Abstract
Background:
Total elbow replacement (TER) is indicated in inflammatory arthritis, osteoarthritis and fractures that are not amenable to reconstruction. There is no series in literature, to the best of our knowledge, regarding the results of revision of the Souter-Strathclyde prosthesis (SSP) to the Coonrad-Morrey prosthesis (CMP). The aim of this study is to present the medium term results of primary CMP total elbow replacement and revision of the SSP to CMP.
Materials and Methods:
50 primary CMPs (Group I) and 11 revision CMPs (Group II) were included in the study. Demographic, operative, followup and radiological data were analysed. The indication for revision of the primary implant was peri-prosthetic fracture in six cases, aseptic loosening in four cases and instability in one case.
Results:
The mean age in Group I was 67.28 ± 12.45 years and in Group II was 57.09 ± 11.25 years. The mean period of followup was 8.08 ± 2.95 years and 7.46 ± 2.39. There was a significant improvement in range of motion and pain in both groups. The complications seen were nerve palsy, infection, fractures and heterotopic ossification. The 5-year survival rate in Group I was 94%. The results were good in 36 elbows, fair in 8 elbows and poor in 5 elbows. In Group II, the results were good in 8 elbows, fair in 2 elbows and poor in 1 elbow. The complications seen were nerve palsy, fractures and heterotopic ossification.
Discussion:
Primary CMP TER provides a functionally useful range of movement of 100° which is enough to perform most activities of daily living. It also produces a pain free and stable joint. Similar results are achieved after revision of the SSP to CMP. The unique toggle-hinge mechanism of articulation provides inherent stability and good survivorship.
Conclusion:
Semiconstrained prostheses like CMP provide good functional results and survivorship and are the implant of choice in both primary and revision total elbow replacements.
Keywords: Coonrad-Morrey prosthesis, revision elbow replacement, total elbow replacement
Keywords: Elbow, arthroplasty, joint prosthesis
INTRODUCTION
The kinematics of the elbow joint is affected by trauma, osteoarthritis and rheumatoid arthritis; thus, affecting the functionality of the individual. Reconstruction of the joint is performed to achieve anatomical and biomechanical stability and make the joint pain free and functionally effective.1 Total elbow arthroplasty (TEA) is offered as the last modality of management after exhaustion of all other conservative and minimally invasive surgical techniques. The results of semiconstrained implants like the Coonrad-Morrey prosthesis (CMP) have been reported to be better than that of unlinked implants.2,3 Revision TER is a challenging procedure due to the significant bone loss seen following retrieval of the primary implant. It is not known how the results of revision of the Souter-Strathclyde prosthesis (SSP) to CMP compare with primary CMP TER. The biomechanics of these unconstrained implants differ from semiconstrained implants like CMP. The aim of this study is to present the medium term results of primary total elbow arthroplasty with CMP and the results of revision of SSP to CMP.
MATERIALS AND METHODS
Fifty elbows (47 patients) in which primary CMP was done (Group I) and 11 elbows (10 patients), which had revision of SSP to CMP (Group II) were included in the study. The results were evaluated from clinical case records and radiographs. Demographic parameters such as age, gender, side operated upon and limb dominance were recorded [Table 1]. Surgical data included diagnosis, indication for surgery [Table 2], details of surgeries performed before TER, preoperative pain, range of motion, date of surgery, approach used, intraoperative complications, operative time, and postoperative complications. The followup data included condition of the surgical wound, infection, neurological deficit, range of movement, stability of the prosthesis in axial compression and varus/valgus stress, severity of pain, appearance of radiolucent zones at the implant-bone and bone cement interfaces, integrity of the prosthesis and shift of the implant tip.
Table 1.
Demographic parameters
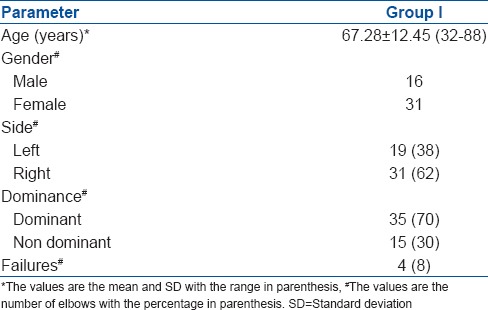
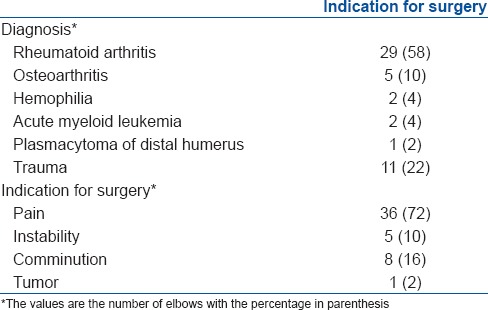
Table 2.
