Abstract
Background
Evidence suggests that recent and projected future investments in percutaneous coronary intervention (PCI) programs at U.S. hospitals fail to increase access to timely reperfusion for patients with ST segment elevation myocardial infarction (STEMI).
Methods and Results
We set out to estimate the annual number and costs of new PCI programs in U.S. hospitals from 2004–2008, and to identify the characteristics of hospitals, neighborhoods and states where new PCI programs have been introduced. We estimated a discrete-time hazard model to measure the influence of these characteristics on a hospital’s decision to introduce a new PCI program. In 2008, 1739 U.S. hospitals were capable of performing PCI, a relative increase of 16.5% (251 hospitals) over 2004. The percent of the U.S. population with projected access to timely PCI grew by 1.8%. New PCI programs were more likely to be introduced in areas that already had a PCI program with more competition for market share, near populations with higher rates of private insurance, in states that had weak or no regulation of new cardiac catheterization labs, and in wealthier and larger hospitals.
Conclusions
Our data show that new PCI programs were systematically duplicative of existing programs and did not help patients gain access to timely PCI. The total cost of recent U.S. investments in new PCI programs is large and of questionable value for patients.
Keywords: percutaneous coronary intervention, catheterization, ST-segment elevation myocardial infarction, mapping, angioplasty
Background
For patients with ST segment elevation myocardial infarction (STEMI), primary percutaneous coronary intervention (PCI) improves survival and reduces serious complications1 if it can be delivered with minimal reperfusion-related delay.2, 3 Approximately 80% of the U.S. population lives within driving distance of timely PCI4 but fewer than half of patients with STEMI get access to PCI in an emergency.5
There is widespread debate about the potential of voluntary STEMI regional plans to improve utilization of PCI among patients with STEMI6–11 and a variety of such voluntary agreements have been implemented and evaluated.12–15 As a backdrop to regionalization, individual hospitals have acted unilaterally by introducing new PCI at a robust pace in every state since 2001. In recent work, we have shown that historical4 and projected future16 independent investments in new PCI programs do not help patients gain timely access to the procedure. Others have shown that emergent and elective utilization of PCI has remained flat since 2001,17 suggesting that new programs are not helping to increase access to the procedure. This is the first analysis using longitudinal data to assess whether new PCI programs duplicate existing ones, and to identify the factors associated with a hospital’s decision to introduce a new PCI program.
Methods
In previous work, we validated use of American Hospital Association (AHA) Annual Survey data for use in creating annual inventories of the number of U.S. hospitals that can perform PCI emergently.4 For this analysis, we combined annual AHA survey data from 2004 through 2008 with 2000 Census data, and with American Health Planning Association (AHPA) annual directories of State Certificate of Need Programs from 2004–2008 in order to (1) estimate change over time in the number of PCI programs offered by U.S. hospitals, (2) estimate change over time in population access to timely PCI, and (3) assess the hospital-, neighborhood-, and state-level factors that are associated with the introduction of a PCI program where one did not exist before.
Study Data
To meet our inclusion criteria, a hospital had to provide acute care to the U.S. adult (over age 18) population. Government facilities, hospital units within an institution, psychiatric and drug dependency hospitals, long term care facilities, and children’s hospitals were excluded from the analysis. We began our analysis in 2004, to coincide with the first year the AHA survey asked hospitals to specify if a lab was used for adult interventional care. Prior to 2004, hospitals were asked about ownership of cardiac catheterization labs of any type, not distinguishing interventional from diagnostic labs. We judged hospitals as having PCI capability prior to 2004 only if they reported both owning a catheterization lab and offering angioplasty as a service.
Hospital-level characteristics were collected from the AHA survey. Independent variables included measures of hospital size, inpatient and outpatient volume, teaching status, accreditations, and ownership of other advanced medical technologies. Hospital size was measured by number of hospital beds, staffing (physician and dentist FTEs), and expenditures (the sum of payroll and non-payroll expenses excluding bad debt). Hospital volumes were measured with several variables, including the ratio of outpatient to inpatient revenue, total surgical operations, total emergency department visits, and total non-emergency outpatient visits. A hospital was considered a teaching hospital if it reported at least one of the following (1) residency training approval by Accreditation Council for Graduate Medical Education, (2) medical school affiliation reported to AMA, (3) membership on the Council of Teaching Hospitals of the Association of American Medical Colleges. We defined hospitals as meeting a high accreditation status if they met at least three of the following four accreditations: (1) JACHO, (2) Hospital-controlled professional nursing school reported by National League for Nursing, (3) Blue Cross contracting or participating, (4) Medicare certification by the U.S. Department of Health and Human Services (DHHS). Hospitals were considered “high tech” if they reported ownership of at least 2 of the following technologies: (1) Positron Emission Tomography (PET), (2) Multi-slice Computed Tomography (MSCT), (3) Single-photon Emission Computed Tomography (SPECT), and (4) radiation therapy. To further adjust for the effects of hospital size, several variables were standardized to 100 beds: total hospital expenditures, FTE physicians and dentists, total surgical operations, emergency room (ER) visits, and non-emergency outpatient visits. Several skewed variable distributions were transformed on the natural log scale.
Area and state characteristics were estimated by aggregating selected variables from the Census within uniquely estimated neighborhood boundaries for every hospital in the U.S., as described below (Model 2). Census variables included area estimates of gender, age, race, income, and foreign birth. To facilitate comparison, these variables were standardized to a z-distribution; we report effects that are associated with a one standard deviation change in each of these demographic characteristics. State-by-State Certificate of Need (CON) policy data were collected from American Health Planning Association (AHPA) annual directories.18 We specified states with no program as the reference category against states with programs that did not require review of catheterization labs (class 2) and states with programs that did require review of catheterization labs (class 3). The CON variable was allowed to vary over time and was lagged two years to account for time to develop a program and report its appearance to the AHA.
