Abstract
Background
Reactivation of latent varicella zoster virus, partly due to age-related immunosenescence and immunosuppressive conditions, results in herpes zoster (HZ) and its associated complications. The management of the most important complication, post-herpetic neuralgia (PHN), is challenging, particularly in the elderly, and is generally unsatisfactory. No previous reviews have reported the incidence of HZ-associated mortality.
Methods
We carried out a systematic literature review to identify studies and databases providing data for HZ-associated mortality in adults aged ≥50 years in Europe.
Results
We identified 12 studies: Belgium (1); France (1); Germany (1); the Netherlands (2); Portugal (1); Spain (4) and England/Wales (2) and 4 databases from Europe: France; Germany and England/Wales. The incidence was available from eight studies; it was highest in those aged ≥95 in France (19.48/100,000). In the European (WHO) database, the overall mortality ranged from 0 to >0.07/100,000. The age- and gender-specific HZ mortality rates from the other databases showed that while in younger age groups the HZ mortality rate was higher in males, in older patients the rate was much higher in women. The case fatality rate was 2 and 61/100 000 in those 45–65 and ≥65 years, respectively. A similar increase with age was seen for the hospital fatality rate; 0.6% in those 45–65 years in the UK and 7.1% in those ≥80 in Spain.
Conclusions
Although the data were sparse and heterogeneous, HZ-associated mortality clearly increases with age. In addition, the elderly who develop HZ often have underlying diseases and are at increased risk of functional decline and loss of independence. Mortality should be taken into account in health-economics models.
Keywords: Herpes zoster, Varicella-zoster virus, Mortality, Europe
Background
Varicella-zoster virus (VZV) is a herpes virus that infects nearly all humans and causes two distinct diseases: varicella, the primary infection which usually occurs in childhood, and herpes zoster (HZ) which is the result of the reactivation of VZV which remains latent in the sensory ganglia following primary infection. This reactivation occurs when VZV-specific cellular-mediated immunity decreases, mainly due to age-related immunosenescence and immunosuppressive conditions.
HZ is characterized by a vesicular skin rash localized in the sensory region of the affected ganglia, and is often preceded, or accompanied by acute pain or itching. The individual lifetime risk of developing HZ is between 24% and 30%, or approximately 1 in 4 people [1-5]. However, for individuals aged 85 and over, this risk increases to 1 in 2 [6]. HZ incidence increases markedly after 50 years of age, with two-thirds of HZ cases occurring in individuals aged 50 years and over [7]. Anyone who has had varicella is at risk of HZ; in Europe varicella affects over 90% of children before the age of 15 [8].
HZ is painful during the acute phase, but pain may persist for months or even years. Post-herpetic neuralgia (PHN), defined as chronic pain persisting after rash onset, occurs in 20% to 50% of patients, and can lead to several months of treatment and loss of quality of life [9,10]. After 1 year, almost 10% of patients, mainly older people, still have persistent pain [11,12].
A recent literature review showed that the annual HZ incidence is similar throughout Europe, varying from 2.0 to 4.6/1 000 person-years, with no clear geographic trend [13]. Age-specific HZ incidence rates are around 1/1 000 children <10 years, around 2/1 000 adults aged <40 years, and around 1–4/1 000 adults aged 40–50 years, increasing to around 7–8/1 000 after age 50 years, up to 10/1 000 after 80 years of age. This review confirmed that, in Europe, HZ incidence increases with age, particularly after 50 years of age [13]. Similarly, data on the percentage of HZ cases who develop PHN are available across EU [14]. PHN, defined as HZ-associated pain lasting for at least three months, has been reported to occur in 10% to 20% of patients. However, the prevalence and severity of PHN increases with age, and has been reported to be as high as 60% to 70% of patients aged ≥60 [14]. In people aged over 50 years, there is a higher rate of HZ-associated hospitalization and HZ and PHN have a greater impact on the quality of life of patients and their relatives.
To date, a review of the data for HZ-associated mortality has not been published. To fill this gap and to have a complete picture of the burden of HZ and PHN, we performed a systematic literature review of data on HZ-associated mortality in people aged ≥50 years in Europe.
Methods
Objectives
The objective of this systematic literature review was to summarize the available data on the HZ-associated mortality in adults aged ≥50 years in Europe.
Search strategy
We searched PubMed from 1st January 1990 to 31 October 2013 using a combination of the following search terms as free text and medical subheading (MeSH) terms: mortality; death; case fatality rate; hospital fatality rate; Herpes Zoster [MeSh]; Herpes Zoster Ophthalmicus [MeSh]; Herpes Zoster Oticus [MeSh]; Encephalitis, Varicella Zoster [MeSh]; shingles, herpes zoster. We also scanned reference lists in selected publications to identify additional references, including publications known to the authors, not indexed on PubMed. No language restrictions were used.
In addition, European surveillance data, such as the European Detailed Mortality Database (DMDB) [15], national surveillance data, such as the CépiDc database from INSERM [16], the Office for National Statistics for England and Wales [17] and the German Federal Health Monitoring System [18] and the websites of the national health institutes and sentinel networks were searched.
The literature search was performed by one author (MH). The search results were downloaded into EndNote® for screening.
Inclusion and exclusion criteria
We included publications or websites/databases that provided HZ-associated mortality data for adults aged ≥50 years, irrespective of their health status, in any of the following European Union (EU) countries: Austria; Belgium; Bulgaria; Croatia; Cyprus; Czech Republic; Denmark; Estonia; Finland; France; Germany; Greece; Hungary; Ireland; Italy; Latvia; Lithuania; Luxembourg; Malta; the Netherlands; Norway; Poland; Portugal; Romania; Slovakia; Slovenia; Spain; Sweden; Switzerland; and United Kingdom. Case reports were excluded.
The HZ-associated mortality data could include: total number of HZ deaths; HZ-mortality incidence; HZ case fatality rate (CFR) or hospital fatality rate (HFR). The CFR was defined as the percentage of those who died among community-based cases and the HFR as the percentage of those who died among hospitalized cases.
