Abstract
Enteric duplication cysts (EDCs) are benign congenital anomalies that are found incidentally in adults. Gastric duplication cysts (GDCs) are the least common subtype of EDC, but when located near the pancreas, may resemble other neoplastic conditions. We report a case of GDC adjacent to the pancreas with high cystic fluid amylase and carcinoembryonic antigen (CEA) and 3 different epithelia (respiratory, gastric, and intestinal), all diagnosed via endoscopic ultrasound with fine-needle aspiration.
Introduction
Enteric duplication cysts (EDCs) are rare congenital malformations that usually lie alongside the gastrointestinal tract.1,2 EDCs appear most often in children, but may remain asymptomatic until incidental diagnosis is made by radiologic or endoscopic imaging.3 Diagnosis can be made by computed tomography (CT), ultrasound, or endoscopic ultrasound (EUS) with or without fine needle aspiration (FNA).4 GDCs account for approximately 4% of EDCs,5,6 and are often mislabeled as pancreatic cystic neoplasms or pseudocysts when located within or near the pancreas, despite advanced imaging technology.3 Malignancy may arise from a GDC.7
Case Report
A 43-year-old female presented with chronic abdominal pain for 1 year without any alarming signs. An upper endoscopy was unremarkable. An abdominal CT demonstrated a well-defined sausage-shaped retroperitoneal cystic lesion adjacent to the pancreatic tail, measuring 7.4 cm x 3.6 cm, distinct from the stomach wall. A magnetic resonance imaging (MRI) / magnetic resonance cholangiopancreatography (MRCP) showed no communication between the lesion and the stomach or pancreatic duct (Figure 1). EUS with FNA visualized an anechoic cystic lesion near the tail of the pancreas not connected with the pancreatic duct or the stomach wall (Figure 2). Cystic fluid analysis revealed a CEA of 865 ng/mL and an amylase of 1878 U/L without evidence of malignancy. Given the lesion's high malignant potential, high cystic fluid CEA, and amylase suspicious for neoplastic process, the patient underwent a laparoscopic-assisted distal pancreatectomy, splenectomy, and partial gastroectomy with an unremarkable postoperative course. The surgical specimen revealed a gastric duplication cyst lined predominantly by respiratory epithelium (Figure 3) with a focus of gastric mucosa with intestinal metaplasia (Figure 4) and no malignancy.
Figure 1.
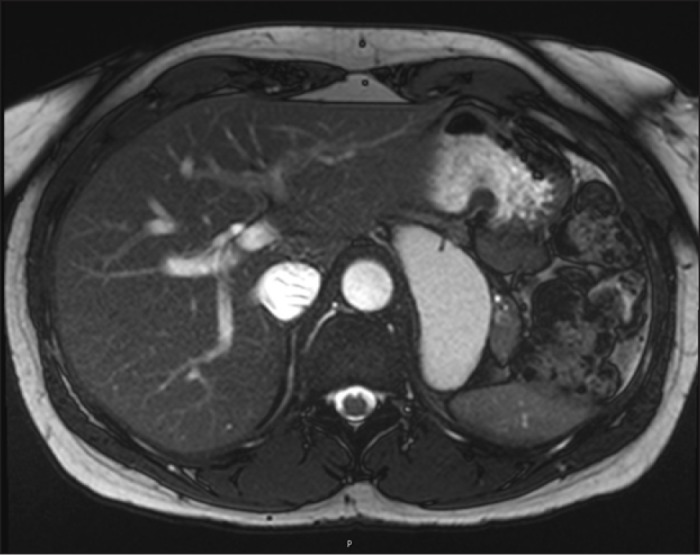
Cyst lesion measuring 7.1 x 3.3 cm adjacent to the pancreas demonstrates increased signal on T2-weighted image. The lesion is separate from the adjacent pancreas and stomach.
Figure 2.
