Abstract
We studied associations between two pediatrics primary care interventions promoting parental responsiveness and maternal depressive symptoms among low-income mothers. This RCT included two interventions (Video Interaction Project [VIP], Building Blocks [BB]) and a control group. VIP is a relationship-based intervention, using video-recordings of mother-child dyads to reinforce interactional strengths. BB communicates with parents via parenting newsletters, learning materials and questionnaires. At mean (SD) child age 6.9 (1.2) months, depressive symptoms were assessed with the PHQ-9, parental responsiveness was assessed with StimQ-I. 407 dyads were assessed. Rates of mild depressive symptoms were lower for VIP (20.6%) and BB (21.1%) than Controls (32.1%, p=.04). Moderate depressive symptoms were lower for VIP (4.0%) compared to Controls (9.7%, p=.031). Mean PHQ-9 scores differed across 3 groups (F=3.8, p=.02): VIP mothers scored lower than controls (p=.02 by Tukey hsd). Parent-child interactions partially mediated VIP-associated reductions in depressive symptoms (indirect effect −.17, 95% CI −.36, −.03).
Keywords: Parenting, Maternal Depressive Symptoms, Intervention, Pediatrics
INTRODUCTION
Maternal depression places children at risk for a broad range of adverse developmental outcomes manifesting early in infancy, including delays in early communication1 and insecure attachment2. The impact of maternal depression is especially significant for children growing up in poverty for a number of reasons. First, depressive symptoms are found in approximately 25-35% of low-income families, compared to approximately 10-15% of families with greater resources3,4. Second, poverty is associated with reduced mother-infant interactions1 and adverse child outcomes5 in general, and depression additionally magnifies risks to mother-child dyads6. Third, low income mothers with depressive symptoms are less likely to seek help, posing a challenge to delivery of effective treatment7. As a result, depression’s impacts on child outcomes in the context of poverty represent a highly challenging problem.
Maternal depression in the context of poverty and associated stressors and risks (e.g., limited social support, low education and literacy, and material hardship) poses challenges to meeting the demands of child-rearing8. Two areas of specific challenge relate to: 1) mothers’ perceptions of their own parenting skills, and 2) mothers’ ability to understand and cope with their children’s developmental and behavioral issues. Regarding the former, depressed mothers are more likely to have lower self-efficacy and feelings of competence9,10, as well as an external locus of control in which they perceive others to have the greatest impact on their children11,12. Regarding the latter, depressed mothers are more likely to negatively interpret their children’s behaviors13. For example, depressed mothers have significant difficulty coping with typical behaviors such as crying, and are more likely to perceive their infants to have colic or a difficult temperament14-16. Interestingly, relationships between depression and parenting-challenges appear to be bi-directional. For example, mothers’ perceived feelings of inadequate self-efficacy and perceptions of their infants as presenting difficult temperaments have also been shown to lead to depressive symptoms17.
Of critical importance is the significant negative impact of maternal depressive symptoms on child developmental outcomes, even in the presence of sub-threshold symptoms not meeting DSM criteria. Indeed, a large body of research has been performed with low income mothers in which impaired parent-child interactions have been shown to be associated with depressive symptoms not necessarily meeting clinical criteria18,19. Furthermore, depressive symptoms even at a low level have been robustly associated in low income families with adverse child outcomes across domains6.
Because of the robust relationship between maternal depressive symptoms and child developmental outcomes, a number of public health initiatives have been developed to enhance parenting self-efficacy and mother-infant interactions in the context of these symptoms. Two illustrative examples are Nurse Family Partnership (NFP)20 and Family Check Up (FCU)21. Both are delivered as home visitation programs, and both have sought to enhance self-efficacy and interactions in low income mothers either at risk for depressive symptoms (NFP) or with depressive symptoms already present (FCU). In studies of NFP, the greatest impacts on child developmental outcomes were found for were found for mothers with low psychological resources (including presence of depressive symptoms), suggesting potential for benefits from preventive interventions addressing interactions among depressed mothers20. Studies of FCU not only documented similar impacts in depressed mothers, but also showed that enhanced interactions were associated with reduced depressive symptoms21. This body of work strongly supports the potential for benefit from addressing interactions among low income mothers at risk for depression.
The documented impacts of programs such as NFP and FCU have led policymakers to consider whether there might be additional public health venues for addressing maternal depression and its comorbidities. The pediatric primary care platform has been of particular interest, given its potential for scalability, population-level impact and low cost. Two areas of focus in the pediatric platform have been early identification of maternal depressive symptoms22 and prevention of child co-morbidities through enhanced parent-child interactions23. Regarding the former, the American Academy of Pediatrics (AAP) in collaboration with the U.S. Department of Health and Human Services Health Resources and Services Administration Maternal and Child Health Bureau (Bright Futures) has sought to promote screening, identification, and services for mothers with depressive symptoms23,24. Regarding the latter, clinically oriented programs such as Triple P have been shown to enhance interactions in depressed mothers utilizing the pediatric platform25.
A number of interventions in the pediatric platform have sought to enhance interactions among low income dyads universally. While these interventions have not specifically targeted mothers with depressive symptoms, many mothers receiving these interventions had depressive symptoms and all were at risk on the basis of poverty. Reach Out and Read26 and the Video Interaction Project are prominent examples, in that extensive research has documented beneficial impacts on interactions among at-risk, low income mothers27-32. Although the well-documented interrelationships between depression and parent-child interactions described above suggest the possibility that such preventive interventions might also prevent maternal depressive symptoms, this has not previously been studied.