Diagnosis and indications for surgery in group I
The indication for revision of the primary implant was peri-prosthetic fracture in six cases, aseptic loosening in four cases and instability in one case. The mean period of followup was 7.46 ± 2.39 years (range: 5.2-11.25 years).
Statistical analysis
Analysis of the demographic, surgical and followup data collected was done using the statistical software SPSS® (17.0) (IBM, New York, United States). Descriptive analysis of the data such as age, gender, side operated, limb dominance, diagnosis, indication for surgery, operative time, presence of infection, nerve palsy, and complications was performed. Comparison between pre and postoperative ranges of motion in the flexion extension and pronation/supination planes was performed using the paired t-test. Pre and postoperative pain was compared using the Wilcoxon signed rank test. A multiple logistic regression model was used to analyze whether gender, dominance of hand, side operated or diagnosis were predictors of failure. Kaplan–Meier analysis of the cumulative probability of survival of the CMP was performed, taking revision or removal of one or both components of the prosthesis for any reason as end points. The outcome of the procedure was classified as good, fair and poor based on the presence of pain, range of movement and radiological changes.4
RESULTS
Group I
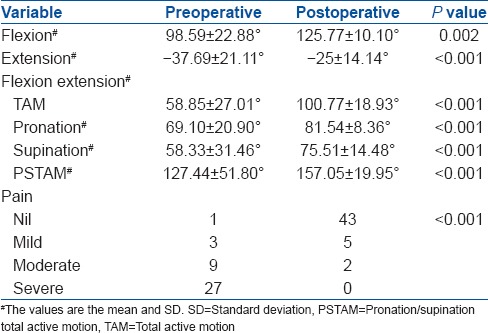
The mean age of the patients was 67.28 ± 12.45 years (range 32-88 years). The mean period of followup in Group I was 8.08 ± 2.95 years (range 5.08-10.25 years). The mean operative time was 119.08 ± 18.46 min (range 70-186 min). There was a significant improvement in the total range of movement in both flexion extension total active motion (FETAM) and pronation/supination total active motion (PSTAM) axes [Table 3]. There was no significant difference in the postoperative range of movement between the two genders (FETAM P = 0.992, PSTAM P = 0.338). Similarly, the side operated upon (FETAM P = 0.171, PSTAM P = 0.149) and dominance of hand (FETAM P = 0.209, PSTAM P = 0.180) made no significant difference. There was no significant difference between rheumatoid arthritis, osteoarthritis and trauma (FETAM P = 0.173, PSTAM P = 0.655). Thirty six cases had moderate or severe pain preoperatively. Postoperatively 43 of the 50 elbows were pain free. This difference was statistically significant (P < 0.001). Stability was achieved in all cases.
Table 3.
Range of movement and pain in group I
The most common complication seen was nerve palsy, with six cases (12%). There were five cases of ulnar nerve involvement (10%) and one case in which the radial nerve was involved (2%). Four cases of ulnar nerve palsy recovered completely within 8-12 weeks with conservative management. In one case, decompression and anterior transposition was performed 6 months after total elbow replacement surgery and the nerve recovered completely 3 months later. Radial nerve palsy recovered completely after 6 months with conservative management and splintage. The next common complication was infection, superficial in three cases (6%) and deep in two cases (4%). Heterotopic ossification occurred in one case (2%). There were two cases of intraoperative fracture (4%), which were managed conservatively and union was achieved within 12 weeks.
The implants were removed in 4 elbows (8%) [Table 4]. In one case, the prosthesis was removed after 7.4 years due to aseptic loosening of the humeral component, associated with grade four osteolysis. This was revised to a longer stemmed implant. Deep infection was the reason for removal in two cases. One of these patients developed septic arthritis of the contralateral shoulder 6 months after the primary procedure and was treated with arthrotomy, debridement, lavage, and antibiotics. The infecting organism was found to be Staphylococcus aureus. Subsequently, the TER prosthesis was infected, and the implant was removed followed by thorough debridement and lavage. Tissue samples were sent for microbiological analysis and antibiotics were prescribed based on the culture and sensitivity results. Revision surgery was undertaken after 6 months. The second case of deep infection developed methicillin-resistant S. aureus MRSA infection 6 months postoperatively, and the prosthesis was removed after multiple debridement surgeries. The 4th elbow was revised due to a peri-prosthetic humeral fracture.
Table 4.