Study selection process
The first round of screening was performed on the titles and abstracts by one author (MH) and another author (HB) verified the included and excluded publications. Full papers were obtained for the second round of screening that was performed by one author (MH) and verified by another (HB). The reasons for exclusion from this screening round were recorded (using broad categories, e.g. data not available for adults >50; population outside the defined EU countries). The search results were summarised using the PRISMA flow diagram (Figure 1) [19]. Papers reporting HZ-associated mortality data for countries outside Europe were kept for comparisons and discussion.
Figure 1.
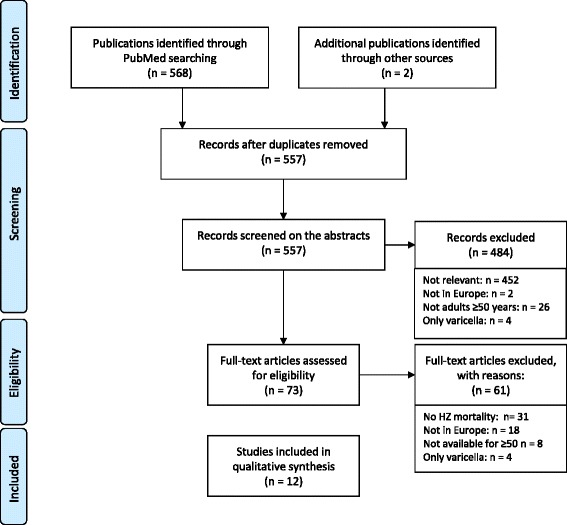
PRISMA diagram - summary of search results.
Quality assessment of included studies
As it was expected that there would not be many studies reporting HZ mortality rates, we decided to include all available data, without restrictions based on quality and to describe the quality of the data.
Data analyses
The following data were extracted from the included studies by one author (MH) and verified by another author (HB): country, date, data source, HZ diagnosis, mean age at HZ related death, presence of comorbidities and HZ mortality related data. In some studies where the available data allowed for estimation, the CFR or HFR were calculated by dividing the number of deaths by the number of HZ cases in the community or by the number of patients hospitalized with HZ, respectively. In addition, in studies where only the annual number of death at the national level was available, the age-specific mortality rate was estimated by obtaining the country age-specific population from the EuroStats database [20].
Results
Data sources identified
A total of 568 references were identified on PubMed and 2 were identified by the authors (Figure 1). Following removal of duplicate publications, 557 abstracts were first screened on titles and abstracts and 484 references were excluded. Full papers were obtained for the remaining 73 references; 12 of these satisfied the inclusion criteria for this review. The reasons for non-inclusion were: no HZ-associated mortality data available (31); not European data (18); not possible to have data for adults aged ≥50 years (8); only varicella (4).
The 12 studies included were from 7 countries: Belgium (1); France (1); Germany (1); the Netherlands (2); Portugal (1); Spain (4) and England and Wales (2) (Table 1) [2,21-31]. In addition, we identified four databases that provided HZ-associated mortality data from Europe (1); France (1); Germany (1) and England and Wales (1) (Table 2) [15-18]. A number of other mortality databases were identified but it was not possible to extract HZ-specific mortality [32].
Table 1.
Characteristics of included studies
| Study ID [ref] | Country/Dates | Data source | HZ diagnosis | Age (years) | Comorbidity | HZ-associated mortality data available or calculated* |
|---|---|---|---|---|---|---|
| Bilcke 2012 [21] | Belgium/1990-2007 | National death certificates | Code for HZ as possible cause of death (no indication of primary or associated) and independent evaluation by 5 experts | ≥60 | None | Overall incidence |
| Gonzalez Chiappe 2010 [27] | France/2000-2007 | National death certificate database (INSERM CepiDC: http://www.cepidc.inserm.fr/) | ICD-10 codes B020.0-B020.9 as primary or associated cause of death | 96.8% of deaths occurred in ≥65 | 21.6% had ≥1 underlying condition (59.6% malignancies, 12.5% diabetes, 10.9% blood dyscrasias and some immune deficiencies) | Age-specific incidence; disease-specific number of HZ deaths and hospital fatality rate* |
| Ultsch 2011 [30] | Germany/2007-2008 | Federal Health Monitoring database | ICD-10 codes of primary disease | ≥50 | None | Overall, and age- and gender-specific incidences and hospital fatality rate* |
| van Lier 2010 [31] | Netherlands/2000-2007 | National Statistics (CBS) database | ICD-10 codes B02 and G530 as primary cause of death | 92% of deaths in ≥75 | None | Number of HZ deaths; incidence of HZ mortality* |
| de Melker 2006 [23] | Netherlands/1996-2002 | National Statistics (CBS) database | ICD-10 code B02 as primary cause of death | 97% in ≥60 | None | Number of VZV deaths, incidence of HZ mortality* |
| Mesquita 2013 [28] | Portugal/2000-2010 | National Health Hospital Ministry Database | IDC-9 codes 053.10-13, 053.19-22, 053. 29, 053.71, 053.79, 053.8, 053.9 as primary diagnosis at hospital admission | All ages, with 10-year groups from 50 to 99 | None | In-hospital fatality rate (not available by gender) |
| Perez-Sola 2011 [29] | Spain/2000-2006 | Registry for drug safety in rheumatic patients treated with anti-TNF (100 Spanish health centres) | Microbiological diagnosis | 50 (mean; SD = 14) | Rheumatic diseases treated with TNF antagonists | Number of HZ deaths |
| Gil 2009 [24] | Spain/1998-2004 | National hospital discharge database (CMBD) | ICD-9 code for primary or secondary diagnosis: 0.53, 053.0-053.9 | 68.3 (SD = 15.5) for hospitalisations | None | Number of HZ deaths; age-specific hospital-mortality incidence; age-specific hospital fatality rate |
| Gil-Prieto 2011 [26] | Spain/1998-2004 | National hospital discharge database (CMBD) | ICD-9 code for primary or secondary diagnosis (053; 053.0-053.9) | >50 | 60.8% with diabetes, COPD and/or cardiovascular diseases, Exclusion of immunocompromised | Overall, age-specific and disease-specific hospital fatality rate |
| Gil-Prieto 2012 [25] | Spain/1997-2008 | National hospital discharge database (CMBD) | ICD-9-CM code for primary or secondary diagnosis for HZ ophthalmicus HZO 053.2, 053.20-22, 053.29 | >50; 50–59; 60–69; >70 | 25% immunocompromised (all ages) | Number of HZO deaths; HZO overall hospital-fatality rate; HZO age specific hospital-fatality rate |
| Comorbidities (cardiac chronic diseases, diabetes, COPD, asthma, chronic renal diseases) | ||||||
| Brisson 2003 [22] | England and Wales/1993-2000 | Hospitalisation Episode Statistics database (national) & Office for National Statistics (death certificates) | ICD-10 code B02 as primary diagnosis and ICD Code for HZ as cause of death | 45-64; 65+ | 8% with underlying conditions | Number of HZ deaths; Age-specific incidence; hospital-fatality rate |
| Edmunds 2001 [2] | England and Wales/1998 (1985–94; 1995–1999) | Hospitalisation Episode Statistics database (national) & Office for National Statistics (death certificates) | ICD-10 code B02 in any of the 7 diagnosis fields/ICD-9 code 053 death (no details for primary or associated) | 45+; and 5-year sub-groups | None | Age-specific mortality and case fatality rate |
*to indicate that these have been calculated.
