Abstract
Objectives:
To re-evaluate the epidemiology of hand, foot, and mouth disease (HFMD) in a non-vaccinated population in Zunyi, China.
Methods:
We used laboratory-based data from the Third Affiliated Hospital of Zunyi Medical College, Zunyi, China to assess the epidemiology of the HFMD caused by enteroviruses between January 2012 and November 2014. Real-time polymerase chain reaction was used to determine human enteroviruses from a total of 12313 probable cases enrolled in this retrospective study. All analyses were stratified by enterovirus serotype, gender, and age.
Results:
Virological results were available for 12313 cases of probable HFMD. A total of 5750 cases were positive for viral detection, and the positive rates of infection caused by other enteroviruses was 46.7%, EV71 9%, and CVA16 4.7%. During the study period there was a substantial increase in the occurrence of HFMD. Most of the HFMD patients (87.4%) were aged 0-59 months (median 24; range 0-59). Males showed a higher HFMD prevalence rate (62.4%) than females (37.6%).
Conclusion:
Enterovirus infection remains an important public health problem and other entroviruses are emerging as the major causative agent of the HFMD in Zunyi, China.
Hand, foot, and mouth disease (HFMD) is a common viral infectious disease in China, with rates especially high in children under 5 years of age.1-4 Hand, foot, and mouth disease is caused by various enteroviruses, and enterovirus 71 (EV71) and Coxsackie virus A16 (CVA16) have been reported to be the main causative agents of this disease.1,4 This self-limiting disease can be complicated by fatal neurological and systemic complications, which are commonly responsible for the death.5 In addition, the significant increase in HFMD cases is a threat to the public prevention and therapy of this disease.1 The HFMD is a nationally notifiable disease in China. Previous epidemiology evidence before the year of 2012 has shown that EV71 and CVA16 are the most common enteroviruses responsible for HFMD. However, in a report by Lu and coworkers,2 the Coxsackie A virus 6 was predominant in southern China. Over time, it is possible that the circulating pattern of enteroviruses may differ from the pattern observed several years ago. Knowledge of the changing characteristics of the epidemic HFMD and monitoring of the trends of virus transmission will greatly improve our strategies to control and prevent this disease. There is a lack of comprehensive epidemiology evidence of recent enterovirus infections. The aim of this study is to present updated epidemic evidence of this disease in Zunyi, China. All analyses were stratified by enterovirus serotype, age, and gender.
Methods
Zunyi, located on latitude 27º42′ north and longitude 106°55′ east belongs to the Guizhou Province of China, and has a population of approximately 8 million people. It can be divided into 15 districts, with a total land area of 30762 square kilometers. We included probable cases of HFMD between January 2012 and November 2014 in Zunyi, China. A total of 12313 probable cases were enrolled in this retrospective study. The HFMD case data was extracted from the laboratory information system. The Third Affiliated Hospital of Zunyi Medical College, Zunyi, China is the primary official hospital approved to accept HFMD patients during an HFMD outbreak in Zunyi. No work with human subjects was directly involved in this work, because samples were tested for enterovirus serotype by real-time polymerase chain reaction (PCR) in clinical practice. Permission to conduct the research was granted by the Third Affiliated Hospital of Zunyi Medical College. This work was approved by the Ethics Committee of the Third Affiliated Hospital of Zunyi Medical College.
Case definitions
The HFMD was diagnosed based on the guidebook provided by the Ministry of Health of China (version 2009), in which the terms of disease, the criteria of clinical manifestations and laboratory evidence are clearly described.4 A probable case of HFMD was defined as illness in a patient with papular or vesiclar rash on hands, feet, mouth, or buttocks, with or without fever.1 Patients with these manifestations were subjected to viral detection. In this report, a confirmed case was considered if a probable patient has a laboratory evidence of enterovirus infection detected by real-time PCR. Cases were reported to the Chinese Center for Disease Control and Prevention at the time of diagnosis. Most patients with these manifestations were regarded as outpatients. Patients were hospitalized if they had signs or symptoms indicating a more serious illness. These included high fever (temperature higher than 38°C), vomiting, tachypnea, and indications of neurologic complications (encephalitis, aseptic meningitis, and so forth) or cardiopulmonary complications (pulmonary edema, pulmonary hemorrhage, or myocarditis).6
Collection and testing of specimens
We used laboratory-based data from the laboratory information system to measure disease caused by HFMD between January 2012 and November 2014. Throat swabs collected from outpatients and inpatients were the only sample sources. Specimens were shipped following the instructions of the Ministry of Health of China.