Reason for failure
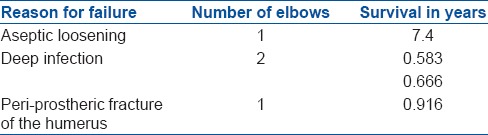
Multiple logistic regression analysis showed that age, gender, side operated upon, dominance of limb, and diagnosis were not significant predictors of prosthesis failure (P > 0.05). The Kaplan–Meier survivorship curve showed a 94% 5-year survival rate [Figure 1]. The results were good in 36 elbows, fair in 8 elbows and poor in 5 elbows.
Figure 1.
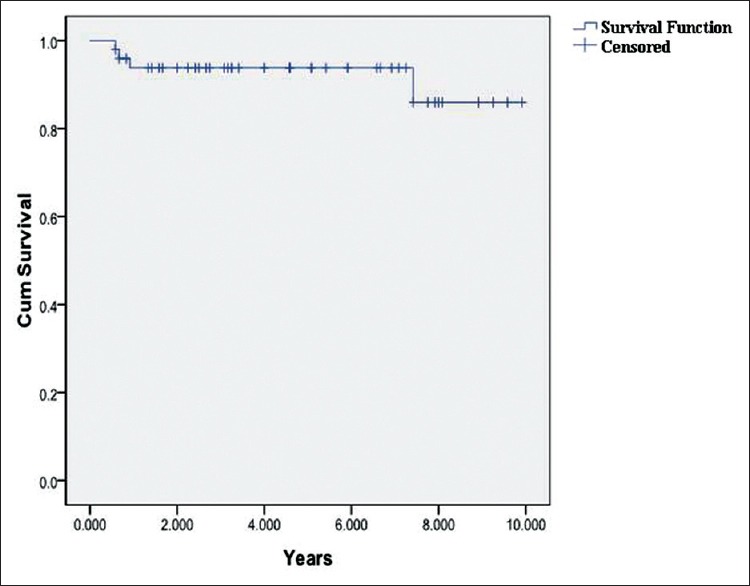
Kaplan–Meier curve of primary Coonrad-Morrey prosthesis
Group II
In Group II, the mean age at the time of revision surgery was 57.09 ± 11.25 years (range 39-79 years). The primary diagnosis for which SSP TER was done was rheumatoid arthritis in nine cases (81.8%), posttraumatic osteoarthritis in one case and grossly comminuted distal humerus fracture in one case. There were five males and five females. The left: Right ratio was 3:8. The dominant limb was operated upon in eight cases. The final postoperative range of flexion was 129° ± 7.35°, extension −18.64° ± 8.97°, FETAM 110.45° ± 14.57°, pronation 87.27° ± 4.67°, supination 83.64° ± 10.26° and PSTAM 170.91° ± 14.46°. Preoperatively, the pain was mild in 5 elbows, moderate in three and severe in 3 elbows. Postoperatively, there was no pain in 9 elbows and mild pain in 2 elbows. The Wilcoxon signed rank test showed a significant improvement in pain postoperatively, in comparison with preoperative values (P < 0.001). Superficial infection occurred in one case and completely resolved with antibiotics. Olecranon fracture occurred in one case [Figure 2]. Ulnar component protrusion [Figure 3] through the cortex occurred in one case and it was managed by using a burr to smoothen the protruding part to the level of the cortex. Nerve palsy was seen in two cases (18.2%). Transient ulnar nerve palsy, which recovered with conservative management within 11 weeks, was noted in one case. Radial nerve palsy was encountered in the other case. Decompression was done after 5 months, following which the nerve recovered completely after 1-year. Intraoperatively, the nerve was found to be compressed by bone cement. A peri-prosthetic fracture and failure of the ulnar component occurred 9 months after the index revision surgery in the same case [Figure 4]. The implant was removed. The patient refused a second revision surgery and opted for arthrodesis of the elbow with a fibular graft [Figure 5]. Isolated polyethylene bushing revision for wear and instability was performed in one case, 7 years after the index revision surgery. The results were good in 8 elbows, fair in 2 elbows and poor in 1 elbow.
Figure 2.

Plain x-ray elbow joint lateral view showing olecranon fracture in revision Coonrad-Morrey prosthesis
Figure 3.

Plain x-ray elbow joint lateral view showing ulnar component protrusion
Figure 4.

X-ray of forearm with elbow joint anteroposterior view showing failure of revision Coonrad-Morrey prosthesis
Figure 5.

