Abstract
AIM: To investigate the effect of chronic inflammatory bowel disease (CIBD) specific risk factors for cholecystolithiasis, as duration and involvement pattern of the disease and prior surgery in patients with Crohn's disease (CD) and ulcerative colitis (UC).
METHODS: A total of 222 patients with CD (135 females, 87 males; average age, 35.8 ± 11.8 years; range 17-81 years) and 88 patients with UC (39 females, 49 males; average age, 37.2 ± 13.6 years; range 16-81 years) underwent clinical and ultrasound examinations. Besides age, sex and degree of obesity, patients? CIBD specific parameters, including duration and extent of disease and prior operations were documented and evaluated statistically using logistic regression.
RESULTS: The overall prevalence of gallbladder stone disease in patients with CD was 13% (n = 30). Only age could be shown to be an independent risk factor (P = 0.014). Compared to a collective representative for the general population in the same geographic region, the prevalence of cholecystolithiasis was higher in all corresponding age groups. Patients with UC showed an overall prevalence of gallbladder stone disease of only 4.6%.
CONCLUSION:Only age but not disease-specific factors such as duration and extent of disease, and prior surgery are independent risk factors for the development of cholecystolithiasis in patients with CIBD.
Keywords: Crohn's disease, Ulcerative colitis, Gallstone disease, Ultrasonography, Ultrasound
INTRODUCTION
Besides the other extraintestinal complications[1] there is an increased rate of cholecystolithiasis in patients suffering from chronic inflammatory bowel disease (CIBD)[2-5]. The findings reported for ulcerative colitis (UC) are contradictory[6,7]. In the case of Crohn抯 disease (CD), the reports published to date are also inconsistent with regard to disease-specific factors, such as the duration of the disease[3,5,7,8] prior surgery (bowel resection)[2-4,7,8] and the pattern of disease involvement[2-6]. However, the incidence rate of gallbladder stone disease in patients with CIBD is often twice as high as in the general population, though the reason for this difference has yet to be satisfactorily explained[2-4]. In the majority of European and North American studies of the prevalence of cholecystolithiasis, there is a preponderance of cholesterol gallstones in the general population. The main identifiable risk factors for developing gallbladder stones include female sex, obesity and increasing age. In Asians, who show a high proportion of pigment gallstones, this predominance of females over males is not seen[9,10].
The pathophysiological explanation for the increased prevalence of gallbladder stones in patients with CD refers to the reduced absorption of bile acids in individuals with extensive involvement of the terminal ileum or following ileal resection[6,8]. The absolute number of bowel resections, the length of resected bowel and postoperative hypomotility of the gallbladder with subsequent formation of sludge and later, stones are currently under discussion as major risk factors for the higher prevalence of cholecystolithiasis in patients with CIBD[2-5].
The present study was to evaluate the importance of both the classical cholecystolithiasis risk factors, such as age, female sex and obesity and the effect of disease-specific parameters such as duration of the disease, pattern of involvement and prior surgery on the prevalence of gallbladder stones in patients with CD and UC.
MATERIALS AND METHODS
Patients
A total of 310 patients with CIBD presenting consecutive to our departmental section on Crohn's disease and ulcerative colitis over a period of approximately one year were screened for inclusion in the present study. The present study was conducted prospectively in accordance with the principles of the Helsinki Declaration and approved by the Ethics Commission of the Medical Faculty.
Inclusion criteria included histologically confirmed CIBD and no history of cholecystolithiasis prior to first diagnosis of CIBD. Included in the study population were 222 patients with CD (135 females, 87 males; average age, 35.8 ± 11.8 years; range 17-81 years) and 88 patients with UC (39 females, 49 males; average age, 37.2 ± 13.6 years; range 16-81 years). The average period since the first diagnosis was 8.9 ± 7.5 years (range: 0-34 years) in the group with CD and 6.8 ± 5.8 years (range: 0-29 years) in the UC collective.
Risk factors
Besides the classical risk factors (age, female sex, obesity), disease-specific parameters such as time elapsed since the first diagnosis, pattern of disease involvement and prior surgical bowel resection in patients with CIBD were studied. Patients were subdivided into four age groups: ≤30 years, 31-40 years, 41-50 years and 51 years and above.