The competitive environment was estimated with two measures: a design variable to indicate the presence of another PCI lab in the neighborhood surrounding the hospital (duplication of PCI); and a modified Herfindahl-Hirschman Index (HHI), a measure combining the market shares of all of the sellers in a marketplace (concentration of PCI).19 We modeled HHI as the sum of squares of each hospital’s share of the total adjusted average daily hospital census within a neighborhood.20
Model 1. The number and total costs of new PCI programs
We used AHA data to identify hospitals in all 50 states and the District of Columbia that were capable of performing emergent PCI each year from 2004–2008 (Table 1). All hospitals were uniquely identified through their AHA identification number and located within a geographic information system (GIS) using latitude and longitude coordinates. Using longitudinal data we identified new programs at individual hospitals. We imputed missing observations of PCI capability during the study period by carrying the last observation forward if PCI capability was in place at any time during 1994–2007 and by carrying the most recent observation backward if a hospital reported no PCI capability in 2004–2008. To track change over time in the number of PCI programs, we estimated both relative and absolute change in the number of new PCI programs for each year after 2004, taking into account hospitals that were lost to follow-up due to closures, mergers, and survey non-response.
Table 1.
Change in Number of and Access to PCI Programs (Models 1 and 2)
| Region | Statistic | 2004 | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|---|---|
| U.S. | Eligible hospitals (N) | 4544 | 4614 | 4675 | 4629 | 4686 |
| Hospitals with PCI (N) | 1524 | 1603 | 1673 | 1697 | 1739 | |
| Hospitals with PCI (%) | 33.5 | 34.7 | 35.8 | 36.7 | 37.1 | |
| Hospitals with new PCI (N) | --- | 84 | 69 | 52 | 46 | |
| Annual growth (%) | --- | 5.5 | 4.3 | 3.1 | 2.7 | |
| Total growth (%) | --- | --- | --- | --- | 16.5 | |
| Pop. within 1 hour drive to any hospital (%) | 94.4 | 94.5 | 94.6 | 94.4 | 94.6 | |
| Pop. within 1 hour drive to PCI hospital (%) | 79.1 | 79.7 | 80.3 | 80.5 | 80.9 | |
| Pop. with PCI as closest hospital within 1 hour drive (%) | 52.3 | 54.2 | 55.5 | 56.5 | 57.4 | |
| Median (IQR) estimated elapsed time from 911 call to closest PCI hospital within 1 hour (mins.) | 26.1 (21.5, 34.6) | 25.9 (21.4, 34.2) | 25.7 (21.3, 34.1) | 25.7 (21.3, 34) | 25.7 (21.2, 33.8) | |
|
| ||||||
| Midwest | Eligible hospitals (N) | 1347 | 1376 | 1374 | 1334 | 1381 |
| Hospitals with PCI (N) | 389 | 420 | 433 | 437 | 459 | |
| Hospitals with PCI (%) | 28.9 | 30.5 | 31.5 | 32.8 | 33.2 | |
| Hospitals with new PCI (N) | --- | 29 | 17 | 15 | 13 | |
| Annual growth (%) | --- | 7.5 | 4.0 | 3.5 | 3.0 | |
| Total growth (%) | --- | --- | --- | --- | 19.0 | |
| Pop. within 1 hour drive to any hospital (%) | 95.4 | 95.5 | 95.5 | 94.7 | 95.5 | |
| Pop. within 1 hour drive to PCI hospital (%) | 75.2 | 76.6 | 76.8 | 77.0 | 77.6 | |
| Pop. with PCI as closest hospital within 1 hour drive (%) | 54.0 | 57.2 | 59.4 | 60.7 | 60.8 | |
| Median (IQR) estimated elapsed time from 911 call to closest PCI hospital within 1 hour (mins.) | 25.6 (21.1, 34.8) | 25.4 (21, 34.1) | 25.3 (20.9, 34) | 25.3 (20.9, 33.9) | 25.2 (20.9, 33.5) | |
|
| ||||||
| Northeast | Eligible hospitals (N) | 626 | 616 | 614 | 613 | 602 |
| Hospitals with PCI (N) | 230 | 240 | 246 | 255 | 259 | |
| Hospitals with PCI (%) | 36.7 | 39.0 | 40.1 | 41.6 | 43.0 | |
| Hospitals with new PCI (N) | --- | 11 | 8 | 9 | 7 | |
| Annual growth (%) | --- | 4.8 | 3.3 | 3.7 | 2.7 | |
| Total growth (%) | --- | --- | --- | --- | 15.2 | |
| Pop. within 1 hour drive to any hospital (%) | 97.8 | 97.9 | 97.9 | 97.9 | 97.8 | |
| Pop. within 1 hour drive to PCI hospital (%) | 87.4 | 87.4 | 87.5 | 88.0 | 88.5 | |
| Pop. with PCI as closest hospital within 1 hour drive (%) | 44.6 | 48.0 | 50.1 | 52.5 | 55.2 | |
| Median (IQR) estimated elapsed time from 911 call to closest PCI hospital within 1 hour (mins.) | 25.6 (20.8, 34.4) | 25.2 (20.6, 34.1) | 24.8 (20.3, 34) | 24.7 (20.3, 34) | 24.7 (20.2, 33.9) | |
|
| ||||||
| South | Eligible hospitals (N) | 1774 | 1794 | 1820 | 1807 | 1816 |
| Hospitals with PCI (N) | 595 | 613 | 655 | 664 | 675 | |
| Hospitals with PCI (%) | 33.5 | 34.2 | 36.0 | 36.7 | 37.2 | |
| Hospitals with new PCI (N) | --- | 29 | 39 | 20 | 19 | |
| Annual growth (%) | --- | 4.9 | 6.4 | 3.1 | 2.9 | |
| Total growth (%) | --- | --- | --- | --- | 18.0 | |