Ribonucleic acid (RNA) isolation and real time PCR. The methods for detecting cases of HFMD did not change during the study period. Viral RNA was extracted with available commercial kits (Da An Gene Co. Ltd, Guangzhou, China) as per the manufacturer’s protocols. We tested RNA from each sample with specific primers and probes that targeted panenterovirus, EV71, and CVA16. Testing was carried out in biosafety level 2 facilities. Five microliters of extracted RNA were subjected to reverse transcription (RT) and real time PCR as per the manufacturer’s protocols7 (Da An Gene Co. Ltd, Guangzhou, China). Of note, reverse transcription and real-time amplification was carried out in one tube according to the manufacturer’s instruction. We classified test results into 4 groups according to the manufacturer’s instruction: EV71 positive, CVA16 positive, panenterovirus, or enterovirus negative.
Data analysis
Numeration data were described by positive example and rate, and then analyzed with use of the x2 test. All analyses were carried out using Microsoft Excel (Microsoft 2007, need complete details).
Results
Cases
Between January 2012 and November 2014, the Third Affiliated Hospital admitted a total of 12313 probable cases of HFMD. Figure 1 shows a substantial increase in the annual number of confirmed cases of HFMD in Zunyi since 2012. The monthly distribution showed that the numbers of HFMD cases differed significantly by month (Figure 2). In the year of 2012, beginning with a handful of cases, the number of HFMD cases increased significantly, and the number peaks at 244 cases in June. A total of 634 cases were reported between May 1 and July 31, during the first wave of the epidemic. The second wave occurred from October to December in 2012, and included 261 cases. The peak started slightly earlier in March and lasted for a longer period of time in 2013 than in 2012. In the year 2013, a total of 1412 cases were reported between March 1 and July 31 during the first wave of the epidemic, which accounted for 80.5% (1412/1754) of the total HFMD cases. In 2013, a second wave occurred from October 1 to Decenber 31, albeit to a small degree. Similar to the epidemic in 2013, the first wave occurred between March and July in 2014, and the number of reported HFMD cases during this period accounted for 76.3% (2251/2952) of the reported cases up to November 11, 2014. A smaller peak is likely to occur in October or November in 2014 if the data are available for the coming one and a half months.
Figure 1.
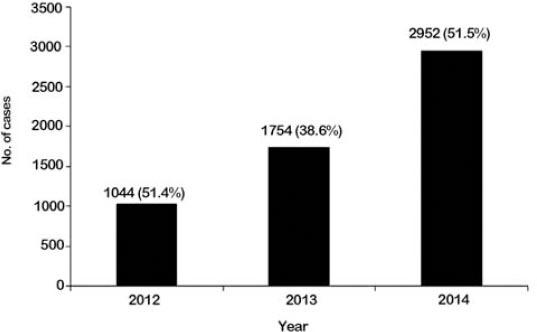
The annual number of confirmed cases of hand, foot, and mouth disease in Zunyi, China from January 1, 2012 to November 11, 2014. Figures in brackets refer to percentage of confirmed cases in the corresponding year.
Figure 2.
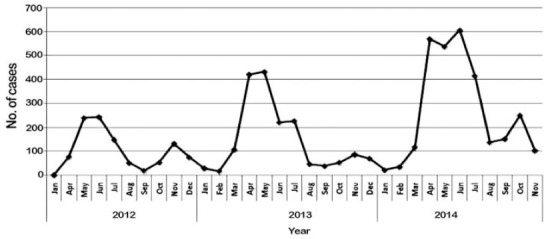
Monthly distribution of hand, foot, and mouth disease in Zunyi, China from January 1, 2012 to November 11, 2014.
Gender-specific HFMD cases infected with enteroviruses in Zunyi
Of 5750 HFMD patients, 3590 were males and 2160 were females (Figure 3). There were significant differences between the prevalence of HFMD in males and females. The prevalence of HFMD cases in males was 62.4%, which was significantly higher than females (37.6%) (p=0.0078 by the x2 test), indicating that the HFMD is more common in males than females.
