Abstract
Objective
Examine longitudinal associations between sources of social support and social undermining for healthy eating and physical activity and weight change.
Design and Methods
Data are from 633 employed adults participating in a cluster-randomized multilevel weight gain prevention intervention. Primary predictors included social support and social undermining for two types of behaviors (healthy eating and physical activity) from three sources (family, friends, and coworkers) obtained via self-administered surveys. The primary outcome (weight in kg) was measured by trained staff. Data were collected at baseline, 12 months, and 24 months. Linear multivariable models examined the association of support and social undermining with weight over time, adjusting for intervention status, time, gender, age, education, and clustering of individuals within schools.
Results
Adjusting for all primary predictors and covariates, friend support for healthy eating (β=−0.15), coworker support for healthy eating (β=−0.11), and family support for physical activity (β=−0.032) were associated with weight reduction at 24 months (p-values<0.05). Family social undermining for healthy eating was associated with weight gain at 24 months (β=0.12; p=0.0019).
Conclusions
Among adult employees, friend and coworker support for healthy eating and family support for physical activity predicted improved weight management. Interventions that help adults navigate family social undermining of healthy eating are warranted.
Keywords: social support, social undermining, weight change, healthy eating, physical activity
Introduction
With over two-thirds of U.S. adults classified as overweight (33.0%) or obese (35.9%) (1), effective interventions that help adults achieve and maintain a healthy weight are imperative for the prevention and management of obesity and related diseases. Social relationships and interactions can have positive and negative influences on diet, physical activity, and weight status (2–7).
Previous studies indicate inconsistent associations between social support and obesity-related health behaviors and outcomes (5–12). Kiernan and colleagues behavioral weight loss intervention study indicated that lack of support was prevalent among overweight and obese women, with most women reporting never or rarely receiving support from family members and friends for weight loss efforts (6). Lack of social support may be characterized with respect to frequency of perceived receipt (i.e., never or infrequent) (6) or lack of access to a network of individuals available to provide support in times of need (13, 14). Less well investigated is the influence of social undermining, distinct from lack of support and defined as negative social interactions that attempt to hinder goal attainment, whether intentionally or not (15), on weight status. Both social undermining and lack of support related to healthy eating and/or physical activity have been shown to be positively associated with weight (6, 16), yet no studies to our knowledge have compared the effects of perceived support and social undermining from more than two sources on weight.
Enhancing social support for behavior change may be critical for preventing long-term excess weight gain (17–20). Common sources of social support include family members and friends, with less known about coworkers (6, 8, 21, 22). Previous studies utilized cross-sectional designs and/or examined the impact of social support on health behaviors only. Relatively few studies have examined the role of social support on anthropometric outcomes (8) or examined longitudinal associations between support, social undermining, and weight (16). Findings from a two-year study of young women indicated friend support for physical activity was associated with less weight gain over time, whereas friend social undermining of healthy eating and physical activity were associated with greater weight gain over time (16). Cross-sectional data from a worksite weight reduction trial indicated positive associations between worksite social support and physical activity and fruit and vegetable consumption, but no association with body mass index (BMI) among employees (8). No study to our knowledge has examined longitudinal associations between various sources of support and social undermining and weight among men and women.
This study aims to examine the relative contribution of various sources (family, friends, and coworkers) of perceived support and social undermining for healthy eating and physical activity on two-year change in weight among employees participating in a worksite weight gain prevention intervention. We hypothesized that greater support for healthy eating and physical activity would be associated with improved weight management (e.g., reduced weight gain), and social undermining for healthy eating and physical activity would be associated with increased weight gain. As previous research suggests that family and friend social support is associated with weight loss or reduced weight gain over time whereas coworker social support is not (6, 8, 16), and given that the home environment constitutes a major behavioral setting where social interactions related to eating and physical activity take place (23), we hypothesized that family support or social undermining would have a greater influence on weight gain prevention than friend or coworker support or social undermining. We also hypothesized that greater support for healthy eating and/or physical activity (from any source) is associated with improved weight management, and that greater social undermining of healthy eating and/or physical activity (from any source) is associated with increased weight gain.
Methods
Setting, Design, and Participants
Data from this study are from a cohort of school employees participating in a cluster-randomized controlled trial of a multilevel weight gain prevention intervention. Participants completed assessments at baseline, 12 months, and 24 months. The study was conducted from 2010–2012 at 12 public high schools in Central Massachusetts. Site and participant recruitment, enrollment, baseline measures, and site stratification by school size and urbanicity were completed prior to randomization of schools to study condition. Trained study staff screened employees for eligibility and obtained written informed consent from interested participants. Inclusion criteria for participants were: 1) English-speaking, 2) no plans to leave employment in the next two years, 3) worked at least 15 hours per week, 4) not pregnant or had not given birth in the past 6 months, and 5) no physical impediment to being weighed.