Table 2.
Characteristics of included surveillance systems/databases
| Database name [Ref] | Region/dates covered | HZ diagnosis | HZ-associated mortality data available |
|---|---|---|---|
| WHO-DMDB [15] | Europe/2010, except Belgium and France: 2009 | ICD-10 code: B02 for primary cause of death | Age-specific and overall incidence by country |
| CépiDc [16] | France/2010 | ICD-10 code: B02 for primary cause of death | Age-specific incidence |
| Federal Health Monitoring System [18] | Germany/2011 and previous years | ICD-10 code: B02 and sub-codes | Number and incidence for overall and sex by year |
| Office for National Statistics [17] | England and Wales/2012 | ICD-10 code: B02 and sub-codes for underlying cause of death | Age-specific incidence |
Characteristics of studies and databases
Published studies
All the studies used databases to identify HZ-related deaths (Table 3). Five studies used national statistics databases that collected data from death certificates for the general population [21,23,27,30,31]. Four of the remaining studies used national hospital statistics databases, two used both types of database and the last used data from a drug safety register, BIOBADASER, that monitors patients with rheumatic diseases treated with biological agents in 100 Spanish health centres [2,22,24-26,28,29]. Three studies reported mortality data specifically for patients with underlying conditions [26,27,29]. Four studies presented mortality data for deaths with HZ as the primary cause, one with HZ as the primary diagnosis at hospital admission and three with HZ as primary or associated cause; the remaining four studies did not specify if HZ was the primary or associated cause. Five studies used International classification of diseases-10 (ICD-10) codes and five used ICD-9 codes to identify HZ-associated deaths. The study in Spain using a drug safety database was the only one that reported the use of microbiological confirmation of infection to diagnoses HZ [29]. For the other studies, no information on the use of microbiological confirmation of the HZ diagnosis was provided. Some hospital-based studies reported underlying conditions: one in France reported that 22% of patients had ≥1 underlying conditions and another in Spain reported that 25% of the patients were immunocompromised but they did not provide mortality data for these patients separately [25,27]. Eight of the studies provided age-specific HZ-associated mortality data [2,22,24-28,30].
Table 3.
HZ mortality data from included studies
| Study (ref) | Country | Period | Age (years) | Age at HZ-related death | Mortality incidence/100 000 (95% CI) | Case fatality rate (%) | Hospital fatality rate (%) | Number |
|---|---|---|---|---|---|---|---|---|
| Bilcke 2011 [21] | Belgium | 1990-2007 | 60-70 | 0.06 | ||||
| 70+ | 0.63 | |||||||
| Gonzalez Chiappe 2010 [27] | France | 2000-2007 | Overall | 96.8% (1360; 170/year) in those aged ≥65 years | 0.286 (0.244-0.328) | 0.075 | 2.012 | 1 405 (176 ± 13/year) |
| ≥65 | 4.36 ± 0.20 | |||||||
| 45-54 | 0.031 (0–0.069) | 0.007 | ||||||
| 55-64 | 0.072 (0.009-0.135) | 0.012 | ||||||
| 65-74 | 0.236 (0.102-0.370) | 0.027 | ||||||
| 75-84 | 1.25 (0.90-1.60) | 0.127 | ||||||
| 85-94 | 7.24 (5.66-8.82) | 0.672 | ||||||
| ≥95 | 19.48 (11.50-27.47) | 1.356 | HFR: Malignancies: 4.236 (449/10 599) HIV/AIDS: 0.357 (26/7 277) | |||||
| Diabetes: 1.654 (94/5 682) | ||||||||
| Blood dyscrasias: 3.907 (82/2 099) | ||||||||
| RA: 1.759 (38/2 160) | ||||||||
| Malnutrition: 6.196 (64/1 033) | ||||||||
| Organ transplant: 0.049 (1/2 023) | ||||||||
| Ultsch 2011 [30] | Germany | 2007-2008 | 50-54 | 73% (n = 48) deaths in ≥80 years | 0.02 (0.00-0.10) | 0.003 | 1 | |
| 55-59 | 0.00 NA | 0 | 0 | |||||
| 60-64 | 0.02 (0.00-0.13) | 0.003 | 1 | |||||
| 65-69 | 0.06 (0.01-0.17) | 0.005 | 3 | |||||
| 70-74 | 0.11 (0.04-0.27) | 0.010 | 5 | |||||
| 75-79 | 0.30 (0.14-0.57) | 0.025 | 9 | |||||
| 80-84 | 0.54 (0.28-0.94) | 0.043 | 12 | |||||
| 85-89 | 1.20 (0.67-1.98) | 0.096 | 15 | |||||
