Abstract
AIM: To compare irritable bowel syndrome (IBS) patients with apparently healthy persons and to evaluate body awareness therapy, which is a physiotherapeutic remedy focusing on normalising tensions in the body, for the treatment of IBS with the hypothesis that altered body tension is associated with the syndrome.
METHODS: Twenty-one IBS patients received body awareness therapy two hours weekly for 24 wk. At baseline as well as after 12 and 24 wk, they underwent examinations including resource oriented body examination in combination with body awareness scale evaluation and filled in gastrointestinal and psychological symptom questionnaires. Saliva cortisol was analysed. A group of 21 apparently healthy persons underwent the same examinations once.
RESULTS: Compared to the apparently healthy group, IBS patients scored higher at baseline for gastrointestinal and psychological symptoms. They showed more often alterations in normal body tension patterns, as well as deviating cortisol slopes in saliva. After 24 wk of body awareness therapy, their gastrointestinal and psychological symptoms were reduced overall. Somatic symptoms decreased in parallel with depressive symptoms. Whole body pain score decreased, coping ability as well as biochemical stress markers improved.
CONCLUSION: IBS patients scored higher for gastrointestinal and psychological symptoms, and presented with altered biochemical stress markers. Their body tension deviated compared to healthy controls. Furthermore, body awareness therapy gave relief of both somatic complaints, psychological symptoms and normalised body tension. These findings indicate that distorted tension constitutes an important part of the symptoms in IBS.
Keywords: Irritable bowel syndrome, Pain, Cortisol, Physiotherapy, Body awareness therapy, Psychosomatics, Gastrointestinal tract, Stress
INTRODUCTION
Irritable bowel syndrome (IBS) is considered the most common of all gastrointestinal disorders with a prevalence of 5%-25%[1-4]. Bowel habits are altered in association with abdominal pain and discomfort. The diagnosis of IBS is made in the absence of alarming symptoms, such as fever, bleeding or weight loss based on the clinical criteria[5,6]. In addition, associated symptoms, like headache and dysuria are often evident in IBS patients. These patients have often other disorders such as fibromyalgia, panic disorder, anxiety states and depressions[7-9].
The aetiology is still insufficiently understood, but altered gastrointestinal motility and visceral hyperalgesia have been advocated as mechanisms underlying IBS[10-12]. Mucosal inflammation and disturbances in the brain-gut axis are other tentative explanations for the causal pathophysiology[13,14]. These patients are vulnerable to stress and there is also a connection to traumatic life events. Psychological mechanisms may evoke the syndrome[15]. IBS patients are also shown to have a lower sense of coherence compared to controls, weakening their ability to cope with the disorder[16,17].
Overall, the therapeutic aim is both a reduction in the severity and frequency of symptoms and a general improvement in quality of life. Therapy has until recently focused on symptomatic relief of pain, diarrhoea and constipation in particular[18]. However, many IBS patients have not any long lasting relief of symptoms after drug treatment. Therefore, alternative therapies, such as psychotherapy and hypnosis, have been applied[19-22].
IBS has been classified as a functional/psychosomatic disorder associated with altered body image and tension[23,24]. A common defence mechanism may lead to blockage and further development of different organ manifestations. A physiotherapeutic approach to adjustment of pathological tension in the body is the body awareness therapy (BAT). This psychosomatic physiotherapeutic treatment is a synthesis of clinical experiences mostly based on the works of W. Reich and eastern body tradition. It's objective is to take care of, and to improve the patient’s ability to become aware of his or her own bodily status and to recapture a normal balance in the body[25-29]. The degree of body tension before and after treatment can be assessed by resource examination methods such as resource oriented body examination[30,31] in combination with body awareness scale evaluation[32-34].
It was reported that 12 wk of treatment with BAT gives symptomatic relief of both gastrointestinal and psychological symptoms, mostly to the constipated patients[35]. However, this was not seen in IBS control patients, having ordinary medical intervention, but not receiving BAT.
The aim of the present study was to compare IBS patients with apparently healthy persons and to determine the effect of body awareness therapy for 24 wk in patients with IBS, concerning gastrointestinal and psychological symptoms, body function and tension, as well as cortisol levels in saliva, with the hypothesis that IBS is associated with an altered body tension.
MATERIALS AND METHODS
Study population
Patients with IBS diagnosed by their clinicians were referred to participate in the study. Thus, the patients were randomly selected, with a slight bias towards subjects not responding to basic therapy. Patients with an acute psychiatric disease or patients not understanding the Swedish language were excluded from the study. The study population was obtained from three different groups undergoing body awareness therapy. No subject participated in more than one course. A total of 30 patients were invited to participate in the study. Nine subjects were excluded since they did not complete the treatment. Reasons for their drop out were traumatic events in their family (4 persons), stressful working situations (2 persons) or difficulties with the daily life activities (3 persons).
The IBS patients consisted of 18 women and 3 men, 21-67 years of age with a BMI of 23.1 ± 3.8. Sixteen patients had suffered from their gastrointestinal symptoms for more than 5 years and the other five patients for less than 5 years.
A healthy control group (AHC) consisted of 18 women and 3 men, 21-61 years of age. They had a BMI of 22.3 ± 2.2 and were free of gastrointestinal symptoms and with no ongoing medication.
Study design
IBS patients received body awareness therapy for 24 wk. At baseline and after 12 and 24 wk of body awareness therapy, the patients underwent complete physiotherapeutic examinations in accordance to resource oriented body examination (ROBE) and body awareness scale (BAS). They also filled in the questionnaires of gastrointestinal symptoms (GIS), SCL90, SOC and pain drawing. Saliva samples were collected at 0, 12 and 24 wk. The patients also completed the GIS, SCL90 and pain-drawing during the 6-mo follow-up. The AHC group answered the same questionnaires once, underwent complete physiotherapeutic examinations, as well as sampling of saliva. The study was approved by the Ethics Committee of the University of Göteborg. All subjects gave their written consent before acceptance of inclusion in the study.