| Pop. within 1 hour drive to any hospital (%) | 93.3 | 93.3 | 93.6 | 93.4 | 93.5 | |
| Pop. within 1 hour drive to PCI hospital (%) | 74.4 | 74.9 | 76.3 | 76.5 | 76.8 | |
| Pop. with PCI as closest hospital within 1 hour drive (%) | 50.9 | 51.5 | 54.0 | 54.8 | 56.0 | |
| Median (IQR) estimated elapsed time from 911 call to closest PCI hospital within 1 hour (mins.) | 27.5 (22.3, 37.3) | 27.5 (22.3, 37.1) | 27.3 (22.2, 36.8) | 27.4 (22.3, 36.6) | 27.3 (22.2, 36.4) | |
|
| ||||||
| West | Eligible hospitals (N) | 797 | 828 | 867 | 875 | 887 |
| Hospitals with PCI (N) | 310 | 330 | 339 | 341 | 346 | |
| Hospitals with PCI (%) | 38.9 | 39.9 | 39.1 | 39.0 | 39.0 | |
| Hospitals with new PCI (N) | --- | 15 | 5 | 8 | 7 | |
| Annual growth (%) | --- | 4.8 | 1.5 | 2.4 | 2.1 | |
| Total growth (%) | --- | --- | --- | --- | 11.3 | |
| Pop. within 1 hour drive to any hospital (%) | 92.2 | 92.3 | 92.6 | 92.4 | 92.6 | |
| Pop. within 1 hour drive to PCI hospital (%) | 83.3 | 83.8 | 83.9 | 84.0 | 84.2 | |
| Pop. with PCI as closest hospital within 1 hour drive (%) | 59.5 | 60.9 | 58.5 | 58.5 | 58.2 | |
| Median (IQR) estimated elapsed time from 911 call to closest PCI hospital within 1 hour (mins.) | 25.4 (21.6, 31.6) | 25.1 (21.5, 31.1) | 25 (21.4, 30.9) | 25 (21.4, 30.9) | 25 (21.4, 30.7) | |
We updated a previously developed framework for estimating the construction, medical equipment and operations and costs of introducing a new PCI program21 to 2008 U.S. dollars, using the National Income and Product Accounts (NIPA) GDP deflator.22 The introduction of a new PCI program may be made in hospitals with and without existing cardiac surgery programs, but access to on-site or nearby (via transfer) cardiac surgery back-up is recommended or required in most places. Hospitals without onsite or nearby back-up surgery may therefore have to invest in that service along with the opening of a new PCI program. To estimate a lower and upper bounds for the cost of new PCI programs to the US healthcare system over our study period, we multiplied the unit cost for a new program developed with and without existing surgical back-up.
Model 2. Access to PCI
To assess change in access to PCI, we estimated annual proportions of the population over the age of 18 living within a sixty minute drive of every PCI hospital (Table 1). To do this, we followed methods described in previous work on drive times to U.S. hospitals.23–26 We defined a “neighborhood” specific to every hospital in the U.S., defined as the area covered by a 60-minute drive time to the hospital from neighboring census tracts. Drive times were estimated using road network and speed limit data from ESRI’s ArcGIS StreetMap dataset with the Network Analyst extension.27 Extra time was added to account for dispatch of the EMS vehicle (1.4 minutes for urban and suburban tracts and 2.9 minutes for rural tracts), time from EMS depot to scene (total time was multiplied by a constant of 1.6, 1.5, or 1.4 for urban, suburban, or rural tracts, respectively) and time spent on scene (13.5 minutes for urban and suburban tracts and 15.1 minutes for rural tracts). These constants were derived in a meta-analysis of empirically determined pre-hospital care times for trauma.28
The population of a census tract was considered to have access to PCI if its centroid – the geographic location that represents the mean center of a polygon – lay within the hospital’s neighborhood boundary. Populations in tracts covered by multiple hospitals were counted once to avoid duplication. We estimated annual and total change in the potential reach of PCI programs across the U.S., the four Census Regions, 50 states and the District of Columbia.
Model 3. Hospital-, neighborhood-, and state-level factors associated with new PCI programs
To assess the hospital-, neighborhood-, and state-level factors that are associated with the decision to adopt PCI, we estimated a series of discrete-time hazard models on hospitals that did and did not adopt PCI after 2004 (Table 2). Hospital-level covariates were time-varying and lagged two years to account for elapsed time from the decision to adopt PCI and the appearance of a lab in the AHA survey. In the event that a new hospital entered the dataset, current year values were used in place of nonexistent lagged data. Univariate models were used to identify candidate covariates from AHA-, Census-, and AHPA-derived variables. Independent variables that were moderately strongly associated (p<0.10) with new PCI adoption in univariate models were selected for inclusion in the initial multivariate models.
Table 2.
