Abstract
A 20-year-old male presented with 2 months of progressive abdominal distension due to ascites and Budd-Chiari syndrome. He underwent transjugular intrahepatic portosystemic shunt (TIPS) placement, but soon after had elevated liver enzymes. MRCP revealed mild left intrahepatic biliary dilatation without stones or obvious stricture. Endoscopic retrograde cholangiopancreatography (ERCP) demonstrated a focal stricture due to compression by the TIPS. The stricture was dilated and a 10 Fr x 15-cm plastic stent was placed with excellent biliary drainage. The patient's symptoms and liver tests normalized within 1 week. This is the first case of biliary obstruction due to TIPS placement effectively managed by ERCP.
Introduction
Transjugular intrahepatic portosystemic shunt (TIPS) is an effective therapy for refractory portal hypertension. Complications from TIPS most often consist of encephalopathy, infection, and renal failure.1 While biliary complications after TIPS are rare, the most frequent is the development of biliary-venous fistulas between the biliary system and the portal vein or newly placed TIPS.2-7 Biliary obstruction secondary to a TIPS placement is uncommon, with only 2 case reports describing such an occurrence, both ultimately requiring surgery.3,8
Case Report
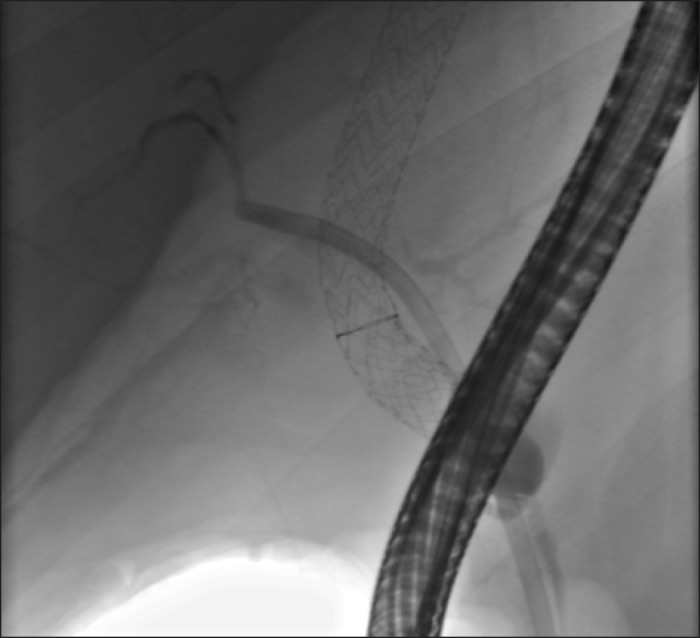
A 20-year-old male with splenomegaly and asthma presented with 2 months of progressive abdominal distension. His initial laboratory tests were notable for INR 1.6, platelets 139/µL, and total bilirubin 3.9 mg/dL. Computed tomography showed splenomegaly, ascites, advanced cirrhosis, and heterogeneous appearance of the liver with poor visualization of the hepatic veins, concerning for Budd-Chiari syndrome. Peritoneal fluid studies revealed a serum-ascites albumin gradient (SAAG) of 1.3 and total protein of 3.8. The patient was started on a heparin infusion. His hypercoaguable work-up was negative. Venography demonstrated multiple spider collaterals and a clot in the right hepatic vein with a hepatic venous pressure gradient (HVPG) of 24 mm Hg. Liver biopsy showed centrilobular necrosis with marked congestion of zone 3. The patient underwent TIPS placement with a decrease in HVPG from 18 mm Hg to 5 mm Hg (Figure 1).
Figure 1.
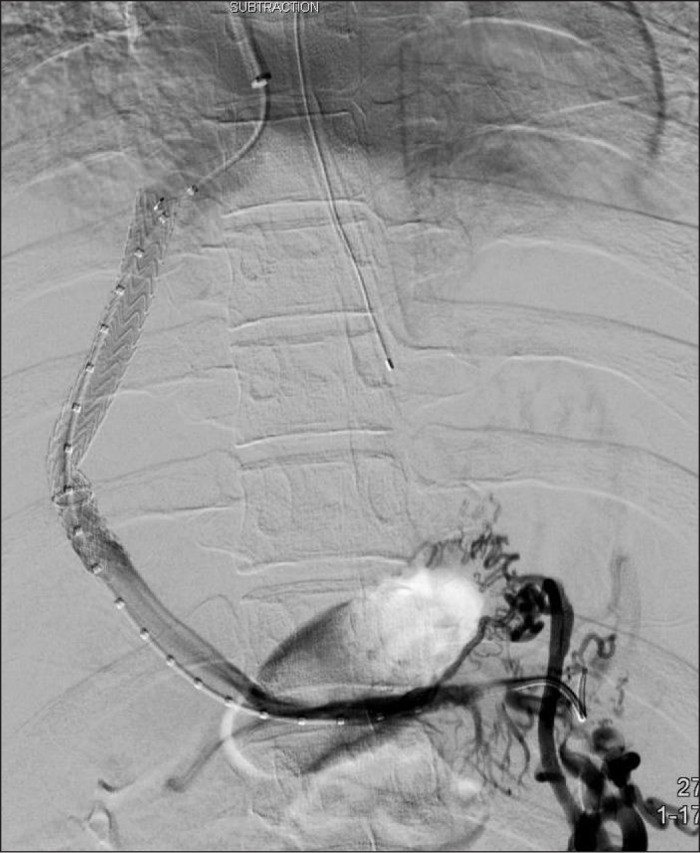
TIPS placement to decrease HVPG from 18 mm Hg to 5 mm Hg.