Physiotherapeutic procedures
The IBS patients in groups of 7-10 received body awareness therapy, two hours a week for 24 wk. Two physiotherapists were present during the sessions. Questions raised during sessions were taken care of. Body awareness therapy represents a body-oriented physiotherapeutic approach focusing on both the physical and psychological aspects of body dysfunctions[25-29]. Assisted by a physiotherapist, the patients were working with the basic functions of movements related to posture, co-ordination, free breathing and awareness. The physiotherapist encouraged the patients to move in more optimal ways by using both body gestures and words for guiding. Turning the attention both to the patient’s own performance and to what is experienced during the exercises is central elements of the therapy and stimulates mental presence and awareness.
Examinations
The resource oriented body examination (ROBE) includes examination of different items related to posture, respiration, body function and muscle palpation in a standardised manner[30]. All items were assessed on three to five category scales. Body awareness scale (BAS-H)[33] test was performed during video recording. The test was based on observations made by a physiotherapist of defined items on basic movements (Basobs) as well as standardized questions in order to measure the patients’ own opinion concerning their body awareness (Basself). The scale ranged 0-6, where zero represents a normal value and 6 the most pathological one.
Questionnaires
A modified gastrointestinal symptom questionnaire (GIS) was used[36]. This survey elevates 35 general gastrointestinal symptoms. A total score and subscales of specified symptoms were used. The test uses a seven-graded scale (0-6). A higher score means increased gastrointestinal complaints.
The distribution and quality of pain were visualised on a pain-map figuring the human body with a front and back side. When results were calculated, the body was divided into sections[37]. Points were given for every section where pain was marked irrespective of quality. The points were summed up to a score.
The symptom checking list questionnaire (SCL90) is a self report rating scale using questions related to everyday life with an emphasis on psychological symptoms[38]. The questionnaire includes 90 questions with answers scoring on a five-graded scale (0-4). The higher the score is, the more the symptoms are. A total score and subscales of specific symptoms were used.
The sense of coherence scale (SOC) is an overall assessment of the subject’s ability to cope with stressors and often used by physiotherapists working with patients[39]. This is a 29-item instrument where the answers score in a seven-graded scale (0-6) and allow subdivision in order to measure perceived comprehensibility, manage-ability, meaningfulness and quality of life. A high score means a stronger SOC.
Biochemical analysis
For saliva samples, cotton swabs (Salivette® tubes, Sarstedt, Landskrona, Sweden added with Stabilyte® solution, Bio-pool AB, Sweden) were chewed during daytime at 8.00 (in two consecutive days), 11.45, 17 and 20 h. After chewing the swabs, they were put back in the test tubes and stored in a freezer for later analysis of saliva cortisol (Spectria kit™, Orion Diagnostica, Sweden). Saliva were centrifuged at 3000 × g for 15 min and stored at -70°C before analysis.
Statistical analysis
This study consisted of nominal data (ROBE) and ordinal data (ROBE; BAS and questionnaires) and quantitative data (biochemical parameters). Median, interquartile range (IQR), mean ± SD and percentage were used for presentation of data. Although median and IQR were optimal for ordinal data, means were presented as well for better visualisation. Chi-square test was used for nominal data. Mann Whitney U/Wilcoxon signed rank test or Kruskal Wallis test was used for ordinal, quantitative and categorised data[40]. Boxplots used in the figures show the 10th and the 90th percentile outside the box and the 25th, 50th (median) and 75th percentile of the variable in the box.
RESULTS
In the three groups undergoing body awareness therapy, the overall attendance was 72% (range 58%-96%). The presence in each group was 67%, 77% and 71%, respectively. The reasons for the absence were illness, birthdays, other meetings, etc.
Resource oriented body examination (ROBE)
ROBE showed deviations from normality regarding posture, body function and muscle palpation (tendency) among IBS patients compared to healthy controls before the therapy (Table 1). Concerning respiration, 80% of the patients were marred by wrinkles and 25% with furrows, indicating that the IBS patients had a restricted respiration pattern compared to the control group for which the corresponding figures were 41% and 4% respectively. Eighteen of the 21 IBS patients showed a decreased thoracic kyphosis, two patients showed neutral and one increased kyphosis. The corresponding figures for the AHC group were as follows: 14 subjects presented with neutral and seven with decreased thoracic kyphosis. During treatment, the patients improved their body-function and showed tendencies to normalise muscle palpation grade as well as posture (Table 1).
Table 1.
Resource oriented body examination (ROBE)
| Type | ITEM | Category |
IBS patients |
AHC | ||
| 0 wk | 12 wk | 24 wk | ||||
| % | % | % | % | |||
| (a) | ||||||
| Posture | Joint | Flexed | 35 | 30 | 28 | 22 |
| Neutral | 31 | 40b | 48b | 56b | ||
| Extended | 34 | 30 | 24 | 22 | ||
| Muscle | Grade | High | 42 | 37 | 25 | 25 |
| Palpation | Increased | 35 | 26 | 41 | 27 | |
| Neutral | 19 | 30b | 29b | 45 | ||
| Decreased | 4 | 7 | 5 | 3 | ||
| (b) | M Md (IQR) | M Md (IQR) | M Md (IQR) | M Md (IQR) | ||
| Body | ||||||
| Function | 2.2 | 2.5(1) | 2.5 3 (1)b | 2.6 3 (1)b | 2.7 3 (0.5)b | |
Resource oriented body examination for posture, body function and muscle palpation presented in (a) as %, in (b) as M Md(IQR) for IBS patients at 0, 12 and 24 wk of treatment and for AHC group. For body-function, the lower the score is, the more the symptoms are. M denotes mean, Md: median; IQR: inter quartile range; AHC: apparently healthy controls. bP < 0.001 vs IBS patients at 0 wk.
Body awareness scale (BAS)
The IBS patients as observed by the physiotherapist (BASobs) at baseline, totally and in the different subclasses scored more of dysfunction in body movements in comparison to the healthy control group. However, after 12 wk of treatment, especially after 24 wk of treatment, the body pattern of the IBS patients improved significantly (Table 2).
Table 2.