| ≥90 | 3.86 (2.36-5.96) | 0.293 | 20 | |||||
| Overall | 0.21 (0.16-0.26) | 0.022 | 66 | |||||
| van Lier 2010 [31] | Netherlands | 2000-2007 | ≥60 | 92% deaths occurred in ≥ 75 years | 0.59 (estimated with pop ≥60 from Eurostat) | Mean 18 deaths/year (range 13–26) | ||
| de Melker 2006 [23] | Netherlands | 1996-2002 | ≥75 | 97% occurred in ≥60 years | 1.92 (estimated with pop ≥75 from Eurostat) | Mean 18 deaths/year (range 13 to 26) | ||
| Mesquita 2013 [28] | Portugal | 2000-2010 | 50-59 | 76.8 years (SD = 13.6) | 1.0 | 17 (total) | ||
| 60-69 | 0.4 | |||||||
| 70-79 | 0.8 | |||||||
| 80-89 | 2.9 | |||||||
| 90-99 | 3.8 | |||||||
| Perez-Sola 2011 [29] | Spain | 2000-2006 | 0 | |||||
| Gil 2009 [24] | Spain | 1998-2004 | 50-59 | 0.3 | 3.8 | 156/year (mean) | ||
| 60-69 | 0.6 | 3.7 | ||||||
| 70-79 | 1.5 | 4.5 | ||||||
| ≥80 | 3.9 | 7.1 | ||||||
| Gil-Prieto 2011 [26] | Spain | 1998-2004 | 50-59 | 3.0*/1.1 | ||||
| 60-69 | 2.7*/1.7 | |||||||
| ≥70 | 5.3*/2.7 | |||||||
| 50-59 | No comorbidity: 1.1 | |||||||
| Comorbidity: 3.0 | ||||||||
| Diabetes: 3.0 | ||||||||
| COPD: 4.2 | ||||||||
| CVD: 3.7 | ||||||||
| 60-69 | No comorbidity: 1.7 | |||||||
| Comorbidity: 2.7 | ||||||||
| Diabetes: 1.9 | ||||||||
| COPD: 2.7 | ||||||||
| CVD: 3.4 | ||||||||
| ≥70 | No comorbidity: 2.7 | |||||||
| Comorbidity: 5.3 | ||||||||
| Diabetes: 5.0 | ||||||||
| COPD: 5.0 | ||||||||
| CVD: 5.9 | ||||||||
| Gil-Prieto 2012 [25] | Spain | 1997-2008 | First diagnosis | |||||
| ≥50§ | 2.51§ (1.42-3.61)/ | 20 | ||||||
| ≥50# | 1.62# (0.67-2.5) | 11 | ||||||
| 50-59 | ||||||||
| 60-69 | 0/0 | 0§/0# | ||||||
| ≥70 | 1.16§ (0–0.76)/0# | 2§/0# | ||||||
| 3.61§ (1.97-6.25)/ | 18§/11# | |||||||
| 2.48# (1.03-3.93) | ||||||||
| All ages | 22§/11# | |||||||
| 1.89§ (1.1-1.27)/ | ||||||||
| 1.22# (1.9-5.0) | ||||||||
| Any diagnosis: | ||||||||
| ≥50 | 117§/70# | |||||||
| 50-59 | 4§/1# | |||||||
| 60-69 | 16§/3# | |||||||
| ≥70 | 97§/66# | |||||||
| Brisson 2003 [22] | England & Wales | 1991-2000 | 45-64$ | 0.014 | 0.002 | 0.612 | 2$ | |
| ≥65$ | 0.566 | 0.061 | 3.190 | 47 | ||||
| all ages$$ | 0.094 | 0.031 | 2.722) | 49 | ||||
| Edmunds 2001 [2] | England & Wales | 1995-1999 | ≥60 | 2.0 – 4.0 | ||||
| 50-54 | 0.009 | |||||||
| 55-59 | 0.009 | |||||||
| 60-64 | 0.027 | |||||||
| 65-69 | 0.027 | |||||||
| 70-74 | 0.035 | |||||||
| 75-79 | 0.092 | |||||||
| 80-84 | 0.487 | |||||||
| ≥85 | 2.018 |
*in those with diabetes, COPD and cardiovascular; § all; #immuno-competent; $data from national statistics; $$ HES data base.
Databases
We identified four databases that provided age-specific HZ mortality data (Table 2) [15-18]. Three of these databases were country-specific (France, Germany and United Kingdom (England and Wales)); the fourth database provided data for all European countries. As the national databases all contributed their data to the European database, we did not analyse their data, but extracted the data from the European database. This European database used International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) code (B02) for all countries included in this review, except for Greece, which used ICD-9 codes, but there was no HZ mortality data available for Greece. We extracted HZ mortality data corresponding to people aged ≥50 years on 7 March 2014.
HZ-associated mortality
Overall and age-specific incidence rates
Eight of the studies provided HZ-mortality rates or provided data that could be used to estimate the mortality rates [2,21-23,27,28,30,31]. The age groups used were different between the studies but the overall trend was always towards a higher mortality incidence rate in the older age groups (Figure 2A). The mortality rates ranged from 0 in those aged 55–59 years in Germany to 19.5/100 000 for those aged ≥95 years in France [27,30].
Figure 2.
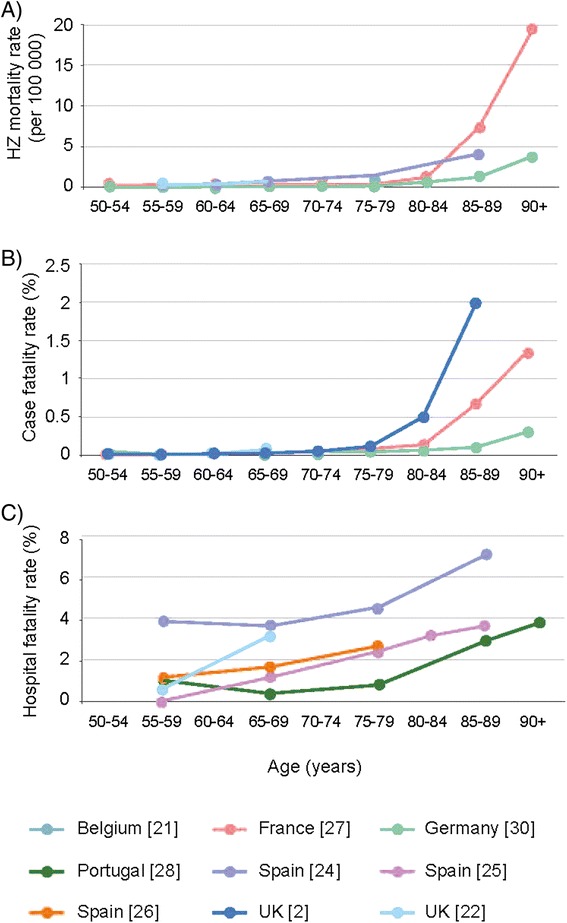
Mortality data from published studies: A) HZ mortality rate by age (years); B) HZ case fatality rate by age (years); C) HZ hospital fatality rate by age (years).
