Abstract
Background
Osteosarcoma is the most frequent type of malignant bone tumor in children and adolescents and is associated with a high propensity for lung metastasis. Recent experiments have indicated that PLA2G16 contributes to osteosarcoma progression and metastasis in both mouse and human osteosarcoma cell lines. The aim of this study was to compare the expression of PLA2G16 in non-metastatic and metastatic osteosarcomas to determine whether PLA2G16 expression can serve as a biomarker of osteosarcoma prognosis and metastasis.
Methods
Quantitative real-time PCR was used to examine PLA2G16 mRNA in primary osteosarcoma patients (18 patients without metastases and 17 patients with metastases), and immunohistochemistry (IHC) staining of PLA2G16 was performed on tissue microarrays from 119 osteosarcoma patients. Tumor metastatic behavior and survival of the patients were followed up for a minimum of 36 months and a maximum of 171 months. The prognostic value of PLA2G16 expression was evaluated by the Kaplan–Meier method and a log-rank test. Multivariate Cox regression analysis was used to identify significant independent prognostic factors.
Results
Osteosarcoma patients with metastasis showed a higher expression of PLA2G16 at both the mRNA and protein levels (both at P values< 0.05) than did patients without metastasis. Osteosarcoma patients with positive IHC staining of PLA2G16 expression at primary sites had shorter overall survival and metastasis-free survival (both at P values <0.02). Moreover, multivariate Cox analysis identified PLA2G16 expression as an independent prognostic factor to predict poor overall survival and metastasis-free survival (both P values < 0.03).
Conclusions
This study indicated that PLA2G16 expression is a significant prognostic factor in primary osteosarcoma patients for predicting the development of metastases and poor survival.
Introduction
Worldwide, osteosarcoma is the most frequent primary solid malignant bone tumor in adolescents and young adults [1]. It usually involves long bones and is a highly aggressive tumor that metastasizes primarily to the lungs. The prognosis for patients with metastatic osteosarcoma remains poor with a 5-year survival rate at only 10 to 20%, despite aggressive multi-modality therapy [2, 3]. Thus, it is highly desirable to identify novel targets and develop new strategies that inhibit lung metastasis from the primary osteosarcoma site.
Recently, PLA2G16 has been shown to contribute to osteosarcoma progression and metastasis in both mouse and human osteosarcoma cell lines [4]. PLA2G16 is classified as a Group XVI phospholipase A2 (PLA2G16) and is expressed in most normal tissues [5, 6]. The enzymatic activity of PLA2G16 hydrolyzes the ester bond at the sn-2 position of membrane phospholipids, preferably phosphatidylcholine, and releases free fatty acids (FFA) and lysophospholipid [5], both of which increase proliferation, migration, and metastasis[7–10]. Previously, PLA2G16 was identified as a class II tumor suppressor because it inhibited H-ras-induced transformation [11] and its expression was lost in some human tumor types, including breast, ovary, kidney and testicular germ cell [6, 12]. However, a recent study indicated that PLA2G16 may act to promote cellular growth in a subset of non-small cell lung carcinomas [13]. Furthermore, Cancer Profiling Array I analysis showed that the PLA2G16 expression levels were increased in not only lung but also colon, stomach, and rectum cancers, suggesting that PLA2G16 can act as an oncogene in these tumors [13]. These findings suggested that PLA2G16 may play different roles in various types of malignancies. In this study, we examined PLA2G16 expression in human osteosarcoma patients by quantitative real-time PCR (qRT-PCR) and immunohistochemistry (IHC) assays and determined whether the expression of PLA2G16 can be used as a prognostic or metastasis marker of human osteosarcoma.
Material and Methods
Ethics statement
The research ethics committee of the Cancer Institute and Hospital of Tianjin Medical University (China) provided ethical approval for this study, and all patients provided written informed consent. All specimens were handled and stored anonymously according to ethical and legal standards.