Body awareness scale (BAS-H)
| Group |
0 wk |
12 wk |
24 wk |
|||
| Category | M | Md (IQR) | M | Md (IQR) | M | Md (IQR) |
| BASobs | ||||||
| AHC totally | 1.5 | 2 (2)d | ||||
| Grounding | 1.5 | 2 (2)d | ||||
| Mid-line | 2.1 | 2 (2)d | ||||
| Centring | 2.1 | 2 (1)d | ||||
| Flow | 1.5 | 1 (2)d | ||||
| Respiration | 1.4 | 2 (2)d | ||||
| Boundaries | 0.5 | 0(0) | ||||
| IBS totally | 2.3 | 2 (4) | 1.8 | 2 (3)d | 1.7 | 2 (3)d |
| Grounding | 2.3 | 2 (2) | 2.2 | 2 (2) | 2.0 | 2 (1)a |
| Mid-line | 2.9 | 3 (2) | 2.4 | 2 (3)b | 2.1 | 2 (2)d |
| Centring | 2.9 | 3 (2) | 2.4 | 2 (1)d | 2.0 | 2 (2)d |
| Flow | 2.4 | 2 (4) | 2.0 | 2 (3)a | 1.8 | 2 (3)d |
| Respiration | 3.6 | 4 (1) | 2.7 | 3 (2)d | 2.4 | 2 (1)d |
| Boundaries | 0.9 | 0 (2) | 0.7 | 0 (0)a | 0.6 | 0 (0)b |
| BASself | ||||||
| AHC totally | 1.6 | 2 (2)d | ||||
| Grounding | 0.8 | 0 (2)b | ||||
| Mid-line | 1.6 | 2 (2)d | ||||
| Centring | 1.3 | 0 (2) | ||||
| Flow | 2.1 | 2 (4)d | ||||
| Respiration | 1.0 | 0 (2)d | ||||
| Boundaries | 1.7 | 2 (3)b | ||||
| IBS totally | 2.4 | 2 (4) | 2.1 | 2 (4)d | 1.7 | 2 (3)d |
| Grounding | 1.7 | 2 (3) | 1.5 | 2 (2) | 0.9 | 0 (2)d |
| Mid-line | 2.8 | 3 (4) | 2.4 | 2 (4) | 2.0 | 2 (4)b |
| Centring | 1.5 | 2 (2) | 1.1 | 0 (4) | 0.7 | 0 (2)b |
| Flow | 3.4 | 4 (4) | 3.4 | 4 (4) | 2.8 | 3 (3)a |
| Respiration | 2.7 | 2 (4) | 2.0 | 2 (4)a | 1.6 | 2 (2)b |
| Boundaries | 2.3 | 2 (4) | 2.0 | 2 (3)b | 1.7 | 2 (2)d |
Results from the test BASobs and BASself for 21 apparently healthy controls and 21 IBS patients at 0, 12 and 24 wk. The result is shown totally and as items categorized. The higher the score is, the more the symptoms are. M denotes mean, Md: median; IQR: inter quartile range; AHC: apparently healthy controls.
P < 0.05,
P < 0.01,
P < 0.001 vs IBS patients at 0 wk.
On self-estimation (BASself) before treatment, the IBS patients scored higher in terms of body disturbances than the healthy control group. After 12 wk of treatment, they improved the score overall. This was evident especially for the ability of the subclasses to set up boundaries and way of feeling respiration. After 24 wk of treatment, all the subclasses were significantly improved (Table 2).
Gastrointestinal symptoms (GIS)
The IBS patients demonstrated higher gastrointestinal symptom scores before treatment compared to the AHC group (Table 3). After body awareness therapy, lower scores for IBS patients were seen. The symptoms of flatulence and constipation both diminished after 12 wk of body awareness therapy. After 24 wk of body awareness therapy, also a relief in pain and diarrhoea could be seen. This improvement in GI scores persisted during the 6-mo follow-up (Table 3).
Table 3.
Gastrointestinal symptom score for 21 apparently healthy controls and for 21 IBS patients at 0, 12 and 24 wk of treatment and 6 mo after end of treatment
| Category |
Before treatment |
After 12 wk |
After 24 wk |
6 mo after end of treatment |
||||
| M | Md (IQR) | M | Md (IQR) | M | Md (IQR) | M | Md (IQR) | |
| AHC group | ||||||||
| Totally | 0.4 | 0 (1)d | ||||||
| Pain | 0.4 | 0 (1)d | ||||||
| Flatulence | 0.4 | 0 (1)d | ||||||
| Nausea | 0.2 | 0 (1) | ||||||
| Constipation | 0.6 | 0 (1)b | ||||||
| Diarrhoea | 0.3 | 0 (1)d | ||||||
| Motility | 0.5 | 0 (1)d | ||||||
| Other | 0.3 | 1 (0)d | ||||||
| IBS patients | ||||||||
| Totally | 1.8 | 1 (3) | 1.6 | 1 (3)d | 1.3 | 1 (2)d | 1.4 | 1 (2)d |
| Pain | 1.9 | 2 (2) | 1.9 | 2 (3) | 1.5 | 2 (2)d | 1.4 | 1 (2)d |
| Flatulence | 2.5 | 2 (3) | 2.2 | 2 (2)b | 1.8 | 2 (2)d | 2.0 | 2 (2)b |
| Nausea | 1.4 | 1 (2) | 1.0 | 0 (2)a | 0.9 | 0 (2)a | 0.8 | 0 (1)a |
| Constipation | 1.9 | 2 (3) | 1.5 | 1 (2)a | 1.1 | 1 (2)b | 1.4 | 1 (2)a |
| Diarrhoea | 1.9 | 1 (3) | 1.6 | 2 (1) | 1.2 | 1 (2)d | 1.2 | 1 (2)b |
| Motility | 2.6 | 2 (3) | 2.2 | 2 (2)a | 1.9 | 2 (1)a | 2.1 | 2 (2) |
| Others | 1.2 | 1 (1) | 1.2 | 1 (1) | 1.1 | 1 (1)a | 1.1 | 0 (1)a |
The result is shown totally and categorized. The higher score the more symptoms. M denotes mean, MD: median; IQR: inter quartile range; AHC: apparently healthy controls.
P < 0.05,
P < 0.01,
P < 0.001 vs IBS patients at 0 wk.