Figure 3.
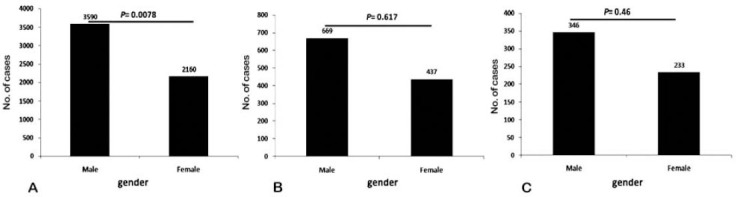
The prevalence of hand, foot, and mouth disease according to gender in Zunyi, China from January 1, 2012 to November 11, 2014. A) panenterovirus, B) EV71, and C) CVA16.
Age distribution of HFMD cases in Zunyi
When the ages of patients were taken into consideration, most of the HFMD patients (87.4%) were aged 0-59 months (Figure 4). Lower numbers of HFMD cases were observed in the age group >59 months (12.6%). The number of HFMD cases decreased as age increased, except for the age group <12 months. Most of those hospitalized, 883 of 980 (90.1%), were younger than 5 years. The incidence of HFMD varied greatly with age, with highest rates in children aged 12 months to 2 years (Figure 4).
Figure 4.
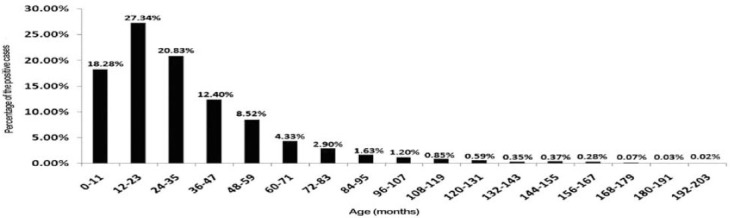
Age distribution of hand, foot, and mouth disease cases with a range of 12 months in Zunyi, China from January 1, 2012 to November 11, 2014.
Overall distribution of the causative agents of HFMD in Zunyi
Between January 2012 and November 2014, enteroviruses were obtained from 5750 patients, with the greatest number in 2014. We found that other enteroviruses predominated in laboratory-confirmed cases. Cases due to other enteroviruses strains increased by 2-fold, from 565 in 2012, to 1581 in 2013, and continued to increase in 2014 (Figure 5). The overall rate of EV71 decreased from 33.3% in 2012, to 20% in 2014. Similar decreases were found for CVA16 infection (16% in 2012, to 13% in 2014).
Figure 5.
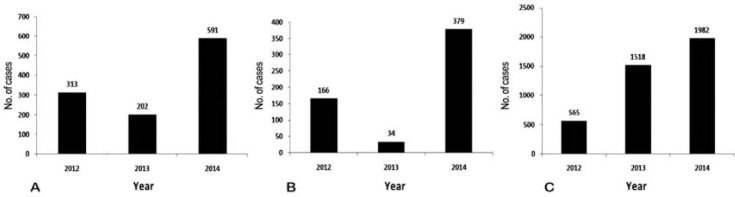
Overall distribution of the causative agents of hand, foot, and mouth disease in Zunyi, China from January 1, 2012 to November 11, 2014. A) EV71 B) CVA16, and C) others.
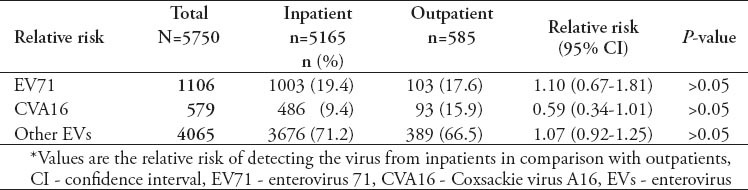
Table 1 shows the relative risk of enterovirus detected from outpatients and inpatients who were suspected of having uncomplicated or severe enterovirus infection. The frequency of EV71, CVA16, or other enteroviruses did not vary significantly between outpatients and inpatients (p>0.05 by the x2 test). The relative risks of EV71 and other enteroviruses were higher among inpatients than outpatients, but not statistically significant (p>0.05 by the x2 test; Table 1). In addition, there was a trend for CVA16 to have a higher risk among outpatients than inpatients, although it was not statistically significant (p>0.05 by the x2 test; Table 1). Nevertheless, these data suggest in addition to EV71, a trend toward a higher prevalence of other enteroviruses among severe patients.