The two-year multilevel intervention was coordinated by school employees designated as intervention “coaches” (consisting of mostly school nurses) and an Employee Advisory Board comprised of school employees. Guided by the social ecological model (24), the intervention included individual-level strategies (i.e., health promotion displays and healthy food tastings, weight loss and weight maintenance challenges), interpersonal strategies (i.e., organization of employee walking groups and healthy potlucks, physical activity campaigns and challenges, onsite group fitness classes), and organizational strategies (i.e., access to onsite fitness facilities, availability of healthy lunch options, limiting access to sugar-sweetened beverages in faculty lounges, and point-of-purchase nutritional information in cafeterias). The comparison condition consisted of print (e.g., employee resource book with healthy recipes, walking maps, and weight loss tips) and electronic (e.g., project website and weekly e-newsletter) materials only. Additional details regarding study recruitment, retention, intervention conditions, and measures have been previously reported (25). Study attrition rate at 24 months was 19.2%.
Measures
The primary outcome, weight, was measured by trained staff using portable digital scales with readings taken to the nearest 2/10th pound. Heights were measured to the nearest 1/8th inch using portable stadiometers. Participants wore light clothing and removed shoes for height and weight measurements. BMI was calculated as weight in kilograms divided by meters squared (kg/m2). Weight and BMI were examined continuously, and BMI was also categorized as underweight (<18.5 kg/m2), healthy weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), or obese (≥30.0 kg/m2).
Perceived social support and social undermining were assessed using Sallis et al.’s survey of social support for diet and exercise behaviors (26). The 23-item survey included four subscales: support for healthy eating (5 items); support for physical activity (11 items); social undermining for healthy eating (5 items); and social undermining for physical activity (2 items). Example items assessing support included: “complimented me on changing my eating habits”; “encouraged me not to eat unhealthy foods when I’m tempted to do so”; “exercised with me”; and “helped plan activities around my exercise.” Example social undermining items included: “brought me foods I’m trying not to eat”; “ate high-fat foods in front of me”; “complained about the time I spent exercising”; and “criticized me or made fun of me for exercising.” Each item was rated on a scale of 1 to 5 (1 = none; 5 = very often), with respondents asked to rate support and social undermining perceived from family, friends, and coworkers. Summary scores of support and social undermining for healthy eating and physical activity from family, friends, and coworkers were generated from survey responses and examined continuously. Items were the same across source to maintain measurement consistency. Possible ranges for support scores were 5–25 for healthy eating and 11–55 for physical activity; possible ranges for social undermining scores were 5–25 for healthy eating and 2–10 for physical activity. Higher scores represent greater support or social undermining. The internal reliability of the four subscales ranged from Cronbach’s α = 0.73–0.77 for family, 0.72–0.76 for friends, and 0.72–0.76 for coworkers, indicating acceptable reliability (27).
Demographic characteristics were assessed via self-report surveys and included gender, age (years), race/ethnicity (White, Hispanic/Latino, Black/African American, Asian, American Indian/Alaskan Native, Hawaiian/Pacific Islander, and/or Other), education (highest level attained), occupation type (teacher or staff), and marital status. All measures were obtained at baseline, 12 months, and 24 months. Study protocol and procedures were approved by the Institutional Review Board at the University of Massachusetts Medical School.
Statistical Analyses
Means and standard deviations for continuous variables and frequencies for categorical variables were computed to describe the study sample at baseline. Correlations between types and sources of support and social undermining at baseline were examined. Mixed effects regression models with repeated measures were used to examine trends in support and social undermining over time. Linear mixed effects regression models were used to estimate the association between social influence (support and social undermining) specific to each behavioral domain (healthy eating and physical activity) from each source (family, friends, and coworkers) on employee weight change. All models adjusted for clustering of individuals within schools. Predictors in the final model included baseline support and social undermining from all three sources for each behavioral domain, intervention status and time. Gender, education, and age were also included as covariates, given gender differences in the association between social relationships and obesity (5); inverse association between education level and BMI (28); and average adult weight gain over time (29). Interaction effects between support and social undermining within each behavioral domain and between gender and each support and social undermining predictor were examined using interaction terms. Analyses were restricted to the participants who completed baseline, 12 and 24 month assessments (N=633). All statistical tests were conducted using SAS version 9.3.
Results
Of the 633 adult public high school employees participating in the study, most were female (65.6%), non-Latino White (96.2%), and married (71.6%). Participants averaged 44.6 years (SD=11.3), and over half (58%) were employed as teachers. The mean baseline BMI was 27.6 kg/m2 (SD=5.6), with 36.6% and 26.7% of participants who were overweight and obese, respectively. No participants were underweight. See Table 1 for additional study sample baseline characteristics.