We therefore sought to address this gap in knowledge within an ongoing randomized controlled trial (RCT), the Bellevue Project for Early Language, Literacy and Education Success (BELLE), in which two interventions provided within the pediatric primary care platform were compared to a control group. The two interventions under study were the Video Interaction Project (VIP) and Building Blocks (BB). VIP is an individualized, relationship-based intervention building on Reach Out and Read that takes place at the time of participants’ regular pediatric visits. In VIP, mother-child dyads meet with an interventionist who provides developmentally-appropriate learning materials, discusses plans for play and shared reading, and then video-records the dyads interacting together. Following creation of the video, the interventionist reviews it with the mother, reinforcing strengths and discussing additional opportunities for interaction. BB utilizes mailed parenting newsletters, learning materials and parent-completed questionnaires to educate and communicate with parents.
Both interventions have been previously shown to improve parental responsiveness27, 33, with greater impacts for VIP, consistent with its greater intensity and relationship-based approach. Therefore, as part of the larger BELLE RCT, we sought to test the hypothesis that VIP and BB would result in reduced depressive symptoms through enhanced parental responsiveness. Given VIP’s previously determined impacts, we hypothesized that this intervention would also be associated with reduced maternal depressive symptoms, mediated by enhanced parental responsiveness. Given BB’s very low intensity and smaller impacts on responsiveness, we did not have strong hypotheses regarding it impacts on depressive symptoms but performed exploratory analyses within the context of the clinical trial.
MATERIALS AND METHODS
Study Design
This was a single-blind, three-way randomized controlled trial (RCT), with two preventive interventions (VIP and BB) compared to a control group. IRB approval was obtained from New York University School of Medicine Institutional Review Board and the Bellevue Hospital Center Research Review Committee. Parents provided informed consent prior to participation. The trial was registered at clinicaltrials.gov (NCT00212576).
Sample
Enrollment of all families in the larger, ongoing study was performed in the postpartum unit of an urban public hospital (BHC) serving low income, primarily immigrant, families, between November, 2005 and October, 2008. Consecutive mother–newborn dyads planning to receive pediatric primary care at Bellevue Hospital Center and who met eligibility criteria were enrolled in the current study. These criteria, which have been described previously27,33, were: child full-term newborn with no significant medical/perinatal complications, and mother primary caregiver with primary language English or Spanish, ability to maintain contact with the program, and no prior participation in VIP or BB.
Randomization Groups
Following enrollment, mother-child dyads were randomized to VIP, BB or control using a random number generator. Randomization group assignments were concealed from research assistants performing enrollment. Following enrollment, randomization group assignments were provided to study participants.
1. The Video Interaction Project (VIP)
VIP, which has been previously described27-31,33,34, takes place from birth to three years, with sessions taking place primarily on the same day as regularly-scheduled well-child primary care visits. Families in the current study received up to four possible visits by infant age 6 months. Sessions are facilitated by an interventionist, who meets one-on-one with families for approximately 30 minutes, providing an individualized, relationship-based intervention. The interventionist delivers a curriculum focused on supporting parent-child interactions in the context of pretend play, shared reading and daily routines, to enhance child development and school readiness. The estimated cost of VIP is less than $150 per child, including learning materials, hospital space, and interventionist salary. VIP utilizes the following strategies:
Video-recording of mother-child interaction: A 5 to 7 minute video of each mother-child dyad engaging in activities suggested and modeled by the interventionist using a provided developmentally-appropriate learning material is created and reviewed. The mother and interventionist then watch the video together, with the interventionist making observations about the mother’s interactions with her child. The interventionist reinforces positive interactions (e.g., mother responding to the child’s vocalizations, engaging the child in back and forth conversation as the child develops language) and provides suggestions regarding missed opportunities for interaction. A copy of the video is given to the parent to take home to support the implementation of activities in the home and shared with other family members.
Provision of learning materials: Developmentally appropriate learning materials, including a toy and/or book, are given to families at each visit to take home. Learning materials were selected to promote parent-child engagement in activities likely to support child development.
Pamphlets: Messages are reinforced using written, visit-specific pamphlets which the interventionist reviews with each mother. Each pamphlet includes suggestions for interacting with the child through play, shared reading and daily routines. Pamphlets were developed in English and Spanish, and written at a 4th to 5th grade reading level using “plain language” principles35. The interventionist encourages the parent to show the pamphlet to the pediatric provider who further reinforces messages.
2. Building Blocks (BB)
BB takes place from birth to three years. Similar to VIP, BB delivers a curriculum which is focused on boosting parental self-efficacy and supporting interactions in the context of pretend play, shared reading and daily routines, in order to enhance child development and school readiness. In contrast to VIP, this curriculum is delivered through written pamphlets and learning materials that are mailed monthly to the family, rather than by an interventionist. Families in the current study who were randomized to BB received five mailings prior to child age 6 months. The estimated BB cost is less than $75 per child per year, including learning materials, staff member salary, and hospital space. BB utilizes the following strategies:
Building Blocks newsletters (Primeros Pasos in Spanish): Monthly age-specific newsletters are designed to encourage parents to interact with their child around a specific developmental activity, building on “parent education by mail”36. BB newsletters provide specific information on child development, play and learning activities, and general parenting information (e.g., feeding, discipline). BB newsletters have a clean, simple, user-friendly format and are written at a 3rd to 4th grade reading level.