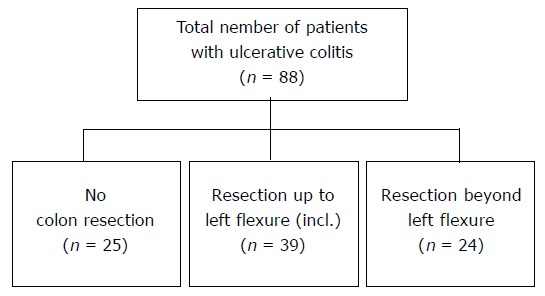
For evaluation of obesity, patients were divided into three groups on the basis of their body-mass index (BMI):
Math 1
Math 1.
Math(A1).
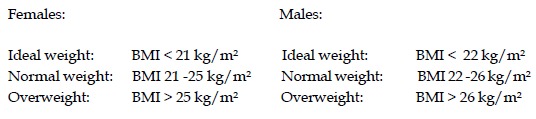
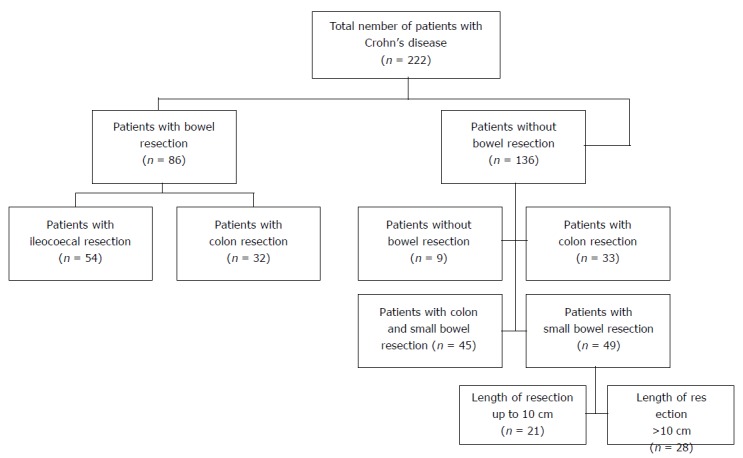
In order to study the effects of the duration of the disease (expressed as time elapsed since the first diagnosis with histological confirmation to the time of examination in the present study), patients were divided into four groups: up to 5 years, 6-10 years, 11-15 years and greater than 15 years. With regard to the parameter extent/pattern of disease, we differentiated in the CD group between patients who underwent or did not undergo surgical bowel resection. The group of patients who underwent resection was further subdivided into those who underwent ileocaecal resection and those who had undergone colectomy we did not further differentiate between partial and total colectomy (Figure 1). Type and number of bowel resections were obtained from the patient's chart. Patients with UC were divided into three subgroups: patients with no active disease, patients with disease involvement up to the left colic flexure, and patients with disease extending beyond the left colic flexure (Figure 2). Because only a few patients in the UC collective underwent either partial or total colectomy, a further differentiation between subcollectives with or without history of prior surgery was not done.
Figure 1.
Pattern of involvement and bowel resections in patients with Crohn's disease.
Figure 2.
Pattern of involvement and bowel resections in patients with ulcerative colitis.
Examination
Patients presented in the morning for ultrasound examination in a fasting state.
The criteria for the diagnosis of cholecystolithiasis were defined as follows: one or more echogenic structures in the gallbladder with dorsal shadow; one or more echogenic structures in the gallbladder without dorsal shadow, which by means of multiplanar visualization or attempted mobilization could be differentiated with certainty from a gallbladder septum, Heister's valve or gallbladder polyps; a structure with significant echogenicity and dorsal shadow in the area of the gallbladder, whose lumen was not definitely visualized; one or more echogenic structures in the gallbladder with or without dorsal shadow in the biliary tract; and no visualized gallbladder lumen in patients with history of prior cholecystectomy and corresponding incision(s) in the right upper abdominal quadrant.