Table 1.
Baseline Characteristics of Public School Employees (N=633) Participating In a Weight Gain Prevention Intervention
| Characteristic | Study Sample (N=633) |
|---|---|
|
| |
| N (%) | |
| Gender | |
| Female | 415 (65.6%) |
| Race/ethnicity | |
| White | 609 (96.2%) |
| Non-White | 24 (3.8%) |
| Education (highest level attained) | |
| < College degree | 136 (21.5%) |
| College degree | 194 (30.6%) |
| Graduate degree | 303 (47.9%) |
| Occupation | |
| Teacher | 367 (58.0%) |
| Staff | 266 (42.0%) |
| Marital Status | |
| Married | 453 (71.6%) |
| Living as married | 33 (5.2%) |
| Separated or divorced | 44 (7.0%) |
| Widowed | 11 (1.7%) |
| Never married | 92 (14.5%) |
| Weight status | |
| Healthy weight (BMI 18.5–24.9) | 232 (36.7%) |
| Overweight (BMI 25.0–29.9) | 232 (36.6%) |
| Obese (BMI ≥30.0) | 169 (26.7%) |
| Mean (SD) | |
| Age (years) | 44.6 (11.3) |
| Weight (kg) | 78.8 (18.2) |
| BMI (kg/m2) | 27.6 (5.6) |
Participants’ baseline support and social undermining scores were normally distributed, with family members perceived to provide the most frequent support for healthy eating and physical activity and the most frequent social undermining of healthy eating and physical activity (see Figures 1 and 2). Positive correlations between sources of support and social undermining by each behavioral domain were observed (see Table 2). The intra-class correlation (ICC) for 24-month change in weight within schools was 0.034. No significant changes in support or social undermining over time by source were observed for the overall study sample. Within-group analyses indicated that among intervention participants, coworker support for physical activity increased from baseline to 12 months, whereas among control participants, coworker support for physical activity decreased from baseline to 12 months and 24 months (p’s <0.05).
Figure 1.
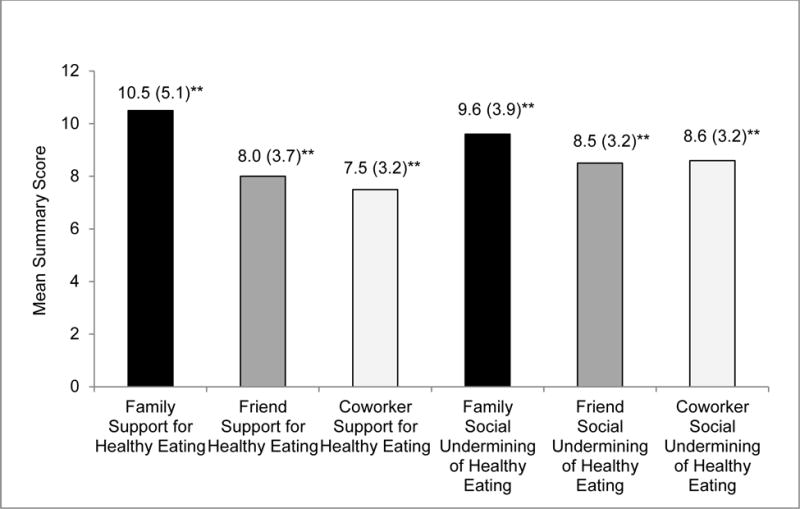
Baseline Measures† of Social Support for and Social Undermining of Healthy Eating by Source* among Public High School Employees (N=633) Participating In a Weight Gain Prevention Intervention
†Mean (SD)
*p-values are from F-tests estimating differences in mean support for healthy eating across all three sources and differences in mean social undermining of healthy eating across all three sources; level of significance set at p < 0.05.
**p < 0.0001
Figure 2.