Learning materials: A developmentally stimulating toy, book or other learning material is included with each BB package.
Parent-completed questionnaires: Two to three times a year, parents are mailed written developmental questionnaires, the Ages and Stages Questionnaire37, for parents to complete and return to the program, with a goal of encouraging parents to observe their child’s development and accomplish ongoing developmental screening. The first questionnaire in the Ages and Stages sequence is administered at infant age four months.
3. Control
As described above, control families received all standard pediatric care, including all routine anticipatory guidance and developmental surveillance.
Measures
Assessments were performed through interviews with mothers by bilingual research assistants who were masked to group assignment.
Dependent variable
The dependent variable for this study was the presence of symptoms of maternal depression, assessed using the Patient Health Questionnaire-9 (PHQ-9) at child age 6 months. The PHQ-9 is a screening instrument based on nine questions that assess depressed mood (“feeling down, depressed or hopeless”) during the prior 2 weeks38. Examples include “little interest or pleasure in doing things” and “feeling tired or having little energy”. Each question is scored from 0 to 3, with total scores ranging from 0-27 and higher scores representing greater frequency of symptoms. It is available and has been validated in Spanish39,40, which was the primary language of administration in the current study. Standard cut points were used, with 5 representing mild depressive symptoms and 10 representing moderate depressive symptoms38. In studies conducted in adult primary care and obstetric and gynecological settings, the PHQ-9 using a cutoff of 10 has been shown to have a sensitivity of >88% and a specificity of >88% for major depression as diagnosed through a mental health interview and by using the Structured Clinical Interview for DSM-IV, while the cutoff of 5 signifies sub-clinical symptoms important both because of increased risk of later major depression41 as well as adverse impacts on parent-child interactions18,19.
Additional Variables
Sociodemographic characteristics were assessed by parental interview at enrollment. Parent characteristics included mother’s age, country of origin, education level, primary language spoken, and marital status, and family Hollingshead Four Factor Socioeconomic Status (SES)42 based on parental education and occupation. Mothers were considered to be at increased social risk if they had one or more of: being a victim of violence, homelessness, involvement with child protective services, significant financial hardship (e.g., difficulty paying bills), food insecurity, or reported cigarette smoking or alcohol use during pregnancy. In addition, to determine if depression had been similar across groups at baseline, mothers were asked if they had been diagnosed with a mental illness in the two years prior to delivery, and then asked to specify the diagnosis. Infant information about gender and birth order was also obtained.
Responsive parenting, conceptualized as play with toys, reading and verbal responsiveness was assessed using StimQ-Infant (StimQ-I)43, an office-based structured interview at infant age 6 months. Examples of questions include: “While you read to your child, do you point to pictures and name them or describe them, or is your child too young or distractable for that?” and “Do you have the opportunity to point things out around the house for your child?” StimQ was designed for use in low-SES populations in English and Spanish. It has good validity with measures of cognitive, language, and social development. StimQ has been used in a number of recent studies of early child development44,45 and has been used in previous studies of VIP28,29 as well as the present study of VIP and BB to demonstrate impacts on parent-child interaction27, 33.
Statistical analysis
Sample size for the study was estimated based on 80% power to find clinically relevant impacts of interventions on primary outcomes (i.e., parent-child interaction, child development), assuming 33.3% attrition by the age of 2 years. This resulted in enrollment of 225 families per group, for a total of 675. Statistical analyses were performed using SPSS 19.0 based on intent to treat. First, we compared assessed and non-assessed families for sociodemographic characteristics and prior history of depression using t-tests for continuous variables and chi-square with continuity correction for categorical variables. Next, we compared baseline characteristics for families completing the 6 month assessment using ANOVA for continuous variables and chi-square for categorical variables. To compare mean depression score across groups, we performed unadjusted and adjusted (linear regression) analyses; effect sizes were calculated using Cohen’s d. To compare proportions of mothers reaching thresholds for mild and moderate depressive symptoms, we performed additional unadjusted and adjusted logistic regression analyses. Adjusted linear and logistic regression analyses included all variables significantly associated with whether families completed the assessment (language, immigration, education) or with maternal depressive symptoms (language, social risk). We also calculated absolute risk reduction (ARR), relative risk reduction (RRR) and number needed to treat with corresponding 95% confidence estimates. Finally, path analysis was used to determine whether enhanced parental responsiveness, measured by StimQ, mediated VIP- and BB-associated reductions in maternal depressive symptoms. The presence of mediation was assessed using Baron and Kenny criteria46. Indirect effects were calculated, and statistically tested using the Sobel test47.
