Abstract
Introduction
Diabetes disproportionately affects underserved racial/ethnic groups in the United States. Diabetes prevention interventions positively influence health; however, further evaluation is necessary to determine what role culture plays in effective programming. We report on the status of research that examines cultural adaptations of diabetes prevention programs.
Methods
We conducted database searches in March and April 2014. We included studies that were conducted in the United States and that focused on diabetes prevention among African Americans, American Indians/Alaska Natives, Asian Americans/Pacific Islanders, and Latinos.
Results
A total of 58 studies were identified for review; 29 were excluded from evaluation. Few adaptations referenced or followed recommendations for cultural adaptation nor did they justify the content modifications by providing a rationale or evidence. Cultural elements unique to racial/ethnic populations were not assessed.
Conclusion
Future cultural adaptations should use recommended processes to ensure that culture’s role in diabetes prevention–related behavioral changes contributes to research.
Introduction
Almost 29 million US adults have diabetes, and as many as 86 million have prediabetes (1). The high rate of diabetes among US minority populations is concerning because diabetes is a risk factor for cardiovascular disease, vision loss, end stage renal disease, disability, and mortality (2). From 2010 through 2012, African Americans (13.2%), American Indians/Alaska Natives (AI/ANs) (15.9%), Asian Americans and other Pacific Islanders (9.0%), and Latinos (12.8%) were more often diagnosed with diabetes than were non-Hispanic whites (7.6%) (1). Diabetes is preventable through lifestyle changes that may also assist in diabetes control.
The Institute of Medicine (IOM) examined the impact of social and cultural environments on health outcomes and recommends that research advance in this area (3). According to the IOM report, health behaviors and other social variables occur in a cultural context that must be understood to determine which cultural variables influence adoption of health recommendations.
There is evidence that interventions (eg, for cancer care, mental health, health education) that emphasize integration of cultural knowledge (ie, ideas, rules of etiquette, and knowledge needed in social life) improve outcomes among adults (4–6). Emerging data suggest similar effects in diabetes interventions (7). Although data on cultural adaptations for youths are equivocal (5) and concerns have been raised about the impact and consequences of constituency involvement in assessments of cultural appropriateness for public health interventions (8), further evaluation is warranted to determine the key factors affecting outcomes.
Castro et al (9) suggest that the aim of cultural adaptations should be “to generate a culturally equivalent version of a model prevention program” when elements in the original intervention produce resistance to program activities or are in conflict with cultural attitudes. Castro et al (5) identified steps to guide decisions to culturally adapt evidence-based interventions, which involves justification of the effort. Justification for adaptation may be based on previous failure to engage members of priority populations or the presence of unique cultural risk factors and symptoms, or both. Once justified, an evidence-based intervention is selected and cultural adaptations of content and delivery are completed (5).
Frameworks for cultural adaptations have emerged in 2 forms. One form involves modification within content categories (10–12), with early discussions emphasizing “surface” and “deep structures” of modification (11). “Surface structure” modifications involve inclusion of photos, symbols, and recruitment and outreach strategies (11). Resnicow et al refer to “deep structure” as recognizing, reinforcing, and building on a group’s values and behaviors to provide context and meaning to important intervention components (11). The framework proposed by Kreuter et al further specifies surface and deep cultural elements (10). Culturally sensitive programming requires changes to peripheral, evidential, linguistic, constituent-involving, and sociocultural categories (10). Peripheral approaches focus on colors, fonts, photographs, or declarative titles. Linguistic strategies assure that all intervention materials are in the preferred language of the group (12). Evidential approaches make use of testimonials, narratives, stories, and statistics specific to the group and raise awareness of perceived vulnerability to the health issue (10). Constituent-involving strategies include hiring or training group members or from the community or extensively engaging the community (10), which takes advantage of members’ insider knowledge about the community’s health perceptions and may increase acceptability and relevance (13). Sociocultural approaches discuss disease in the context of social or cultural characteristics (eg, including traditional foods and physical activities) (10).
The second form of cultural adaptation frameworks defines the steps of the intervention adaptation process (5,9,14) and offers the opportunity for a systematic process. The PEN-3 model completes cultural adaptions in 2 phases that support community input on the appropriate adaptation elements. The first phase, assessment, involves information gathering to learn about the community and its perspective (the resources that promote [ie, nurturers] or inhibit [ie, barriers] behavioral change and the roles that friends and family play in behavioral change). Once this information is gathered, the community and researchers use assessment data to critique current strategies and collaboratively develop culturally appropriate interventions (14).