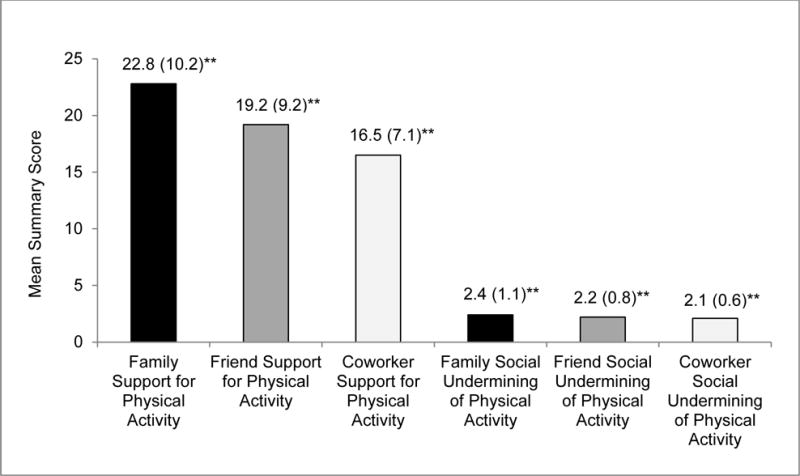
Baseline Measures† of Social Support for and Social Undermining of Physical Activity by Source* among Public High School Employees (N=633) Participating In a Weight Gain Prevention Intervention
†Mean (SD)
*p-values are from F-tests estimating differences in mean support for healthy eating across all three sources and differences in mean social undermining of healthy eating across all three sources; level of significance set at p < 0.05
**p < 0.0001
Table 2.
Correlations† between Baseline Summary Scores of Support and Social undermining for Healthy Eating and Physical Activity among School Employees (N=633)
| Family support for healthy eating | Friend support for healthy eating | Coworker support for healthy eating | Family social undermining for healthy eating | Friend social undermining for healthy eating | Coworker social undermining for healthy eating | |
|---|---|---|---|---|---|---|
| Family support for healthy eating | 1.00 | |||||
| Friend support for healthy eating | 0.54* | 1.00 | ||||
| Coworker support for healthy eating | 0.39* | 0.70* | 1.00 | |||
| Family social undermining for healthy eating | 0.33* | 0.33* | 0.26* | 1.00 | ||
| Friend social undermining for healthy eating | 0.32* | 0.45* | 0.30* | 0.59* | 1.00 | |
| Coworker social undermining for healthy eating | 0.28* | 0.35* | 0.31* | 0.51* | 0.75* | 1.00 |
| Family support for physical activity | Friend support for physical activity | Coworker support for physical activity | Family social undermining for physical activity | Friend social undermining for physical activity | Coworker social undermining for physical activity | |
|---|---|---|---|---|---|---|
| Family support for physical activity | 1.00 | |||||
| Friend support for physical activity | 0.46* | 1.00 | ||||
| Coworker support for physical activity | 0.27* | 0.15* | 1.00 | |||
| Family social undermining for physical activity | 0.16* | 0.16* | 0.13* | 1.00 | ||
| Friend social undermining for physical activity | 0.29* | 0.29* | 0.20* | 0.55* | 1.00 | |
| Coworker social undermining for physical activity | 0.19* | 0.19* | 0.28* | 0.40* | 0.55* | 1.00 |
level of significance set at p < 0.05
p-value<0.0001
Table 3 presents effect estimates for baseline support and social undermining by source for each behavioral domain in association with weight from fully-adjusted multivariable linear mixed regression models. Results indicated that friend support for healthy eating (β=−0.15; p=0.0010), coworker support for healthy eating (β=−0.11; p=0.026), and family support for physical activity (β=−0.032; p=0.034) were associated with reduced weight at 24 months, whereas family social undermining for healthy eating was associated with weight gain at 24 months (β=0.12; p=0.0019). All other sources of support and social undermining were not associated with change in weight. No significant interactions effects were observed. Primary associations of interest were not significant at 12 months.
Table 3.
Results from a Multivariable Linear Mixed Effects Regression Model* Examining Type and Source of Support and Social Undermining Associated with 24-month Weight Change (kg) among School Employees (N=633)
| Effect estimate (95% CI) | p-value† | |
|---|---|---|
| Support for Healthy Eating | ||
| Family | −0.029 (−0.31, 0.091) | 0.35 |
| Friends | −0.15 (−0.24, −0.063) | 0.0010 |
| Coworkers | −0.11 (−0.21, −0.013) | 0.026 |
| Social Undermining for Healthy eating | ||
| Family | 0.12 (0.044, 0.20) | 0.0019 |
| Friends | −0.068 (−0.18, 0.038) | 0.21 |
| Coworkers | 0.0054 (−0.11, 0.10) | 0.92 |
| Support for Physical Activity | ||
| Family | −0.032 (−0.063, −0.0023) | 0.034 |
| Friends | −0.020 (−0.054, 0.015) | 0.27 |
| Coworkers | 0.034 (−0.050, 0.073) | 0.089 |
| Social Undermining for Physical Activity | ||
| Family | −0.10 (−0.35, 0.14) | 0.41 |
| Friends | 0.17 (−0.20, 0.54) | 0.38 |
| Coworkers | −0.12 (−0.51, 0.27) | 0.59 |
adjusted for all sources of support and social undermining for healthy eating and physical activity, gender, age, education level, intervention status, time, and clustering of individuals within schools
level of significance set at p < 0.05
Discussion
Despite widespread recognition that social support is an important component of weight control, this study is among the first to assess perceived social support from a variety of sources in association with change in weight. The current study is also among the first to examine associations between perceived social undermining and weight in sample of men and women. Our results indicated that friend and coworker support for healthy eating and family support for physical activity was associated with slight weight reduction at 24 months.