The data from the World Health Organisation (WHO) database showed that the estimates for the overall HZ mortality incidence in those aged ≥50 years varied widely between the countries for which estimates were available in 2011, ranging from 0.002 in Poland to 0.070 per 100 000 in Denmark, with a median of 0.039 per 100 000 (Figure 3) [15]. In countries where data are available for >1 year, although there were variations over time there did not seem to be any particular increasing or decreasing trends in the HZ mortality rate overall or for those aged 50–69 or ≥70 years (data not shown). The HZ mortality rate varied by gender and was generally higher in women, although in Spain, Italy, France and, particularly, Denmark, the mortality rate was higher in men (Figure 4).
Figure 3.
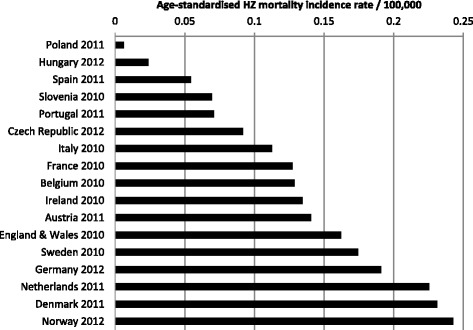
Age-standardized HZ mortality rate per 100 000 in all adults aged ≥50 years [15].
Figure 4.
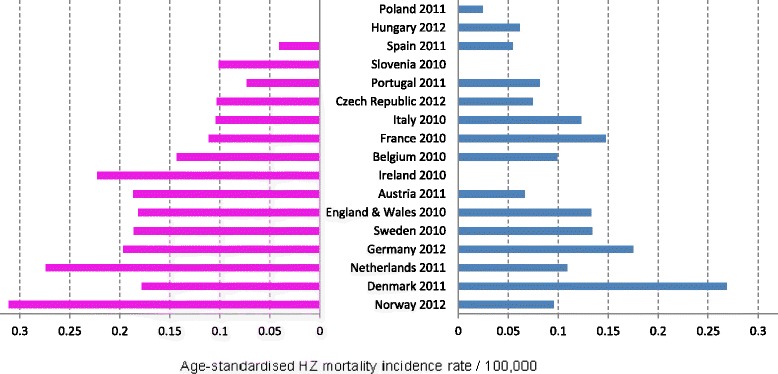
Age-standardized HZ mortality rate per 100 000 in females (left) and males (right) aged ≥50 years [15].
Despite the between-countries differences in rates, there was a trend towards higher mortality rates in older age groups in all countries, with the increase occurring from the age of 70–74 years (Figure 5).
Figure 5.
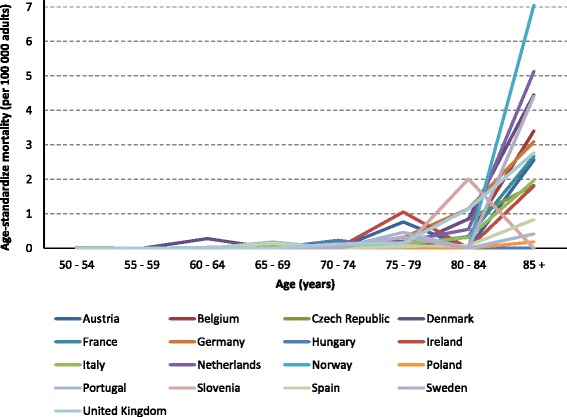
Age-standardized HZ mortality rate per 100 000 in adults by age group in the European countries [15].
Age-specific case fatality and hospital fatality rates
Eight of the studies provided data to be used to estimate age-specific CFR (3), HFR (4) both (1) [2,22,24-28,30]. The age groups analysed varied between the studies but the overall trend was towards much higher rates in older age groups. The studies from UK provided estimation of CFRs that were around 2/100 000 in those aged 45 to 65 years old; and 61/100 000 in those aged ≥65. The CFR was available in four studies and varied from 0 in those aged 55–59 years in Germany to 2.02% in those aged ≥85 years in England and Wales (Figure 2B). The HFR was available in five studies and varied from 0.4% in those aged 60–69 years in Portugal to 7.1% in those aged >80 years in Spain (Figure 2C). The HFRs reported in Spain were higher than in other countries where the HFR was generally under 1% until the age of 75 to 85 years. Data from the two studies that provided fatality rates for sub-groups of patients with underlying conditions showed that there was a higher fatality rate in these populations [26,27]. In one of the studies, the fatality rate was also reported to increase with age in these populations [26]. One study in patients with ophthalmic HZ reported HFRs of 2.5% and 1.6% in those aged ≥50 in the overall population and in immunocompetent patients, respectively [25].
Discussion
The results from this review show that HZ-associated mortality rate is generally low and, that despite the data being heterogeneous, in all studies mortality increased with age. Globally HZ-associated mortality is very low (<0.1/100 000) in those aged under 70 to 75 years and increases in older people, reaching between 1.2 to 7.2/100 000 in those aged ≥85 years. Not all studies reported trends in HZ mortality incidence over time, but one study in England and Wales reported a reduction in HZ-associated mortality over the 90's [22]. The overall EU data from the Detailed Mortality Database (DMDB) showed variations over time for those aged 50–69 years and those aged ≥70 years. However, the HZ mortality rate did not appear to increase or decrease from 1994 to 2012.
Similar to the EU data reported here, data from the US, for 1979 to 2007, showed that the HZ mortality rate was higher in older patients; an average of 134 deaths were recorded with HZ as the underlying cause, and 45% of these occurred in those aged ≥85 years [33]. The overall age-adjusted HZ-mortality was reported to decrease by 42% from 7.8 to 4.5 per 100 000. In another study in the US, from 1986 to 1995 the overall HZ-HFR was 5.3%; in those with underlying conditions the HFR was 8.7%, compared with 3.7% in those without [34]. In Australia, it was also reported to be higher in older people and women; 219 of the 238 (92%) deaths with HZ as the primary cause recorded from 1971 to 1993; (219) were in people aged >65 years and 65% were women [35]. Also the overall crude HZ mortality incidence was stable over this period (0.068 per 100 000); 0.043 and 0.092 per 100 000 in men and women, respectively. In another study in Australia, from July 1998 to June 1999 the overall HZ-HFR was 4% (186/4718) [36]. The HFR was higher in those with HZ as a secondary diagnosis compared with those with HZ as a primary diagnosis: 6% vs. 1%.