Table 1.
Relative risk of enterovirus detected from inpatients and outpatients, from January 2012 to November 2014 in Zunyi, China.
Discussion
China is the most serious epidemic area of hand, foot, and mouth disease, and, in the years before 2012, EV71/CVA16 were the primary pathogens of HFMD among young children in China.1 It has been reported that most HFMD cases (86.5%) were caused by EV71/CVA16 in Shanghai from 2009-2010,4 and the percentages of EV71/CVA16 were also very high in Guangdong at 91.5%,8 and in Shandong at 98.5% (67/68) in the year of 2009.9 However, the percentage of EV71/CVA16 infected cases reduced to 70.7% in Shanghai from 2010-2011,10 and a similar reduction was observed in the Guangdong area, where EV71/CVA16 only accounted for 25.5% of the new enterovirus infections in 2013 (January-August).2 Consistent with their reports, our data shows that the percentage of EV71/CVA16 is reduced to 13.5% (236/1754) in Zunyi in 2013. Thus, the present work expands our knowledge on the changing epidemiology of enterovirus serotypes, which will help to fine-tune our strategies to control HFMD.
Vaccination is an attractive public heath strategy to control enterovirus infections. It has been reported that some formulations, including formalin-inactivated EV71 (FI-EV71) and bivalent FI-EV71/FI-CVA16 formulations, were protective against their target strains in animal models or human clinical trials.11,12 However, according to the present data, it seems that the current formulations have a very limited coverage of enteroviruses, and suggest that further work on vaccine development is needed. Consistent with previous data,1,4 the study population showed a high prevalence of HFMD in the young population, especially in children younger than 5 years (Figure 4) and in the warmer seasons, such as late spring and early summer (Figure 2). Age and season are therefore, important factors that must be considered in the prevention and control of HFMD transmission. It has been reported that EV71 infection is associated with severe complications, which have a higher mortality rate.13 Our study confirms previous results showing higher risk for EV71 infection and the circulation of EV71 and CVA16 in this area.6,14 Importantly, this study shows the progressive increase in the incidence of other enteroviruses in populations, especially in populations aged 0-59 months. The reasons for the higher incidence rate of other enteroviruses than that of the EV71 are currently not clear, and further detailed studies are needed to explore these apparent variations in other enteroviruses incidence rates. Nevertheless, this finding indicates that it is necessary to re-estimate HFMD prevalence in populations before the introduction of human enterovirus vaccination.
Study limitations
First, there is one and a half months missing in 2014, while the number of the cases is significantly increased compared with that in 2013. Secondly, it was because very few samples were tested for enteroviruses at the early stage of the testing that the data is missing in February and March 2012. Another major limitation of the current research is that we did not determine which serotype of the other enteroviruses is becoming predominant in this area, for example, serotype Coxsackie A virus 6 has been found to be predominant in southern China.2 Further studies are needed to identify the non-typed serotypes of the enteroviruses in future.
In conclusion, in the last 3 years, other enteroviruses account for nearly 50% of the HFMD cases, and the rate is still on the increase.
Footnotes
Illustrations, Figures, Photographs.
Four copies of all figures or photographs should be included with the submitted manuscript. Figures submitted electronically should be in JPEG or TIFF format with a 300 dpi minimum resolution and in grayscale or CMYK (not RGB). Printed submissions should be on high-contrast glossy paper, and must be unmounted and untrimmed, with a preferred size between 4 × 5 inches and 5 × 7 inches (10 × 13 cm and 13 × 18 cm). The figure number, name of first author and an arrow indicating “top” should be typed on a gummed label and affixed to the back of each illustration. If arrows are used these should appear in a different color to the background color. Titles and detailed explanations belong in the legends, which should be submitted on a separate sheet, and not on the illustrations themselves. Written informed consent for publication must accompany any photograph in which the subject can be identified. Written copyright permission, from the publishers, must accompany any illustration that has been previously published. Photographs will be accepted at the discretion of the Editorial Board.