Barrera et al (6) reviewed the past decade’s literature to identify elements that are common to cultural adaptations of behavioral health interventions relevant for diabetes interventions. The authors report 5 stages of cultural adaptation that are a refinement of earlier recommendations: information gathering, preliminary design, preliminary testing, refinement, and final trials (3,6). The review suggests that interventions involving the inclusion of cultural elements in an adaptation are more effective than control or usual care conditions (6). The authors recommended that studies evaluate cultural adaptations completed in these stages.
In this article, we examine the cultural adaptation of diabetes prevention programs and the extent to which the call for research advances in this area is being met. We also examine content and characteristics of cultural adaptations and the extent to which the recommended “how” and “what” of adaptation have been adopted. Recommendations for next steps are provided.
Methods
The studies included in this review were compiled from a search of computerized databases conducted in March and April of 2014. The search performed was Academic Search Complete, and the following databases were selected: Academic Search Complete, CINAHL (Cumulative Index to Nursing and Allied Health Literature), CINAHL Plus, Family and Society Studies Worldwide, Global Health, Global Health Archive, Medline, PsycINFO, and Social Work Abstracts. Research published from 2004 through 2014 was included to capture systematic research of cultural adaptations of diabetes prevention programs among ethnic minorities (3,6,10–12). Key words were used to search titles, abstracts, and subject headings in all databases. The Boolean search used key words, including “Diabetes Prevention Program” or “DPP” or “diabetes prevention” and “translation” or “translating” and “African American” or “African-American” or black or “American Indian” or “Native American” or “Latino” or “Latina” or “Hispanic” or “Asian” or “Asian American”; “Diabetes Prevention Program” or “DPP” or “diabetes prevention” and “translation” or “translating” and “sociocultural” or “cultural adaptation” or “sociocultural adaptation.” A supplemental search used the terms “PEN-3” and “deep culture” to identify additional articles.
Each study identified had to meet the following criteria for inclusion: 1) was a quantitative or qualitative research study completed in the United States; 2) had diabetes prevention as the primary focus, research question, or hypothesis of the study; 3) had diabetes education and interventions aimed at prevention activities, such as diet, exercise or physical activity, or health communication; and 4) included group-specific analyses on African Americans, AI/AN, Asian Americans/Pacific Islanders, or Latinos (although these priority populations did not have to be the only group studied). The reference lists of these articles were reviewed to identify other studies that met the inclusion criteria. Review articles, meta-analyses, dissertation abstracts, and articles in languages other than English were excluded from this evaluation. Journal articles reporting data from a single study were reported separately but evaluated as a single study.
Included studies were evaluated for 1) study population included; 2) diabetes prevention activity and program studied; 3) cultural adaptation process used; 4) formative research completed and analytic method (quantitative or qualitative) used; 5) cultural components and attributes (ie, peripheral, linguistic, evidential, sociocultural, constituent-involving) included to address values, attitudes, and behaviors; 6) inclusion of community strengths and resources in program or intervention; 7) channel or media selected or used in intervention; and 8) unique cultural elements assessed (eg, inclusion of spiritual factors, identity, rituals). Studies were coded by a graduate research assistant trained by the first author (V.L.S.). The first author then reviewed all studies and coding to resolve questions identified by the graduate research assistant or the author.
Results
A total of 58 published manuscripts were initially identified; 29 were excluded from the evaluation. A total of 29 studies were included in the qualitative synthesis for this review (Figure).
Figure.
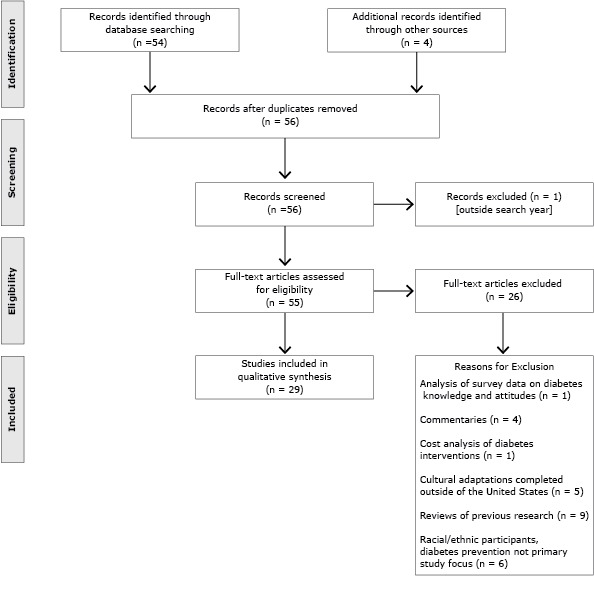
Number and reasons for article exclusion. Qualitative review of use of culturally focused theoretical frameworks for adaptations of diabetes prevention programs, United States, 2014.