RESULTS
Study Sample
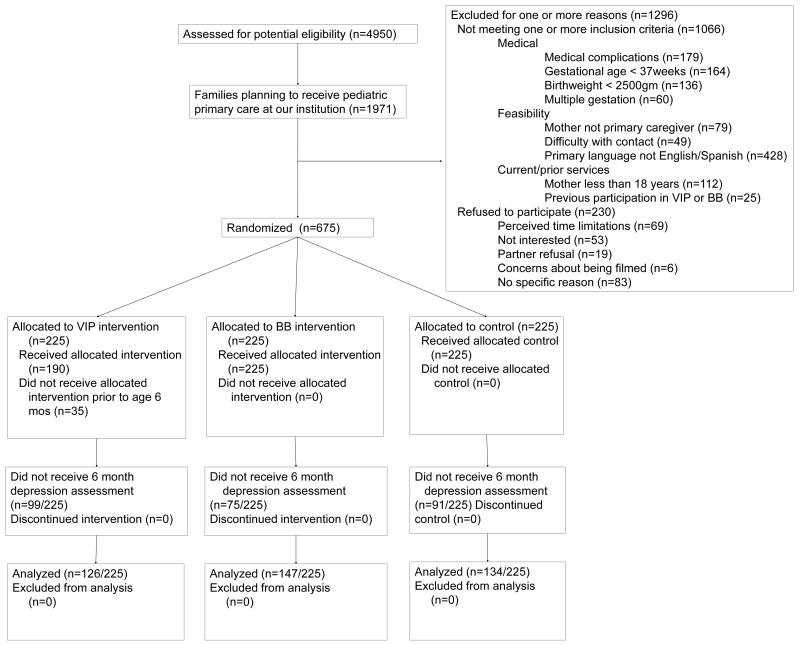
Participant enrollment and flow is shown in Figure 1. 407/675 families (60.2%) were assessed for maternal depressive symptoms at mean (SD) child age 6.9 (1.2) months, including 126 VIP, 147 BB and 134 Controls. Assessed and non-assessed families did not demonstrate significant differences on most variables, including maternal age, ethnicity, marital status, SES, and social risks. However, compared to mothers who were not assessed, mothers who were assessed were more likely to be immigrants to the United States and speak Spanish as primary language (both p<.001) and have lower education (p=.01). Of particular relevance to this analysis, there were no differences in baseline depressive symptoms between assessed and non-assessed mothers. As previously reported, both VIP and BB families had good adherence27,33.
Figure 1.
Participant enrollment and assessment
Baseline family sociodemographic characteristics and information on prior maternal depressive symptoms (assessed at enrollment) are shown in Table 2 for the 407 families completing the 6 month assessment. No differences were found between groups for any of these characteristics, including depressive symptoms at baseline, with 6.3% of VIP mothers reporting depressive symptoms in the prior two years, compared with 5.4% of BB mothers and 4.5% of control mothers (.80).
Table 2.
Baseline family sociodemographic characteristics for families completing the 6 month assessment (% or mean SD)
| VIP n=126 |
BB n=147 |
C n=134 |
p | |
|---|---|---|---|---|
| Mother | ||||
| Age in years (SD) | 27.52 (4.94) | 26.79 (5.40) | 27.76 (6.23) | .31 |
| Latina | 91.3% | 95.2% | 92.5% | .41 |
| Immigrant | 88.9% | 86.4% | 88.1% | .81 |
| Spanish language | 80.2% | 78.9% | 85.8% | .29 |
| Married/Partner | 82.5% | 86.4% | 82.8% | .62 |
| Educationa | 10.17(3.67) | 10.29(3.70) | 9.56(3.52) | .21 |
| Low SESb | 89.7% | 87.7% | 91.7% | .54 |
| Social risksc | 35.7% | 28.6% | 28.4% | .34 |
| Depression in prior 2 years | 6.3% | 5.4% | 4.5% | .80 |
| Child | ||||
| Female gender | 54.0% | 52.4% | 50.0% | .81 |
| First born | 42.1% | 40.8% | 41.8% | .97 |
Last grade completed
Hollingshead socioeconomic status level 4 or 5
1 or more of: being a victim of violence, homelessness, involvement with child protective services, significant financial hardship (e.g., difficulty paying bills), food insecurity, or reported cigarette smoking or alcohol use during pregnancy
Depressive symptoms: Descriptive information
Mean PHQ-9 score for the sample was 3.11 (SD=3.91). 24.6% of mothers exhibited symptoms of mild depression, and 7.1% of mother exhibited symptoms of moderate depression.
Depressive symptoms: Group status
Table 3 shows the association between group status and mean PHQ-9 score. In both unadjusted and adjusted analyses, mean PHQ-9 score was significantly lower for VIP families compared to controls; effect size based on Cohen’s d for the unadjusted difference was 0.34. BB families were not statistically significant for mean PHQ-9 score (p=.11).
Table 3.
Impact of VIP and BB on Mean Maternal Depression Score at 6 months [PHQ-9 mean(sd)]a
| N | PHQ-9 Mean (SD) |
Difference in PHQ- 9 Total Score for VIP and BB Compared to Controls (Unadjusted) |
95% CI | Difference in PHQ-9 Total Score for VIP and BB Compared to Controls (Adjusted) |
95% CI | |
|---|---|---|---|---|---|---|
| VIP | 126 | 2.47 (3.59) | −1.32 | (−2.27, −.38) | −1.86 | (−2.46, −.62) |
| BB | 147 | 3.05 (3.95) | −.74 | (−1.66, .17) | −.81 | (−1.70, .07) |
| Control | 134 | 3.79 (4.07) | refb | refb |
AOR: Adjusted odds ratio based on linear regression with VIP and BB as the independent variables and depression symptoms based on the above indicated threshold as the dependent variable. Adjusted linear regression analyses included all variables significantly associated with whether families completed the assessment (language, immigration, education) or with maternal depressive symptoms (language, social risk).