Factors Associated with New PCI Programs (Model 3)
| Model 3.1 Duplication Obs = 11293 |
Model 3.2 Concentration Obs N = 10919 |
|||
|---|---|---|---|---|
| HR | 95% CL | HR | 95% CL | |
| Year | 0.83 | (0.74, 0.94) ** | 0.85 | (0.75, 0.95) ** |
| HOSPITAL-LEVEL | ||||
| Ratio of outpatient to inpatient revenue † | 0.78 | (0.67, 0.93) ** | 0.70 | (0.59, 0.85) *** |
| Total hospital expenses, $ †‡ | 2.13 | (1.70, 2.64) *** | 2.17 | (1.73, 2.68) *** |
| FTE physicians and dentists, n †‡ | 0.91 | (0.83, 0.99) * | 0.91 | (0.84, 0.99) * |
| Hospital Beds, n † | 2.48 | (2.13, 2.89) *** | 2.37 | (2.03, 2.77) *** |
| Total surgical operations, n †‡ | 1.07 | (0.96, 1.22) | 1.07 | (0.95, 1.22) |
| ER visits, n †‡ | 1.06 | (0.98, 1.17) | 1.09 | (0.98, 1.23) |
| Other outpatient visits, n †‡ | 0.89 | (0.84, 0.95) *** | 0.90 | (0.85, 0.97) ** |
| Accreditation, (Ref: low) | 1.50 | (1.05, 2.19) * | 1.39 | (0.97, 2.04) |
| Part of a hospital system, (yes vs. no) | 1.19 | (0.87, 1.66) | 1.16 | (0.85, 1.61) |
| Teaching hospital, (Ref: no) | 0.73 | (0.51, 1.03) | 0.75 | (0.52, 1.06) |
| Ownership of advanced technology, (Ref: low) | 1.40 | (1.03, 1.92) * | 1.41 | (1.03, 1.94) * |
| New hospital, (Ref: no) | 13.06 | (8.62, 19.43) *** | 12.81 | (8.43, 19.13) *** |
| NEIGHBORHOOD-LEVEL | ||||
| PCI hospital in neighborhood, (Ref: no) | 1.48 | (1.05, 2.10) * | --- | --- |
| HHI§ | --- | --- | 0.80 | (0.65, 0.98) * |
| Foreign born, percent of neighborhood § | 0.71 | (0.59, 0.84) *** | 0.70 | (0.58, 0.83) *** |
| > 65 years old, percent of neighborhood § | 0.71 | (0.57, 0.88) ** | 0.71 | (0.57, 0.88) ** |
| < 2 X FPL, percent of neighborhood § | 1.10 | (0.92, 1.29) | 1.09 | (0.91, 1.28) |
| Male, percent of neighborhood § | 0.94 | (0.76, 1.12) | 0.95 | (0.76, 1.14) |
| Non-Hispanic White, percent of neighborhood § | 0.96 | (0.76, 1.23) | 0.95 | (0.75, 1.22) |
| STATE-LEVEL | ||||
| CON (Ref: States with no CON program) | ||||
| CON State without cath lab review | 1.19 | (0.81, 1.74) | 1.21 | (0.83, 1.77) |
| CON State with cath lab review | 0.60 | (0.42, 0.85) ** | 0.57 | (0.40, 0.82) ** |
Log transformed; hazard is expressed as the association of doubling in the predictor in the original scale
Standardized to 100 beds
Normalized to z-score
p-value < 0.05,
p-value < 0.01,
p-value < 0.001
All variables are time varying and lagged two years except census data and new hospital indicator. Demographic variables come from the 2000 US Census.
We estimated two models with alternative measures of neighborhood competition. In model 3.1, we measured duplication of PCI with a time-varying and two-year lagged indicator for the presence of another PCI program within the hospital’s neighborhood (Duplication Model). In model 3.2, we measured concentration of market share with a time-varying and two-year lagged modified HHI (Concentration Model). We assumed proportional hazards and estimated three sequential equations for each model, with hospital covariates alone, hospital + neighborhood covariates, and hospital + neighborhood + state covariates. We assessed deviations from the assumption of proportional hazards by graphing the hazard function over time and by testing the significance of independent variable interactions with time. All statistical analyses were completed with SAS version 9.2 (SAS Institute, Cary, NC).
Results
Model 1 (Table 1) revealed a substantial growth in the number of hospitals that introduced a new PCI program between 2004 and 2008. In 2004, 1,524 (33.5%) of 4,544 acute care hospitals in the 50 states and the District of Columbia were capable of performing adult interventional PCI. Four years later, 1,739 (37.1%) of 4,686 acute care hospitals were capable of performing the procedure. After accounting for hospital closures and mergers, this represented 251 new interventional PCI programs and a 16.5% total growth in the number of PCI capable hospitals. Both the relative and absolute annual rates of growth in PCI capability declined over time from a high of 5.5% relative growth in 2005 (absolute increase of 84 hospitals or 1.8%) to a low of 2.7% in 2008 (absolute increase of 46 or 1.0%) and averaged 3.9% relative annual growth over the four years.
Our estimate of the 2008 per-program cost of introducing a new PCI program was $7,810,892 if back-up for surgical revascularization already existed on-site and $16,410,201 if it did not. The total cost for 251 new PCI programs under these two scenarios would therefore be more than $1.9B if all 251 hospitals already had cardiac surgery programs in place and $4.1B if none of them did. This calculation suggests the total cost of new PCI programs during our study period was $2–4 Billion.
Model 2 (Table 1) showed that access to PCI grew by a small margin over the period, from 79.1% of the population in 2004 to 80.9% in 2008. Access to PCI-capable hospitals varied by region and these relationships did not change substantially over time. Access was highest in the Northeast (87.4% in 2004 and 88.5% in 2008) and lowest in the South (74.4% in 2004 and 76.8% in 2008). Access to PCI also varied by state (data not shown). More than 90% of the population in eight states and the District of Columbia had 60 minute access to primary PCI in 2008, including California (91.1%), Connecticut (93.6%), Delaware (91.7%), Florida (91.6%), Maryland (92.5%), Massachusetts (94.6%), New Jersey (96.0%), Rhode Island (96.3%) and Washington DC (100.0%). Less than 50% of the population in seven states had 60 minute access to the procedure in 2008, including North Dakota (48.9%), South Dakota (44.6%), Vermont (38.3%), West Virginia (46.4%), Alaska (44.3%), Montana (45.3 %) and Wyoming (30.5%). Mississippi had the biggest percent change in access to PCI over the 5 year period, growing from 42.0% of the population in 2004 to 59.2% in 2008, representing a relative rate increase of 40.9%. This was achieved through the expansion of PCI to 14 hospitals that did not offer the procedure in 2004, a relative increase of 140%.
Of populations living within a maximum of 60 minutes from a PCI capable hospital, the estimated elapsed time from 9-1-1 call to arrival at the closest of those hospitals decreased from a national median of 26.1 minutes in 2004 (inter-quartile range [IQR] 21.5 to 34.6) to 25.7 minutes in 2008 (IQR 21.2 to 33.8), a drop of 24 seconds for the typical patient. The median drive time also varied by location in 2004, from a low of 21–23 minutes in Illinois, Washington DC, and Wyoming to a high of 33–35 minutes in Missouri and Vermont. This measure did not change by more than 2 minutes over the four-year follow-up in any state except Missouri, where it dropped from 33 to 29 minutes.