Mortality rates were higher when HZ was reported to be an associated or secondary cause of death suggesting that the HZ episode could have an indirect role in mortality [37]. Underlying comorbidities can increase the severity of the HZ episode and thus the risk of mortality [24]. It has been estimated that the risk of dying was five-times higher within three years of HZ reactivation than in age-matched controls that had not had HZ [27]. Diagnosis of HZ infection can increase the risk of subsequent diagnosis of diseases such as cancer, cerebrovascular disease or myocardial infarction and HIV [38-40]. In addition, hospitalisation of elderly people for acute diseases can result in functional decline and loss of autonomy [41-43].
It is important to be cautious when making comparisons between countries given the differences in study methodologies and coding practices in each country. Also, the data are presented for differing age groups, some of which are very large, making comparisons between studies difficult. In particular, some data are given for patients aged ≥65 years when we know that HZ-associated mortality rates are very different between those aged 65 to 75 years and those aged ≥85 years.
The differences in case definitions used could account for a substantial part of the heterogeneity. Most studies used clinical diagnosis for HZ, without requiring laboratory confirmation. In an elderly population, with many patients presenting underlying conditions or other comorbidities, it is difficult for a physician to be certain about the causal relationship between HZ and death, particularly if the certifying physician does not have access to all the patient’s medical records and autopsy results.
It is possible that the variations in the HZ-HFR are due to differences in the numerator since HZ hospitalisation rates may vary between countries due to different healthcare pathways, healthcare seeking behaviours, or perception of symptoms. In addition, differences in coding practices could contribute to this heterogeneity. Although only four studies in this review reported CFRs, there was less heterogeneity observed; it has been reported that HZ incidence rates do not vary between European countries [13]. Other factors such as differences in the prevalence of underlying risk factors for severe illness, differences in comorbidity rates or some other unidentified factors in different populations may also contribute to the observed heterogeneity.
Although most studies used HZ codes on death certificates for the primary cause of death, some used the codes for either primary or associated causes of death. Some of the limitations of using death certificates for estimating mortality incidence include incompleteness and errors. In the US, an assessment of the hospital records for decedents, whose death certificate recorded HZ as the underlying cause of death, showed that HZ was the underlying cause in only 52.5% (21/40) of cases and a contributing cause in another 12.5% (5/40) [33]. Other studies have reported that use of electronic or paper death certificates can lead to underestimations or overestimates of the true mortality rate due to other infectious and non-infectious diseases [44-47].
The strengths of our review include the fact that many studies and databases provide mortality data from national databases thus providing data for the whole population. However, there are some limitations. For example, the data are not from patient-level longitudinal prospective studies and, therefore, the retrospective design of the studies could reduce the accuracy of the data and provide an underestimation of the burden of HZ mortality. Some studies only reported mortality with HZ as the primary cause, whereas it has been suggested that the mortality is higher when HZ is an associated or contributory cause of mortality [36]. In addition, there were not much data available and there was a range of methods used for the estimations.
Six European Union countries have national surveillance systems and five have sentinel systems for HZ [32]. In the future, access to these surveillance databases should improve the quality of data concerning the incidence of HZ in Europe. In addition, the recent initiatives to harmonise coding for death certificates within Europe should play an important role in future HZ surveillance programmes, in particular by improving the comparability of data sources [48]. The initiatives are important for the evaluation of the impact of infant varicella vaccination and adult HZ vaccination on HZ incidence and mortality rates.
Conclusions
In conclusion, although the available data on HZ-associated mortality are too heterogeneous to allow inter-country comparisons, they demonstrate that the mortality rate for HZ is not high, especially in younger people. However, mortality rates increase with age, particularly in those aged ≥75 years who often have underlying diseases and are at risk of functional decline and loss of independence if they are hospitalised.
Acknowledgements
The review was funded by Sanofi Pasteur MSD who commercialise the herpes zoster vaccine (ZOSTAVAX®) in Europe. They did not have a role in the design, in the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication. HB is employed by Sanofi Pasteur MSD; MH received consultancy fees for this project from Sanofi Pasteur MSD and was formerly employed by Sanofi Pasteur MSD; OO and RGP did not receive any funding for their participation in this review.
Abbreviations
- CFR
Case fatality rate
- DMDB
Detailed Mortality Database
- EU
European Union
- HFR
Hospital fatality rate
- HZ
Herpes zoster
- ICD
International classification of diseases
- MeSH
Medical Subheading
- PHN
Post-herpetic neuralgia
- VZV
Varicella-zoster virus
- WHO
World Health Organisation
Footnotes
Competing interests
HB is employed by Sanofi Pasteur MSD who commercialise the herpes zoster vaccine (ZOSTAVAX®) in Europe; MH received consultancy fees for this project from Sanofi Pasteur MSD and was formerly employed by Sanofi Pasteur MSD; OO and RGP declare that they have no competing interests.
Authors’ contributions
HB conceived the systematic review; HB and MH developed the review protocol; all authors validated the protocol; MH performed the literature search, selection of studies and data extraction; HB validated the included and excluded studies; OO and RGP validated the included studies; HB, OO and RGP validated the extracted data; MH wrote the first draft of the manuscript; all authors critically reviewed the drafts of the manuscript for important intellectual content; all authors have given final approval of the version to be published; all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Contributor Information
Hélène Bricout, Email: hbricout@spmsd.com.
Margaret Haugh, Email: mhaugh@medicom-consult.com.
Olugbenga Olatunde, Email: olugbenga.olatunde@ons.gsi.gov.uk.
Ruth Gil Prieto, Email: ruth.gil@urjc.es.