After TIPS placement, he was noted to have elevated liver enzymes in a cholestatic pattern. MRCP revealed mild intrahepatic ductal dilatation along with a caliber change or possible disruption in continuity of the left and right intrahepatic ducts at the level of the TIPS, thought to be from a focal stricture or possible biliary injury (Figure 2). ERCP showed stenosis at the takeoff of the left intrahepatic duct due to extrinsic compression from the TIPS (Figure 3). The stenosis was dilated (Figure 4), and a 7-French x 15-cm plastic stent was deployed without complications (Figure 5). His liver enzymes improved and his ascites resolved. The patient had a repeat ERCP 2 months later, and cholangiogram revealed persistent stenosis at the level of the TIPS with upstream biliary dilatation. A larger 10-French x 15-cm plastic stent was placed upstream of the stenosis, with plan for removal in 6 to 9 weeks.
Figure 2.
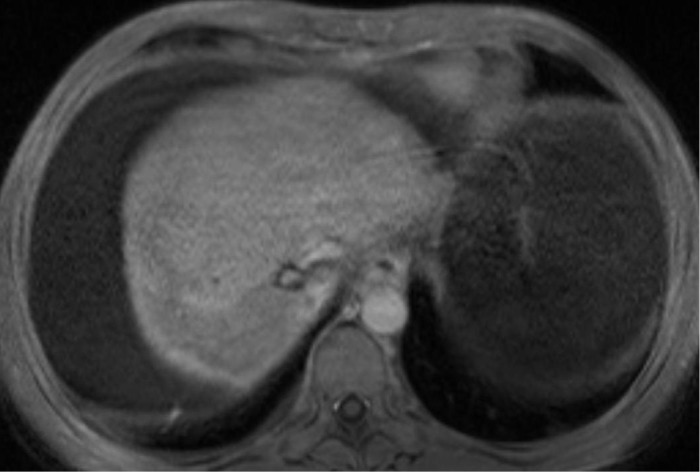
MRCP demonstrating mild intrahepatic ductal dilatation.
Figure 3.
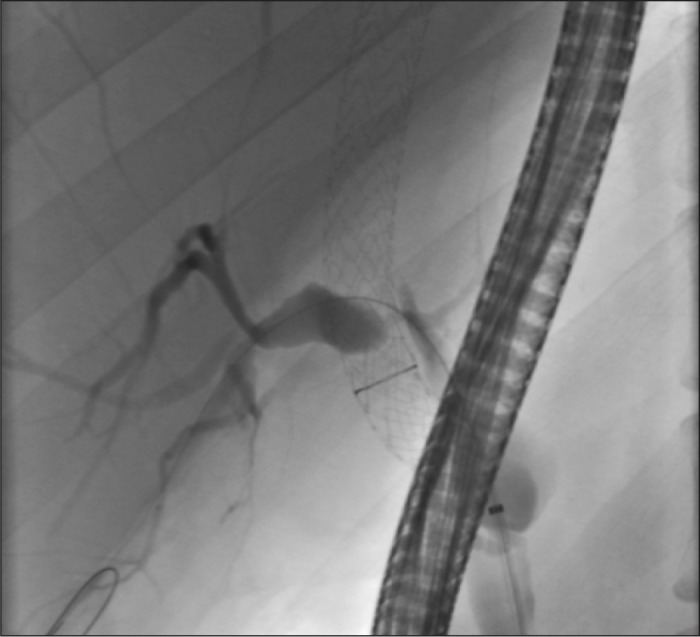
ERCP image demonstrating the stricture (non-filling portion) and dilated duct above.
Figure 4.