Pain
At baseline, pain-drawing gave higher scores for IBS patients than for healthy controls. The pain gradually decreased and was significantly less after 24 wk of body awareness therapy. This reduction in pain remained during the 6-mo follow-up (Table 4). Pain of different qualities was located in the abdomen but also in other parts of the body such as arm, shoulder, head, back, breast, leg and foot (Table 4).
Table 4.
Score of pain presented as M, Md (IQR) experienced as drawings for apparently healthy controls and IBS patients at 0, 12, 24 wk of treatment and 6 mo after end of treatment and different qualities of pain from the pain drawing. The qualities are as marked in descending order
| Pain | Baseline | 12 wk | 24 wk | 6 mo after | ||||
| M | Md (IQR) | M | Md (IQR) | M | Md (IQR) | M | Md (IQR) | |
| AHC group | 4.2 | 3 (4)d | ||||||
| IBS patients | 14.4 | 13 (14) | 13.3 | 11(13) | 9.7 | 7 (8)b | 10.0 | 9(19)b |
| Bodypart | Pain quality | |||||||
| Neck | Burning, shooting | |||||||
| Arm | Ache slightly, numbing, shooting | |||||||
| Shoulder | Twinging, ache slightly, cramping | |||||||
| Head | Ache slightly, twinging | |||||||
| Back | Ache slightly, twinging, cramping | |||||||
| Stomach | Numbing, cramping, twinging, rasping | |||||||
| Breast | Twinging, cramping, pressure | |||||||
| Leg | Burning, ache slightly, numbing, shooting, cramping | |||||||
| Foot | Numbing, pain | |||||||
The higher the score is, the more the symptoms are. M denotes mean, Md = median, IQR = inter quartile range, AHC: apparently healthy controls.
P < 0.01,
P < 0.01 vs IBS patients at 0 wk.
Symptom checking list questionnaire (SCL90)
Psychological symptoms at baseline measured with SCL90 were significantly more common in the IBS group than in the healthy control group (Table 5). After 12 wk of treatment, the IBS patients had relief in obsessive-compulsive symptoms concerning the sensitivity, hostility, paranoid ideation, psychotisism and somatisation. After 24 wk of body awareness therapy, further improvements were seen and during the 6-mo follow-up, the improvements remained. The subclasses of “depression” and “soma-tisation” correlated positively (Chi-square test, P < 0.01).
Table 5.
SCL90 score from 21 apparently healthy controls and 21 IBS patients at 0, 12 and 24 wk of treatment and 6 mo after end of treatment
| Category |
Before treatment |
After 12 wk |
After 24 wk |
6 mo after end of treatment |
||||
| M | Md (IQR) | M | Md (IQR) | M | Md (IQR) | M | Md (IQR) | |
| AHC | ||||||||
| Totally | 0.3 | 0 (0)d | ||||||
| Obsessive-compulsive | 0.4 | 0 (1)d | ||||||
| Sensitivity | 0.3 | 0 (0)d | ||||||
| Depression | 0.4 | 0 (1)d | ||||||
| Anxiety | 0.4 | 0 (0)d | ||||||
| Hostility | 0.2 | 0 (0)d | ||||||
| Phobic anxiety | 0.01 | 0 (0)d | ||||||
| Paranoid ideation | 0.2 | 0 (0)d | ||||||
| Psychotisism | 0.1 | 0 (0)d | ||||||
| Somatisation | 0.2 | 0 (0)d | ||||||
| Others | 0.4 | 0 (1)d | ||||||
| IBS patients | ||||||||
| Totally | 1.0 | 0 (2) | 0.9 | 0 (1)d | 0.6 | 0 (1)d | 0.7 | 0 (1)d |
| Obsessive-compulsive | 1.3 | 1 (2) | 1.1 | 1 (2)b | 0.8 | 0 (1)d | 0.9 | 0 (1)d |
| Sensitivity | 0.9 | 1 (1) | 0.6 | 0 (1)d | 0.4 | 0 (1)d | 0.5 | 0 (1)d |
| Depression | 1.3 | 1 (2) | 1.2 | 1 (2) | 0.8 | 0 (1)d | 0.9 | 1 (2)d |
| Anxiety | 0.9 | 1 (2) | 1.0 | 0 (2) | 0.8 | 0 (1)a | 0.8 | 0 (1)b |
| Hostility | 0.5 | 0 (1) | 0.3 | 0 (0)b | 0.3 | 0 (0)d | 0.3 | 0 (0)b |
| Phobic anxiety | 0.2 | 0 (0) | 0.2 | 0 (0) | 0.2 | 0 (0)a | 0.2 | 0 (0) |
| Paranoid ideation | 0.8 | 0 (1) | 0.5 | 0 (1)d | 0.4 | 0 (1)d | 0.3 | 0 (1)d |
| Psychotisism | 0.4 | 0 (1) | 0.3 | 0 (0)a | 0.2 | 0 (0)d | 0.2 | 0 (0)b |
| Somatisation | 1.7 | 2 (3) | 1.5 | 1 (3)a | 1.2 | 1 (2)d | 1.3 | 1 (2)d |
| Other | 1.2 | 1 (2) | 1.2 | 1 (2) | 0.9 | 0 (1)d | 0.9 | 0 (2)b |
The result is shown totally and as items categorised. The higher score the more symptoms. M denotes mean, MD: median; IQR: inter quartile range; AHC: apparently healthy controls.
P < 0.05,
P < 0.01,
P < 0.001 vs IBS patients at 0 wk.
Sense of coherence (SOC)
The IBS patients showed a lower sense of coherence than the AH controls before treatment (Table 6). There were also differences in the subclasses of comprehensibility, manageability and meaningfulness. After 12 and 24 wk of body awareness therapy, the sense of coherence improved significantly in total and for each subclass.
Table 6.
Sense of coherence (SOC) score from 21 AH controls and 21 IBS patients at 0, 12 and 24 wk of treatment
| Category |
AHC |
0 wk |
12 wk |
24 wk |
||||
| M | Md (IQR) | M | Md (IQR) | M | Md (IQR) | M | Md (IQR) | |
| SOC totally | 4.2 | 4 (2)d | 3.5 | 4 (3) | 3.8 | 4 (2)d | 3.9 | 4 (2)d |
| Comprehensibility | 3.7 | 4 (2)d | 3.0 | 3 (2) | 3.2 | 3 (3)a | 3.3 | 3(3)b |
| Manageability | 4.4 | 5 (3)d | 3.7 | 4 (3) | 4.0 | 4 (3)d | 4.2 | 5(2)d |
| Meaningfulness | 4.6 | 5 (1)d | 3.9 | 4 (2) | 4.2 | 4 (2)b | 4.1 | 4(2)b |
The result is shown totally and as items categorised. The higher the score is, the better the SOC is. M denotes mean, Md: median; IQR: inter quartile range; AHC: apparently healthy controls.