Most studies addressed adaptation of diabetes prevention programs for Latinos (44.8%; Mexican, Puerto Rican, Dominican, and Caribbean) (15–27) and African Americans (31.0%) (28–36). Other adaptations were found for Asian Americans (2 studies: Korean, Filipino/Pacific Islanders) (37,38), AIs (4 studies: Northern Plains Indians, AI/ANs, urban southwest Indian) (39–42), and 1 study focused on a combined population (43) (Latinos/African Americans). One study focused on men (20), and 4 studies targeted women or involved mostly women (17,26,32,42) (Table 1).
Table 1. Summary of Diabetes Prevention Program Cultural Adaptations, by Race/Ethnicity, United States, 2014a .
| Characteristic | Latino (n = 13) | African American (n = 10) | American Indian/ Alaska Native (n = 4) |
Asian American (n = 2) |
|---|---|---|---|---|
| Demographic | ||||
| Female only | 2 | 1 | 1 | 0 |
| Male only | 1 | 0 | 0 | 0 |
| Youth | 1 | 2 | 3 | 0 |
| Program modified | ||||
| Diabetes Prevention Program | 8 | 6 | 4 | 2 |
| Other | 3 | 3 | 0 | 0 |
| Cultural adaptation | 13 | 9 | 4 | 2 |
| Adaptation uses theoryb | ||||
| Cultural | 2 | 0 | 0 | 0 |
| Other theory | 7 | 3 | 1 | 2 |
| Study type | ||||
| Formative only | 4 (mean, 46.3 [range, 16–100]) | 1 (N = 25) | 1 (N = 31) | 1 (N = 127) |
| Pilot/feasibility | 5 (mean, 31.4 [range, 12–91]) | 5 (mean, 32.8 [range, 8–62]) | 1 (N = 64) | 1 (N = 48) |
| Trial | 3 (mean, 175 [range, 69–312]) | 1 (N = 604) | 1 (N = 2,553) | 0 |
| Latino/African American, 1 (n = 183) | ||||
| Level of adaptationc | ||||
| Surface | 4 | 3 | 2 | 2 |
| Deep | 13 | 6 | 3 | 2 |
| Outcome | ||||
| Weight (eg, loss, BMI) | 7 | 5 | 1 | 2 |
| A1c, glucose, insulin sensitivity | 2 | 2 | 0 | 1 |
| Physical activity | 4 | 3 | 1 | 1 |
Abbreviations: A1c, hemoglobin A1c; BMI, body mass index.
Values are whole numbers unless otherwise indicated. Values in columns may not sum to total or may exceed total value for n, because studies could adapt to accommodate more than 1 attribute or could report more than 1 outcome.
Theory-driven cultural adaptation process: C, cultural (PEN-3, Castro et al, 2010 [5]); OT, other theory/model (eg, community-based participatory research, social-cognitive theory, grounded theory).
Level of adaptation adapted from Resnicow et al (11).
The Diabetes Prevention Program (DPP) was the dominant evidence-based program subject to adaptation (84.6%). Of the 7 non-DPP adaptations, 1 was based on a program (Group Lifestyle Balance Program) (19) that was an earlier adaptation of DPP. DPP was adapted for each of the racial/ethnic categories.
Despite the availability of guidelines for completing the cultural adaptation process (3,6,9,14) and identifying potential areas for content modification (8,9), few studies referenced these approaches to cultural adaptation (15,16). The studies using cultural adaptation used Barrera et al (6), with a reference to Resnicow et al (11) and Airhihenbuwa’s PEN-3 model (14). Eleven adaptations (17,20,22,23,26–28,36,37,39,43) used various other frameworks, with community-based participatory research (CBPR) most widely cited (24.1%) (Table 2).