References
- 1.Xing W, Liao Q, Viboud C, Zhang J, Sun J, Wu JT, et al. Hand, foot, and mouth disease in China, 2008–12: an epidemiological study. Lancet Infect Dis. 2014;14:308–318. doi: 10.1016/S1473-3099(13)70342-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu J, Zeng H, Zheng H, Yi L, Guo X, Liu L, et al. Hand, foot and mouth disease in Guangdong, China, in 2013: new trends in the continuing epidemic. Clin Microbiol Infect. 2014;20:442–445. doi: 10.1111/1469-0691.12468. [DOI] [PubMed] [Google Scholar]
- 3.Yip CC, Lau SK, Lo JY, Chan KH, Woo PC, Yuen KY. Genetic characterization of EV71 isolates from 2004 to 2010 reveals predominance and persistent circulation of the newly proposed genotype D and recent emergence of a distinct lineage of subgenotype C2 in Hong Kong. Virol J. 2013;10:222. doi: 10.1186/1743-422X-10-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yan XF, Gao S, Xia JF, Ye R, Yu H, Long JE. Epidemic characteristics of hand, foot, and mouth disease in Shanghai from 2009 to 2010: Enterovirus 71 subgenotype C4 as the primary causative agent and a high incidence of mixed infections with coxsackievirus A16. Scand J Infect Dis. 2012;44:297–305. doi: 10.3109/00365548.2011.634433. [DOI] [PubMed] [Google Scholar]
- 5.Solomon T, Lewthwaite P, Perera D, Cardosa MJ, McMinn P, Ooi MH. Virology, epidemiology, pathogenesis, and control of enterovirus 71. Lancet Infect Dis. 2010;10:778–790. doi: 10.1016/S1473-3099(10)70194-8. [DOI] [PubMed] [Google Scholar]
- 6.Chang LY. Enterovirus 71 in Taiwan. Pediatr Neonatol. 2008;49:103–112. doi: 10.1016/S1875-9572(08)60023-6. [DOI] [PubMed] [Google Scholar]
- 7.Wang YR, Sun LL, Xiao WL, Chen LY, Wang XF, Pan DM. Epidemiology and clinical characteristics of hand foot, and mouth disease in a Shenzhen sentinel hospital from 2009 to 2011. BMC Infect Dis. 2013;13:539–544. doi: 10.1186/1471-2334-13-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De W, Changwen K, Wei L, Monagin C, Jin Y, Cong M, et al. A large outbreak of hand, foot, and mouth disease caused by EV71 and CAV16 in Guangdong, China, 2009. Arch Virol. 2011;156:945–953. doi: 10.1007/s00705-011-0929-8. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y, Tan XJ, Wang HY, Yan DM, Zhu SL, Wang DY, et al. An outbreak of hand, foot, and mouth disease associated with subgenotype C4 of human enterovirus 71 in Shandong, China. J Clin Virol. 2009;44:262–267. doi: 10.1016/j.jcv.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Xu M, Su L, Cao L, Zhong H, Dong N, Xu J. Enterovirus genotypes causing hand foot and mouth disease in Shanghai, China: a molecular epidemiological analysis. BMC Infect Dis. 2013;13:489. doi: 10.1186/1471-2334-13-489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kung YA, Hung CT, Liu YC, Shih SR. Update on the development of enterovirus 71 vaccines. Expert Opin Biol Ther. 2014;14:1455–1464. doi: 10.1517/14712598.2014.935330. [DOI] [PubMed] [Google Scholar]
- 12.Ku Z, Liu Q, Ye X, Cai Y, Wang X, Shi J, et al. A virus-like particle based bivalent vaccine confers dual protection against enterovirus 71 and coxsackievirus A16 infections in mice. Vaccine. 2014;32:4296–4303. doi: 10.1016/j.vaccine.2014.06.025. [DOI] [PubMed] [Google Scholar]
- 13.Wang X, Zhu C, Bao W, Zhao K, Niu J, Yu X-F, et al. Characterization of Full-Length Enterovirus 71 Strains from severe and mild disease patients in Northeastern China. PloS One. 2012;7:e32405. doi: 10.1371/journal.pone.0032405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yan Y, Guo J, Zhou JZ, Tang GP, Wang DM. [Analysis on molecular epidemiological features of enterovirus type 71 in Guizhou Province, 2008-2011] Bing Du Xue Bao. 2013;29:176–179. Chinese. [PubMed] [Google Scholar]