Healthy eating
Individuals with higher friend and coworker support for healthy eating lost weight, with an estimated 0.15 and 0.11 kg decrease in weight, respectively, for each unit increase in support scores. Relatively little is known about the influence of friend and coworker support on healthy eating behaviors and weight among adults. Our finding contrasts with Ball and Crawford’s observational study (16) indicating no association between friend support for healthy eating and two-year weight change among young women. One possible explanation for the divergent findings may be the relative absence of perceived support for healthy eating from friends compared with family members. Qualitative research among low-income Latina women indicated that lack of friends to provide advice about food was a key barrier to healthy weight management (30). Results from a group-based behavioral weight loss program targeting women showed that participants who never received friend support for healthy eating were actually most likely to lose weight compared to those who experienced higher frequency of friend support (6); investigators speculate that this surprising finding may be due to the group-based intervention providing support that was lacking from participants’ existing friendships. With respect to support from coworkers, cross-sectional findings from Tamers and colleagues (8) demonstrated a positive association between level of worksite social support and mean fruit and vegetable intake but no association with BMI among adult employees. Our results suggest that while friend and coworker support for healthy eating may be lacking or less frequent compared to support from family members, friends and coworkers comprise important sources of support for healthy eating.
Family support for healthy eating did not influence participants’ change in weight, whereas family social undermining of healthy eating was associated with weight gain over a two year period. One possible explanation for this finding is that family members concurrently provide support and social undermining for healthy eating, as supported by the positive correlations between family support and social undermining for healthy eating observed in this study sample. For example, while supportive of individual efforts to lose or maintain weight in some situations, family members may also intentionally or unintentionally undermine efforts in other situations. The positive correlations between support and social undermining may also reflect different social interactions within each source; one family member may provide support for healthy eating while another family member who exerts a stronger influence on eating behaviors may undermine healthy eating efforts. Qualitative research among low-income women indicate that partner support is a critical motivator for weight loss, yet difficulty in changing family-centered behaviors, such as unhealthy eating, presented a major barrier for weight loss efforts (30–32). Several studies indicate that accommodating family members’ food preferences (i.e., partners/spouses and other family members who refused to eat healthy foods) deterred women’s efforts to eat healthy and manage their weight (30, 32, 33). Interventions that include family-oriented sessions may enhance family support, reduce family social undermining, and foster family-level changes in healthy eating that may ultimately lead to successful and sustained healthy weight management (31).
Physical activity
Study results indicated that individuals with higher family support for physical activity on average had a 0.032 kg decrease in weight at 24 months for each unit increase in support scores. Companionship from family members and friends is associated with increased physical activity levels among adults (34–36), with qualitative research indicating that physical activity companions provide support for physical activity through motivational, social, facilitative, and instructional roles (37). These findings along with results from our study suggest that among adults, family support for physical activity may be an important intervention target for healthy weight management.
A possible reason why friend and coworker support for physical activity were not associated with weight change in this study may be the limited opportunities for friends and coworkers to influence physical activity behaviors, as adult employees are likely to have more leisure time exposure (frequency and duration) with family members than with friends and coworkers. The null finding of the influence of friend support for physical activity contradicts results from a previous study indicating that friend support for physical activity was associated with less weight gain over time (16), although the study was conducted among young adult women who had different demographic, behavioral, and weight status profiles compared to our study sample of adult employees.
The current study’s finding that social undermining for physical activity (from any source) was not associated with weight change may be due to the limited number of opportunities or situations for family members, friends, and/or coworkers to deter efforts to be physically active (i.e., criticize the individual for exercising) compared to the number of opportunities or situations that deter efforts to eat healthfully (i.e., eat unhealthy foods in front of the individual, refuse to eat healthy foods with the individual, bring unhealthy foods to the individual, or encourage the individual to indulge in unhealthy foods). Additionally, the restricted range of the physical activity social undermining subscale may have limited the detection of a significant association. Further research on the association between support and social undermining for exercise and weight management over time and the differential roles of family, friends and coworkers in providing exercise support or social undermining on weight are needed.