Table 2. Detailed Summary of Diabetes Prevention Programs Evaluated for Cultural Adaptations, United States, 2014.
| Author | Population | Program Modified |
Cultural Adaptation | Adaptation Process |
Formative Studies |
Content Category)a |
Nurturer/ Barriers)b |
Community Resources |
|---|---|---|---|---|---|---|---|---|
| Atkinson et al, 2009 (28) | African American | Church-based DPP | Yes | Grounded theory | Yes | E, S, C | N, B | Church |
| Boltri et al, 2011 (30) | African American | Group lifestyle DPP |
Yes | — | No | S | N | Church |
| Boltri et al, 2008 (31) | African American | DPP | Yes | — | No | L, S | N | Church |
| Brown et al, 2010 (39) | Northern Plains, AI youth | DPP | Yes | CBPR | Yes | See below | N,B | Montana reservation |
| Brown et al, 2013 (40) | Northern Plains, AI youth |
DPP | Yes | — | See Brown et al, 2010 | P, L, E, S, C | N,B | Montana reservation |
| Burnet et al, 2011 (29) | African American (9-12 yrs) |
Reach out | Yes | — | Yes | L, S | N, B | — |
| Chasan-Taber et al, 2014 (17) | Latina (pregnant) | Lifestyle intervention |
Yes | Socio-cognitive/ TTM |
Yes | L | B | — |
| Coleman et al, 2010 (18) | Latino Family | DPP | Yes | — | No | L, S | N, B | School |
| Cox et al, 2013 (32) | African American, women |
DPP | Yes | — | No | C | — | — |
| Gutierrez et al, 2014 (43) | African American, Latino |
DPP | Yes | CBPR | Yes | L, S | N, B | Church |
| Islam et al, 2013 (37) | Korean American | DPP | Yes | CBPR | Yes | P, E, L, S | N, B | — |
| Jiang et al, 2013 (41) | AI/AN youth | DPP | Yes | — | Yes | S | N, B | — |
| Kramer et al, 2013 (19) | Hispanic | GLB (DPP adaptation) | Yes | — | No | L, S | N | WIC |
| Mau et al, 2010 (38) | Filipino, Pacific Islander | DPP | Yes | CBPR | Yes | P,E, L, S,C | — | Gurdwara sites |
| Martinez et al, 2012 (20) | Male Mexican Immigrant | Formative | Yes | Socio-Ecological Model | Yes | L, S | N, B | — |
| Melancon et al, 2009 (16) | Mexican American and Mexican Native | Formative | Yes | PEN-3 | Yes | S, C | N, B | — |
| Merriam et al, 2009 (see Ockene) (21) | Latino (Caribbean) |
DPP | Yes | — | No | P, L, S | — | YWCA |
| Millard et al, 2011 (22) | Immigrant Hispanic | Diabetes Empowerment Education Program | Yes | CBPR, TTM, Socio-Ecological Model | No | L, S, C | N, B | — |
| Ockene, et al, 2012 (23) | Dominican/Puerto Rican Spanish speakers | DPP | Yes | Socio-cognitive theory | Yes | L, S | B | YWCA |
| Osuna et al, 2011 (15) | Latino/a | Mediterranean Lifestyle Program | Yes | Castro et al, 2010 | Yes | P, L, S | N, B | — |
| Ramal et al, 2012 (24) | Latino/a, low-income | Formative | Yes | — | Yes | S | N, B | — |
| Ruggiero et al, 2007 (25) | Latino/a, | DPP | Yes | — | No | L, C | — | — |
| Ruggiero et al, 2011 (26) | Spanish speaking | DPP | Yes | CBPR | No | L, C | — | Community settings |
| Shaibi et al, 2012 (27) | Latino, adolescents | DPP | Yes | CBPR | No | S, C | N | YMCA |
| Sharma and Fleming, 2012 (33) | African American, youth | — | No | — | — | — | — | Community-based |
| Tang et al, 2014 (34) | African American | NDEP “Power to Prevent” | Yes | — | No | C | N | Church |
| Wells, 2011 (35) | African American | DPP | Yes | — | — | S | N,B | Church |
| Willging et al, 2006 (42) | American Indian, women, urban Southwest | DPP | Yes | — | Yes | P, S, C | N, B | — |
| Williams et al, 2013 (36) | African American | Fit Body and Soul | Yes | Socio-ecological | Yes | P, E, C | N | Church |
Abbreviations: —, information unavailable or ambiguous; AI, American Indian; AN, Alaska Native; CBPR, community-based participatory research; DPP, Diabetes Prevention Program; NDEP, National Diabetes Education Program.
Content categories: P, peripheral; L, linguistic; E, evidential; S, sociocultural; C, constituent involving.
N, nurturers; B, barriers. Adapted from Airhihenbuwa (14).
Approximately 55.6% of studies conducted some form of information gathering or formative research in preparation for the cultural modification of an evidence-based program (15–17,23,24,28,31,36–43). Most studies collected qualitative data or used mixed methods. The primary data collection methods included focus groups for qualitative studies (n = 11) and surveys for quantitative studies (n = 4).