Ultrasound examinations were performed using either the Ultramark 4 Plus or Ultramark 9 HDI with the 3.5- and 5.0-MHz transducer heads (ATL, Bothell, Washington, USA). Examination of the upper abdomen was conducted using the 3.5-MHz transducer head, while examination of the bowel was performed using the 5.0-MHz head. Ultrasound examinations were performed exclusively by two physicians experienced in diagnostic ultrasound of the abdomen. One-time visualization of concrements in the gallbladder based on the above criteria led to the patient's classification as suffering from cholecystolithiasis.
Evaluation of the pattern of disease involvement in the bowel was performed on the basis of sonographic criteria considering thickening of the intestinal wall. Wall thickness greater than 3 mm was considered pathologic. Bowel resection and time elapsed since the first diagnosis were established from the patient's history and chart.
Statistical treatment of the data
All data were first evaluated descriptively. For quantitative parameters, either mean with standard deviation or median with minimum and maximum was documented. While for qualitative parameters, relative and absolute frequencies were calculated.
The evaluation for prevalence in the subgroups and their confidence intervals was performed using a logistic regression model[11]. This model reproduces the influence of potential risk factors (independent variables) for the occurrence of a disease (dichotomous target parameter: here, cholecystolithiasis: yes/no). The importance of the potential risk factor was determined by the likelihood ratio test. By multiple application, several influence parameters could be simultaneously tested in one model and their respective influences were adjusted with regard to the other variables. The respective odds ratios, 95% confidence intervals and P-values served to quantify the change in risk of developing cholecystolithiasis due to the given factor. P-values between 0.05 and 0.1 were considered to represent trends or tendencies, while P<0.05 was considered statistically significant and the factor was classified as a "risk" The classical risk factors such as age, sex and BMI were included in the evaluation. Statistical calculation was performed using the SAS statistics software program (Institute Inc., Cary, NC).
RESULTS
Crohn's Disease
Patients with existing cholecystolithiasis and those with prior cholecystectomy were treated as a single group. Examination revealed gallbladder stones in 18 of the 222 patients with CD, while the other 12 underwent prior cholecystectomy, yielding a gallbladder stone prevalence of 13.5% (n = 30). The group of patients ≤30 years of age numbered 101 subjects, representing nearly half of the collective. In these patients, gallbladder stone prevalence stood at 8% (n = 8). Prevalence of gallbladder stone disease increased with advancing age. The highest prevalence was found in the group of patients aged ≥51 years, and stood at 37% in 10 of 27 subjects. No sex-specific differences were observed (Table 1).
Table 1.
Prevalence of cholecystolithiasis in relation to age and sex in Crohn's disease patients
| Age(yr) | n | Males prevalence (%) | n | Females prevalence (%) | n | Total prevalence (%) |
| ≤30 | 39 | 3 | 62 | 11 | 101 | 8 |
| 31-40 | 20 | 10 | 41 | 12 | 61 | 11 |
| 41-50 | 14 | 14 | 19 | 16 | 33 | 15 |
| 51≥ | 14 | 36 | 13 | 38 | 27 | 37 |
| Total | 87 | 11 | 135 | 15 | 222 | 13.5 |
Due to disease-specific implications, overweight patients with CD were rare. Thus, 45% of patients belonged to class I (n = 100), 37% to class II (n = 83) and only 18% to class III (n = 39). Assignment of patients to the various weight classes yielded a gallbladder stone prevalence of 14% (n = 14) for class I, 11% (n = 9) for class II and 13% (n = 7) for class III (Table 2).
Table 2.
Prevalence of cholecystolithiasis in relation to BMI, disease duration, pattern of involvement and bowel resections in Crohn's disease patients
| BMI-classes | Patients (n) | Prevalence (%) |
| Ideal weight (males:< 22; females:< 21) | 100 | 14 |
| Normal weight (males: 22-26; females: 21-25) | 97 | 11 |
| Overweight (males: > 26; females: > 25) | 26 | 13 |
| Total | 222 | 13.5 |
| Disease duration in years | ||
| 1-5 yr | 86 | 8 |
| 6-10 yr | 57 | 12 |
| 11-15 yr | 32 | 9 |
| 16-34 yr | 47 | 28 |
| Total | 222 | 13.5 |
| Pattern of disease involvement | ||
| or prior surgery | ||
| No visualized involvement | 9 | 22 |
| Isolated to small bowel | 49 | 6 |
| Isolated to colon | 33 | 6 |
| Both small bowel and colon involved | 45 | 13 |
| Ileocaecal-/ileal resection | 54 | 22 |
| Partial or total colectomy | 32 | 16 |
| Total | 222 | 13.5 |
Another parameter studied was the duration of CIBD. In the group of patients in whom elapsed time since the first diagnosis was 1-5 years, prevalence was the lowest. While in the other groups, the prevalence stood at 12%, 9%, and 28%, respectively (Table 2).