reference group
Table 4 shows the association between group status and PHQ-9 based on the mild and moderate thresholds. In unadjusted and adjusted analyses, both VIP and BB assignment were significantly associated with reduced mild depressive symptoms. These differences corresponded to an absolute risk reduction for VIP of 11.5% (95% CI: .7%, 21.8%) and for BB of 11.0% (95% CI: .7%, 21.1%), and a relative risk reduction (RRR) for VIP of 35.7% (95% CI: 2.0%, 57.8%) and for BB of 34.3% (95% CI: 2.2%, 55.9%). Eight VIP families (95% CI: 5, 142) and 9 BB families (95% CI: 5, 147) would need to receive the respective intervention to prevent one mother from having mild maternal depressive symptoms. For moderate depressive symptoms, associations were found for VIP only. In unadjusted analyses, VIP was associated with a trend for reduced moderate symptoms (p=0.08); this difference became statistically significant following adjustment. This association corresponded to an absolute risk reduction for VIP of 5.7% (95% CI: .6%, 12.3%) a relative risk reduction (RRR) for VIP of 59.1% (95% CI: 11.4%, 85%) and a number needed to treat of 17 (95% CI: −160, 8).
Table 4.
Impact of VIP and BB for Meeting Thresholds for Mild and Moderate Depressive Symptoms at 6 Months (Measured using PHQ-9)
| Scores 5 or abovea | Scores 10 or aboveb | |||||
|---|---|---|---|---|---|---|
| n(%) | OR (95% CI) |
AOR (95% CI)c | n (%) | OR (95% CI) |
AOR (95% CI)c | |
| VIP | 26 (20.6%) |
.55 (.31, .97) |
.48 (.27, .86) | 5 (4.0%) | .39 (.13, 1.11) | .30 (.10, .89) |
| BB | 31 (21.1%) |
.57 (.33, .97) |
.53 (.31, .96) | 11 (7.5%) | .75 (.33, 1.74) | .67 (.28, 1.60) |
| Control | 43 (32.1%) |
refd | 13 (9.7%) | refd | ||
Indicates mild depression
Indicates moderate depression
AOR: Adjusted odds ratio based on logistic regression with VIP and BB as the independent variables and depression symptoms based on the above indicated threshold as the dependent variable. Adjusted logistic regression analyses included all variables significantly associated with whether families completed the assessment (language, immigration, education) or with maternal depressive symptoms (language, social risk).
reference group
Parental responsiveness as mediator for intervention impacts
Path analysis was utilized to determine whether enhanced parental responsiveness, previously reported to differ across groups and measured by StimQ27, mediated intervention-associated reductions in maternal depressive symptoms. As shown in Figure 2, criteria for partial mediation were met for VIP, with VIP associated with enhanced parental responsiveness in unadjusted analysis, increased parental responsiveness associated with reduced maternal depressive symptoms, and reduced association between VIP and depressive symptoms after adjustment for parental responsiveness(indirect effect −.17, 95% CI −.36, −.03). Evidence of mediation by parental responsiveness was not found for BB.
Figure 2.
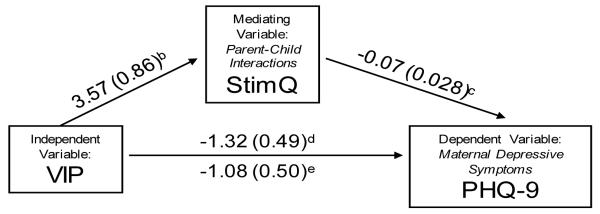
Path analysis-Enhance parent-child interactions (StimQ) partially mediating VIP-associated reductions in maternal depressive symptomsa
aValues shown are unstandardized regression coefficients (Standard Error)
bUnadjusted, p<.001
cAdjusted for VIP, p=.02
dUnadjusted, p=.007
eAdjusted for parent-child interactions (StimQ), p=.03
CONCLUSION
Maternal depression and poverty status together adversely affect mother-infant interactions and have detrimental effects on child developmental outcomes5. Interventions to reduce these disparities require effective strategies to prevent depressive symptoms among low income mothers that can be implemented at the population level. The current study has established that low-cost, low-intensity strategies targeting parental responsiveness and located within pediatric primary care settings may be effective in preventing emergence of maternal depressive symptoms.
We studied two pediatric primary care preventive interventions, VIP and BB, and found that each resulted in reduced maternal depressive symptoms. Overall effect sizes were of sufficient magnitude to be clinically meaningful, with a relative risk reduction of approximately one-third for each of these programs. Two aspects of our results are of particular note: First, both VIP and BB targeted parental responsiveness rather than depressive symptoms per se; for VIP, impacts were partially mediated by enhancements in these interactions. This finding is consistent with studies of the Family Check-Up (FCU)21, which employed individual parenting consultants who worked with families to enhance their self-efficacy and parenting skills, work that in turn resulted in reduced parental depression. Similar to the FCU’s results, it is possible that in the current study, mothers’ relationships with their interventionists may have had some impacts on depressive symptoms, especially in the case of VIP. Second, both VIP and BB had impacts on depressive symptoms despite being low intensity, low cost programs. This finding adds to a growing body of evidence suggesting a role for low intensity interventions addressing maternal depressive symptoms in at-risk populations in pediatric primary care20,21,25,27-34.
Consistent with our hypotheses, findings were more robust for VIP than for BB. While both programs were associated with significant reductions in the rate of mild symptoms, VIP was also significantly associated with reduced moderate symptoms41, which previous research has shown may still significantly negatively impact parent-child interactions and in turn lead to adverse child outcomes18,19. These findings were not predicted in the context of the larger project, but were encouraging given VIP’s use of an individualized, relationship-based approach, a strategy found to be effective in enhancing parental responsiveness and mitigating symptoms of maternal depression48.