Patients and Samples
Fresh osteosarcoma tissue samples (n = 35) were obtained from 18 primary osteosarcoma patients without metastases and 17 patients with metastases. All patients presented at the Tianjin Medical University Cancer Institute and Hospital between 2006 and 2014.Diagnoses were confirmed by pathological examination. None of the patients had received radiotherapy or chemotherapy before surgery. These tissue samples were frozen in liquid nitrogen and kept at -80°C until RNA extraction.
Primary tumor samples were collected from 119 patients who had undergone surgical treatment for osteosarcoma with pathologic identification in the Cancer Institute and Hospital of Tianjin Medical University (China) from 1996 to 2011.Patients were enrolled in this retrospective study based on the following criteria: diagnosis of osteosarcoma with histopathological assessment, no prior anticancer treatment, and the availability of complete clinicopathologic and follow-up data. Tumor tissue specimens were grouped according to the sixth edition of the TNM classification of the International Union against Cancer (UICC).
Quantitative real-time PCR
The total RNA was extracted and purified with TRIzol reagent (Life Technologies, NY, USA) according to the manufacturer’s instructions. A parallel tube without RT (RT-negative control) was included in the RT reactions and subsequent TaqMan PCR procedures as the control for possible DNA contamination.
The reverse transcription of RNA to cDNA was conducted using a High Capacity cDNA Archive Kit (Applied Biosystems, Foster City, CA). One hundred nanograms of total cDNA were added per 20 μl reaction with sequence-specific primers and Taqman probes. Quantitative gene expression was analyzed for PLA2G16 (Hs00912734_m1) and GAPDH (Hs02758991_g1) with gene-specific probes (Applied Biosystems) using Taqman Universal PCR Master Mix and was carried out in triplicate on an ABI Prism 7900 system according to the manufacturer’s instructions. The data were then quantified using the comparative Ct method for relative gene expression compared with GAPDH as endogenous control.
Tissue Microarrays and Immunohistochemistry
Tissue Microarrays (TMAs) were constructed as previously described [14]. Briefly, samples were fixed in 4% buffered formalin, decalcified using EDTA if required, and embedded in paraffin to construct TMAs. Thick portions of tumors were serially sectioned (4 mm), with the most representative areas of the tumor region carefully selected and sampled for the TMA collector blocks. To validate the concordance between TMAs and whole tumor sections, we further detected PLA2G16 expression for 20 patients randomly chosen from the 119 patients for comparison with whole tumor sections.
Immunohistochemical examination of PLA2G16 was performed with polyclonal PLA2G16 antibodies (No.10337, Cayman chemical) at a 5ug/ml dilution. Antigen retrieval was performed by high-voltage plerosis in Tris (0.01 mmol/L, pH = 6.0) and then EDTA buffer solution (1 mmol/L, pH = 9.0) for 150 s. After deparaffinization, rehydration, and heat-induced antigen retrieval, tissues were incubated with primary antibodies overnight at 4°C.After incubation for 30 minutes with the secondary antibody, the sections were developed in diaminobenzidine solution under microscopic observation and counterstained with hematoxylin. Negative control slides with the primary antibodies omitted were included for all assays.
IHC staining was evaluated by two independent pathologists who were blinded to the clinicopathological parameters and clinical outcomes of the patients. The staining was determined semi-quantitatively according to the intensity (0 = no staining, 1 = weak staining, 2 = moderate staining, 3 = strong staining) and the percentage of positive cells (0: none or <5%; 1: 5% to 20%; 2: 21% to 40%; 3: >40%). Scores of 0 to 2 were considered negative, and scores of 3 to 6 were considered positive. Cells were counted in at least three fields (at ×400 magnification) in the tumor areas.
Statistical Analysis
The differences in thePLA2G16 mRNA expression levels between primary non-metastatic osteosarcoma samples and the metastatic osteosarcoma samples were analyzed using Student’s t-test. For the IHC analysis, the correlation of PLA2G16 expression with the clinicopathologic data was analyzed using a Chi-square test. Patient survival curves were plotted according to the Kaplan—Meier method and a log-rank test. Multivariate Cox regression analysis was used to identify significant independent prognostic factors. The overall survival was defined as the time period from the date of diagnosis to that of death or the last follow-up. For the metastasis-free survival (MFS) analysis, the duration was defined as the time from diagnosis until the occurrence of metastasis. If these patients had metastatic disease at diagnosis, the event was considered time 0.A two-sided P value <0.05 was considered statistically significant. All statistical analyses were carried out using the SPSS version 18.0 statistical software (SPSS, Chicago, IL).