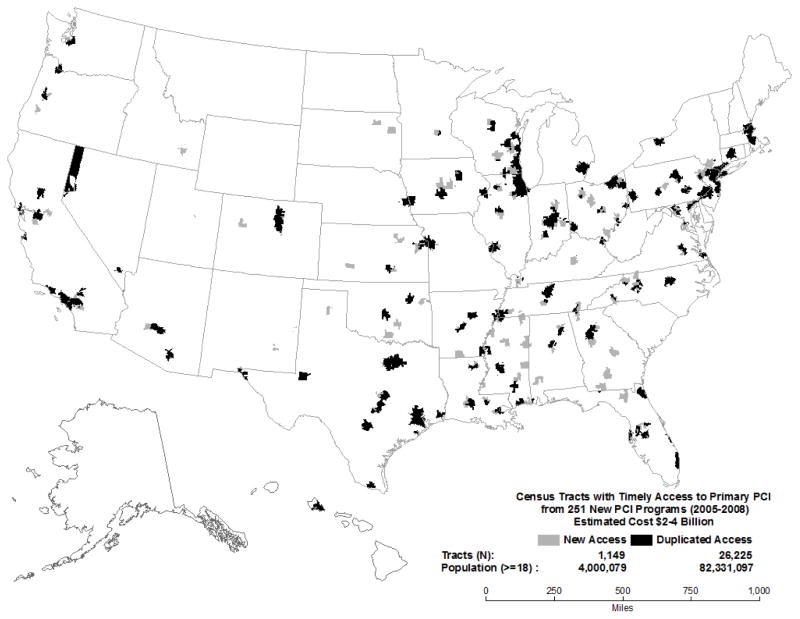
Model 3 (Table 2) demonstrated that several factors are associated with the decision to introduce a new PCI program. Hospitals were more likely to adopt PCI if they were newly opened, larger (i.e., had higher expenditures and more hospital beds), owned other expensive medical technology, and if PCI was already offered in the neighborhood. By far, the strongest influence on PCI adoption was its inclusion as part of an entirely new hospital, which increased the hazard approximately 13-fold in a year. Hospitals with twice the average annual expenditure of other non-PCI hospitals had more than a two-fold increased risk of adoption each year. Similarly, having twice the average number of beds than other non-PCI hospitals increased the annual risk of adoption two-fold. Ownership of other expensive medical technology was associated with a 40% increased yearly risk of adopting PCI, and the prior existence of another PCI lab in the neighborhood increased the chances of adoption annually by 50%. Figure 1 depicts duplicated and newly served census tracts within sixty-minutes of new PCI programs after 2004.
Figure 1. Timely Access to Primary PCI from 251 New PCI Programs (2005–2008).
This map illustrates sixty-minute drive times surrounding 251 PCI programs at U.S. hospitals that were newly introduced in 2005–2008. Black-shaded areas depict Census tracts that already had timely access to PCI in 2004 and for which the new program represented duplication. Grey-shaded areas depict Census tracts that did not have timely access to PCI in 2004 and for which the new PCI program represented new access.
Hospitals were less likely to adopt PCI if they had a higher volume of outpatient services (higher outpatient/inpatient revenue and more non-emergency outpatient visits), if they operated in a more competitive market, in a neighborhood with a higher percentage of foreign born and elderly residents, and in a state that maintained laws requiring automatic review of new catheterization labs. Having twice the average ratio of outpatient to inpatient revenue of other non-PCI hospitals in a year reduced the risk of adopting PCI by 30% while having twice the average number of outpatient visits reduced the risk by approximately 10%. One standard deviation above the mean percent of foreign born or elderly residents in a hospital’s neighborhood was associated with a decreased risk of adoption each year by 30%. One standard deviation above mean HHI reduced the annual risk of adoption by 20%. Teaching hospitals trended toward a lower risk of adopting PCI. Emergency room and surgical volumes were not associated with adoption of PCI, nor were area gender, income or percent of the population that was of non-Hispanic white race.
Operating in a state that maintained CON with automatic review of catheterization labs reduced the risk of PCI adoption by approximately 40%. We ran sub analyses to explore this effect in more detail. We interacted CON and our duplication measure to see if this effect was modified in areas without duplication, but the interaction was non-significant. We also assessed whether CON had any effect on times to treatment and access to care. The median estimated elapsed time from 911 to closest hospital declined by 0.3 minutes in no CON states, by 0.3 minutes in CON states without automatic review and by 0.8 minutes in CON states with automatic review. These elapsed time reductions amount to 18, 18, and 48 seconds, respectively, not long enough to change outcomes in patients with STEMI. However, we did find a potentially substantial effect of CON with automatic review on access to PCI. In no-CON states, access to PCI was extended to 1.5% of the population and the population living closest to PCI grew by 1.8%. In states maintaining CON without automatic review, these figures were 2.2 and 3.7%, respectively. In states maintaining CON with automatic review, they were 2.0 and 8.3%. Automatic review of catheterization labs seemed to result in a substantial increase to the population whose closest hospital could perform PCI.
Discussion
New PCI programs from 2004 to 2008 were systematically targeted to neighborhoods that were already served by existing programs, where competition for patients was high, and where they did not improve timely access for patients with STEMI. This finding elaborates on results from previous work on PCI program adoption4 and is consistent with the findings of a similar study on new cardiac surgery (CABG) programs in the U.S.29
Hospital investments in PCI from 2004 to 2008 continued at a fast but slowing pace and have been expensive. During the study period, 251 new programs were introduced in the US. In the last two years of our analysis 52 and 46 new programs opened up, respectively. Every 50 new PCI programs costs an estimated $400–800 Million, representing a sizable fixed cost that presumably redounds to increased insurance premiums, Medicare and Medicaid program costs, and patients’ out-of-pocket costs.