X-ray elbow joint anteroposterior and lateral views showing elbow arthrodesis
DISCUSSION
The most important finding in our study was that no specific factor had an impact on loosening and failure of the prosthesis, probably because in the context of the relatively small size of our series, the individual effect of most factors was obscured; thus, denying any statistical correlation. Loosening can be caused by a variety of factors including biomechanical instability, deep infection and peri-prosthetic fracture. The elbow is affected in approximately half of the patients suffering from rheumatoid arthritis.5,6 In our series, it was the underlying diagnosis in the majority of patients. The rate of deep infection in literature ranges from 0% to 9%7 and the incidence of intraoperative condylar fracture from 0% to 4%.7,8,9 The peculiar bone cut required during the preparation of the humerus and the sub-optimal quality of bone in inflammatory arthritis are probably responsible for this complication. Deep infection and fractures are common in elderly patients with rheumatoid arthritis.10 This is probably because such patients have immune system dysfunction and a compromised soft tissue cover. Nerve palsy is the most common complication in TER. The incidence of ulnar nerve palsy in literature ranges from 0% to 26%.7,9,10,11,12 A standard triceps aponeurosis reflecting technique was used in all our cases. Meticulous dissection and isolation of the ulnar nerve is required to minimize the occurrence of ulnar nerve palsy. Literature suggests that despite these precautions nerve palsies can occur in stiff elbows that regain a considerable range of motion after surgery.13 Anterior transposition of the nerve may be considered in such elbows based on the intraoperative increase in range of movement achieved.
A minimum of 100° of range of movement is required in the flexion extension axis (range 30-130° of flexion) and the pronation/supination axis (pronation 50° and supination 50°) to perform most activities of daily living.14 This functionally useful range of movement was achieved in all cases in our series. This puts forward the view that the biomechanics and functional result of the CMP is conducive to the performance of most activities of daily living. This is also the case in other series in literature.7,8,12
Another important finding in our study was that the revision of SSP to CMP produced a functionally useful range of movement of 100° and provided significant pain relief in a majority of cases. There is a significant amount of bone loss associated with revision surgery. Significant release of soft tissue is usually required during revision, necessitating that stability be achieved through the implant. Long stemmed semiconstrained implants like the CMP help bypass the defect and provide stability to the construct through the toggle hinge mechanism of articulation. As in primary TER, the most common complication in revision TER is also nerve palsy. Neuropraxia accounts for the palsy in most series in literature. In addition, we believe that the cement can extrude through the void created by bone loss, seen after removal of the SSP and cause nerve palsy.
The occurrence of ulnar component protrusion and olecranon fracture emphasizes the difficulty in insertion of implants during revision surgery and the poor quality of the bone encountered along with suboptimal soft tissues and contractures.
The failure rate of primary CMP in literature has ranged from 0% to 31.7%.7,9,11 The 5-year survivorship of primary TER ranges from 68% to 100% in the literature.4,8,15 The survivorship of our primary CMP series was at the higher end of this spectrum at 5-year. The survivorship of SSP revised to CMP was also as good as primary implants. The medium term functional results are good in the majority of the patients. Statistical comparison between the two groups in our series would not be appropriate, considering the difference in indication and diagnosis. However, a pain free elbow with a functionally useful arc of motion of 100° was achieved in majority of cases in both groups, probably suggesting that the results of revision of unlinked implants to CMP were comparable to primary CMP arthroplasty in terms of the final functional outcome. The toggle hinge mechanism of the CMP gives flexible stability, reproducing the movements of the native elbow, thus probably contributing to long term survivorship. There have been considerable changes in the design and articulation of the prosthesis to achieve this flexible stability, such that the actual movements produced during physiological loading were within the parameters of the laxity inbuilt in the design. The original Coonrad prosthesis (Type I), introduced in 1973, had high molecular weight polyethylene bushings and a varus-valgus laxity of 2-3°. It was associated with an unacceptable rate of aseptic loosening in rheumatoid arthritis.4 Improved understanding of the biomechanics of the normal elbow, subsequently, highlighted the importance of