Results
Expression of PLA2G16 mRNA in human non-metastatic and metastatic primary osteosarcoma samples
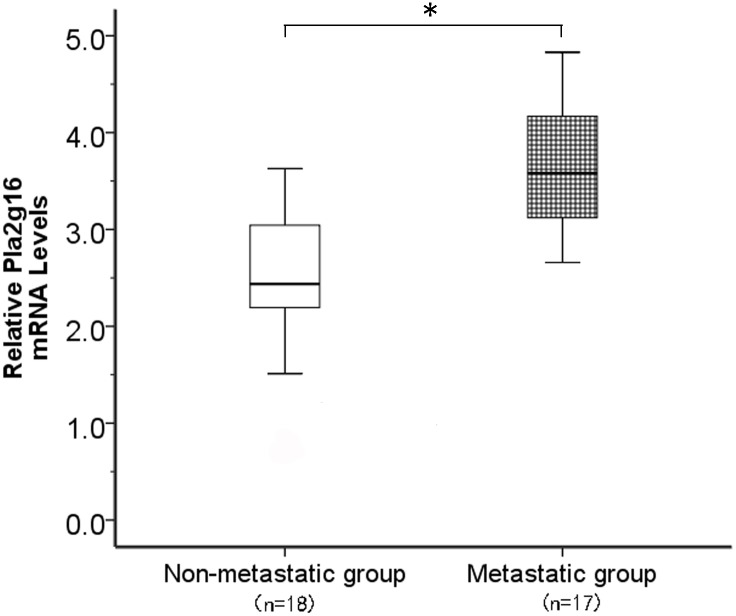
To examine the expression of PLA2G16 mRNA in fresh osteosarcoma patient samples, we harvested 18 primary tumor samples without metastasis and 17 primary tumor samples with metastasis. According to the qRT-PCR analysis, the expression levels of PLA2G16 mRNA were found to be significantly increased by 1.47-fold, on average, in the metastatic group compared with the non-metastatic group (Fig 1). The statistical analysis showed that the relative level of PLA2G16 mRNA expression in metastatic primary osteosarcoma tissues (mean ± SD: 3.65 ± 0.60) was clearly higher than that in non-metastatic tissues (mean ± SD: 2.49± 0.69; P < 0.05, Fig 1). These data suggested that the higher expression level of PLA2G16 in osteosarcoma was associated with metastasis.
Fig 1. PLA2G16 expression in osteosarcoma tumors with or without metastasis.
The PLA2G16 mRNA levels were determined by real-time quantitative PCR. *denote p values P<0.05.
Association of IHC staining for PLA2G16 with clinicopathologic variables in osteosarcoma patients
To examine the expression of PLA2G16 in human osteosarcoma patients at the protein level, we collected 119 osteosarcoma patient samples and made a TMA of the samples. Seventy-three male and 46 female patients were included in the study. Follow-up was available for all patients, with a median time of 94 months (range: 2 months to 171 months).Sixty patients (60/119, 50.4%) died during the follow-up period, primarily due to metastases (45/60, 75%). Fifty patients (50/119, 42%) developed metastases at a mean of 14.5 months (range 0–65 months). Of these patients, 41 had metastases in the lung, and four had metastases in bones (five patients had both lung and bone metastases).The median overall and metastasis-free survival times were 86 months (95% confidence interval [CI], 37.5–136.5 months) and 34.9 months (95% CI, 17.6–154.4 months), respectively. The clinical and histopathological details of the 119 cases are listed in Tables 1 and 2 and S1 Table.