References
- 1.Guidelines for the management of shingles. report of a working group of the British Society for the Study of Infection (BSSI). J Infect. 1995;30:193-200. [PubMed]
- 2.Edmunds WJ, Brisson M, Rose JD. The epidemiology of herpes zoster and potential cost-effectiveness of vaccination in England and Wales. Vaccine. 2001;19:3076–90. doi: 10.1016/S0264-410X(01)00044-5. [DOI] [PubMed] [Google Scholar]
- 3.Gross G, Schofer H, Wassilew S, Friese K, Timm A, Guthoff R, Pau HW, Malin JP, Wutzler P, Doerr HW. Herpes zoster guideline of the German Dermatology Society (DDG) J Clin Virol. 2003;26:277–89. doi: 10.1016/S1386-6532(03)00005-2. [DOI] [PubMed] [Google Scholar]
- 4.Lee VK, Simpkins L. Herpes zoster and postherpetic neuralgia in the elderly. Geriatr Nurs. 2000;21:132–5. doi: 10.1067/mgn.2000.108260. [DOI] [PubMed] [Google Scholar]
- 5.Thiry N, Beutels P, Shkedy Z, Vranckx R, Vandermeulen C, Wielen MV, Damme PV. The seroepidemiology of primary varicella-zoster virus infection in Flanders (Belgium) Eur J Pediatr. 2002;161:588–93. doi: 10.1007/s00431-002-1053-2. [DOI] [PubMed] [Google Scholar]
- 6.Schmader K. Herpes zoster in older adults. Clin Infect Dis. 2001;32:1481–6. doi: 10.1086/320169. [DOI] [PubMed] [Google Scholar]
- 7.Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, Sy LS. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007;82:1341–9. doi: 10.4065/82.11.1341. [DOI] [PubMed] [Google Scholar]
- 8.Sengupta N, Breuer J. A global prospective of the epidemiology and burden of varicella-zoster-virus. Curr Ped Rev. 2009;5:207–28. doi: 10.2174/157339609791317315. [DOI] [Google Scholar]
- 9.Hannouche D, Alfandari S, Bouhour D, Fouchard N, Geffray L, Quinet B. Management of VZV infections [Prise en charge des infections à VZV] Med Mal Infect. 1998;28:1. doi: 10.1016/S0399-077X(98)80102-9. [DOI] [Google Scholar]
- 10.Johnson RW, Wasner G, Saddier P, Baron R. Postherpetic neuralgia: epidemiology, pathophysiology and management. Expert Rev Neurother. 2007;7:1581–95. doi: 10.1586/14737175.7.11.1581. [DOI] [PubMed] [Google Scholar]
- 11.Scott FT, Johnson RW, Leedham-Green M, Davies E, Edmunds WJ, Breuer J. The burden of Herpes Zoster: a prospective population based study. Vaccine. 2006;24:1308–14. doi: 10.1016/j.vaccine.2005.09.026. [DOI] [PubMed] [Google Scholar]
- 12.Scott FT, Leedham-Green ME, Barrett-Muir WY, Hawrami K, Gallagher WJ, Johnson R, Breuer J. A study of shingles and the development of postherpetic neuralgia in East London. J Med Virol. 2003;70(Suppl 1):S24–30. doi: 10.1002/jmv.10316. [DOI] [PubMed] [Google Scholar]
- 13.Pinchinat S, Cebrian-Cuenca AM, Bricout H, Johnson RW. Similar herpes zoster incidence across Europe: results from a systematic literature review. BMC Infect Dis. 2013;13:170. doi: 10.1186/1471-2334-13-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mick G, Hans G. Postherpetic neuralgia in Europe: the scale of the problem and outlook for the future. J Clin Gerontol Geriatr. 2013;4:102–8. doi: 10.1016/j.jcgg.2013.03.001. [DOI] [Google Scholar]
- 15.European Detailed Mortality Database. [http://data.euro.who.int/dmdb/]
- 16.French Mortality Database: CepiDc. [http://www.cepidc.inserm.fr/site4/]
- 17.Office for National Statistics (England and Wales). [http://www.statistics.gov.uk]
- 18.German Federal Health Monitoring System. [http://www.gbe-bund.de/gbe10/pkg_navigation.prc_sitemap?p_uid=gast&p_aid=&p_sprache=E&p_help_context=H_HOME]
- 19.PRISMA Statement website. [http://www.prisma-statement.org/].
- 20.Eurostat. [http://ec.europa.eu/eurostat/tgm/table.do?tab=table&init=1&language=en&pcode=tps00001&plugin=1]
- 21.Bilcke J, Marais C, Ogunjimi B, Willem L, Hens N, Beutels P. Cost-effectiveness of vaccination against herpes zoster in adults aged over 60 years in Belgium. Vaccine. 2012;30:675–84. doi: 10.1016/j.vaccine.2011.10.036. [DOI] [PubMed] [Google Scholar]
- 22.Brisson M, Edmunds WJ. Epidemiology of Varicella-Zoster Virus in England and Wales. J Med Virol. 2003;70(Suppl 1):S9–14. doi: 10.1002/jmv.10313. [DOI] [PubMed] [Google Scholar]
- 23.de Melker H, Berbers G, Hahne S, Rumke H, van den Hof S, de Wit A, Boot H. The epidemiology of varicella and herpes zoster in The Netherlands: implications for varicella zoster virus vaccination. Vaccine. 2006;24:3946–52. doi: 10.1016/j.vaccine.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 24.Gil A, Gil R, Alvaro A, San Martin M, Gonzalez A. Burden of herpes zoster requiring hospitalization in Spain during a seven-year period (1998–2004) BMC Infect Dis. 2009;9:55. doi: 10.1186/1471-2334-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gil-Prieto R. The Burden of Hospitalisations for Herpes Zoster Ophtalmicus in Spain (1997–2008) World J Vaccines. 2012;02:164–71. doi: 10.4236/wjv.2012.23022. [DOI] [Google Scholar]
- 26.Gil-Prieto R, San Martin M, Alvaro-Meca A, Gonzalez-Lopez A, Gil de Miguel A. Herpes zoster hospitalizations of patients with chronic illnesses in Spain, 198–2004. Vacunas. 2011;12:95–101. doi: 10.1016/S1576-9887(11)70013-9. [DOI] [Google Scholar]
- 27.Gonzalez Chiappe S, Sarazin M, Turbelin C, Lasserre A, Pelat C, Bonmarin I, Chosidow O, Blanchon T, Hanslik T. Herpes zoster: burden of disease in France. Vaccine. 2010;28:7933–8. doi: 10.1016/j.vaccine.2010.09.074. [DOI] [PubMed] [Google Scholar]