Our analysis shows that, on average, recent large investments in new PCI programs have been of low value for patient health because they did not lead to increased access or decreased treatment times. This is true not only for emergent PCI, the focus of our study, but also for elective PCI. If adoption through 2008 was meant to increase access to elective procedures, it has not succeeded: elective procedure rates have also been flat since at least 2001, 17 when approximately 563 fewer programs were in place.24 In this era of flat utilization, furthermore, systematic duplication can only reduce average hospital PCI volumes, a trend that could result in lower procedure quality and worse outcomes for patients with coronary artery disease. Hospital leaders and other stakeholders may hope that every new program will improve patient health, but quite the opposite may now be happening after introduction of PCI. Future introductions of this service should be assessed in this light.
There are important caveats to our findings. First, in regions with low baseline rates of access to the procedure in 2004, new programs in 2005 and beyond did improve access for patients with STEMI. This was the case in Mississippi, where access to the procedure was low in the baseline year and grew substantially after new PCI programs were introduced in follow-up years. This may also have been the case in Missouri, where median projected transport times dropped by 4 minutes over the four year follow-up. This suggests that there may be a role for new PCI programs in underserved areas. Second, the pace of investment in new PCI programs is slowing over time. This suggests that there is an upper limit to the introduction of new PCI programs, and many regions of the U.S. may be approaching that limit.
At least three types of health system strategies are available around the U.S. to increase access to PCI for patients with STEMI while restraining duplicative investment:
Voluntary interventions
One class of strategies is the development of voluntary STEMI systems of care in local communities or in states.14, 30 Known at STEMI Systems or STEMI Regional Plans, these may be defined as the systematic, iterative assessment and implementation of voluntary agreements between hospitals and emergency medical service systems that are designed to improve access to timely PCI. The largest such program in the U.S., the North Carolina RACE protocol, has been successful at establishing inter-hospital agreements and have shown benefit for patients with coronary artery disease (CAD).31 Other plans have been implemented elsewhere and have shown promising results.15
Market-based interventions
Market interventions such as payment reform may also help to address duplicative investments in PCI. Our results show that PCI investments are declining over time and may soon approach zero; therefore, the prime opportunity for targeted payment reform in this procedure may have passed as many as 10 years ago.4, 17 There is evidence, however, of continued robust investment in PCI. If investments continue while utilization of the procedure remains flat, payment for these procedures may be reduced potentially, to discourage future investments without reducing access to the procedure. Other candidates for this kind of analysis and reform may include interventions in robotics, lasers, nuclear medicine and radiology.
Regulatory interventions
Health systems interventions do not have to be voluntary or market-based. Twenty seven states in the U.S. are equipped with regulatory programs that can be used to compel a formal review of hospitals that wish to open new interventional catheterization labs.18 Our analysis showed that hospitals in states with robust CON programs were 40% less likely introduce a new PCI program in any given year, suggesting that this policy mechanism can restrain diffusion of interventional catheterization labs. Of note, automatic review was the only non-voluntary regulation that seemed to have an inhibitory effect on the introduction of new PCI programs. Other CON mechanisms, such as review of major medical equipment (MME) and capital expenditures above specified thresholds, appeared to have no effect. Further work is needed to establish whether this review mechanism works to restrain low-value diffusion in other medical technologies.
Our findings and those from studies of other technology-intensive medicine also suggest a new priority for health services research: an urgent need to track and assess the value obtained from health system investments in medical technology. Rapid change in medical technology has been a chief suspect in the escalation of U.S. health expenditures for decades, but its value for patient and population health has been unclear. Health technology assessments32 and economic research33, 34 have sought to address the role of technology in patient and national outcomes, respectively, but the relationship between change in medical technology over time and outcomes in hospitals, accountable care organizations, and other health systems is poorly understood. Better information and methods are needed to assist decision makers in these settings plan for capital investments, regional partnerships, service-line offerings and other critical health services decisions. Recent advances in spatial statistics, data collection and computing power have spurred novel methods to describe changes over time in the availability, utilization, outcomes and costs of medical technology in cardiac care, imaging, cancer, surgery, trauma, burns, stroke and other clinical domains.23–26, 28, 29, 35–42 Health services researchers could make strides in our understanding of the effects of medical technology change in health systems, but a special focus is needed on this theme.
The AHA Annual Survey offers a comprehensive source of information on U.S. hospitals and their capabilities, but it is subject to the usual limitations of self-reported survey data, including problems with non-response and misclassification. To address a small amount of missing data in our outcome variable, we used a widely accepted imputation procedure, allowing us to infer the non-existence of PCI labs in hospitals that later reported not owning one and the continued existence of a PCI lab in hospitals that previously reported owning one. Some survey data may also suffer from misclassification. In past research, we have validated AHA self reports of PCI capability against hospital utilization data, finding a high rate of congruence between the two data sources.4
In summary, our data show that new PCI programs in the four years after 2004 were systematically duplicative of existing programs and did not help patients gain access to timely PCI. The total cost of recent U.S. investments in new PCI programs is large and of questionable value for patients. We recommend three policy options that may help to improve patient access to timely PCI and restrain duplicative investments in PCI programs. We also recommend an emerging priority for health services research, to track and assess medical technology change in health systems.
Acknowledgments
The authors wish to thank Joseph Newhouse, PhD, and Benjamin Cook, PhD, both of Harvard University, for reviewing and commenting on a version of the manuscript that was presented at the 2011 Congress of the International Health Economics Association in Toronto, Canada. James M. Gaylor, BA, of Boston University School of Medicine, also read and commented on an early version of the manuscript.
Funding Sources
Dr. Concannon was supported by the Agency for Healthcare Research and Quality (AHRQ K01 HS017726) and by the Tufts Medical Center Research Fund. Mr. Nelson was supported by the Tufts Medical Center Research Fund. Drs. Kent and Griffith were supported by the National Center for Research Resources (UL1 RR025752) and the National Center for Advancing Translational Sciences (UL1 TR000073), NIH. The content is solely the responsibility of the authors and does not necessarily represent the official views of AHRQ or NIH.
Footnotes
Conflict of Interest Disclosures
None.