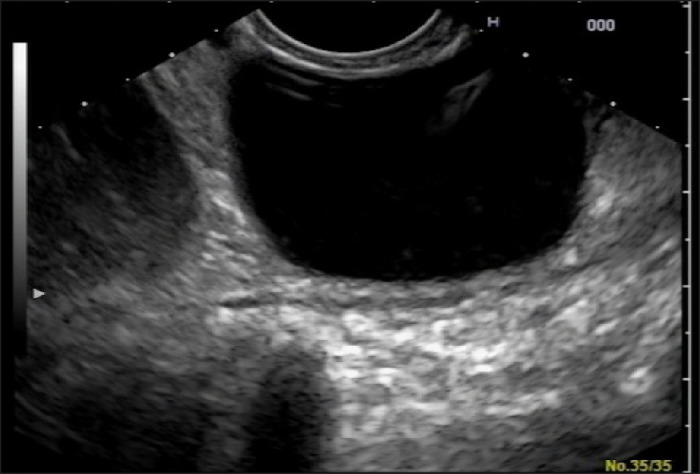
EUS showing an anechoic cystic lesion at the tail of the pancreas without direct communication with the pancreatic duct or stomach wall.
Figure 3.
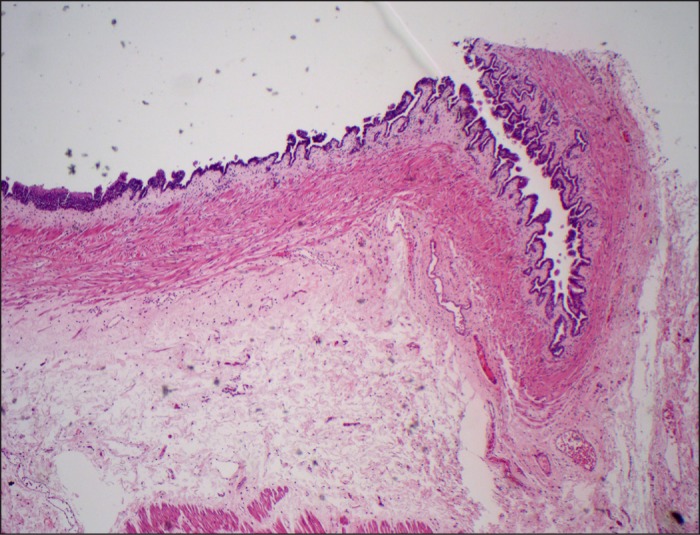
Respiratory epithelium on H&E stain showing serrated lining in gastric duplication cyst (4x magnification).
Figure 4.
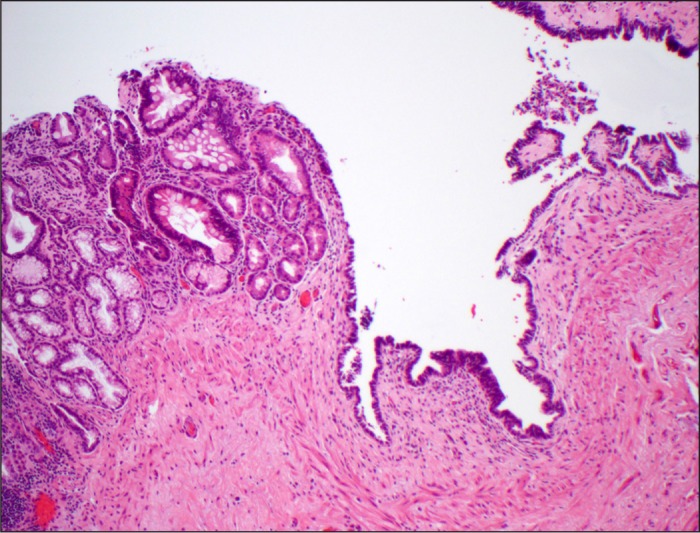
Respiratory epithelium of gastric duplication cyst transitioning focally into gastrointestinal-type epithelium.