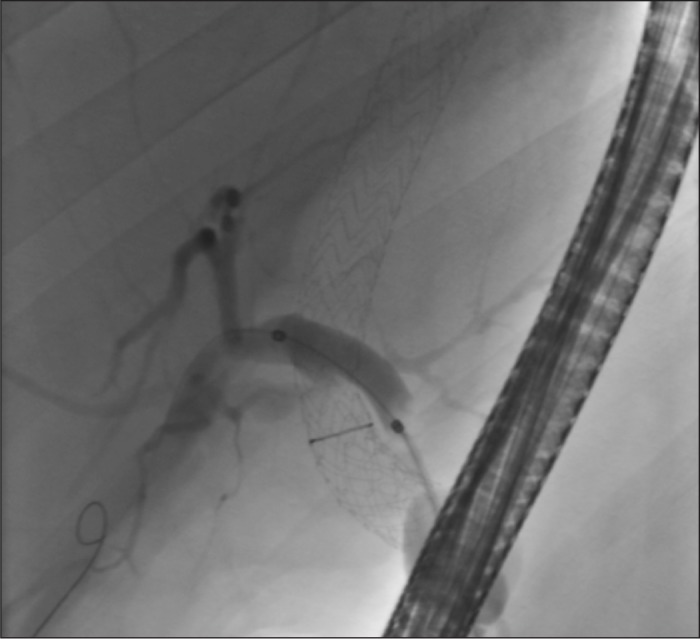
Balloon dilation of the stricture.
Figure 5.
Stent placement with effective drainage.
Discussion
TIPS is a common and effective method for the treatment of Budd-Chiari syndrome. Serious biliary complications from TIPS are rare and occur in less than 1% of cases. Reported biliary complications have included biliary-venous fistula, secondary sclerosing cholangitis, and biliary obstruction due to malpositioning of the TIPS. Of these complications, formation of a biliary-venous fistula is the most common and can lead to hemobilia. This may manifest clinically with elevated liver enzymes, biliary colic, melena, and ultimately cholangitis. This is differentiated from bilhemia (bile mixing with blood), which may present with hyperbilirubinemia, depending on the pressure gradient between the bile duct and hepatic vein. Hemobilia is typically managed with angiography and embolization, though ERCP can be diagnostic and allow biliary decompression. Bilhemia can be managed with ERCP, with transpapillary stent placement and/or sphincterotomy.
This is the first reported case of TIPS-associated biliary obstruction effectively managed by ERCP with stent placement. Biliary obstruction from mechanical compression of the biliary system should be considered in patients with elevated liver enzymes after TIPS placement.
Disclosures
Author contributions: P. Korrapati drafted the manuscript. K. Bidari and S. Komanduri edited the manuscript. S. Komanduri is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Boyer TD.Transjugular intrahepatic portosystemic shunt in the management of complications of portal hypertension. Curr Gastroenterol Rep. 2008;10(1):30–35. [DOI] [PubMed] [Google Scholar]
- 2.Silva RF, Arroyo PC Jr, Duca WJ, et al. Complications following transjugular intrahepatic portosystemic shunt: A retrospective analysis. Transplant Proc. 2004;36: 926–928. [DOI] [PubMed] [Google Scholar]
- 3.Paterno F, Khan A, Cavaness K, et al. Malpositioned transjugular intrahepatic portosystemic shunt in the common hepatic duct leading to biliary obstruction and liver transplantation. Liver Transpl. 2011;17(3):344–6. [DOI] [PubMed] [Google Scholar]
- 4.Singal AK, Kathuria MK, Malhotra A, et al. Bilhemia after transjugular intrahepatic portosystemic shunt and its management with biliary decompression. World J Gastroenterol. 2009;15(29):3681–3683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jawaid Q, Saeed ZA, Di Bisceglie AM, et al. Biliary-venous fistula complicating transjugular intrahepatic portosystemic shunt presenting with recurrent bacteremia, jaundice, anemia and fever. Am J Transplant. 2003;3(12):1604–1607. [DOI] [PubMed] [Google Scholar]
- 6.Willner IR, El-Sakr R, Werkman RF, et al. A fistula from the portal vein to the bile duct: An unusual complication of transjugular intrahepatic portosystemic shunt. Am J Gastroenterol. 1998;93: 1952–1955. [DOI] [PubMed] [Google Scholar]
- 7.Mallery S, Freeman ML, Peine CJ, et al. Biliary-shunt fistula following transjugular intrahepatic portosystemic shunt placement. Gastroenterology. 1996;111: 1353–1357. [DOI] [PubMed] [Google Scholar]
- 8.Duller D, Kniepeiss D, Lackner C, et al. Biliary obstruction as a complication of transjugular intrahepatic portosystemic shunt. Liver Transpl. 2009;15(5):556–557. [DOI] [PubMed] [Google Scholar]