Four studies (25,32,34,36) focused only on surface adaptations of the intervention programs (10); an additional 7 combined surface and deep content modifications (15,21,26,37,38,40,42). Efforts included the use of community locations for meetings and organizations to assist in recruiting (21,26,34,36,38–40). Beyond churches (24.1%), the YMCA/YWCA (10.3%) was the most frequently identified community resource used in (primarily Latino) cultural adaptations. Five studies (17.2%) reported the use of racial/ethnic media for recruitment, dissemination of information, or education (21,28,31,37,38).
Of the studies completing adaptations of deep structure (n = 23), most (91.3%) used sociocultural adaptations (15,16,18–24,27–31,35–38,40,41,43), which included modifications of recipes, cooking and tasting demonstrations, recommendations for physical activity, leaders as role models and to deliver content, and the use of talking circles, storytelling, narratives, novellas, and soap opera video formats; this was followed by linguistic adaptations (61.5%), primarily for Spanish speakers (15,17–23,25,26,30,31,37,38,40,43). In all but 2 instances, language adaptations were combined with other changes. Modifications of evidential components occurred least often (19.2%) (28,36–38,40).
Approximately 52% of studies incorporated both nurturing elements of culture (promotes healthy behaviors) and cultural barriers (inhibits healthy behaviors) (15,16,18,20,22,24,28,31,35,37,39–43). Two studies (6.9%) focused solely on barriers (17,23), and 6 (20.7%) focused exclusively on nurturing elements (19,27,29,30,34,36). Nurturing elements focused on gaining support of elders and church leaders, prayer and spirituality, collectivism, and social support (14). Barriers focused on mistrust, privacy concerns, concerns about neighborhood safety and marginalization, and food traditions (14). No studies evaluated program components included as a part of a cultural modification.
Consistent with a recent review of DPP evaluations (44), 18 studies reported outcomes of cultural adaptation feasibility, pilot studies, and trials (13,18,19,22,23,25–27,29–33,37,38,40,41,43), with a primary outcome of weight loss. Seven studies from Latino communities reported weight loss (18,19,22,23,25–27) and improvement in hemoglobin A1c (23) and insulin sensitivity (27). The results of a family focused adaptation were mixed; weight loss and increased physical activity was reported among parents but not among youths (18). The church-based adaptation for Latinos and African Americans (43), 5 studies focused on African Americans (13,29–32), 2 on Asian Americans (37,38), and 1 AI/AN trial (41) reported similar weight loss findings. Two African American (29,30) and 1 Asian American study reported decreased blood glucose levels (37). Among African American studies, a family focused study (31) reported mixed findings, with changes among youths but not parents, and a youth intervention (33) resulted in changes in fat intake among boys but not girls. One AI study reporting a 3-month follow-up (40) failed to produce changes in body mass index.
Discussion
This analysis suggests an increasing number of diabetes prevention cultural adaptations across racial/ethnic populations, reporting positive outcomes, primarily weight loss. The lack of comparisons to evidence-based interventions (no control or reliance on usual care controls) made it difficult to ascertain superior cultural adaptations. However, study data combined with the results of a recent diabetes treatment cultural adaptation (7) support the importance of continued research.
Few studies referenced recommendations for cultural adaptation processes or content. Given the recent emergence of some process recommendations, this is understandable (5,6); however, the PEN‑3 model (14) and content recommendations are older (10,11). Although the use of CBPR and various theoretical frameworks resulted in community input into cultural adaptations, a culturally focused approach may increase understanding of how specific cultural health beliefs vary across multiple populations and subpopulations (8) and aid in identification of key mechanisms for change (7).
Also of concern was the limited documentation of the rationale for modifications, as illustrated by Osuna et al (15) and the fact that only 52% of studies involved information gathering or a formative research phase to support the cultural modifications made to the original evidence-based diabetes prevention program. These data may have been reported as subpopulation research studies and may have been missed in our search, or authors omitted this information from study reports. However, a deliberative process should occur to avoid modifications informed by stereotypical or monolithic views of racial/ethnic communities. For example, it should not be assumed that all members of a Latino community speak Spanish as their primary language. Issues related to socioeconomics, religion, and sexual orientation should also be included.
That studies varied in their use of peripheral, linguistic, evidential, sociocultural and constituent-involving strategies is not surprising. As Osuna et al note (15), cultural adaptations should be restricted to issues and elements dictated by current research evidence and data emerging from the information-gathering phase. Although the types of modifications reported in studies seemed effective, the failure to measure participants’ responses to cultural elements is a lost opportunity to understand program acceptance and behavioral change.