As participants were part of a worksite weight gain prevention study and results were pooled across intervention status, substantial weight change was not anticipated. While the modest weight change observed in the current study is not clinically significant, small shifts in population weight may result in large population benefit (38). The worksite-based intervention specifically targeted worksite support (25); thus, increases in perceived coworker support for physical activity were seen among intervention participants over time as hypothesized, with no significant changes in family, friend, or coworker support observed for the overall study sample. These findings suggest that strategies to help individuals: 1) solicit support (either from existing members of their social network and/or from new members) among those reporting low support for healthy eating and physical activity; and 2) navigate social undermining of healthy eating and physical activity among those reporting frequent social undermining may be key intervention targets for clinicians, practitioners, and investigators. Consistent with a previous worksite intervention targeting obesity among hospital employees (39), findings demonstrate the potential of worksite wellness interventions to increase perceived coworker support for physical activity. Although previous worksite studies targeting weight suggest an inconclusive association between worksite social support and health behavior change (8, 40), results from the current study warrant further investigation of the relation between support, social undermining, behavior, and weight across numerous sources.
Strengths and limitations
This study addresses important gaps in the literature by examining longitudinal associations between social support, social undermining, and weight. To our knowledge, this is the first study to examine family, friend, and coworker support and social undermining associated with weight over time among male and female adults, the majority of whom were overweight or obese. Importantly, this study distinguished between positive and negative social influences by examining summary scores of support and social undermining for each behavioral domain and each reference group.
Findings from this study should be considered within the context of several limitations. As the study sample comprised of voluntary participants who enrolled in the worksite weight gain prevention study, participants may be more motivated to engage in weight gain prevention efforts (and thus demonstrate weight loss) than non-participants. Additionally, measurement bias may have accounted for the observed results (e.g., participants inclined to report greater social support at baseline may be more motivated to manage their weight throughout the study duration than those inclined to report infrequent social support, and those inclined to report greater social undermining at baseline may be less motivated). As the scales assessed frequency of social interactions, the positive correlations between support and social undermining suggest the possibility of responses reflecting frequency of contact by source rather than perceived support and social undermining by source. Measurement limitations include the restricted variability of most predictors, in particular the physical activity social undermining variable. As family, friends, and coworkers were each examined as distinct sources, perceived frequency of support and social undermining is likely to be within the middle of the response range, rather than the extremes. Additionally, the original instrument was designed to assess support from family members and friends (26), and certain items (e.g., gave me rewards for exercising) may be more relevant to assess among close family members than coworkers. Scales did not capture the number of sources or divergence in the presence or absence of support and social undermining (e.g., one family member may provide support while another family member may not) within each referent group. Thus, advancements in the measurement of social support and social undermining across a variety of sources are needed. The small school sample size and specific study population (public high school employees of predominantly White racial/ethnic background) limits generalizability of findings to other populations.
Conclusion
Findings from this study contribute to our understanding of the role of social support and social undermining from various sources on weight. Obesity and weight management interventions should include strategies that solicit support to help adults lose and/or maintain weight and overcome social influences and interactions that undermine healthy eating efforts. Further research on the associations between social support and social undermining for healthy weight management behaviors and weight in other populations, particularly socioeconomically disadvantaged and racial/ethnic minority populations at greatest obesity risk, is warranted. Understanding which sources exert the most influence on weight may inform the tailoring of intervention strategies and settings for the target population.
What is already known about this subject.
Social relationships can have positive and negative influences on eating behaviors, physical activity, and weight status.
Social support is associated with improved eating and physical activity behaviors.
Family and friends comprise key sources of support for healthy weight management.
What this study adds.
Social support and social undermining for healthy eating and physical activity from different sources have distinct longitudinal associations with change in weight among male and female employed adults.
Friend and coworker social support for healthy eating and family support for physical activity were associated with slight weight reduction over time.
Family social undermining of healthy eating was associated with weight gain.
Acknowledgments
ML Wang conceived the research question and analyzed the data. All authors were involved in writing the manuscript and have approved the submitted version. We thank Karen Ronayne and Susan Garland for their roles in implementing the intervention and Dante Simone and Nancy O’Mealey for their roles in data collection. We also thank the project coaches, leadership and staff at each of the participating schools. This research was funded by grant number R01 CA132941 from the National Cancer Institute and cooperative agreement number U48 DP001933, awarded to the University of Massachusetts Worcester Prevention Research Center through the CDC Prevention Research Center program.