This study positions pediatric primary care as a promising venue to reduce and possibly prevent maternal depressive symptoms among at-risk, low-income families at a population level. Identification and engagement of low income families represent a challenge for public health programs49. Pediatric primary care has the potential to facilitate identification and engagement of low income mothers at risk for depression50, by taking advantage of visits required for screening and immunizations51 in the context of initiatives to increase access to care such as S-CHIP52. Furthermore, utilization of existing infrastructure and travel allows delivery of preventive interventions at low cost. Our findings add to reports of recent efforts to utilize pediatric primary care to enhance identification of mothers with depressive symptoms and contribute to a growing body of work supporting developmental intervention in pediatric primary care.
This study has some important limitations. First, there was larger-than-expected loss to follow-up at 6 months because of limitations in resources which led us to prioritize later assessments. The threat to validity resulting from loss to follow-up was likely to have been limited as assessed participants were equivalent across groups for all measures. Second, depressive symptoms and parental responsiveness were assessed concurrently; as a result we cannot determine whether improved interactions resulted in reduced depressive symptoms or vice versa, or whether impacts were bi-directional. Ongoing longitudinal study of the cohort will allow for subsequent analyses that will help us to better understand directionality of impact as well as long-term impacts. Third, our results apply to primarily low-income, Latino, immigrant families and may not be generalizable to families with more resources. Fourth, differences between assessed and non-assessed participants related to U.S. immigration and Spanish language may limit generalizability.
In conclusion, this study has established a promising role for low-intensity interventions to promote parent-child interactions in the prevention of maternal depression as part of a broad public health strategy utilizing pediatric primary care as a potentially universal, low cost platform.
Table 1.
Sociodemographic characteristics for assessed vs. non-assessed families (% or mean, SD)
| Assessed (N=407) |
Non-assessed (N=268) |
p | |
|---|---|---|---|
| Mother | |||
| Age in years (mean, SD) | 27.36 (5.56) | 27.15 (6.37) | .09 |
| Latina | 93.1% | 89.5% | .12 |
| Immigrant | 87.7% | 77.6% | <.001 |
| Spanish language | 81.6% | 67.2% | <.001 |
| Married/Partner | 84.0% | 82.1% | .53 |
| Education (mean years of education) |
10.0 (3.6) | 10.8 (3.6) | .01 |
| Low SESa | 89.6% | 90.2% | .90 |
| Social risksb | 30.7% | 25.4% | .14 |
| Depression in prior 2 years | 5.4% | 7.1% | .41 |
| Child | |||
| Female gender | 52.1% | 44.4% | .06 |
| First born | 41.5% | 39.9% | .69 |
Hollingshead socioeconomic status level 4 or 5
1 or more of: physical abuse, homeless, child protection, late prenatal care, financial hardship, food insecurity
ACKNOWLEDGEMENTS
This study was supported by grant R01 HD047740-01-07 from the National Institutes of Health/National Institute of Child Health and Human Development and by the Tiger Foundation, the Marks Family Foundation, the Rhodebeck Charitable Trust, Children of Bellevue, Inc., KiDS of NYU, and ECRIP.
We would like to thank many colleagues for their guidance and support, including Arthur Fierman, Virginia Flynn, Gilbert Foley, Emily Forrest, Perri Klass, Wendy Tineo, and Linda van Schaick. Finally, we are grateful to many additional individuals who contributed to this project, including Melissa Acevedo, Jenny Arevalo, Pamela Kim, Jennifer Ledesma, Elizabeth Jennifer Lee, Lesley Morrow, Daniela Romero, Melissa Tunik, Jessica Urgelles, Triana Urraca, Kristina Vlahovicova, Linda Votruba, Lisa White, Caroline Wilkes, Margaret Wolff and Brenda Woodford.
Footnotes
There are no conflicts of interest to disclose.