- 28.Mesquita M, Froes F. Hospital admissions for herpes zoster in portugal between 2000 and 2010. Acta Med Port. 2013;26:531–6. [PubMed] [Google Scholar]
- 29.Perez-Sola MJ, Torre-Cisneros J, Perez-Zafrilla B, Carmona L, Descalzo MA, Gomez-Reino JJ. Infections in patients treated with tumor necrosis factor antagonists: incidence, etiology and mortality in the BIOBADASER registry. Med Clin (Barc) 2011;137:533–40. doi: 10.1016/j.medcli.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 30.Ultsch B, Siedler A, Rieck T, Reinhold T, Krause G, Wichmann O. Herpes zoster in Germany: quantifying the burden of disease. BMC Infect Dis. 2011;11:173. doi: 10.1186/1471-2334-11-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Lier A, van der Maas NA, Rodenburg GD, Sanders EA, de Melker HE. Hospitalization due to varicella in the Netherlands. BMC Infect Dis. 2011;11:85. doi: 10.1186/1471-2334-11-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varicella and herpes zoster surveillance and vaccination recommendations 2010–2011 [http://venice.cineca.org/report_final_varicella.pdf]
- 33.Mahamud A, Marin M, Nickell SP, Shoemaker T, Zhang JX, Bialek SR. Herpes zoster-related deaths in the United States: validity of death certificates and mortality rates, 1979–2007. Clin Infect Dis. 2012;55:960–6. doi: 10.1093/cid/cis575. [DOI] [PubMed] [Google Scholar]
- 34.Lin F, Hadler JL. Epidemiology of primary varicella and herpes zoster hospitalizations: the pre-varicella vaccine era. J Infect Dis. 2000;181:1897–905. doi: 10.1086/315492. [DOI] [PubMed] [Google Scholar]
- 35.Chant KG, Sullivan EA, Burgess MA, Ferson MJ, Forrest JM, Baird LM, Tudehope DI, Tilse M. Varicella-zoster virus infection in Australia. Aust N Z J Public Health. 1998;22:413–8. doi: 10.1111/j.1467-842X.1998.tb01405.x. [DOI] [PubMed] [Google Scholar]
- 36.MacIntyre CR, Chu CP, Burgess MA. Use of hospitalization and pharmaceutical prescribing data to compare the prevaccination burden of varicella and herpes zoster in Australia. Epidemiol Infect. 2003;131:675–82. doi: 10.1017/S0950268803008690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.DeLaGarza VW, Arbogast JG, Podolinski CF, Gunel E. Reactivation of herpes zoster (shingles) infection associated with an increased risk of death in immunocompetent older persons. W V Med J. 2008;104:22–4. [PubMed] [Google Scholar]
- 38.Sogaard OS, Lohse N, Ostergaard L, Kronborg G, Roge B, Gerstoft J, Sorensen HT, Obel N. Morbidity and risk of subsequent diagnosis of HIV: a population based case control study identifying indicator diseases for HIV infection. PLoS One. 2012;7:e32538. doi: 10.1371/journal.pone.0032538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Breuer J, Pacou M, Gauthier A, Brown MM. Herpes zoster as a risk factor for stroke and TIA: a retrospective cohort study in the UK. Neurology. 2014;82:206–12. doi: 10.1212/WNL.0000000000000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sreenivasan N, Basit S, Wohlfahrt J, Pasternak B, Munch TN, Nielsen LP, Melbye M. The short- and long-term risk of stroke after herpes zoster - a nationwide population-based cohort study. PLoS One. 2013;8:e69156. doi: 10.1371/journal.pone.0069156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.de Saint-Hubert M, Schoevaerdts D, Poulain G, Cornette P, Swine C. Risk factors predicting later functional decline in older hospitalized patients. Acta Clin Belg. 2009;64:187–94. doi: 10.1179/acb.2009.034. [DOI] [PubMed] [Google Scholar]
- 42.Hoogerduijn JG, Schuurmans MJ, Duijnstee MS, de Rooij SE, Grypdonck MF. A systematic review of predictors and screening instruments to identify older hospitalized patients at risk for functional decline. J Clin Nurs. 2007;16:46–57. doi: 10.1111/j.1365-2702.2006.01579.x. [DOI] [PubMed] [Google Scholar]
- 43.Vidan Astiz MT, Sanchez Garcia E, Alonso Armesto M, Montero Errasquin B, Martinez de la Casa A, Ortiz FJ, Serra Rexach JA. Functional decline during hospitalization in elderly patients. Benefits of admission to the geriatrics service. Rev Esp Geriatr Gerontol. 2008;43:133–8. doi: 10.1016/S0211-139X(08)71172-7. [DOI] [PubMed] [Google Scholar]
- 44.Agarwal R, Norton JM, Konty K, Zimmerman R, Glover M, Lekiachvili A, McGruder H, Malarcher A, Casper M, Mensah GA, Thorpe L. Overreporting of deaths from coronary heart disease in New York City hospitals, 2003. Prev Chronic Dis. 2010;7:A47. [PMC free article] [PubMed] [Google Scholar]
- 45.Fox CS, Evans JC, Larson MG, Kannel WB, Levy D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: the Framingham Heart Study. Circulation. 2004;110:522–7. doi: 10.1161/01.CIR.0000136993.34344.41. [DOI] [PubMed] [Google Scholar]
- 46.Hunt LW, Jr, Silverstein MD, Reed CE, O'Connell EJ, O'Fallon WM, Yunginger JW. Accuracy of the death certificate in a population-based study of asthmatic patients. JAMA. 1993;269:1947–52. doi: 10.1001/jama.1993.03500150059027. [DOI] [PubMed] [Google Scholar]
- 47.Bancroft EA, Lee S. Use of electronic death certificates for influenza death surveillance. Emerg Infect Dis. 2014;20:78–82. doi: 10.3201/eid.2001.130471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.European Parliament Commission Regulation (EU) No 328/2011 of 5 April 2011. OJ. 2011;L90:22–24. [Google Scholar]