Isolated disease involvement affecting only the small bowel was observed in 49 patients. Isolated disease involvement affecting only the colon was seen in 33 patients, while the remaining 45 patients suffered from disease involving both the small bowel and colon. Patients who underwent surgical treatment were counted as a separate subgroup. The subgroup of patients with isolated disease affecting either the small intestine or colon only showed prevalence of 6%, each. Patients with disease affecting both the small and large bowel, gallbladder stone prevalence stood at 13% (Table 2).
Evaluating for length of affected bowel segments, prevalence of gallbladder stones in a group of 21 patients with segment length up to 10 cm stood at 5% (n = 1) and at 7% in 28 patients with segment length exceeding of 10 cm (n = 2).
Eighty-six of all the patients in the CD group, underwent surgical bowel resection. Fifty-four patients underwent ileocaecal and/or ileum resection, while four other patients underwent ileotransversostomy or ileoascendostomy in addition to ileocaecal resection. Seventeen patients had a history of right hemicolectomy, while the other 10 underwent segmental colectomy. Only one patient underwent total colectomy. The groups with ileocaecal resection and ileum resection were combined in the univariate statistical analysis and compared to the group with colon resections.
In the group of patients who underwent partial resection of the small bowel, prevalence of gallbladder stone disease stood at 22% (12 of 54) and at 16% (5 of 32) in the colec-tomized group.
A logistic regression model considering patients? age, sex and BMI identified only age as a risk factor for developing gallbladder stone disease. No correlation with the prevalence of gallbladder stones was observed for the parameters such as sex, BMI, disease pattern, duration of the disease and prior intestinal resections (Table 3).
Table 3.
Risk factors for gallbladder stone disease at multiple logistic regression in patients with Crohn's disease
| Risk factors | Odds ratio | 95% | P |
| (OR) | CI | ||
| Age (yr) | 1.048 | 1.010-1.089 | 10.0143 |
| Female Sex | 1.732 | 0.704-4.263 | 0.2321 |
| BMI (kg/m2) | 0.937 | 0.822-1.069 | 0.3357 |
| Duration of disease | 1.045 | 0.983-1.111 | 0.1627 |
| Pattern of involvement / bowel resections | 0.236 | 0.025-4.611 | 0.497 |
statistically significant.
Ulcerative Colitis
Criteria used in the evaluation of the collective of patients with UC corresponded to those applied to CD patients. The overall prevalence of gallbladder stones in the UC group was lower than the comparable prevalence in the CD group. In the smaller subcollective of the UC group, gallbladder stones were observed only in female subjects. Using the same BMI-based weight classes applied to the CD collective, the following distribution according to weight was found in the UC group: 42% (n = 37), ideal weight; 34% (n = 30), normal weight; and 24% (n = 21), overweight. In the group of UC patients at ideal body weight, 5% (n = 2) had gallbladder stones, compared to 7% (n = 2) in those at normal weight and in none of the 21 overweight patients
Univariate analysis yielded a gallbladder stone prevalence of 2% in patients who had elapsed 1-5 years since the first diagnosis of UC, 10% in the 6-10 year group and 6% in the 11-15 year group. In the group of patients who had passed 16-34 years since the first diagnosis, no disease was complicated by the development of cholecystolithiasis.