Table 1. Relationship between PLA2G16 and Clinicopathologic Factors of Patients.
| Variables | PLA2G16 expression (N) | ||||
|---|---|---|---|---|---|
| Total (N = 119) | Positive | Negative | X2 | P-values | |
| Gender | |||||
| Male | 73(61.3%) | 41 | 32 | 0.181 | 0.670 |
| Female | 46(38.7%) | 24 | 22 | ||
| Age | |||||
| ≤ 20 years | 68(57.1%) | 36 | 32 | 0.181 | 0.671 |
| >20 years | 51(42.9%) | 29 | 22 | ||
| Tumor Location | |||||
| Femur | 56(47.1%) | 25 | 31 | 8.435 | 0.077 |
| Tibia | 24(20.2%) | 13 | 11 | ||
| Humerus | 13(10.9%) | 11 | 2 | ||
| Fibula | 11(9.2%) | 8 | 3 | ||
| Others | 15(12.6%) | 8 | 7 | ||
| Histological classification | |||||
| Osteoblastic | 79(66.4%) | 44 | 35 | 0.966 | 0.617 |
| Chondroblastic | 22(18.5%) | 13 | 9 | ||
| Others | 18(15.1%) | 8 | 10 | ||
| Metastasis | |||||
| Yes | 50(42.0%) | 38 | 12 | 15.900 | P<0.001 |
| No | 69(58.0%) | 27 | 42 | ||
| HIstological grade | |||||
| I | 34(28.6%) | 16 | 18 | 1.586 | 0.452 |
| II | 53(44.5%) | 29 | 24 | ||
| III | 32(26.9%) | 20 | 12 | ||
| Enneking staging | |||||
| I | 12(10.1%) | 4 | 8 | 4.812 | 0.186 |
| II A | 25(21.0%) | 16 | 9 | ||
| II B | 71(69.7%) | 37 | 34 | ||
| III | 11(9.2%) | 8 | 3 | ||
Abbreviation: PLA2G16, Group XVI phospholipase A2.
Table 2. Clinicopathologic patient characteristics and univariate survival analysis.
| Variable | Patients (n = 119) | 3-y OS Rate (%) | P value | 3-y MFS Rate (%) | P value |
|---|---|---|---|---|---|
| Male | 73 | 64.4% | 0.118 | 52.8% | 0.329 |
| Female | 46 | 82.6% | 62.3% | ||
| Age at diagnosis | |||||
| ≤ 20 years | 68 | 75.0% | 0.613 | 62.6% | 0.634 |
| > 20 years | 51 | 66.67% | 60.0% | ||
| Tumor location | |||||
| Femur | 56 | 75.0% | 0.608 | 63.2% | 0.693 |
| Tibia | 24 | 66.7% | 49.8% | ||
| Humerus | 13 | 61.5% | 44.9% | ||
| Fibula | 11 | 81.8% | 63.6% | ||
| Others | 15 | 66.7% | 53.3% | ||
| Histological classification | |||||
| Osteoblastic | 79 | 69.6% | 0.459 | 56.1% | 0.570 |
| Chondroblastic | 22 | 63.6% | 54.2% | ||
| Others | 18 | 88.9% | 66.2% | ||
| Lung metastasis | |||||
| Yes | 50 | 42.0% | <0.001 | 17.6 | <0.001 |
| No | 69 | 92.8% | 82.6 | ||
| Histological grade | |||||
| I | 34 | 88.2% | 0.005 | 81.7% | 0.005 |
| II | 53 | 66.0% | 57.9% | ||
| III | 32 | 52.9% | 40.0% | ||
| Enneking staging | |||||
| I | 12 | 100% | <0.001 | 100% | <0.001 |
| II A | 25 | 76.0% | 63.3% | ||
| II B | 71 | 68.9% | 59.9% | ||
| III | 11 | 18.2% | 0 | ||
| PLA2G16 | |||||
| Negative | 54 | 75.7% | 0.013 | 74.0% | 0.008 |
| Positive | 65 | 63.1% | 47.4% | ||
Abbreviation: OS, Overall survival; MFS, Metastasis-free survival; PLA2G16, Group XVI phospholipase A2.