P < 0.05,
P < 0.01,
P < 0.001 vs IBS patients at 0 wk.
Salivary analysis
At baseline, the IBS patients showed lower cortisol levels in saliva than the AH controls during the day at all time points except for 11.45 h (borderline significance) and 17.00 h. There were wide confidence intervals among the IBS patients from high to low values (Figure 1A). In the IBS patients, the slopes gave no differences during the treatment period. However, when divided in tertiles at baseline, one could notice that those showing tertiles with either a low or a high slope approached the slope of middle and the slope of controls over time (Figure 1B). The expression of somatic symptoms was associated with biochemical symptoms. A relationship was found between the most normal score of muscle palpation and a more optimal slope of saliva cortisol (Figure 2).
Figure 1.
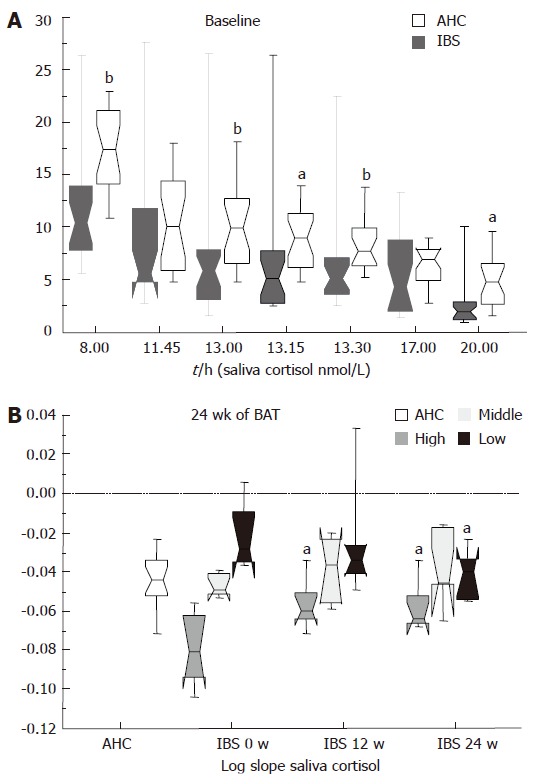
Saliva cortisol (nmol/L) at different time points during the day for appa-rently healthy controls (AHC) and IBS patients at baseline (A). Log of slope of the day for saliva cortisol, AHC and IBS patients (divided at tertiles) at baseline and during treatment (24 wk of body awareness therapy) (B). aP < 0.05, bP < 0.01.
Figure 2.
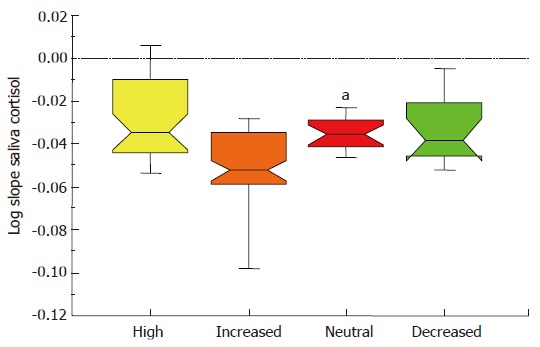
Log slope of saliva cortisol for IBS patients divided in the grade of muscle palpation as high, increased, neutral or decreased. aP < 0.05.
DISCUSSION
In this study of IBS patients, we found at baseline, significant differences in all the parameters studied between the test group (IBS patients) and the control group (apparently healthy volunteers).
Treatment with body awareness therapy for 24 wk gave relief of not only gastrointestinal symptoms, but also of psychological symptoms, as well as improved body awareness and tension in IBS patients. A decreased pain was also seen in other parts of the body in addition to the decreased abdominal pain. The patients had relief of both somatic and depressive symptoms in parallel. The study groups were re-examined during the 6-mo follow-up showing relief of gastrointestinal and psychological symptoms. Their sense of coherence or coping ability also improved after treatment. The saliva slope of cortisol during the day was normalised, supporting the view that body awareness therapy may reduce biochemical stress markers.
Our hypothesis that IBS is associated with altered body tension and body awareness is supported by the differences found between IBS patients and controls at baseline, as well as by the improvement seen after treatment. However, most of the patients in our test group suffered from severe or long lasting IBS. Whether this hypothesis holds true for IBS in general is likely but has to be proven. It has been shown that psychological treatment is essential for some IBS patients[20]. A limitation of our study is the small number of patients. However, our present findings are confirmed by a previous study[35].
In the present study, we did not include IBS control patients, since this was done in a previous study[35]. We did not randomise patients, but included consecutive patients for therapy in the study. There are in the literature reflections on methodological aspects of randomised controlled trials regarding psychotherapy[41] and some researchers argue that these studies are of less value. Therefore, following the same patients systematically, before, under and after therapy seems to be the best method of choice at present. However, the placebo effect cannot be totally excluded in this pilot study testing the acceptance of a new treatment.
A tentative disadvantage of the therapy itself could be the duration of the treatment, two hours a week for 24 wk. In the beginning of the group sessions, body awareness therapy involved a certain time learning the procedure. Body awareness training is needed for the patients to be aware of their own body tension, in order to be able to learn how to apply the body awareness therapy. Especially for the patients with diarrhoea predominant IBS, longer treatment time seems to be needed.
The habits of wrong movements and tension patterns, whether due to chronic stress or other mechanisms, become entrenched in the body and the patients are incapable of changing them. The habits are integrated as a part of their self-perception and can be kept hidden together with suppressed feelings and tensions. To deal with habitual muscular pattern, the individuals must be re-educated in new patterns feeling at least equally familiar as the old ones[29].This teaching/training aspect of body awareness therapy may indicate that this therapy is a way of learning how to handle tension in the body, rather than a short-lived remedy. The remaining relief of symptoms during the 6-mo follow-up supports this view.