In 39 patients, disease did not extend the left colic flexure, while areas of bowel involvement beyond the left colic flexure were observed in 24 patients. Failure to visualize thickening of the intestinal at the time of examination was documented in 25 patients. Prevalence of gallbladder stone disease stood at 3% (n = 1) in patients with disease not extending the left colic flexure, but in 12.5% (n = 3) in those with disease involvement beyond the left colic flexure. We did not find evidence of gallbladder stone disease in any of the patients without documented bowel wall thickening at the time of examination. Unlike the group of patients with CD, the number of patients in the UC group with a history of prior bowel resections was too small for meaningful statistical analysis.
Because of the small number of gallstones (n = 4) identified in the UC group, no subgroup analyses were conducted
DISCUSSION
The prevalence of gallbladder stones in patients with Crohn's disease in our collective was 13.5%, which is almost twice as high as that (7-8%) for age-matched groups of the general population in the same geographic area[12]. Comparable findings have also been reported from Italy and Sweden[2-4]. On the other hand, patients with ulcerative colitis have a prevalence of 4.6% and are not more frequently affected by cholecystolithiasis. Only Lorusso et al[6] and Jones et al[13] have reported that the prevalence of cholecystolithiasis is higher in UC patients than in the general population. Recent prospective sonographic surveys of larger CD and UC populations have studied the prevalence of cholecystolithiasis in these groups in comparison to a general population and used a multivariate logistic regression model to estimate the relative risk associated with the respective parameters[2-6]. Many, mostly earlier studies are unsuitable for comparison because of selection bias in the reference group, non-correspondence of the survey period or survey in another geographic region[14-17]. Other researchers have not drawn a comparison[7,18].
In the group of patients with CD, the prevalence increased with age from 8% in the group of subjects under 30 years of age to 37% in the 51-and-over age group. The multivariate analysis identified only age as an independent risk factor (OR: 1.048; CI: 1.010-1.089; P = 0.0143). It was reported that the prevalence of gallbladder stone increases in higher age groups[5,6] . In our own collective of patients with UC, we were not able to identify any correlation between advancing age and increased prevalence of cholecystolithiasis.
In our initial evaluation, sex was also identified as a univariate risk factor in CD and UC patients, though this did not hold true when the multiple logistic regression model was applied. The actual influence of female sex as a risk factor in the etiology of gallbladder stones is controversial[2,3,6,7,14]. Because of the small number of subjects in most studies, the results should be interpreted with caution.
Multiple analysis failed to demonstrate an increased prevalence of cholecystolithiasis in relation to the degree of obesity in either the CD (P = 0.3357) or UC (P = 0.8397) groups in our population. Most studies, especially the newer ones, have not included BMI as a risk factor in studies of UC patients[14-16,19]. Lorusso et al[6] and Schõlmerich et al[7] have also failed to identify evidence supporting patients? degree of obesity as an independent risk factor contributing to the development of cholecystolithiasis.
Univariate analysis of disease duration suggested a correlation between the increasing length of time elapsed since the first diagnosis of CIBD and the prevalence of gallbladder stone disease. This was not confirmed by multiple logistic regression analysis (P = 0.1627) as it has been previously[2,3]. Findings in the literature are contradictory[17,20,21]. Reasons for the divergent findings are to be sought in the characteristics of the disease and in individual disease history of patients. In order to arrive at a relevant and objective evaluation of disease duration as an independent risk factor contributing to increased prevalence of cholecystolithiasis, analysis must include other factors, such as inflammatory activity, pattern of disease involvement, number and type of bowel resections, number and duration of remission phases, as well as type and success of other therapeutic measures. Because of the small number of cases in this subgroup, further statistical evaluation of these influence parameters was not meaningful. Gallstone prevalence was at 22% in patients with partial resection of the small bowel (n = 12) and 16% in the group that underwent resection of the colon (n = 12). Partial resection of the small bowel could not be identified as an independent risk factor in the multivariate analysis (P = 0.4970). Our data contradict those of previous[2,3]. A possible reason for the failure to identify the extent and number of bowel resections as independent risk factors at multivariate analysis may be the smaller number of patients in our collective who underwent ileocecal resection.
