Abstract
We present a case of acute esophageal necrosis (AEN) likely caused by chronic use of bismuth subsalicylate, an active ingredient in over-the-counter Pepto-Bismol®, which contains 220 g of salicylic acid in each 30 mL quantity. While aspirin is known to cause gastritis and gastric ulcers, this is the first case, to our knowledge, reporting AEN after chronic bismuth subsalicylate use.
Introduction
Acute esophageal necrosis (AEN), or black esophagus, is a rare entity caused by variety of factors. One theory is that the relatively low perfusion state in the distal areas of the esophagus make it susceptible to mucosal injury. We present the first case report of AEN after using large doses of over-the-counter Pepto-Bismol® (bismuth subsalicylate).
Case Report
An woman in her early 80s with past medical history significant for ulcerative colitis and gastroesophageal reflux (GERD) with use of bismuth subsalicylate was admitted to the hospital for 2 days of constant, diffuse abdominal pain with melena. She denied any tobacco, alcohol, illicit drug, or any nonsteroidal anti-inflammatory drug (NSAID) use. On admission, the patient was hemodynamically stable; her physical exam was notable for a slightly distended abdomen with diffuse tenderness to palpation without any rebound or guarding. She had positive guaiac stool with negative stool cultures. Laboratory tests revealed leukocytosis and hemoglobin of 10.1 g/dL (baseline: 14 g/dL). The basic metabolic panel, hepatic function panel, coagulation studies, and urinalysis were all normal.
On the second day of admission, the patient underwent an esophagogastroduodenoscopy (EGD) that revealed an ulcerated and darkened necrotic esophageal mucosa extending continuously from 20 cm beyond the incisors to the gastroesophageal junction (Figure 1). A biopsy revealed extensive necrosis, marked inflammation, and absence of esophageal epithelium consistent with AEN (Figure 2).
Figure 1.
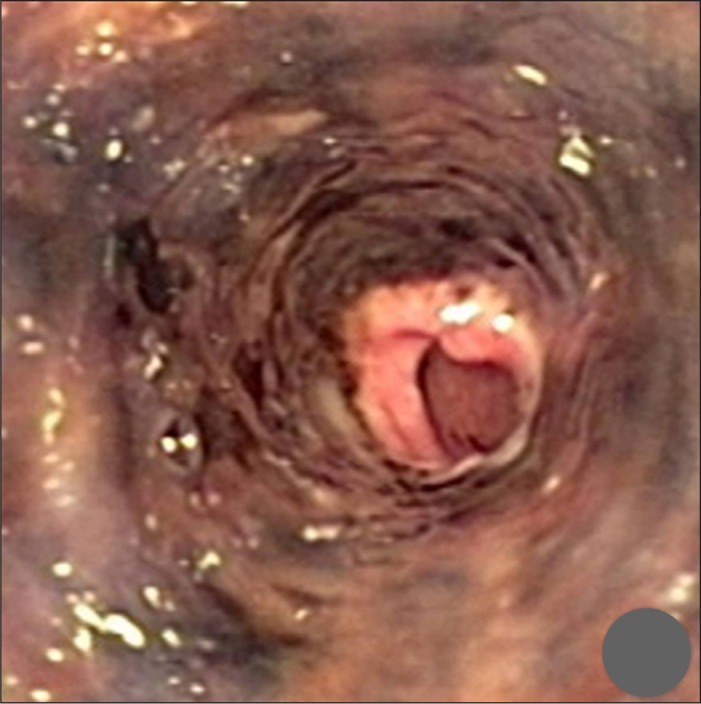
Endoscopy performed at the time of admission shows an ulcerated and necrotic esophageal mucosa starting 20 cm beyond the incisors to the gastroesophageal junction with normal gastric mucosa.
Figure 2.
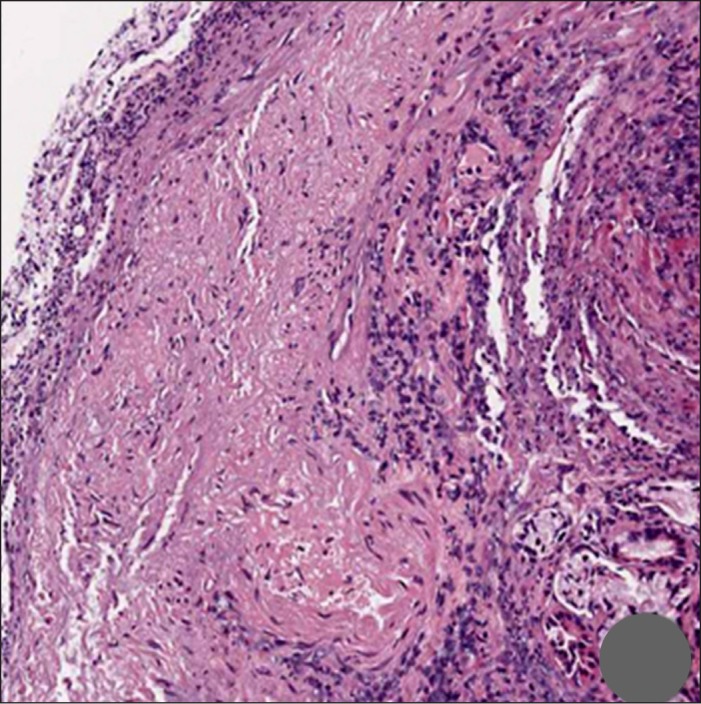
Endoscopic biopsy demonstrates an ulcerated esophageal mucosa with complete absence of the epithelium and replacement by a fibrinopurulent exudate characteristic of ulcerative lesions. The underlying mucosa shows increased inflammation and vascularity.