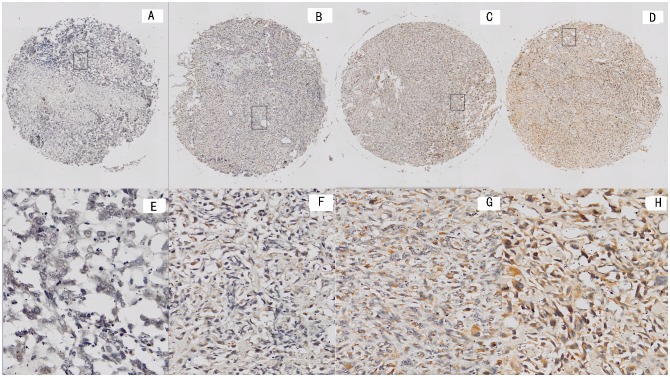
Positive PLA2G16 IHC staining was mainly present in the cytoplasm of the tumor cells (Fig 2A–2H).Of the 119 osteosarcoma patients, positive PLA2G16 expression was observed in 65 patients (54.6%).The PLA2G16 expression levels in the whole tumor sections were entirely consistent with the results from the TMA analysis. To elucidate the biologic significance, we investigated the association of patient clinicopathologic features and PLA2G16 expression levels. Although positive staining of PLA2G16 was present in both non-metastatic and metastatic tumors, the percentage of PLA2G16-positive staining in osteosarcoma with metastases (38/50, 76.0%) was significantly higher than in the samples without metastases (27/69, 39.1%; P<0.01, Table 1). Positive PLA2G16 expression was more frequent in osteosarcoma tissues with metastasis (P<0.01, X2 test). These data were consistent with the qRT-PCR analyses. However, no significant difference was observed between the expression of PLA2G16 and patient gender, age, tumor location, histological classification, histological grade and Enneking staging.
Fig 2. Representative immunohistochemical staining forPLA2G16 in tissue microarray.
Representative PLA2G16 staining samples at magnification of 40at levels of 0, 1, 2, and 3 (A), (B), (C) and (D).RepresentativePLA2G16 staining samples at magnification of 200 at levels of 0, 1, 2, and 3 (E), (F), (G) and (H).
Expression of PLA2G16 protein is associated with poor prognosis in patients with osteosarcomas
Further analyses of the patient samples indicated that the 3-year OS and MFS rates were 68.8% and 59.7% for the total study population, respectively. Importantly, the negative PLA2G16 group had significantly greater survival rates for 3-year OS and MFS than did the positive PLA2G16 group (75.7% vs. 63.1%, P<0.02, Fig 3A, and 74.0% vs. 47.4%, P<0.01, Fig 3B, respectively) by the Kaplan—Meier method and a log-rank test. Interestingly, histological grade and Enneking staging were still significant prognostic factors for both OS and MFS (P<0.01; Table 2), suggesting that PLA2G16 was an independent biomarker for OS and MFS in addition to histological grade and Enneking staging. We then performed multivariate Cox regression analysis, which revealed that PLA2G16expression, histological grade and Enneking staging were indeed independent prognostic factors for OS and MFS (P<0.05; Table 3).These data indicated that PLA2G16 may be a significant and novel biomarker for evaluating the prognoses of osteosarcoma patients.
Fig 3. Positive PLA2G16 immunohistochemical staining was associated with poor prognosis and survival.
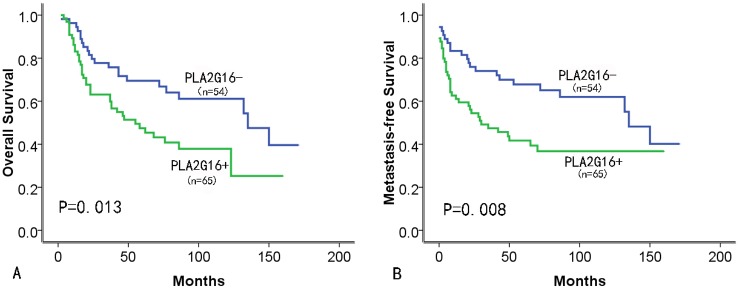
(A) Overall survival (OS)and (B) metastasis-free survival (MFS) of PLA2G16 positive or negative patients was determined by Kaplan-Meier analysis.