Because a separate evaluation of pattern of disease involvement and bowel resection is difficult, we defined these as a single parameter in our multiple logistic regression. The retrospective evaluation of surgical findings further limits the strength of our results. Multiple analysis failed to reveal any correlation between cholecystolithiasis, pattern of disease involvement and prior surgical bowel resection in CD patients (P = 0.4970). Earlier radiologic studies have shown an increase in gallbladder stone prevalence in relation to the length of resected bowel segments[4,8,9,16,18]. The disadvantages of these studies, however, refer primarily to the absence of multivariate analysis and a small number of subjects.
Studies showed that the bile acid pool reduces in patients with Crohn's disease[22]. Lapidus et al[23,24] showed that the risk for pigment gallstones increases in patients with ileocoecal resections accompanied with manifestly elevated bilirubin and deoxycholic acid fractions in the bile suggesting that an increased risk for cholesterol gallstones in these patients does not exist.
Recently published data show that patients with Crohn's disease after colectomy or patients with small bowel Crohn's disease have an increased risk for cholesterol stones, and that patients with ileitis are prone to develop mixed, pigment-rich gallstones[25]. These changes after colectomy have not been detected in patients with ulcerative colitis[26].
In conclusion, the findings of the present study have identified only "age"as an independent risk factor for increased prevalence of gallbladder stones. Neither disease duration, pattern of disease involvement nor number or total length of resected bowel segments appear to be risk factors contributing to the development of gallbladder stones in these patients. Prospective multicenter studies should be conducted to assess all potential risk factors including therapy intervals between disease flares, phases of parenteral nutrition and prospective documentation of surgical data.
Footnotes
Science Editor Wang XL and Guo SY Language Editor Elsevier HK
References
- 1.Lakatos L, Pandur T, David G, Balogh Z, Kuronya P, Tollas A, Lakatos PL. Association of extraintestinal manifestations of inflammatory bowel disease in a province of western Hungary with disease phenotype: results of a 25-year follow-up study. World J Gastroenterol. 2003;9:2300–2307. doi: 10.3748/wjg.v9.i10.2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bargiggia S, Maconi G, Elli M, Molteni P, Ardizzone S. Sonographic prevalence of liver steatosis and biliary tract stonesin patients with inflammatory bowel disease: study of 511 subjects at a single center. J Clin Gastroenterol. 2003;36:417–420. doi: 10.1097/00004836-200305000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Fraquelli M, Losco A, Visentin S, Cesana BM, Pometta R, Colli A, Conte D. Gallstone disease and related risk factors in patients with Crohn disease: analysis of 330 consecutive cases. Arch Intern Med. 2001;161:2201–2204. doi: 10.1001/archinte.161.18.2201. [DOI] [PubMed] [Google Scholar]
- 4.Lapidus A, Bångstad M, Aström M, Muhrbeck O. The prevalence of gallstone disease in a defined cohort of patients with Crohn's disease. Am J Gastroenterol. 1999;94:1261–1266. doi: 10.1111/j.1572-0241.1999.01076.x. [DOI] [PubMed] [Google Scholar]
- 5.Hutchinson R, Tyrrell PN, Kumar D, Dunn JA, Li JK, Allan RN. Pathogenesis of gall stones in Crohn's disease: an alternative explanation. Gut. 1994;35:94–97. doi: 10.1136/gut.35.1.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lorusso D, Leo S, Mossa A, Misciagna G, Guerra V. Cholelithiasis in inflammatory bowel disease. A case-control study. Dis Colon Rectum. 1990;33:791–794. doi: 10.1007/BF02052328. [DOI] [PubMed] [Google Scholar]