Footnotes
Clinical Trial: ClinicalTrials.gov; Identifier: NCT01467284
Conflicts of Interest
The authors have no conflicts of interest to disclose.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. NCHS data brief, no 82. Hyattsville, MD: National Center for Health Statistics; 2012. Prevalence of obesity in the United States, 2009–2010. [PubMed] [Google Scholar]
- 2.Faith MS, Kral TVE. Social Environmental and Genetic Influences on Obesity and Obesity-Promoting Behaviors: Fostering Research Integration. In: Hernandez LM, Blazer DG, editors. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. Washington, D.C.: National Academies Press; 2006. [PubMed] [Google Scholar]
- 3.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–9. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 4.Leahey TM, Gokee LaRose J, Fava JL, Wing RR. Social influences are associated with BMI and weight loss intentions in young adults. Obesity (Silver Spring) 2011;19(6):1157–62. doi: 10.1038/oby.2010.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oliveira AJ, Rostila M, de Leon AP, Lopes CS. The influence of social relationships on obesity: sex differences in a longitudinal study. Obesity (Silver Spring) 2013;21(8):1540–7. doi: 10.1002/oby.20286. [DOI] [PubMed] [Google Scholar]
- 6.Kiernan M, Moore SD, Schoffman DE, Lee K, King AC, Taylor CB, et al. Social support for healthy behaviors: scale psychometrics and prediction of weight loss among women in a behavioral program. Obesity (Silver Spring) 2012;20(4):756–64. doi: 10.1038/oby.2011.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tamers SL, Okechukwu C, Allen J, Yang M, Stoddard A, Tucker-Seeley R, et al. Are social relationships a healthy influence on obesogenic behaviors among racially/ethnically diverse and socio-economically disadvantaged residents? Prev Med. 2013;56(1):70–4. doi: 10.1016/j.ypmed.2012.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tamers SL, Beresford SA, Cheadle AD, Zheng Y, Bishop SK, Thompson B. The association between worksite social support, diet, physical activity and body mass index. Prev Med. 2011;53(1–2):53–6. doi: 10.1016/j.ypmed.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fuemmeler BF, Masse LC, Yaroch AL, Resnicow K, Campbell MK, Carr C, et al. Psychosocial mediation of fruit and vegetable consumption in the body and soul effectiveness trial. Health Psychol. 2006;25(4):474–83. doi: 10.1037/0278-6133.25.4.474. [DOI] [PubMed] [Google Scholar]
- 10.Langenberg P, Ballesteros M, Feldman R, Damron D, Anliker J, Havas S. Psychosocial factors and intervention-associated changes in those factors as correlates of change in fruit and vegetable consumption in the Maryland WIC 5 A Day Promotion Program. Ann Behav Med. 2000;22(4):307–15. doi: 10.1007/BF02895667. [DOI] [PubMed] [Google Scholar]
- 11.Kelsey KSKB, DeVellis R, Earp JA, Ammerman A, Keyserling T, Shannon J, Simpson RJ., Jr Social support as a predictor of dietary change in a low-income population. Health Educ Res. 1996;11:383–395. doi: 10.1177/109019819702400308. [DOI] [PubMed] [Google Scholar]
- 12.Schaffer MA, Lia-Hoagberg B. Effects of social support on prenatal care and health behaviors of low-income women. J Obstet Gynecol Neonatal Nurs. 1997;26(4):433–40. doi: 10.1111/j.1552-6909.1997.tb02725.x. [DOI] [PubMed] [Google Scholar]
- 13.(NCI) NCI. NCI Dictionary of Cancer Terms: social support. [Google Scholar]
- 14.Berkman LF, Glass T. Social integration, social networks, social support and health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 137–173. [Google Scholar]
- 15.Heaney CA, Israel BA. Social networks and social support. In: Glanz KRB, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4. San Francisco, CA: Jossey-Bass; 2008. pp. 189–210. [Google Scholar]
- 16.Ball K, Crawford D. An investigation of psychological, social and environmental correlates of obesity and weight gain in young women. Int J Obes (Lond) 2006;30(8):1240–9. doi: 10.1038/sj.ijo.0803267. [DOI] [PubMed] [Google Scholar]
- 17.Sallis J, Owen N. Physical activity and behavioral medicine. Thousand Oaks, CA: Sage Publications; 1999. [Google Scholar]
- 18.Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: Review and update. Med Sci Sports Exerc. 2002;34(12):1996–2001. doi: 10.1097/00005768-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 19.Kamphuis CB, Giskes K, de Bruijn GJ, Wendel-Vos W, Brug J, van Lenthe FJ. Environmental determinants of fruit and vegetable consumption among adults: A systematic review. Br J Nutr. 2006;96(4):620–35. [PubMed] [Google Scholar]