Table 3. Multivariate analysis of factors associated with overall survival and metastasis-free survival.
| Variable | HR (95% CI) | P value |
|---|---|---|
| OS | ||
| PLA2G16(+vs-) | 1.857 (1.088–3.168) | 0.023 |
| Histological grade | 1.711 (1.165–2.541) | 0.006 |
| Enneking staging | 2.596(1.602–4.208) | <0.001 |
| MFS | ||
| PLA2G16(+vs-) | 1.976 (1.158–3.369) | 0.012 |
| Histological grade | 1.612 (1.101–2.361) | 0.014 |
| Enneking staging | 3.526(1.920–6.475) | <0.001 |
Abbreviation: HR, Hazard ratio; CI, confidence interval; OS, overall survival; MFS, metastasis-free survival; PLA2G16, Group XVI phospholipase A2.
Discussion
The main cause of mortality in osteosarcoma patients is metastasis. Patients with lung or other bone metastases have a 5-year survival rate of less than 20% [2, 3].Despite the many existing treatment strategies, the survival rates for osteosarcoma with metastasis have remained unchanged over the last few decades [15]. Therefore, the study of biomarkers for osteosarcoma metastasis is important for improving the survival of patients. Here, we reported for the first time that PLA2G16 was expressed at a higher level in human osteosarcoma patients with metastasis compared with non-metastatic patients and that the positive PLA2G16 expression in osteosarcoma tissues was significantly correlated with metastatic features and with shorter OS and MFS times. Previously, PLA2G16 was reported to be a crucial gene for obesity development. Loss of Pla2g16 in mice inhibited obesity in Ob/Ob knockout mice [16]. The link between obesity and poor cancer prognosis has recently received much attention. The underlying mechanism may be due to increased lipids and lipid signaling, inflammatory responses, insulin resistance, and adipokines [17].Epidemiological studies have shown that obesity is not only associated with an increased risk of several types of cancer, including colon, endometrial, postmenopausal breast, kidney, esophageal, pancreatic, gallbladder, liver, and hematological malignancy [18, 19] but that it also leads to poorer treatment responses and increased cancer-related mortality [20, 21]. For instance, osteosarcoma patients who have a high BMI at diagnosis have a lower overall survival compared with patients who have a normal BMI [22], which is consistent with our hypothesized role of PLA2G16 in promoting tumor progression and poor prognosis by mediating lung metastases.
Moreover, PLA2G16 generates free fatty acids, usually arachidonic acid, and lysophosphatidic acid (LPA) from phosphatidylcholine [5]. Arachidonic acid can be converted into prostaglandin E2 (PGE2)and other prostaglandins by cyclooxygenase-2 (COX2) [23], which plays a role in regulating the migratory and invasive behavior of cells during the development and progression of cancer [24].Additionally, COX-2 expression in osteosarcoma lung metastases can be used as a prognostic factor [25].Furthermore, LPA has been demonstrated to induce cell proliferation, invasion, migration and survival [7]. With the function of both free fatty acids and LPA in cancer progression and metastasis, it is not surprising to consider PLA2G16 to be an important biomarker for osteosarcoma metastasis. The possible mechanisms of PLA2G16 in osteosarcoma metastasis may be due to arachidonic acid and LPA-induced downstream signaling pathways. Additionally, LPA is known to trigger Hippo [26]and mitogenic signaling [27]. Both of these pathways contribute to tumor progression and metastasis.
Recently, we have also demonstrated that increased expression levels of PLA2G16 mediated by mutant p53 contribute to osteosarcoma progression and metastasis [4].It will be very interesting to investigate whether p53 mutations in osteosarcoma correlate with the expression of PLA2G16. Finally, this study demonstrated thatPLA2G16 can serve as an independent and significant prognostic factor of OS and MFS. Thus, PLA2G16 may be a new therapeutic target for metastatic osteosarcoma patients in the future.
