Abstract
Hepatic portal venous gas (HPVG), a rare condition in which gas accumulates in the portal venous circulation, is often associated with a significant underlying pathology, such as intestinal ischemia, sepsis, and trauma. HPVG after endoscopy or dilation is an unusual complication. We report a case of HPVG following upper endoscopy and dilation for an esophageal stricture in a 34-year-old patient with eosinophilic esophagitis (EoE). The patient was treated conservatively, and his symptoms resolved. Follow-up computed tomography (CT) scan showed resolution of HPVG. This case highlights a rare and potentially ominous complication of upper endoscopy and dilation and underscores the role of conservative management.
Introduction
Hepatic portal venous gas (HPVG) is a rare condition in which intraluminal gas or gas produced by bacteria in the gut enters the portal venous circulation.1 Common precipitating factors favoring the development of portal venous gas include intestinal wall disruption, bowel distention, and sepsis, which typically suggest an ominous underlying pathology.2 We describe a previously unrecognized cause of HPVG following an upper endoscopy and dilation for a benign esophageal stricture in a young male patient with eosinophilic esophagitis (EoE).
Case Report
A healthy 34-year-old male with a past medical history significant for EoE and asthma presented with unexplained dysphagia. He underwent esophagogastroduodenoscopy (EGD), which revealed esophageal mucosal changes that were suggestive of EoE, including loss of vascular pattern and white exudates, and a benign esophageal stricture at the gastroesophageal junction. The stricture was dilated with a balloon size of 18 mm. Esophageal biopsies confirmed the diagnosis of EoE.
Within an hour after the procedure, the patient experienced nausea and epigastric pain. His physical exam was remarkable for diffuse epigastric tenderness with no guarding or rigidity. Laboratory tests were normal (complete blood count, liver, and pancreatic enzymes). Abdominal computed tomography (CT) demonstrated diffuse portal venous gas throughout the right hepatic lobe extending to the periphery of the liver (Figure 1). The patient was hospitalized and treated conservatively with intravenous fluids and pain control. He was discharged the following day after his symptoms had resolved. A follow-up repeat CT scan revealed no residual portal vein air. He continued to do well at a 6-month follow-up.
Figure 1.
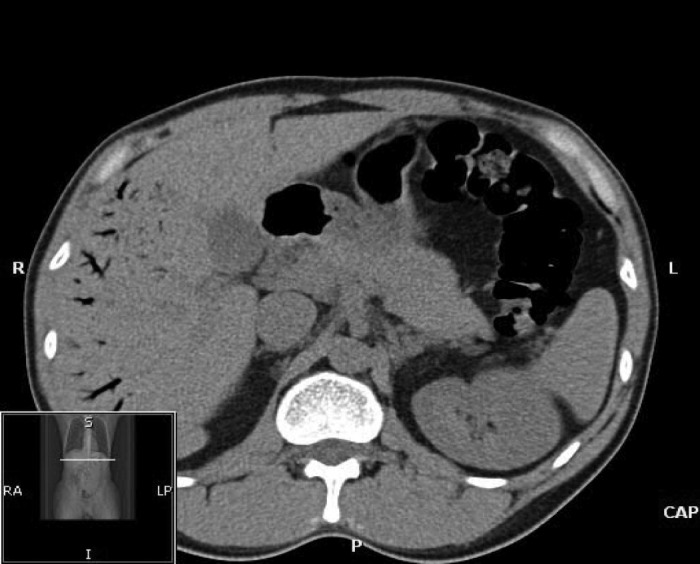
Diffuse portal venous gas throughout the right hepatic lobe extending to the periphery of the liver.
Discussion
HPVG has often been thought of as an ominous clinical finding; it is commonly the result of portomesenteric vein gas accumulation resulting from bowel ischemia.2 Other etiologies associated with HPVG are summarized in Table 1. Only a small fraction of cases are attributed to radiologic and endoscopic procedures. Of these, HPVG has been reported following EGD in patients with a gastric ulcer3 and duodenal tumor,4 after corrosive acid ingestion,5 following esophageal variceal sclerotherapy and banding,6 after percutaneous endoscopic gastrostomy, and after ERCP.5
Table 1.