Future diabetes prevention cultural adaptations should use recommended processes for cultural adaptation, including justification for the adaptation, the processes of formative research and information gathering and modification, modifications in response to data, reports of refinements based on preliminary studies, and the results of final testing (6). Detailed reporting of adaptations helps researchers develop information on common cultural program modifications and makes replication of the adapted intervention easier (45). To build evidence that diabetes prevention interventions that focus on integration of culture positively influence outcomes, studies should compare cultural adaptations to the original evidence-based intervention. Researchers should also evaluate unique cultural elements included in adaptations to determine their utility. Racial/ethnic groups are not monolithic and the cultural issues that affect their responses to health programs should be examined, with the process recommended by Castro et al (5) guiding efforts.
Acknowledgments
We gratefully acknowledge the support and assistance of Jennifer Gallagher and the staff of the Center for Diabetes Translational Research. Preparation for this article was supported in part by the grant no. P30 DK092950. Dr Baumann is also supported by grants no. R25 MH080916, UL1 TR000448, and NCI U54CA155496.
Footnotes
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.
Suggested citation for this article: Sanders Thompson VL, Johnson-Jennings M, Baumann AA, Proctor E. Use of Culturally Focused Theoretical Frameworks for Adapting Diabetes Prevention Programs: A Qualitative Review. Prev Chronic Dis 2015;12:140421. DOI: http://dx.doi.org/10.5888/pcd12.140421.
References
- 1.National diabetes statistics report: estimates of diabetes and its burden to the United States. Atlanta (GA): Centers for Disease Control and Prevention, United States Department of Health and Human Services; 2014. http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed December 26, 2014.
- 2. Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther 2008;88(11):1254–64. 10.2522/ptj.20080020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hernandez LM, Blazer DG. Genes, behavior, and the social environment: moving beyond the nature/nurture debate. Washington (DC): National Academies Press; 2006. [PubMed] [Google Scholar]
- 4. Kagawa-Singer M, Valdez Dadia A, Yu MC, Surbone A. Cancer, culture, and health disparities: time to chart a new course? CA Cancer J Clin 2010;60(1):12–39. 10.3322/caac.20051 [DOI] [PubMed] [Google Scholar]
- 5. Castro FG, Barrera M Jr, Holleran Steiker LK. Issues and challenges in the design of culturally adapted evidence-based interventions. Annu Rev Clin Psychol 2010;6(1):213–39. 10.1146/annurev-clinpsy-033109-132032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Barrera M Jr, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psychol 2013;81(2):196–205. 10.1037/a0027085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Toobert DJ, Strycker LA, Barrera M Jr, Osuna D, King DK, Glasgow RE. Outcomes from a multiple risk factor diabetes self-management trial for Latinas: ¡Viva Bien! Ann Behav Med 2011;41(3):310–23. 10.1007/s12160-010-9256-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Willging CE, Helitzer D, Thompson J. Sharing wisdom: lessons learned during the development of a diabetes prevention intervention for urban American Indian women. Eval Program Plann 2006;29(2):130–40. 10.1016/j.evalprogplan.2006.01.005 [DOI] [Google Scholar]
- 9. Castro FG, Barrera M Jr, Martinez CR Jr. The cultural adaptation of prevention interventions: resolving tensions between fidelity and fit. Prev Sci 2004;5(1):41–5. 10.1023/B:PREV.0000013980.12412.cd [DOI] [PubMed] [Google Scholar]
- 10. Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav 2003;30(2):133–46. 10.1177/1090198102251021 [DOI] [PubMed] [Google Scholar]
- 11. Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis 1999;9(1):10–21. [PubMed] [Google Scholar]
- 12. Sosa ET, Biediger-Friedman L, Yin Z. Lessons learned from training of promotores de salud for obesity and diabetes prevention. J Health Dispar Res Pract 2013;6(1):1–13. 25215265 [Google Scholar]
- 13. Satterfield D, DeBruyn L, Francis CD, Allen A. Communities reclaim native science and traditional ways to prevent diabetes and promote health. Am Indian Cult Res J 2014;38(1):157–90. [Google Scholar]