Supporting Information
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
This work was supported by the Program for National Clinical Research Center of Cancer. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Ritter J, Bielack SS. Osteosarcoma. Annals of oncology: official journal of the European Society for Medical Oncology / ESMO. 2010;21 Suppl 7:vii320–5. Epub 2010/10/15. 10.1093/annonc/mdq276 . [DOI] [PubMed] [Google Scholar]
- 2. Ferguson WS, Goorin AM. Current treatment of osteosarcoma. Cancer investigation. 2001;19(3):292–315. Epub 2001/05/08. . [DOI] [PubMed] [Google Scholar]
- 3. Ta HT, Dass CR, Choong PF, Dunstan DE. Osteosarcoma treatment: state of the art. Cancer metastasis reviews. 2009;28(1–2):247–63. Epub 2009/02/14. 10.1007/s10555-009-9186-7 . [DOI] [PubMed] [Google Scholar]
- 4. Xiong S, Tu H, Kollareddy M, Pant V, Li Q, Zhang Y, et al. Pla2g16 phospholipase mediates gain-of-function activities of mutant p53. Proceedings of the National Academy of Sciences of the United States of America. 2014;111(30):11145–50. Epub 2014/07/16. 10.1073/pnas.1404139111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Duncan RE, Sarkadi-Nagy E, Jaworski K, Ahmadian M, Sul HS. Identification and functional characterization of adipose-specific phospholipase A2 (AdPLA). The Journal of biological chemistry. 2008;283(37):25428–36. Epub 2008/07/11. 10.1074/jbc.M804146200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Husmann K, Sers C, Fietze E, Mincheva A, Lichter P, Schafer R. Transcriptional and translational downregulation of H-REV107, a class II tumour suppressor gene located on human chromosome 11q11-12. Oncogene. 1998;17(10):1305–12. Epub 1998/10/15. 10.1038/sj.onc.1202060 . [DOI] [PubMed] [Google Scholar]
- 7. Mills GB, Moolenaar WH. The emerging role of lysophosphatidic acid in cancer. Nature reviews Cancer. 2003;3(8):582–91. Epub 2003/08/02. 10.1038/nrc1143 . [DOI] [PubMed] [Google Scholar]
- 8. Shida D, Kitayama J, Yamaguchi H, Okaji Y, Tsuno NH, Watanabe T, et al. Lysophosphatidic acid (LPA) enhances the metastatic potential of human colon carcinoma DLD1 cells through LPA1. Cancer research. 2003;63(7):1706–11. Epub 2003/04/03. . [PubMed] [Google Scholar]
- 9. Tawadros T, Brown MD, Hart CA, Clarke NW. Ligand-independent activation of EphA2 by arachidonic acid induces metastasis-like behaviour in prostate cancer cells. British journal of cancer. 2012;107(10):1737–44. Epub 2012/10/06. 10.1038/bjc.2012.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nomura DK, Long JZ, Niessen S, Hoover HS, Ng SW, Cravatt BF. Monoacylglycerol lipase regulates a fatty acid network that promotes cancer pathogenesis. Cell. 2010;140(1):49–61. Epub 2010/01/19. 10.1016/j.cell.2009.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hajnal A, Klemenz R, Schafer R. Subtraction cloning of H-rev107, a gene specifically expressed in H-ras resistant fibroblasts. Oncogene. 1994;9(2):479–90. Epub 1994/02/01. . [PubMed] [Google Scholar]
- 12. Siegrist S, Feral C, Chami M, Solhonne B, Mattei MG, Rajpert-De Meyts E, et al. hH-Rev107, a class II tumor suppressor gene, is expressed by post-meiotic testicular germ cells and CIS cells but not by human testicular germ cell tumors. Oncogene. 2001;20(37):5155–63. Epub 2001/08/30. 10.1038/sj.onc.1204658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nazarenko I, Kristiansen G, Fonfara S, Guenther R, Gieseler C, Kemmner W, et al. H-REV107-1 stimulates growth in non-small cell lung carcinomas via the activation of mitogenic signaling. The American journal of pathology. 2006;169(4):1427–39. Epub 2006/09/28. 10.2353/ajpath.2006.051341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kim MS, Song WS, Cho WH, Lee SY, Jeon DG. Ezrin expression predicts survival in stage IIB osteosarcomas. Clinical orthopaedics and related research. 2007;459:229–36. Epub 2007/03/14. 10.1097/BLO.0b013e3180413dbf . [DOI] [PubMed] [Google Scholar]