- 7.Schölmerich J, Braun G, Volk BA, Spamer C, Hoppe-Seyler P, Gerok W. Detection of extraintestinal and intestinal abnormalities in inflammatory bowel disease by ultrasound. Dig Surg. 1987;4:82–87. doi: 10.1159/000171776. [DOI] [Google Scholar]
- 8.Kangas E, Lehmusto P, Matikainen M. Gallstones in Crohn's disease. Hepatogastroenterology. 1990;37:83–84. [PubMed] [Google Scholar]
- 9.Brett M, Barker DJ. The world distribution of gallstones. Int J Epidemiol. 1976;5:335–341. doi: 10.1093/ije/5.4.335. [DOI] [PubMed] [Google Scholar]
- 10.Kratzer W, Mason RA, Kächele V. Prevalence of gallstones in sonographic surveys worldwide. J Clin Ultrasound. 1999;27:1–7. doi: 10.1002/(SICI)1097-0096(199901)27:1<1::AID-JCU1>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 11.Hosmer DW, Lemeshow S. Applied logistic regression. New York Wiley. 1989. [Google Scholar]
- 12.Kratzer W, Kron M, Hay B, Pfeiffer MM, Kächele V. Prevalence of cholecystolithiasis in South Germany--an ultrasound study of 2,498 persons of a rural population. Z Gastroenterol. 1999;37:1157–1162. [PubMed] [Google Scholar]
- 13.Jones MR, Gregory D, Evans KT, Rhodes J. The prevalence of gallbladder disease in patients with ileostomy. Clin Radiol. 1976;27:561–562. doi: 10.1016/S0009-9260(76)80132-8. [DOI] [PubMed] [Google Scholar]
- 14.Kurchin A, Ray JE, Bluth EI, Merritt CR, Gathright JB, Pehrsson BF, Ferrari BT. Cholelithiasis in ileostomy patients. Dis Colon Rectum. 1984;27:585–588. doi: 10.1007/BF02553842. [DOI] [PubMed] [Google Scholar]
- 15.Baker AL, Kaplan MM, Norton RA, Patterson JF. Gallstones in inflammatory bowel disease. Am J Dig Dis. 1974;19:109–112. doi: 10.1007/BF01072619. [DOI] [PubMed] [Google Scholar]
- 16.Hill GL, Mair WS, Goligher JC. Gallstones after ileostomy and ileal resection. Gut. 1975;16:932–936. doi: 10.1136/gut.16.12.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heaton KW, Read AE. Gall stones in patients with disorders of the terminal ileum and disturbed bile salt metabolism. Br Med J. 1969;3:494–496. doi: 10.1136/bmj.3.5669.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andersson H, Bosaeus I, Fasth S, Hellberg R, Hultén L. Cholelithiasis and urolithiasis in Crohn's disease. Scand J Gastroenterol. 1987;22:253–256. doi: 10.3109/00365528708991889. [DOI] [PubMed] [Google Scholar]
- 19.Bluth EI. Ultrasound evaluation of small bowel abnormalities. Am J Gastroenterol. 1983;78:788–793. [PubMed] [Google Scholar]
- 20.Heaton KW. Disturbances of bile acid metabolism in intestinal disease. Clin Gastroenterol. 1977;6:69–89. [PubMed] [Google Scholar]
- 21.Marks JW, Conley DR, Capretta TL, Bonorris GG, Chung A, Coyne MJ, Schoenfield LJ. Gallstone prevalence and biliary lipid composition in inflammatory bowel disease. Am J Dig Dis. 1977;22:1097–1100. doi: 10.1007/BF01072864. [DOI] [PubMed] [Google Scholar]
- 22.Vantrappen G, Ghoos Y, Rutgeerts P, Janssens J. Bile acid studies in uncomplicated Crohn's disease. Gut. 1977;18:730–735. doi: 10.1136/gut.18.9.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lapidus A, Einarsson K. Effects of ileal resection on biliary lipids and bile acid composition in patients with Crohn's disease. Gut. 1991;32:1488–1491. doi: 10.1136/gut.32.12.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lapidus A, Einarsson C. Bile composition in patients with ileal resection due to Crohn's disease. Inflamm Bowel Dis. 1998;4:89–94. doi: 10.1002/ibd.3780040204. [DOI] [PubMed] [Google Scholar]
- 25.Pereira SP, Bain IM, Kumar D, Dowling RH. Bile composition in inflammatory bowel disease: ileal disease and colectomy, but not colitis, induce lithogenic bile. Aliment Pharmacol Ther. 2003;17:923–933. doi: 10.1046/j.1365-2036.2003.01529.x. [DOI] [PubMed] [Google Scholar]
- 26.Akerlund JE, Einarsson C. Effects of colectomy on bile composition, cholesterol saturation and cholesterol crystal formation in humans. Int J Colorectal Dis. 2000;15:248–252. doi: 10.1007/s003840000228. [DOI] [PubMed] [Google Scholar]