- 14. Airhihenbuwa CO. Health and culture: beyond the Western paradigm. Thousand Oaks (CA): Sage Publications; 1995. [Google Scholar]
- 15. Osuna D, Barrera M Jr, Strycker LA, Toobert DJ, Glasgow RE, Geno CR, et al. Methods for the cultural adaptation of a diabetes lifestyle intervention for Latinas: an illustrative project. Health Promot Pract 2011;12(3):341–8. 10.1177/1524839909343279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Melancon J, Oomen-Early J, del Rincon LM. Using the PEN-3 model to assess knowledge, attitudes, and beliefs about Diabetes Type 2 among Mexican American and Mexican Native men and women in north Texas. Int Electron J Health Educ 2009;12:203–21. [Google Scholar]
- 17. Chasan-Taber L, Marcus BH, Rosal MC, Tucker KL, Hartman SJ, Pekow P, et al. Estudio Parto: postpartum diabetes prevention program for hispanic women with abnormal glucose tolerance in pregnancy: a randomised controlled trial — study protocol. BMC Pregnancy Childbirth 2014;14(1):100. 10.1186/1471-2393-14-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Coleman KJ, Ocana LL, Walker C, Araujo RA, Gutierrez V, Shordon M, et al. Outcomes from a culturally tailored diabetes prevention program in Hispanic families from a low-income school: Horton Hawks Stay Healthy (HHSH). Diabetes Educ 2010;36(5):784–92. 10.1177/0145721710377360 [DOI] [PubMed] [Google Scholar]
- 19. Kramer MK, Cepak YP, Venditti EM, Semler LN, Kriska AM. Evaluation of the Group Lifestyle Balance Programme for diabetes prevention in a Hispanic women, infants and children (WIC) programme population in the USA. Diversity Equality Health Care 2013;10(2):73–82. [Google Scholar]
- 20. Martinez J, Powell J, Agne A, Scarinci I, Cherrington A. A focus group study of Mexican immigrant men’s perceptions of weight and lifestyle. Public Health Nurs 2012;29(6):490–8. 10.1111/j.1525-1446.2012.01026.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Merriam PA, Tellez TL, Rosal MC, Olendzki BC, Ma Y, Pagoto SL, et al. Methodology of a diabetes prevention translational research project utilizing a community-academic partnership for implementation in an underserved Latino community. BMC Med Res Methodol 2009;9(1):20. 10.1186/1471-2288-9-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Millard AV, Graham MA, Wang X, Mier N, Sánchez ER, Flores I, et al. Pilot of a diabetes primary prevention program in a hard-to-reach, low-income, immigrant Hispanic population. J Immigr Minor Health 2011;13(5):906–13. 10.1007/s10903-010-9412-y [DOI] [PubMed] [Google Scholar]
- 23. Ockene IS, Tellez TL, Rosal MC, Reed GW, Mordes J, Merriam PA, et al. Outcomes of a Latino community-based intervention for the prevention of diabetes: the Lawrence Latino Diabetes Prevention Project. Am J Public Health 2012;102(2):336–42. 10.2105/AJPH.2011.300357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ramal E, Petersen AB, Ingram KM, Champlin AM. Factors that influence diabetes self-management in Hispanics living in low socioeconomic neighborhoods in San Bernardino, California. J Immigr Minor Health 2012;14(6):1090–6. 10.1007/s10903-012-9601-y [DOI] [PubMed] [Google Scholar]
- 25. Ruggiero L, Rodriguez-Sanchez M, Oros S. Translating the diabetes prevention program’s (DPP) lifestyle intervention to the community: making the connection Latino pilot study. Diabetes 2007;56(suppl)(A226).
- 26. Ruggiero L, Oros S, Choi YK. Community-based translation of the diabetes prevention program’s lifestyle intervention in an underserved Latino population. Diabetes Educ 2011;37(4):564–72. 10.1177/0145721711411107 [DOI] [PubMed] [Google Scholar]
- 27. Shaibi GQ, Konopken Y, Hoppin E, Keller CS, Ortega R, Castro FG. Effects of a culturally grounded community-based diabetes prevention program for obese Latino adolescents. Diabetes Educ 2012;38(4):504–12. 10.1177/0145721712446635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Atkinson MJ, Boltri JM, Davis-Smith M, Seale JP, Shellenberger S, Gonsalves D. A qualitative inquiry into the community and programmatic dimensions associated with successful implementation of church-based diabetes prevention programs. J Public Health Manag Pract 2009;15(3):264–73. 10.1097/01.PHH.0000349741.26985.16 [DOI] [PubMed] [Google Scholar]
- 29. Burnet DL, Plaut AJ, Wolf SA, Huo D, Solomon MC, Dekayie G, et al. Reach-out: a family-based diabetes prevention program for African American youth. J Natl Med Assoc 2011;103(3):269–77. [DOI] [PubMed] [Google Scholar]