- 15. Chan RJ, Cooper T, Kratz CP, Weiss B, Loh ML. Juvenile myelomonocytic leukemia: a report from the 2nd International JMML Symposium. Leukemia research. 2009;33(3):355–62. Epub 2008/10/29. 10.1016/j.leukres.2008.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jaworski K, Ahmadian M, Duncan RE, Sarkadi-Nagy E, Varady KA, Hellerstein MK, et al. AdPLA ablation increases lipolysis and prevents obesity induced by high-fat feeding or leptin deficiency. Nature medicine. 2009;15(2):159–68. Epub 2009/01/13. 10.1038/nm.1904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Louie SM, Roberts LS, Nomura DK. Mechanisms linking obesity and cancer. Biochimica et biophysica acta. 2013;1831(10):1499–508. Epub 2013/03/09. 10.1016/j.bbalip.2013.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lichtman MA. Obesity and the risk for a hematological malignancy: leukemia, lymphoma, or myeloma. The oncologist. 2010;15(10):1083–101. Epub 2010/10/12. 10.1634/theoncologist.2010-0206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. De Pergola G, Silvestris F. Obesity as a major risk factor for cancer. Journal of obesity. 2013;2013:291546 Epub 2013/09/28. 10.1155/2013/291546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kaidar-Person O, Bar-Sela G, Person B. The two major epidemics of the twenty-first century: obesity and cancer. Obesity surgery. 2011;21(11):1792–7. Epub 2011/08/16. 10.1007/s11695-011-0490-2 . [DOI] [PubMed] [Google Scholar]
- 21. Parekh N, Chandran U, Bandera EV. Obesity in cancer survival. Annual review of nutrition. 2012;32:311–42. Epub 2012/05/01. 10.1146/annurev-nutr-071811-150713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Altaf S, Enders F, Jeavons E, Krailo M, Barkauskas DA, Meyers P, et al. High-BMI at diagnosis is associated with inferior survival in patients with osteosarcoma: a report from the Children's Oncology Group. Pediatric blood & cancer. 2013;60(12):2042–6. Epub 2013/08/21. 10.1002/pbc.24580 . [DOI] [PubMed] [Google Scholar]
- 23. Cao Y, Prescott SM. Many actions of cyclooxygenase-2 in cellular dynamics and in cancer. Journal of cellular physiology. 2002;190(3):279–86. Epub 2002/02/22. 10.1002/jcp.10068 . [DOI] [PubMed] [Google Scholar]
- 24. Greenhough A, Smartt HJ, Moore AE, Roberts HR, Williams AC, Paraskeva C, et al. The COX-2/PGE2 pathway: key roles in the hallmarks of cancer and adaptation to the tumour microenvironment. Carcinogenesis. 2009;30(3):377–86. Epub 2009/01/13. 10.1093/carcin/bgp014 . [DOI] [PubMed] [Google Scholar]
- 25. Rodriguez NI, Hoots WK, Koshkina NV, Morales-Arias JA, Arndt CA, Inwards CY, et al. COX-2 expression correlates with survival in patients with osteosarcoma lung metastases. Journal of pediatric hematology/oncology. 2008;30(7):507–12. Epub 2008/09/18. 10.1097/MPH.0b013e31816e238c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yu FX, Zhao B, Panupinthu N, Jewell JL, Lian I, Wang LH, et al. Regulation of the Hippo-YAP pathway by G-protein-coupled receptor signaling. Cell. 2012;150(4):780–91. Epub 2012/08/07. 10.1016/j.cell.2012.06.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Du J, Sun C, Hu Z, Yang Y, Zhu Y, Zheng D, et al. Lysophosphatidic acid induces MDA-MB-231 breast cancer cells migration through activation of PI3K/PAK1/ERK signaling. PloS one. 2010;5(12):e15940 Epub 2011/01/07. 10.1371/journal.pone.0015940 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.