A, Consolo P, et al. Endoscopic clipping of a colocutaneous fistula following necrotizing pancreatitis: Case report. Dig Liver Dis. 2003;35(12):907–10. [DOI] [PubMed] [Google Scholar]
- 6.Thurairajah P, Hawthorne AB. Endoscopic clipping of a nonhealing gastrocutaneous fistula following gastrostomy removal. Endoscopy. 2004;36(9):834. [DOI] [PubMed] [Google Scholar]
- 7.Siddiqui AA, Kowalski T, Cohen S. Closure of a nonhealing gastrocutaneous fistula using an endoscopic clip. South Med J. 2007;100(1):75–6. [DOI] [PubMed] [Google Scholar]
- 8.Duddempudi S, Ghevariya V, Singh M, et al. Treatment of persistently leaking post PEG tube gastrocutaneous fistula in elderly patients with combined electrochemical cautery and endoscopic clip placement. South Med J. 2009;102(6):585–8. [DOI] [PubMed] [Google Scholar]
- 9.Teitelbaum JE, Gorcey SA, Fox VL. Combined endoscopic cautery and clip closure of chronic gastrocutaneous fistulas. Gastrointest Endosc. 2005;62(3):432–5. [DOI] [PubMed] [Google Scholar]