Other Disclosures
Dr. Concannon had primary responsibility for designing the research, overseeing data collection and analysis, interpreting model results, and writing the manuscript. Mr. Nelson had responsibility for managing data collection and analysis, interpreting model results, and drafting the manuscript. Drs. Kent and Griffith had responsibility for data analysis, interpreting model results and drafting the manuscript.
References
- 1.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 2.Kent DM, Ruthazer R, Griffith JL, Beshansky JR, Grines CL, Aversano T, Concannon TW, Zalenski RJ, Selker HP. Comparison of mortality benefit of immediate thrombolytic therapy versus delayed primary angioplasty for acute myocardial infarction. Am J Cardiol. 2007;99:1384–8. doi: 10.1016/j.amjcard.2006.12.068. [DOI] [PubMed] [Google Scholar]
- 3.Nallamothu BK, Bates ER. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: is timing (almost) everything? Am J Cardiol. 2003;92:824–6. doi: 10.1016/s0002-9149(03)00891-9. [DOI] [PubMed] [Google Scholar]
- 4.Concannon TW, Nelson J, Goetz J, Griffith JL. A percutaneous coronary intervention lab in every hospital? Circ Cardiovasc Qual Outcomes. 2012;5:14–20. doi: 10.1161/CIRCOUTCOMES.111.963868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nallamothu BK, Blaney ME, Morris SM, Parsons LS, Miller DP, Canto JG, Barron HV, Krumholz HM. Acute reperfusion therapy in ST-elevation myocardial infarction from 1994–2003. Am J Med. 2007;120:693.e1–e8. doi: 10.1016/j.amjmed.2007.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Topol EJ, Kereiakes DJ. Regionalization of care for acute ischemic heart disease: a call for specialized centers. Circulation. 2003;107:1463–6. doi: 10.1161/01.cir.0000063680.45780.a0. [DOI] [PubMed] [Google Scholar]
- 7.Rathore SS, Epstein AJ, Volpp KGM, Krumholz HM. Regionalization of Care for Acute Coronary Syndromes: More Evidence Is Needed. JAMA. 2005;293:1383–87. doi: 10.1001/jama.293.11.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jacobs AK. Regionalized care for patients with ST-elevation myocardial infarction: it’s closer than you think. Circulation. 2006;113:1159–61. doi: 10.1161/CIRCULATIONAHA.105.610345. [DOI] [PubMed] [Google Scholar]
- 9.Hannan EL. Evaluating and improving the quality of care for acute myocardial infarction: can regionalization help? JAMA. 2006;295:2177–9. doi: 10.1001/jama.295.18.2177. [DOI] [PubMed] [Google Scholar]
- 10.Henry TD, Sharkey SW, Burke MN, Chavez IJ, Graham KJ, Henry CR, Lips DL, Madison JD, Menssen KM, Mooney MR, Newell MC, Pedersen WR, Poulose AK, Traverse JH, Unger BT, Wang YL, Larson DM. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–8. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 11.Pottenger BC, Diercks DB, Bhatt DL. Regionalization of care for ST-segment elevation myocardial infarction: is it too soon? Ann Em Med. 2008;52:677–85. doi: 10.1016/j.annemergmed.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 12.Ting HH, Rihal CS, Gersh BJ, Haro LH, Bjerke CM, Lennon RJ, Lim C, Bresnahan JF, Jaffe AS, Holmes DR, Bell MR. Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: The Mayo Clinic STEMI Protocol. Circulation. 2007;116:729–36. doi: 10.1161/CIRCULATIONAHA.107.699934. [DOI] [PubMed] [Google Scholar]
- 13.Glickman SW, Granger CB, Ou FS, O’Brien S, Lytle BL, Cairns CB, Mears G, Hoekstra JW, Garvey JL, Peterson ED, Jollis JG. Impact of a statewide ST-segment-elevation myocardial infarction regionalization program on treatment times for women, minorities, and the elderly. Circ Cardiovasc Qual Outcomes. 2010;3:514–21. doi: 10.1161/CIRCOUTCOMES.109.917112. [DOI] [PubMed] [Google Scholar]
- 14.Jollis JG, Granger CB, Henry TD, Antman EM, Berger PB, Moyer PH, Pratt FD, Rokos IC, Acuna AR, Roettig ML, Jacobs AK. Systems of care for ST-segment-elevation myocardial infarction: a report from the American Heart Association’s Mission: Lifeline. Circ Cardiovasc Qual Outcomes. 2012;5:423–8. doi: 10.1161/CIRCOUTCOMES.111.964668. [DOI] [PubMed] [Google Scholar]
- 15.Henry TD. From Concept to Reality: A decade of progress in regional ST-elevation myocardial infarction systems. Circulation. 2012;126:166–168. doi: 10.1161/CIRCULATIONAHA.112.114140. [DOI] [PubMed] [Google Scholar]
- 16.Concannon TW, Kent DM, Normand SL, Newhouse JP, Griffith JL, Cohen JT, Beshansky JR, Wong JB, Aversano T, Selker HP. Comparative effectiveness of STEMI regionalization strategies. Circ Cardiovasc Qual Outcomes. 2010;3:506–513. doi: 10.1161/CIRCOUTCOMES.109.908541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001–2008. JAMA. 2011;305:1769–76. doi: 10.1001/jama.2011.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Directory of State Certificate of Need Programs and Health Planning Agencies. 19 American Health Planning Association; 2008. [Google Scholar]
- 19.Herfindahl–Hirschman Index. Department of Justice; 2012. [Accessed October 12, 2012]. Available at: http://www.justice.gov/atr/public/guidelines/hhi.html. [Google Scholar]
- 20.The AHA Annual Survey Database. American Hospital Association; 2011. [Accessed October 12, 2012]. Available at: http://www.ahadata.com/ahadata/html/AHASurvey.html. [Google Scholar]