REFERENCES
- 1.Cox AD, Puckering C, Pound A, Mills M. The impact of maternal depression in young children. J Child Psychol Psyc. 1987;28:917–928. doi: 10.1111/j.1469-7610.1987.tb00679.x. [DOI] [PubMed] [Google Scholar]
- 2.Cicchetti D, Rogosch FA, Toth SL. Maternal depressive disorder and contextual risk: contributions to the development of attachment insecurity and behavior problems in toddlerhood. Dev Psychopathol. 1998;10:283–300. doi: 10.1017/s0954579498001618. [DOI] [PubMed] [Google Scholar]
- 3.Chaudron LH, Szilagyi PG, Kitzman HJ, Wadkins HI, Conwell Y. Detection of postpartum depressive symptoms by screening at wellchild visits. Pediatrics. 2004;113:551–558. doi: 10.1542/peds.113.3.551. [DOI] [PubMed] [Google Scholar]
- 4.Morris-Rush JK, Freda MC, Bernstein PS. Screening for postpartum depression in an inner-city population. Am J Obstet Gynecol. 2003;188:1217–1219. doi: 10.1067/mob.2003.279. [DOI] [PubMed] [Google Scholar]
- 5.Aber JL, Jones S, Cohen J. The impacts of poverty on the mental health and development of very young children. In: Zeanah CH, editor. Handbook of Infant Mental Health. 2nd edn. The Guilford Press; New York: 2000. pp. 113–128. [Google Scholar]
- 6.Field T, Estroff DB, Yando R, delValle C, Malphurs J, Hart S. “Depressed” mothers’ perceptions ofinfant vulnerability are related to later development. Child Psychiat Hum D. 1996;27:43–53. doi: 10.1007/BF02353445. [DOI] [PubMed] [Google Scholar]
- 7.Weissman MM, Feder A, Pilowsky DJ, et al. Depressed mothers coming to primary care: maternal reports of problems with their children. J Affect Disord. 2004;78:93–100. doi: 10.1016/s0165-0327(02)00301-4. [DOI] [PubMed] [Google Scholar]
- 8.Gershoff ET, Aber JL, Raver CC, Lennon MC. Income is not enough: material hardship into models of income associations with parenting and child development. Child Dev. 2007;78:70–95. doi: 10.1111/j.1467-8624.2007.00986.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cummings EM, Davies PT. Maternal depression and child development. J Child Psychol Psych. 1994;35:73–122. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- 10.Teti DM, Gelfand DM. Behavioral Competence among mothers of infants in the first year: the mediational role of maternal self-efficacy. Child Dev. 1991;62:918–929. doi: 10.1111/j.1467-8624.1991.tb01580.x. [DOI] [PubMed] [Google Scholar]
- 11.Kochanska G, Radke-Yarrow M, Kuczynski L, Friedman SL. Normal and affectively ill mothers’ beliefs about their children. Am J Orthopsychiatry. 1987;57:345–350. doi: 10.1111/j.1939-0025.1987.tb03543.x. [DOI] [PubMed] [Google Scholar]
- 12.Silverstein M, Reid S, DePeau K, Lamberto J, Beardslee W. Functional interpretations of sadness, stress and demoralization among an urban population of low-income mothers. Matern Child Health J. 2010;14:245–253. doi: 10.1007/s10995-009-0445-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dix T, Gershoff ET, Meunier LN, Miller PC. The affective structure of supportive parenting: depressive symptoms, immediate emotions, and child-oriented motivation. Dev Psychol. 2004;40:1212–1227. doi: 10.1037/0012-1649.40.6.1212. [DOI] [PubMed] [Google Scholar]
- 14.Maxted AE, Dickstein S, Miller-Loncar C, et al. Infant colic and maternal depression. Inf Mental Hlth J. 2005;25:56–68. doi: 10.1002/imhj.20035. [DOI] [PubMed] [Google Scholar]
- 15.Vik T, Grote V, Escribano J, et al. Infant colic, prolonged crying, and postnatal maternal depression. Acta Paediatr. 2009;98:1344–1348. doi: 10.1111/j.1651-2227.2009.01317.x. [DOI] [PubMed] [Google Scholar]
- 16.McGrath JM, Records K, Rice M. Maternal depression and infant temperament characteristics. Infant Behav Dev. 2008;31:71–80. doi: 10.1016/j.infbeh.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cutrona CE, Troutman BR. Social support, infant temperament, and parenting self-efficacy: a mediational model of postpartum depression. Child Dev. 1986;57:1507–1518. [PubMed] [Google Scholar]
- 18.Herrera E, Reissland N, Shepherd J. Maternal touch and maternal child-directed speech: effects of depressed mood in the postnatal period. J Affect Disorders. 2004;81:29–39. doi: 10.1016/j.jad.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 19.Murray L, Fiori-Cowley A, Hooper R, Cooper P. The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Dev. 1996;67:2512–2526. [PubMed] [Google Scholar]
- 20.Olds DL, Robinson J, Pettitt LM, et al. Effects of home visits by paraprofessionals and by nurses: age four follow-up results of a randomized trial. Pediatrics. 2004;114:1560–1568. doi: 10.1542/peds.2004-0961. [DOI] [PubMed] [Google Scholar]
- 21.Shaw DS, Connell A, Dishion TJ, Wilson MN, Gardner F. Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development Psychopath. 2009;21:417–439. doi: 10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olson AL, Kemper KJ, Kelleher KJ, Hammond CS, Zuckerman BS, Dietrich AJ. Primary care pediatricians’ roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics. 2002;110:1169–1176. doi: 10.1542/peds.110.6.1169. [DOI] [PubMed] [Google Scholar]
- 23.Garner AS, Shonkoff JP, Siegel BS, et al. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129:e224–e231. doi: 10.1542/peds.2011-2662. [DOI] [PubMed] [Google Scholar]
- 24.Hagen JF, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd edn. American Academy of Pediatrics; Elk Grove, Illinois: 2008. [Google Scholar]
- 25.Sanders MR. Triple P-Positive Parenting Program: towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clinical Child and Family Psychology Review. 1999;2:71–90. doi: 10.1023/a:1021843613840. [DOI] [PubMed] [Google Scholar]
- 26.Klass P, Needlman R, Zuckerman B. Reach Out and Read Program Manual. Boston Medical Center; Boston: 1999. [Google Scholar]