proper alignment, laxity between the prosthetic components and dynamic soft tissue support. These concepts were used in the design of the Coonrad prosthesis (Type II) in 1978 with the introduction of 7° of varus-valgus laxity. The design was again modified at the Mayo clinic in 1981, with the introduction of an anterior flange in the distal end of the humeral component and surface coating with a titanium plasma spray to improve fixation. A bone graft could be placed between the flange and the anterior cortex of the humerus. This change in design prevented posterosuperior migration and improved rotational stability by negating the posteriorly directed vector forces acting on the elbow, thus improving stability and reducing the incidence of aseptic loosening.1 This was called the CMP Type III. In 1991, titanium plasma spray was replaced with sintered titanium beads.12 A further modification was the introduction of a pin-within-pin articulation instead of the original C-ring mechanism, between the humeral and ulnar components. The present implant allows for 7-10° of varus-valgus and 7-10° of rotational laxity, giving flexibility and stability.9
To conclude the CMP provides significant pain relief, stability and a functionally useful range of movement in elbows affected by inflammatory arthritis, trauma and osteoarthritis. The functional results of revision of SSP to CMP mirror that of primary CMP. The prosthesis accomplishes all the aims of elbow reconstruction with good functional outcome and survivorship and significantly reduces the disability of the patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Corradi M, Frattini M, Panno B, Tocco S, Pogliacomi F. Linked semi-constrained total elbow prosthesis in chronic arthritis: Results of 18 cases. Musculoskelet Surg. 2010;94(Suppl 1):S11–23. doi: 10.1007/s12306-010-0070-y. [DOI] [PubMed] [Google Scholar]
- 2.Güttler K, Landor I, Vavrík P, Popelka S, Sosna A, Krásenský J. Total elbow replacement in patients with rheumatoid arthritis. Acta Chir Orthop Traumatol Cech. 2011;78:423–30. [PubMed] [Google Scholar]
- 3.Little CP, Graham AJ, Karatzas G, Woods DA, Carr AJ. Outcomes of total elbow arthroplasty for rheumatoid arthritis: Comparative study of three implants. J Bone Joint Surg Am. 2005;87:2439–48. doi: 10.2106/JBJS.D.02927. [DOI] [PubMed] [Google Scholar]
- 4.Morrey BF, Bryan RS, Dobyns JH, Linscheid RL. Total elbow arthroplasty. A five-year experience at the Mayo Clinic. J Bone Joint Surg Am. 1981;63:1050–63. [PubMed] [Google Scholar]
- 5.Symmons D, Turner G, Webb R, Asten P, Barrett E, Lunt M, et al. The prevalence of rheumatoid arthritis in the United Kingdom: New estimates for a new century. Rheumatology (Oxford) 2002;41:793–800. doi: 10.1093/rheumatology/41.7.793. [DOI] [PubMed] [Google Scholar]
- 6.Hargreaves D, Emery R. Total elbow replacement in the treatment of rheumatoid disease. Clin Orthop Relat Res. 1999;366:61–71. doi: 10.1097/00003086-199909000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Schneeberger AG, Meyer DC, Yian EH. Coonrad-Morrey total elbow replacement for primary and revision surgery: A 2- to 7.5-year followup study. J Shoulder Elbow Surg. 2007;16:S47–54. doi: 10.1016/j.jse.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 8.Gill DR, Morrey BF. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. A ten to fifteen-year followup study. J Bone Joint Surg Am. 1998;80:1327–35. doi: 10.2106/00004623-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Shi LL, Zurakowski D, Jones DG, Koris MJ, Thornhill TS. Semiconstrained primary and revision total elbow arthroplasty with use of the Coonrad-Morrey prosthesis. J Bone Joint Surg Am. 2007;89:1467–75. doi: 10.2106/JBJS.F.00715. [DOI] [PubMed] [Google Scholar]
- 10.Hildebrand KA, Patterson SD, Regan WD, MacDermid JC, King GJ. Functional outcome of semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 2000;82-A:1379–86. doi: 10.2106/00004623-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Aldridge JM, 3rd, Lightdale NR, Mallon WJ, Coonrad RW. Total elbow arthroplasty with the Coonrad/Coonrad-Morrey prosthesis. A 10- to 31-year survival analysis. J Bone Joint Surg Br. 2006;88:509–14. doi: 10.1302/0301-620X.88B4.17095. [DOI] [PubMed] [Google Scholar]
- 12.Morrey BF, Adams RA, Bryan RS. Total replacement for posttraumatic arthritis of the elbow. J Bone Joint Surg Br. 1991;73:607–12. doi: 10.1302/0301-620X.73B4.2071644. [DOI] [PubMed] [Google Scholar]
- 13.Antuña SA, Morrey BF, Adams RA, O’Driscoll SW. Ulnohumeral arthroplasty for primary degenerative arthritis of the elbow: Long term outcome and complications. J Bone Joint Surg Am. 2002;84-A:2168–73. doi: 10.2106/00004623-200212000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63:872–7. [PubMed] [Google Scholar]
- 15.Prasad N, Dent C. Outcome of total elbow replacement for rheumatoid arthritis: Single surgeon's series with Souter-Strathclyde and Coonrad-Morrey prosthesis. J Shoulder Elbow Surg. 2010;19:376–83. doi: 10.1016/j.jse.2009.09.016. [DOI] [PubMed] [Google Scholar]