Discussion
Diagnosis of EDCs can be made by radiological imaging in most cases. When the diagnosis is equivocal, fluid aspiration is recommended to confirm or exclude other neoplastic conditions. Pancreatic cysts can be benign (pseudocyst), precancerous (mucinous cystadenoma and intraductal papillary mucinous neoplasm), or malignant (cystadenocarcinoma). Cystic fluid analysis is useful in differentiating these types, but GDCs located near or within the pancreatic tissue can mimic neoplastic lesions.8 There is only 1 reported case of a GDC with an elevated CEA, amylase, and CA19-9 lined by respiratory-type epithelium; however, EUS was not done prior to the surgery.9 Surgical removal of a pancreatic cyst is reasonable when a neoplastic process is suspected. In our case, given the risk of a pancreatic cystic neoplasm, surgical intervention was recommended.
EDCs are benign congenital malformations that have extremely low malignant potential. Their appearance and location are frequently typical; however, location within another organ (i.e., pancreas, liver, or mediastinum) poses a diagnostic challenge and may encourage an overly aggressive approach. The fluid analysis of EDCs may resemble other neoplastic processes, such as pancreatic cystic neoplasm given the high CEA, amylase, or CA19-9, especially when located outside the alimentary tract.9 Gastroenterologists should consider duplication cysts in the differential diagnosis of cystic pancreatic lesions, even if the cystic fluid analysis is suspicious for malignancy. These lesions may require either a surgical or conservative approach based upon the fluid analysis. Continuous surveillance may be considered in definitive cases.
Disclosures
Author contributions: M. Sultan wrote the manuscript and is the article guarantor. D. Karanovic, W. Chalhoub, A. Ajmera, F. Muafa, S. Shafa, L. Johnson, and N. Haddad reviewed the manuscript. JC Zeck provided the pathology slides.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Komori K, Hirobe S, Toma M, et al. . A gastric duplication cyst of the pancreas associated with a bifid tail causing pancreatitis. J Ped Surg. 2013;1(10):368–72. [Google Scholar]
- 2.D'Journo XB, Moutardier V, Turrini O, et al. . Gastric duplication in an adult mimicking mucinous cystadenoma of the pancreas. J Clin Pathol. 2004;57(11):1215–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bailey CE, Fritz MB, Webb L, et al. . Gastric duplication cyst masquerading as a mucinous pancreatic cyst: Case report and literature review. Ann R Coll Surg Engl. 2014;96(1):88E–90E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Linder JD, Geenen JE, Catalano MF. Cyst fluid analysis obtained by EUS-guided FNA in the evaluation of discrete cystic neoplasms of the pancreas: A prospective single-center experience. Gastrointest Endosc. 2006; 64(5):697–02. [DOI] [PubMed] [Google Scholar]
- 5.Blinder G, Hiller N, Adler SN. A double stomach in an adult. Am J Gastroenterol. 1999;94(4):1100–2. [DOI] [PubMed] [Google Scholar]
- 6.Christians KK, Pappas S, Pilgrim C, et al. . Duplicate pancreas meets gastric duplication cyst: A tale of two anomalies. Int J Surg Case Rep. 2013;4(8):735–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuraoka K, Nakayama H, Kagawa T, et al. . Adenocarcinoma arising from a gastric duplication cyst with invasion to the stomach: A case report with literature review. J Clin Pathol. 2004;57(4):428–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewandrowski KB, Southern JF, Pins MR, et al. . Cyst fluid analysis in the differential diagnosis of pancreatic cysts. A comparison of pseudocysts, serous cystadenomas, mucinous cystic neoplasms, and mucinous cystadenocarcinoma. Ann Surg. 1993;217(1):41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pins MR, Compton CC, Southern JF, et al. . Ciliated enteric duplication cyst presenting as a pancreatic cystic neoplasm: Report of a case with cyst fluid analysis. Clin Chem. 1992;38(8):1501–03. [PubMed] [Google Scholar]