The patient reported consuming 40–50 antacids per day for 8–10 years for her acid reflux disease. Total parenteral nutrition was started and the patient was managed conservatively. A repeat EGD 10 days after admission demonstrated diffuse esophageal edema and pink granulation tissue consistent with healing esophageal mucosa (Figure 3). The patient's diet was slowly advanced and she was discharged in stable condition 2 weeks after admission.
Figure 3.

Repeat endoscopy 10 days after admission shows diffuse esophageal edema, mild friability, and pink granulation tissue consistent with resolving esophagitis.
Discussion
AEN, or black esophagus, is a rare clinical entity with an incidence ranging from 0.01% to 0.2% in autopsy studies and clinical trials.1–3 Prior case studies have shown a predilection for AEN in individuals who suffer from cardiovascular ischemic events, acute alcohol intoxication, and caustic injury from alkaline compounds, but AEN is thought to be a result of many factors.4–6 The most common presentation is hematemesis and melena, with endoscopy demonstrating friable or macerated mucosa involving the distal two-thirds of the esophagus with a very sharp demarcation at the gastroesophageal junction.4 The reason for the location may be due to the relatively low perfusion state compared to more proximal areas of the esophagus that are often affected in patients with vasculopathy. Histopathology often shows mucosal and submucosal necrosis with heavy leukocyte infiltration, as seen in our patient, though biopsy is not required for diagnosis.7 Management is conservative, but patients require close monitoring due to the risk of complications such as superimposed infections, stenosis, strictures, and perforations. Mortality can reach as high as 32% (often in cases presenting with other comorbidities), but mortality specific to AEN is around 6%.6
The exact etiology of AEN in this case is unclear in the absence of vascular disease. AEN in this patient might be secondary to the chronic ingestion of a large dose of antacids (i.e., bismuth subsalicylate) causing chemical injury and necrosis. Bismuth subsalicylate, an active ingredient in over-the-counter Pepto-Bismol®, is used widely to treat symptomatic inflammation of gastric and intestinal epithelium. The reactivity of bismuth with sulfur molecules ingested from food can lead to linguinal hyperpigmentation (black tongue), which is often benign and reversible with medication discontinuation.8 The high doses of an alkalizing medication such as bismuth subsalicylate, which contains 220 g of salicylic acid per 30 mL quantity, may have caused chemical injury to the esophageal epithelium to develop even without the use of other NSAIDs. The chemical reaction between bismuth and sulfur may have created the dark pigmentation of the esophagus classic to AEN.9 To our knowledge, no other case report has reported a black esophagus after prolonged, heavy use of over-the-counter bismuth subsalicylate with rapid recovery after the discontinuation of the causative agent.
Disclosures
Author contributions: J. Abed and P. Mankal wrote the manuscript. H. Judeh and S. Kim provided the case history and photographs. S. Kim is the article guarantor.
Financial disclosure: No conflicts of interest or financial disclosures to report.
The patient consented in writing to all procedures. The authors made every effort to contact the patient and her next of kin, but due to the length of time between the case and this report, neither the patient nor the next of kin could be reached for consent to publish. However, the authors feel that the patient information is sufficiently anonymous and that the patient would not object to this publication.
References
- 1.Postlethwait RW, Musser AW. Changes in the esophagus in 1,000 autopsy specimens. J Thorac Cardiovasc Surg. 1974;68(6):953–6. [PubMed] [Google Scholar]
- 2.Ben Soussan E, Savoye G, Hochain P, et al. Acute esophageal necrosis: A 1-year prospective study. Gastrointest Endosc. 2002;56(2):213–7. [DOI] [PubMed] [Google Scholar]
- 3.Lacy BE, Toor A, Bensen SP, et al. Acute esophageal necrosis: Report of two cases and a review of the literature. Gastrointest Endosc. 1999;49(4pt 1):527–32. [DOI] [PubMed] [Google Scholar]
- 4.Neumann DA 2nd, Francis DL, Baron TH. Proximal black esophagus: A case report and review of the literature. Gastrointest Endosc. 2009;70(1):180–1. [DOI] [PubMed] [Google Scholar]
- 5.Cappell MS. Esophageal necrosis and perforation associated with the anticardiolipin antibody syndrome. Am J Gastroenterol. 1994;89(8):1241–5. [PubMed] [Google Scholar]
- 6.Gurvits GE. Black esophagus: Acute esophageal necrosis syndrome. World J Gastroenterol. 2010;16(26):3219–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rejchrt S, Douda T, Kopacova M, et al. Acute esophageal necrosis (black esophagus): Endoscopic and histopathologic appearance. Endoscopy. 2004;36(12):1133. [DOI] [PubMed] [Google Scholar]
- 8.Cohen PR. Black tongue secondary to bismuth subsalicylate: Case report and review of exogenous causes of macular lingual pigmentation. J Drugs Dermatol. 2009;8(12):1132–5. [PubMed] [Google Scholar]
- 9.Sugawa C, Takekuma Y, Lucas CE, Amamoto H. Bleeding esophageal ulcers caused by NSAIDs. Surg Endosc. 1997;11(2):143–6. [DOI] [PubMed] [Google Scholar]