- 30. Boltri JM, Davis-Smith M, Okosun IS, Seale JP, Foster B. Translation of the National Institutes of Health Diabetes Prevention Program in African American churches. J Natl Med Assoc 2011;103(3):194–202. [DOI] [PubMed] [Google Scholar]
- 31. Boltri JM, Davis-Smith YM, Seale JP, Shellenberger S, Okosun IS, Cornelius ME. Diabetes prevention in a faith-based setting: results of translational research. J Public Health Manag Pract 2008;14(1):29–32. 10.1097/01.PHH.0000303410.66485.91 [DOI] [PubMed] [Google Scholar]
- 32. Cox TL, Krukowski R, Love SJ, Eddings K, DiCarlo M, Chang JY, et al. Stress management-augmented behavioral weight loss intervention for African American women: a pilot, randomized controlled trial. Health Educ Behav 2013;40(1):78–87. 10.1177/1090198112439411 [DOI] [PubMed] [Google Scholar]
- 33. Sharma S, Fleming SE. One-year change in energy and macronutrient intakes of overweight and obese inner-city African American children: effect of community-based Taking Action Together type 2 diabetes prevention program. Eat Behav 2012;13(3):271–4. 10.1016/j.eatbeh.2012.03.003 [DOI] [PubMed] [Google Scholar]
- 34. Tang TS, Nwankwo R, Whiten Y, Oney C. Outcomes of a church-based diabetes prevention program delivered by peers: a feasibility study. Diabetes Educ 2014;40(2):223–30. 10.1177/0145721713520569 [DOI] [PubMed] [Google Scholar]
- 35. Wells R. Impact of social factors in an African American church-based diabetes prevention program. Paper presented at the American Sociological Association Annual Meeting. Las Vegas (NV): 2011. [Google Scholar]
- 36. Williams LB, Sattin RW, Dias J, Garvin JT, Marion L, Joshua T, et al. Design of a cluster-randomized controlled trial of a diabetes prevention program within African-American churches: the Fit Body and Soul study. Contemp Clin Trials 2013;34(2):336–47. 10.1016/j.cct.2013.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Islam NS, Zanowiak JM, Wyatt LC, Chun K, Lee L, Kwon SC, et al. A randomized-controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community. J Community Health 2013;38(6):1030–41. 10.1007/s10900-013-9711-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mau MK, Keawe’aimoku Kaholokula J, West MR, Leake A, Efird JT, Rose C, et al. Translating diabetes prevention into native Hawaiian and Pacific Islander communities: the PILI ’Ohana Pilot project. Prog Community Health Partnersh 2010;4(1):7–16. 10.1353/cpr.0.0111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Brown BD, Harris KJ, Harris JL, Parker M, Ricci C, Noonan C. Translating the diabetes prevention program for Northern Plains Indian youth through community-based participatory research methods. Diabetes Educ 2010;36(6):924–35. 10.1177/0145721710382582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Brown B, Noonan C, Harris KJ, Parker M, Gaskill S, Ricci C, et al. Developing and piloting the Journey to Native Youth health program in Northern Plains Indian communities. Diabetes Educ 2013;39(1):109–18. 10.1177/0145721712465343 [DOI] [PubMed] [Google Scholar]
- 41. Jiang L, Manson SM, Beals J, Henderson WG, Huang H, Acton KJ, Roubideaux Y. Translating the Diabetes Prevention Program into American Indian and Alaska Native communities: results from the Special Diabetes Program for Indians Diabetes Prevention demonstration project. Diabetes Care 2013;36(7):2027–34. 10.2337/dc12-1250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Willging CE, Helitzger D, Thomspon J. “Sharing Wisdom”: Lessons learned during the development of a diabetes prevention intervention for urban American Indian women. Eval Program Plann 2006;29(2):130–40. 10.1016/j.evalprogplan.2006.01.005 [DOI] [Google Scholar]
- 43. Gutierrez J, Devia C, Weiss L, Chantarat T, Ruddock C, Linnell J, et al. Health, community, and spirituality: evaluation of a multicultural faith-based diabetes prevention program. Diabetes Educ 2014;40(2):214–22. 10.1177/0145721714521872 [DOI] [PubMed] [Google Scholar]
- 44. Johnson M, Jones R, Freeman C, Woods HB, Gillett M, Goyder E, et al. Can diabetes prevention programmes be translated effectively into real-world settings and still deliver improved outcomes? A synthesis of evidence. Diabet Med 2013;30(1):3–15. 10.1111/dme.12018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cabassa LJ, Baumann AA. A two-way street: bridging implementation science and cultural adaptations of mental health treatments. Implement Sci 2013;8(1):90. 10.1186/1748-5908-8-90 [DOI] [PMC free article] [PubMed] [Google Scholar]