- 27.Mendelsohn AL, Huberman HS, Berkule SB, Brockmeyer CA, Morrow LM, Dreyer BP. Primary care strategies for promoting parent-child interactions and school readiness in at-risk families: the Bellevue Project for Early Language, Literacy, and Education Success. Arch Pediatr Adolesc Med. 2011;165:33–41. doi: 10.1001/archpediatrics.2010.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mendelsohn AL, Dreyer BP, Flynn V, et al. Use of videotaped interactions during pediatric well-child care to promote child development: a randomized, controlled trial. J Dev Behav Pediatr. 2005;26:34–41. [PMC free article] [PubMed] [Google Scholar]
- 29.Mendelsohn AL, Valdez PT, Flynn V, et al. Use of videotaped interactions during pediatric well-child care: impact at 33 months on parenting and on child development. J Dev Behav Pediatr. 2007;28:206–212. doi: 10.1097/DBP.0b013e3180324d87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mendelsohn AL, Brockmeyer CA, Dreyer BP, Fierman AH, Berkule SB, Tomopoulos S. Do verbal interactions with infants during electronic media exposure mitigate adverse impacts on their language development as toddlers? Infant Child Dev. 2010;9:577–593. doi: 10.1002/icd.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mendelsohn AL, Dreyer BP, Brockmeyer CA, Berkule SB, Huberman HS, Tomopoulos S. Randomized controlled trial of primary care pediatric parenting programs: effect on reduced media exposure in infants, mediated through enhanced parent-child interaction. Arch Pediatr Adolesc Med. 2011;165:42–48. doi: 10.1001/archpediatrics.2010.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Minkovitz CS, Hughart N, Strobino D, et al. A practice-based intervention to enhance quality of care in the first 3 years of life: the Healthy Steps for Young Children Program. JAMA. 2003;290:3081–3091. doi: 10.1001/jama.290.23.3081. [DOI] [PubMed] [Google Scholar]
- 33.Mendelsohn AL, Dreyer BP, Brockmeyer CA, Berkule SB, Morrow LM. Fostering early development and school readiness in pediatric settings. In: Dickinson D, Neuman SB, editors. Handbook of Early Literacy Research: Volume 3. The Guilford Press; New York; 2011. [Google Scholar]
- 34.Mendelsohn AL, Mogilner LN, Dreyer BP, et al. The impact of a clinic-based literacy intervention on language development in inner-city preschool children. Pediatrics. 2001;107:130–134. doi: 10.1542/peds.107.1.130. [DOI] [PubMed] [Google Scholar]
- 35.Doak CC, Doak L, Root JH. Teaching patients with low literacy skills. Lippincott Williams & Wilkins; Philadelphia: 1996. 1996. [Google Scholar]
- 36.Cudaback DJ, Dickinson NS, Wiggins ES. Parent education by mail. Fam Soc-J Contemp H. 1990;71:172–175. [Google Scholar]
- 37.Squires JPL, Bricker D. The ASQ User’s Guide. 2nd ed. Paul Brookes; Baltimore: 1999. [Google Scholar]
- 38.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Diez-Quevedo C, Rangil T, Sanchez-Planell L, Kroenke K, Spitzer RL. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med. 2001;63:679–686. doi: 10.1097/00006842-200107000-00021. [DOI] [PubMed] [Google Scholar]
- 40.Wulsin L, Somoza E, Heck J. The feasibility of using the Spanish PHQ-9 to screen for depression in primary care in Honduras. Prim Care Companion J Clin Psychiatry. 2002;4:191–195. doi: 10.4088/pcc.v04n0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Horwath E, Johnson J, Klerman GL, Weissman MM. What are the public health implications of subclinical depressive symptoms? Psychiat Quart. 1994;65:323–37. doi: 10.1007/BF02354307. [DOI] [PubMed] [Google Scholar]
- 42.Hollingshead AB. Four Factor Index of Social Status. Yale University; New Haven, CT: 1975. [Google Scholar]
- 43.Dreyer BP, Mendelsohn AL, Tamis-LeMonda CS. Assessing the child’s cognitive home environment through parental report; reliability and validity. Early Dev Parenting. 1996;5:271–287. [Google Scholar]
- 44.Boyce LK, Roggman LA, Jump VK, Ortiz EA. Telling stories and making books: evidence for an intervention to help parents in migrant Head Start families support their children’s language and literacy. Early Education & Development. 2010;21:343–371. [Google Scholar]
- 45.Camp BW, Cunningham M, Berman S. Relationship between the cognitive environment and vocabulary development during the second year of life. Arch Pediatr Adolesc Med. 2010;164:950–956. doi: 10.1001/archpediatrics.2010.169. [DOI] [PubMed] [Google Scholar]
- 46.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 47.Howell DC. Statistical Methods for Psychology. 2nd edn. Wadsworth; Belmont CA: 2010. [Google Scholar]
- 48.Gelfand DM, Teti DM, Seiner SA, Jameson PB. Helping mothers fight depression: evaluation of a home-based intervention program for depressed mothers and their infants. J Clin Child Psychol. 1996;25:406–422. [Google Scholar]
- 49.Duggan A, Windham A, McFarlane E, et al. Hawaii’s healthy start program of home visiting for at-risk families: evaluation of family identification, family engagement, and service delivery. Pediatrics. 2000;105:250–259. [PubMed] [Google Scholar]
- 50.Cutler CB, Legano LA, Dreyer BP, et al. Screening for maternal depression in a low education population using a two item questionnaire. Arch Womens Ment Health. 2007;10:277–83. doi: 10.1007/s00737-007-0202-z. [DOI] [PubMed] [Google Scholar]
- 51.American Academy of Pedatrics Immunization Schedules. 2012 http://www2.aap.org/immunization/izschedule.html.
- 52.Rosenbaum S, Johnson K, Sonosky C, Markus A, DeGraw C. The children’s hour: The State Children’s Health Insurance Program. Health Aff. 1998;17:75–89. doi: 10.1377/hlthaff.17.1.75. [DOI] [PubMed] [Google Scholar]