Levels of anxiety and depression are significantly higher in patients with IBS than in apparently healthy persons without IBS[8,9]. Another factor that may contribute to the reduction in health-related quality of life in patients with IBS is an ability to cope with stressful circumstances in life, measured as a reduced sense of coherence (SOC). Antonovsky[39] proposed that a strong SOC allows persons to successfully cope with life stressors. Living with alternating constipation and diarrhoea is a problem of daily living that could be considered highly stressful. Thus a strong SOC might lessen the impact of different stressors on well-being, or stressors themselves might weaken SOC. Motzer et al[17] have searched for interventions targeted at enhancing SOC and quality of life and thus ease the psychological distress associated with IBS. Sperber et al[16] questioned whether SOC represents a predictor of treatment success/a stable characteristic or is an outcome variable (changeable). We believe that SOC can act both as a predictor and as an outcome variable. A low SOC at baseline may reflect the severity of IBS, and could prolong the response to treatment. However, in the end of the study, the patients altered their sense of coherence towards normality as a result of the therapy.
Saliva cortisol in a healthy person has a straight downward slope during daytime. A flatter (lower) slope is regarded to reflect a more negative stress response and the slope has been reported to be a prognostic indicator of accumulated physiological and psychosocial stress[42]. Saliva cortisol in the IBS patients changed during treatment, but not significantly in the whole group. However, if divided into tertiles, the slope of saliva cortisol concentration showed a trend towards a normal range from those in the upper and lower tertile. A lowered slope associated with too high or too low muscle palpation grade was seen in our study. The steeper slope of saliva cortisol belonged mostly to the group with somewhat increased muscle palpation grade. The latter may represent the first phase of the body to compensate for stress while a lowered slope represents chronic stress and/or exhaustion[43].
Body awareness therapy has been used both in psychosomatic gynaecology[27], pain/musculoskeletal disorders[44], IBS patients[35] and psychiatric outpatient care[45]. Treatment effects are improvements of body functions, psychiatric symptoms and self efficacy. Also reduced symptoms and negative self-image, increased self love and body image[27] as well as improved health-related quality of life[44] have been reported. A comparative study has shown that body awareness therapy is more effective than conventional physiotherapeutic treatment[46].
Non-pharmacological treatment as well as psycho-therapy, cognitive behavioural therapy, and hypnotherapy are reported to be effective for symptom relief and essential for some IBS patients[19-22]. Studies have shown that psychotherapy is superior to conventional medical therapy and the psychosocial consequences of the illness become more significant with increasing severity of the disease and, therefore, psychosomatic care is valuable[47]. Some of the hypnotherapies described have points of similarity to body awareness therapy. The Manchester model[48,49] and the North Carolina protocol[50] are combinations of hypnotherapy and psychotherapy techniques that emphasize symptom control together with ego-strengthening, adoption of improved coping resources, relaxation and mental calming and a change of cognitive perspectives. The differences between these hypnosis models and body awareness therapy are small. The IBS patients on body awareness therapy increased their self efficacy and quality of life in the same way as patients on hypnotherapy.
In conclusion, IBS patients had higher score of body tension, gastrointestinal and psychological symptoms and biochemical stress markers than healthy control patients. Body awareness therapy reduced these parameters in patients suffering from IBS, an improvement also presented during the 6-mo follow-up. These results support our hypothesis that body tension plays an important part in the clinical expression of IBS, suggesting that body awareness therapy is an alternative or additional therapy for patients with IBS.
ACKNOWLEDGMENTS
The authors express their sincere gratitude to RPT Monica Möller and the Clinical Chemical laboratory, Sahlgrenska University Hospital/ÖSTRA for expert technical assistance.
COMMENTS
Background
Irritable bowel syndrome is the most common of all gastrointestinal disorders, affecting around 15% of the population at least in the Western societies. Due to the complex nature of the disease no long standing, generally accepted therapies are available and the patients consult a broad variety of different health providers.
Research frontiers
The research frontiers are along different lines. One line is focusing on finding particular intestinal mechanisms possibly affected by pharmacologic means. However, in recent years, research has focused on the psychosomatic aspect of the disease. Thus, psychosomatic remedies like hypnotherapy and psychotherapy have been applied.
Innovations and breakthroughs
Psychotherapy and hypnotherapy have both shown to be more efficient than pharmacologic treatment. Body awareness therapy is a physiotherapeutic approach, which has been used in other psychosomatic disorders and in this study it was applied in patients with IBS.
Applications
Body awareness therapy (BAT) has been shown in this study to be beneficial for patients suffering from IBS. BAT may also be applied in a large number of other stress-related syndromes in the future.
Terminology
Body awareness therapy is made up of different practices including becoming aware of tensions in different muscles in the body during sitting, standing, lying and walking. Body awareness scale and resource oriented body examination are methods to measure the body qualities such as centring, midline, flow, respiration, boundaries, function and tension.
Peer review
Comments from peer reviewers have pointed out that the number of patients was small without a control group. Thus, the placebo effect cannot be ignored. However, this was a pilot study necessitating further research.