- 20.Shaikh AR, Yaroch AL, Nebeling L, Yeh MC, Resnicow K. Psychosocial predictors of fruit and vegetable consumption in adults a review of the literature. Am J Prev Med. 2008;34(6):535–543. doi: 10.1016/j.amepre.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 21.Elliot DL, Goldberg L, Duncan TE, Kuehl KS, Moe EL, Breger RK, et al. The PHLAME firefighters’ study: feasibility and findings. Am J Health Behav. 2004;28(1):13–23. doi: 10.5993/ajhb.28.1.2. [DOI] [PubMed] [Google Scholar]
- 22.Beresford SA, Locke E, Bishop S, West B, McGregor BA, Bruemmer B, et al. Worksite study promoting activity and changes in eating (PACE): design and baseline results. Obesity (Silver Spring) 2007;15(Suppl 1):4S–15S. doi: 10.1038/oby.2007.383. [DOI] [PubMed] [Google Scholar]
- 23.Medicine Io. Progress in Preventing Childhood Obesity: How Do We Measure Up? Washington, DC: National Academies Press; 2005. [Google Scholar]
- 24.Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education Theory, Research, and Practice. 4. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- 25.Lemon SC, Wang ML, Wedick NM, Estabrook B, Druker S, Schneider KL, et al. Weight gain prevention in the school worksite setting: Results of a multi-level cluster randomized trial. Prev Med. 2013 doi: 10.1016/j.ypmed.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–36. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 27.Nunnally JC, Bernstein IH. Psychometric Theory. 3. New York: McGraw-Hill; 1994. [Google Scholar]
- 28.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in adults: United States, 2005–2008. NCHS Data Brief. 2010;(50):1–8. [PubMed] [Google Scholar]
- 29.Lewis CE, Jacobs DR, Jr, McCreath H, Kiefe CI, Schreiner PJ, Smith DE, et al. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol. 2000;151(12):1172–81. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 30.Thornton PL, Kieffer EC, Salabarria-Pena Y, Odoms-Young A, Willis SK, Kim H, et al. Weight, diet, and physical activity-related beliefs and practices among pregnant and postpartum Latino women: the role of social support. Matern Child Health J. 2006;10(1):95–104. doi: 10.1007/s10995-005-0025-3. [DOI] [PubMed] [Google Scholar]
- 31.Setse R, Grogan R, Cooper LA, Strobino D, Powe NR, Nicholson W. Weight loss programs for urban-based, postpartum African-American women: perceived barriers and preferred components. Matern Child Health J. 2008;12(1):119–27. doi: 10.1007/s10995-007-0211-6. [DOI] [PubMed] [Google Scholar]
- 32.Chang MW, Nitzke S, Guilford E, Adair CH, Hazard DL. Motivators and barriers to healthful eating and physical activity among low-income overweight and obese mothers. J Am Diet Assoc. 2008;108(6):1023–8. doi: 10.1016/j.jada.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 33.Chang MW, Baumann LC, Nitzke S, Brown RL. Predictors of fat intake behavior differ between normal-weight and obese WIC mothers. Am J Health Promot. 2005;19(4):269–77. doi: 10.4278/0890-1171-19.4.269. [DOI] [PubMed] [Google Scholar]
- 34.Kieffer EC, Willis SK, Arellano N, Guzman R. Perspectives of pregnant and postpartum latino women on diabetes, physical activity, and health. Health Educ Behav. 2002;29(5):542–56. doi: 10.1177/109019802237023. [DOI] [PubMed] [Google Scholar]
- 35.Hovell M, Sallis J, Hofstetter R, Barrington E, Hackley M, Elder J, et al. Identification of correlates of physical activity among Latino adults. J Community Health. 1991;16(1):23–36. doi: 10.1007/BF01340466. [DOI] [PubMed] [Google Scholar]
- 36.Collins R, Lee RE, Albright CL, King AC. Ready to be physically active? The effects of a course preparing low-income multiethnic women to be more physically active. Health Educ Behav. 2004;31(1):47–64. doi: 10.1177/1090198103255529. [DOI] [PubMed] [Google Scholar]
- 37.Harley AE, Katz ML, Heaney CA, Duncan DT, Buckworth J, Odoms-Young A, et al. Social support and companionship among active African American women. Am J Health Behav. 2009;33(6):673–85. doi: 10.5993/ajhb.33.6.5. [DOI] [PubMed] [Google Scholar]
- 38.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14(1):32–8. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- 39.Lemon SC, Zapka J, Li W, Estabrook B, Rosal M, Magner R, et al. Step ahead a worksite obesity prevention trial among hospital employees. Am J Prev Med. 2010;38(1):27–38. doi: 10.1016/j.amepre.2009.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tamers SL, Thompson B, Cheadle AD, Zheng Y, Bishop SK, Beresford SA. Promoting Changes in Obesogenic Behaviors: Does Coworker Social Support Play a Role? Am J Health Promot. 2014 doi: 10.4278/ajhp.130709-ARB-352. [DOI] [PubMed] [Google Scholar]