Reported Causes of Hepatic Portal Venous Gas
| Abdominal Conditions | Mesenteric ischemia4 Necrotizing entercolitis Inflammatory bowel disease Diverticulitis Intra-abdominal sepsis Pneumatosis intestinalis Pancreatitis Bowel obstruction Suppurative cholangitis5 Bowel necrosis IIleus Peptic ulcer disease C. difficle colitis Infectious enteritis Gastric cancer1 Ileitis10 Volvulus2 Fecal impaction7 |
| Iatrogenic | Corticosteroid therapy11 Endoscopic retrograde cholangiopancreatography Esophageal variceal banding Percutaneous endoscopic gastrostomy Endoscopic balloon dilation5 Upper endoscopy3 Air contrast barium enema Endoscopic ultrasound-guided fine needle biopsy Sclerotherapy Colonoscopy9 |
| Trauma | Gastric dilation Caustic ingestion12 |
| Other | Liver transplant4 Gynecologic cancer2 Chronic obstructive pulmonary disease11 |
HPVG is best diagnosed with CT, where it appears as tubular areas of decreased attenuation in the liver. The low attenuation areas are caused by accumulation of gas in the intrahepatic portal veins, where it is carried by centrifugal blood to the hepatic periphery.2 Due to the high carbon dioxide content of portal venous gas, it is expected to last briefly in the vascular system before it is absorbed or removed by bulk flow, unless gas production persists.7
The mechanism for the formation of HPVG is unclear, but it has been hypothesized that certain factors allow gas to enter the portal circulation through veins or lymphatics of the intestinal wall and reach the hepatic veins through the hepatic sinusoids.7 These factors may include compromised bowel wall integrity, bowel distention, increased intraluminal pressure, and sepsis. Bacterial fermentation of carbohydrates in sepsis may also contribute to the development of HPVG.2
Endoscopic examination of our patient revealed esophageal inflammation with no gross ulcerations. It is possible this underlying esophageal inflammation contributed to compromised mucosal integrity. The esophageal inflammation coupled with the endoscopic procedure (air insufflation) and esophageal dilation likely facilitated diffusion of intraluminal air across the gastrointestinal mucosa. It has been proposed that endoscopic procedures facilitate diffusion in several ways. Specifically, shear pressure caused by dilation may compromise mucosal wall integrity, and gastric or lumen distention caused by insufflation may lead to increased intraluminal pressures, forcing air across the mucosal surface.5,7
The presence of HPVG may convey the notion of a life-threatening complication. However, HPVG is not necessarily an indication for surgical management and may require no treatment.7,8 The underlying etiology and clinical condition of the patient should dictate management. Surgical management is warranted in clinically unstable patients, or if there is evidence of peritonitis or bowel perforation. Conservative management may be used in clinically stable patients or those who have developed HPVG from an invasive procedure.2 Due to the likely iatrogenic-induced HPVG in our patient, he was treated conservatively with fluids and analgesics, which resolved his symptoms and CT findings.
We describe a case of HPVG following EGD and dilation in a young patient with EoE. Only a handful of cases have mentioned HPVG following endoscopic procedures, and a large national database from the American Society for Gastrointestinal Endoscopy does not mention it as a complication after EGD or dilation.9 This case illustrates the need to recognize a rare complication following EGD and dilation. In this setting, HPVG can be effectively managed conservatively.
Disclosures
Author contributions: K. Seeger completed the literature search and review, and wrote the manuscript. SR Achem evaluated the patient, designed the study, wrote and edited the manuscript, and is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Alqahtani S, Coffin CS, Burak K, et al. Hepatic portal venous gas: A report of two cases and a review of the epidemiology, pathogenesis, diagnosis and approach to management. Can J Gastroenterol. 2007;21(5):309–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sebastià C, Quiroga S, Espin E, et al. Portomesenteric vein gas: Pathologic mechanisms, CT findings, and prognosis. Radiographics. 2000;20(5):1213–24; discussion 1224–6. [DOI] [PubMed] [Google Scholar]
- 3.Kuo SM, Chang WK, Yu CY, Hsieh CB. Silent hepatic portal venous gas following upper gastrointestinal endoscopy. Endoscopy. 2009;41(suppl 2):E121–2. [DOI] [PubMed] [Google Scholar]
- 4.Lamparter S, Goecke W, Koehler HH. Hepatic portal venous gas after upper endoscopy in a patient with a gastrointestinal stromal tumor. J Clin Ultrasound. 2009;37(7):401–2. [DOI] [PubMed] [Google Scholar]
- 5.Lee CG, Kang HW, Song MK, et al. A case of hepatic portal venous gas as a complication of endoscopic balloon dilatation. J Korean Med Sci. 2011;26(8):1108–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed K, Atiq M, Richer E, et al. Careful observation of hepatic portal venous gas following esophageal variceal band ligation. Endoscopy. 2008;40(suppl 2):E103. [DOI] [PubMed] [Google Scholar]
- 7.Kesarwani V, Ghelani DR, Reece G. Hepatic portal venous gas: A case report and review of literature. Indian J Crit Care Med. 2009;13(2):99–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franken JM, Veen EJ. Hepatic portal venous gas. J Gastrointestin Liver Dis. 2010;19(4):360. [PubMed] [Google Scholar]
- 9.Ben-Menachem T, Decker GA, Early DS, et al. ASGE Standards of Practice Committee. Adverse events of upper GI endoscopy. Gastrointestinal Endosc. 2012;76(4):707–18. [DOI] [PubMed] [Google Scholar]
- 10.Niki M, Shimizu I, Horie T, et al. Hepatic portal venous gas disappearing within 24 hours. Internal Med. 2002;41(11):950–2. [DOI] [PubMed] [Google Scholar]
- 11.Abboud B, El Hachem J, Yazbeck T, Doumit C. Hepatic portal venous gas: Physiopathology, etiology, prognosis, and treatment. World J Gastroenterol. 2009;15(29):3585–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bani-Hani KE, Heis HA. Iatrogenic gastric dilatation: A rare and transient cause of hepatic-portal venous gas. Yonsei Med J. 2008;49(4):669–71. [DOI] [PMC free article] [PubMed] [Google Scholar]