Footnotes
Supported by grants from Västra Götalandsregionen (proj. No 07), Dagmar (proj. No 643-2000-19) and the University of Gothenburg, Sweden
S- Editor Liu Y L- Editor Wang XL E- Editor Ma WH
References
- 1.Jones R, Lydeard S. Irritable bowel syndrome in the general population. BMJ. 1992;304:87–90. doi: 10.1136/bmj.304.6819.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Longstreth GF, Wolde-Tsadik G. Irritable bowel-type symptoms in HMO examinees. Prevalence, demographics, and clinical correlates. Dig Dis Sci. 1993;38:1581–1589. doi: 10.1007/BF01303163. [DOI] [PubMed] [Google Scholar]
- 3.Talley NJ, Zinsmeister AR, Van Dyke C, Melton LJ. Epidemiology of colonic symptoms and the irritable bowel syndrome. Gastroenterology. 1991;101:927–934. doi: 10.1016/0016-5085(91)90717-y. [DOI] [PubMed] [Google Scholar]
- 4.Wei X, Chen M, Wang J. The epidemiology of irritable bowel syndrome and functional constipation of Guangzhou residents. Zhonghua NeiKe ZaZhi. 2001;40:517–520. [PubMed] [Google Scholar]
- 5.Thompson WG. Irritable bowel syndrome: pathogenesis and management. Lancet. 1993;341:1569–1572. doi: 10.1016/0140-6736(93)90705-l. [DOI] [PubMed] [Google Scholar]
- 6.Olden KW. Diagnosis of irritable bowel syndrome. Gastroenterology. 2002;122:1701–1714. doi: 10.1053/gast.2002.33741. [DOI] [PubMed] [Google Scholar]
- 7.Triadafilopoulos G, Simms RW, Goldenberg DL. Bowel dysfunction in fibromyalgia syndrome. Dig Dis Sci. 1991;36:59–64. doi: 10.1007/BF01300088. [DOI] [PubMed] [Google Scholar]
- 8.Lydiard RB, Greenwald S, Weissman MM, Johnson J, Drossman DA, Ballenger JC. Panic disorder and gastrointestinal symptoms: findings from the NIMH Epidemiologic Catchment Area project. Am J Psychiatry. 1994;151:64–70. doi: 10.1176/ajp.151.1.64. [DOI] [PubMed] [Google Scholar]
- 9.Osterberg E, Blomquist L, Krakau I, Weinryb RM, Asberg M, Hultcrantz R. A population study on irritable bowel syndrome and mental health. Scand J Gastroenterol. 2000;35:264–268. doi: 10.1080/003655200750024128. [DOI] [PubMed] [Google Scholar]
- 10.Abrahamsson H. Gastrointestinal motility in patients with the irritable bowel syndrome. Scand J Gastroenterol Suppl. 1987;130:21–26. doi: 10.3109/00365528709090996. [DOI] [PubMed] [Google Scholar]
- 11.Aggarwal A, Cutts TF, Abell TL, Cardoso S, Familoni B, Bremer J, Karas J. Predominant symptoms in irritable bowel syndrome correlate with specific autonomic nervous system abnormalities. Gastroenterology. 1994;106:945–950. doi: 10.1016/0016-5085(94)90753-6. [DOI] [PubMed] [Google Scholar]
- 12.Bolin TD. Irritable bowel syndrome. Aust Fam Physician. 2005;34:221–224. [PubMed] [Google Scholar]
- 13.Barbara G, De Giorgio R, Stanghellini V, Cremon C, Corinaldesi R. A role for inflammation in irritable bowel syndrome? Gut. 2002;51 Suppl 1:i41–i44. doi: 10.1136/gut.51.suppl_1.i41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Derbyshire SW. Visceral afferent pathways and functional brain imaging. Scientific World Journal. 2003;3:1065–1080. doi: 10.1100/tsw.2003.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Whitehead WE, Crowell MD, Robinson JC, Heller BR, Schuster MM. Effects of stressful life events on bowel symptoms: subjects with irritable bowel syndrome compared with subjects without bowel dysfunction. Gut. 1992;33:825–830. doi: 10.1136/gut.33.6.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sperber AD, Carmel S, Atzmon Y, Weisberg I, Shalit Y, Neumann L, Fich A, Buskila D. The sense of coherence index and the irritable bowel syndrome. A cross-sectional comparison among irritable bowel syndrome patients with and without coexisting fibromyalgia, irritable bowel syndrome non-patients, and controls. Scand J Gastroenterol. 1999;34:259–263. doi: 10.1080/00365529950173654. [DOI] [PubMed] [Google Scholar]
- 17.Motzer SA, Hertig V, Jarrett M, Heitkemper MM. Sense of coherence and quality of life in women with and without irritable bowel syndrome. Nurs Res. 2003;52:329–337. doi: 10.1097/00006199-200309000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Tack J, Fried M, Houghton LA, Spicak J, Fisher G. Systematic review: the efficacy of treatments for irritable bowel syndrome--a European perspective. Aliment Pharmacol Ther. 2006;24:183–205. doi: 10.1111/j.1365-2036.2006.02938.x. [DOI] [PubMed] [Google Scholar]
- 19.Svedlund J, Sjödin I, Ottosson JO, Dotevall G. Controlled study of psychotherapy in irritable bowel syndrome. Lancet. 1983;2:589–592. doi: 10.1016/s0140-6736(83)90678-5. [DOI] [PubMed] [Google Scholar]
- 20.Creed F. Irritable bowel or irritable mind? Psychological treatment is essential for some. BMJ. 1994;309:1647–1648. doi: 10.1136/bmj.309.6969.1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Simrén M. Hypnosis for irritable bowel syndrome: the quest for the mechanism of action. Int J Clin Exp Hypn. 2006;54:65–84. doi: 10.1080/00207140500327239. [DOI] [PubMed] [Google Scholar]
- 22.Whitehead WE. Hypnosis for irritable bowel syndrome: the empirical evidence of therapeutic effects. Int J Clin Exp Hypn. 2006;54:7–20. doi: 10.1080/00207140500328708. [DOI] [PubMed] [Google Scholar]
- 23.Dotevall G. Involvement of cardiac, respiratory and gastrointestinal functions in neural responses to stressful events. Integr Physiol Behav Sci. 1994;29:374–382. doi: 10.1007/BF02691357. [DOI] [PubMed] [Google Scholar]
- 24.Mattsson B, Mattsson M. The concept of "psychosomatic" in general practice. Reflections on body language and a tentative model for understanding. Scand J Prim Health Care. 2002;20:135–138. doi: 10.1080/028134302760234564. [DOI] [PubMed] [Google Scholar]