- 21.Lieu TA, Lundstrom RJ, Ray GT, Fireman BH, Gurley RJ, Parmley WW. Initial cost of primary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 996(28):882–9. doi: 10.1016/s0735-1097(96)00237-9. [DOI] [PubMed] [Google Scholar]
- 22.Newhouse JP. The Baxter Foundation Prize address: measuring medical prices and understanding their effects. The Journal of Health Administration Education. 1988;7:19–26. [PubMed] [Google Scholar]
- 23.Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, Blatt AJ, ReVelle CS. Access to trauma centers in the United States. JAMA. 2005;293:2626–33. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 24.Nallamothu BK, Bates ER, Wang Y, Bradley EH, Krumholz HM. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: implications for prehospital rtiage of patients with ST-elevation myocardial infarction. Circulation. 2006;113:1189–95. doi: 10.1161/CIRCULATIONAHA.105.596346. [DOI] [PubMed] [Google Scholar]
- 25.Klein MB, Kramer CB, Nelson J, Rivara FP, Gibran NS, Concannon T. Geographic access to burn center hospitals. JAMA. 2009;302:1774–81. doi: 10.1001/jama.2009.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nance ML, Carr BG, Branas CC. Access to pediatric trauma care in the United States. Arch Pediatr Adolesc Med. 2009;163:512–8. doi: 10.1001/archpediatrics.2009.65. [DOI] [PubMed] [Google Scholar]
- 27.ArcMap. Version 9.3. Redlands, California: 2009. [Google Scholar]
- 28.Carr BG, Caplan JM, Pryor JP, Branas CC. A meta-analysis of prehospital care times for trauma. Prehospital Emergency Care. 2006;10:198–206. doi: 10.1080/10903120500541324. [DOI] [PubMed] [Google Scholar]
- 29.Lucas FL, Siewers A, Goodman DC, Wang D, Wennberg DE. New cardiac surgery programs established from 1993 to 2004 led to little increased access, substantial duplication of services. Health Aff. 2011;30:1569–1574. doi: 10.1377/hlthaff.2010.0210. [DOI] [PubMed] [Google Scholar]
- 30.American Heart Association. Mission: Lifeline. [Accessed July 28, 2010];Web Page. 2010 Available at: http://www.heart.org/HEARTORG/HealthcareProfessional/Mission-Lifeline-Home-Page_UCM_305495_SubHomePage.jsp.
- 31.Jollis JG, Al-Khalidi HR, Monk L, Roettig ML, Garvey JL, Aluko AO, Wilson BH, Applegate RJ, Mears G, Corbett CC, Granger CB. Expansion of a regional ST-segment elevation myocardial infarction system to an entire state. Circulation. 2012;126:189–195. doi: 10.1161/CIRCULATIONAHA.111.068049. [DOI] [PubMed] [Google Scholar]
- 32.Drummond MF, Schwartz JS, Jonsson B, Luce BR, Neumann PJ, Siebert U, Sullivan SD. Key principles for the improved conduct of health technology assessments for resource allocation decisions. Int J Tech Assessment in Health Care. 2008;24:244–58. doi: 10.1017/S0266462308080343. [DOI] [PubMed] [Google Scholar]
- 33.Cutler DM, McClellan M. Is technological change in medicine worth it? Health Aff. 2001;20:11–29. doi: 10.1377/hlthaff.20.5.11. [DOI] [PubMed] [Google Scholar]
- 34.Philipson T, Eber M, Lakdawalla DN, Corral M, Conti R, Goldman DP. An analysis of whether higher health care spending in the United States versus Europe is “worth it” in the case of cancer. Health Aff. 2012;31:667–75. doi: 10.1377/hlthaff.2011.1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Buckley JW, Bates ER, Nallamothu BK. Primary percutaneous coronary intervention expansion to hospitals without on-site cardiac surgery in Michigan: a geographic information systems analysis. Am Heart J. 2008;155:668–72. doi: 10.1016/j.ahj.2007.10.051. [DOI] [PubMed] [Google Scholar]
- 36.Concannon TW, Kent DM, Normand SL, Newhouse JP, Griffith JL, Ruthazer R, Beshansky JR, Wong JB, Aversano T, Selker HP. A geospatial analysis of emergency transport and inter-hospital transfer in ST-segment elevation myocardial infarction. Am J Cardiol. 2008;101:69–74. doi: 10.1016/j.amjcard.2007.07.050. [DOI] [PubMed] [Google Scholar]
- 37.Carr BG, Branas CC, Metlay JP, Sullivan AF, Camargo CA. Access to emergency care in the United States. Health Policy and Clinical Practice. 2009;54:261–9. doi: 10.1016/j.annemergmed.2008.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dinan MA, Curtis LH, Hammill BG, Patz, Edward F, Jr, Abernethy AP, Shea AM, Schulman KA. Changes in the use and costs of diagnostic imaging among Medicare beneficiaries with cancer, 1999–2006. JAMA. 2010;303:1625–31. doi: 10.1001/jama.2010.460. [DOI] [PubMed] [Google Scholar]
- 39.Barbash GI, Glied SA. New technology and health care costs: The Case of Robot-Assisted Surgery. NEJM. 2010;363:701–4. doi: 10.1056/NEJMp1006602. [DOI] [PubMed] [Google Scholar]
- 40.Clark RA, Coffee N, Turner D, Eckert KA, van Gaans D, Wilkinson D, Stewart S, Tonkin AM. Application of geographic modeling techniques to quantify spatial access to health services before and after an acute cardiac event: The Cardiac Accessibility and Remoteness Index for Australia (ARIA) project. Circulation. 2012;125:2006–14. doi: 10.1161/CIRCULATIONAHA.111.083394. [DOI] [PubMed] [Google Scholar]
- 41.Ranasinghe I, Turnbull F, Tonkin A, Clark RA, Coffee N, Brieger D. Comparative effectiveness of population interventions to improve access to reperfusion for ST-segment elevation myocardial infarction in Australia. Circ Cardiovasc Qual Outcomes. 2012;5:429–36. doi: 10.1161/CIRCOUTCOMES.112.965111. [DOI] [PubMed] [Google Scholar]
- 42.Cram P. Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–36. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]