- 25.Skatteboe UB, Friis S, Hope MK, Vaglum P. Body awareness group therapy for patients with personality disorders. 1. Description of the therapeutic method. Psychother Psychosom. 1989;51:11–17. doi: 10.1159/000288128. [DOI] [PubMed] [Google Scholar]
- 26.Mattsson M, Wikman W, Dahlgren L, Mattsson B, Armelius K. Body Awareness therapy with sexually abused women Part 1. Description of a treatment modality. J Bodywork & MovTher. 1997;1:280–288. [Google Scholar]
- 27.Mattsson M, Wikman M, Dahlgren L, Mattsson B, Armelius K. Body awareness therapy with sexually abused women Part 2. Evaluation of body awareness in a group setting. J Bodywork & MovTher. 1997;2:38–45. [Google Scholar]
- 28.Sjödahl C, Jarnlo GB, Persson BM. Gait improvement in unilateral transfemoral amputees by a combined psychological and physiotherapeutic treatment. J Rehabil Med. 2001;33:114–118. doi: 10.1080/165019701750165934. [DOI] [PubMed] [Google Scholar]
- 29.Lundvik Gyllensten A, Hansson L, Ekdahl C. Patient experiences of basic body awareness therapy and the relationship with the physiotherapist. J Bodywork & MovTher. 2003;7:173–183. [Google Scholar]
- 30.Eriksson E, Mokhtari M, Pourmotamed L, Holmdahl L, Eriksson H. Interrater reliability in a resource-oriented physiotherapeutic examination. Phy Theo & Prac. 2000;16:95–105. [Google Scholar]
- 31.Bunkan BH, Ljunggren AE, Opjordsmoen S, Moen O, Friis S. What are the basic dimensions of movements? A psychometric evaluation of the Comprehensive Body Examination III. Nord J Psychiatry. 2001;55:33–40. doi: 10.1080/080394801750093706. [DOI] [PubMed] [Google Scholar]
- 32.Gyllensten AL, Ekdahl C, Hansson L. Validity of the Body Awareness Scale-Health (BAS-H) Scand J Caring Sci. 1999;13:217–226. [PubMed] [Google Scholar]
- 33.Ryding C, Rudebeck CE, Roxendal G. Assessing body awareness in healthy subjects – the first step towards the construction of the BAS-Health. Adv in Physiother. 2000;2:176–182. [Google Scholar]
- 34.Gyllensten AL, Ovesson MN, Lindström I, Hansson L, Ekdahl C. Reliability of the Body Awareness Scale-Health. Scand J Caring Sci. 2004;18:213–219. doi: 10.1111/j.1471-6712.2004.00272.x. [DOI] [PubMed] [Google Scholar]
- 35.Eriksson E, Nordwall V, Kurlberg G, Rydholm H, Eriksson A. Effects of Body Awareness Therapy in Patients with Irritable Bowel Syndrome. Adv Physiother. 2002;4:125–135. [Google Scholar]
- 36.Agréus L, Svärdsudd K, Nyrén O, Tibblin G. Reproducibility and validity of a postal questionnaire. The abdominal symptom study. Scand J Prim Health Care. 1993;11:252–262. doi: 10.3109/02813439308994840. [DOI] [PubMed] [Google Scholar]
- 37.Margolis RB, Tait RC, Krause SJ. A rating system for use with patient pain drawings. Pain. 1986;24:57–65. doi: 10.1016/0304-3959(86)90026-6. [DOI] [PubMed] [Google Scholar]
- 38.Derogatis LR, Cleary PA. Factorial invariance across gender for the primary symptom dimensions of the SCL-90. Br J Soc Clin Psychol. 1977;16:347–356. doi: 10.1111/j.2044-8260.1977.tb00241.x. [DOI] [PubMed] [Google Scholar]
- 39.Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med. 1993;36:725–733. doi: 10.1016/0277-9536(93)90033-z. [DOI] [PubMed] [Google Scholar]
- 40.Altman DG. Practical statistics for medical research. London: Chapman & Hall;; 1995. [Google Scholar]
- 41.Scott J, Sensky T. Methodological aspects of randomized controlled trials of psychotherapy in primary care. Psychol Med. 2003;33:191–196. doi: 10.1017/s0033291702007262. [DOI] [PubMed] [Google Scholar]
- 42.Sephton SE, Sapolsky RM, Kraemer HC, Spiegel D. Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst. 2000;92:994–1000. doi: 10.1093/jnci/92.12.994. [DOI] [PubMed] [Google Scholar]
- 43.Rosmond R, Björntorp P. Low cortisol production in chronic stress. The connection stress-somatic disease is a challenge for future research. Lakartidningen. 2000;97:4120–4124. [PubMed] [Google Scholar]
- 44.Grahn BE, Borgquist LA, Ekdahl CS. Motivated patients are more cost-effectively rehabilitated. A two-year prospective controlled study of patients with prolonged musculoskeletal disorders diagnosed in primary care. Int J Technol Assess Health Care. 2000;16:849–863. doi: 10.1017/s0266462300102120. [DOI] [PubMed] [Google Scholar]
- 45.Mattsson M, Wikman M, Dahlgren L, Mattsson B. Physiotherapy as empowerment-treating women with chronic pelvic pain. Adv in Physiother. 2000;2:125–143. [Google Scholar]
- 46.Malmgren-Olsson EB, Armelius B�, Armelius K. Comparative study of the Efficacy of Body Awareness Therapy, Feldenkrais and Conventional Physiotherapy in patients with prolonged unspecific musculoskeletal disorders-Changes in physiological symptoms, pain and self-images. Physiotherapy theory practice. 2001;17:77–95. [Google Scholar]
- 47.Moser G. Psychosomatic aspects of bowel diseases. Z Psychosom Med Psychother. 2006;52:112–126. doi: 10.13109/zptm.2006.52.2.112. [DOI] [PubMed] [Google Scholar]
- 48.Whorwell PJ. Effective management of irritable bowel syndrome--the Manchester Model. Int J Clin Exp Hypn. 2006;54:21–26. doi: 10.1080/00207140500323006. [DOI] [PubMed] [Google Scholar]
- 49.Gonsalkorale WM. Gut-directed hypnotherapy: the Manchester approach for treatment of irritable bowel syndrome. Int J Clin Exp Hypn. 2006;54:27–50. doi: 10.1080/00207140500323030. [DOI] [PubMed] [Google Scholar]
- 50.Palsson OS. Standardized hypnosis treatment for irritable bowel syndrome: the North Carolina protocol. Int J Clin Exp Hypn. 2006;54:51–64. doi: 10.1080/00207140500322933. [DOI] [PubMed] [Google Scholar]


