Abstract
Introduction:
Diuretic resistance is a common problem in congestive heart failure patients. It has been defined clinically but can be defined objectively in terms of fractional excretion of sodium (FENa).
Aim:
Aim of the study was to find out the association of FENa with prognosis of decompensated heart failure patients.
Materials and Methods:
One hundred and seventy eligible patients with a primary diagnosis of decompensated heart failure were enrolled and patients were categorized into two groups on the basis of baseline FENa- Group A (65 patients) with diuretic resistance with FENa <0.2% and Group B (105 patients) sensitive to diuretics with FENa ≥0.2%. The patients were followed-up during the hospital stay for the time taken for improvement from NYHA functional class IV to class II. They were followed telephonically at 30 days post admission for all cause mortality.
Result:
The mean time taken to improve from NYHA functional class IV to class II were 146 hours for FENa<.2% and 60 h for FENa≥0.2% (p<0.0001). There was a fair negative correlation between FENa and time taken for improvement from NYHA functional class IV to class II with correlation coefficient being -0.4842. Multiple linear regression analysis showed FENa (standardized “B” is -0.480, p<0.001) and LVEF (standardized “B” is -0.182, p=0.007) as significant predictors of time taken for improvement from NYHA functional class IV to class II. The 30 days all cause mortality was significantly associated with level of Fena (p <0.001) and was inversely proportional.
Conclusion:
CHF patients with FENa <0.2% takes longer time to recover from NYHA functional class IV to class II. 30 days all cause mortality was also significantly higher among CHF patients with FENa <0.2%.Measuring baseline FENa and regulating diuretic dose accordingly at admission to hospital may probably improve the prognosis of CHF patients.
Keywords: Diuretic resistance, FENa
Introduction
Heart failure (HF) is a common health problem. HF leads to frequent hospitalizations, a poor quality of life, and a shortened life expectancy. In the United States, >650,000 new HF cases are diagnosed annually [1]. Administration of diuretics is simple and effective for symptomatic relief of congestive heart failure (CHF) but unfortunately every third patient shows resistance to these diuretics [2]. Clinically, diuretic resistance in the edematous patient has been defined as a state in which diuretic response is diminished or lost before the therapeutic goal of relief from edema has been reached. CHF patients with diuretic resistance take longer time to improve clinically. The major causes of diuretic resistance are nonadherence with medication regimen, functional renal failure (prerenal azotemia), hyponatremia, altered diuretic pharmacokinetics (delayed intestinal absorption of oral diuretics, decreased diuretic excretion into the urine), sodium retention caused by counter regulatory mechanisms intended to reestablish the effective arterial blood volume, increased sodium reabsorption at sites in the nephron other than those inhibited by the diuretic, inadequate diuretic dose [3].
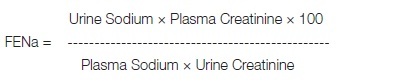
Diuretic resistance can be defined objectively in terms of fractional excretion of sodium (FENa). FENa is the fraction of the filtered sodium load that is reabsorbed by the tubules. FENa depends on sodium intake, effective intravascular volume, GFR, and intact tubular reabsorptive mechanisms [4]. In a study by H. Knauf , diuretic response of the patient depended on the pretreatment FENa. The lower the patient’s FENa, the smaller was the natriuretic response to diuretics. Those patients were diuretic resistant whose FENa was less than 0.2 percent [5]. Hence, low FENa (<0.2%) is considered as an indicator of diuretic resistance.
With this background, the present study was proposed to find out the association of FENa with prognosis of decompensated heart failure patients. The specific objective being (1) to find out the difference in mean time taken for clinical improvement from NYHA functional class IV to class II in CHF patients with diuretic resistance(FENa <0.2%) and without diuretic resistance(FENa >=0.2%). (2) To find out the difference in proportion of deaths during first 30 days of admission in CHF patients with and without diuretic resistance.
Materials and Methods
It is a hospital based observational, descriptive study. 170 eligible patients with a primary diagnosis of decompensated heart failure (ACCF/AHA HF stage C,D; NYHA functional class IV) were enrolled from ICCU, S.M.S. hospital, Jaipur. A total of 170 consecutive patients were enrolled in this study. Patients were categorised into two groups on the basis of baseline FENa- Group A with FENa <0.2% consisting of 65 patients and Group B with FENa ≥0.2% consisting of 105 patients.
Patients were evaluated with history, clinical examination, twelve lead electrocardiogram, chest X-ray PA view and trans-thoracic echocardiography. The patients underwent laboratory investigation with complete blood count, kidney function test (serum creatinine, potassium, urea and sodium levels), liver function test, lipid profile, fasting blood sugar and FENa.
Baseline FENa were calculated from lab test in spot urine sample collected before giving frusemide or at least six hours after the last dose of frusemide. Blood sample for estimation of serum sodium and creatinine were taken at the same time. FENa was calculated by the formula [6].
 |
Loop diuretic frusemide produce marked water diuresis and natriuresis in first 6 h after the intravenous dose. This is usually followed by minimal natriuresis lasting between 6 h and 24 h. So, we calculated FENa from samples taken before giving frusemide or at least six hours after its last dose.
Patients with normal left ventricular ejection fraction; mild symptoms not necessitating adding or increasing the dose of diuretics; patients with chronic kidney disease (i.e. GFR <60 ml/min/1.73 m2); and patient presenting with ACS were excluded from the study.
Glomerular filtration rate was estimated by the MDRD formula. The patients were monitored with daily weight charting, input output chart and were given a low salt (no more than 2.5 gm/day) diet. The patients were continued on anti-failure medications including angiotensin converting enzyme (ACE) inhibitors, spironolactone. Patients were started on intravenous furosemide at admission. Positive inotropic agents were started if low cardiac output signs and symptoms were present.
The patients were followed-up during the hospital stay for the time taken for improvement from NYHA functional class IV to class II. They were followed telephonically at 30 days post admission for all cause mortality.
Results
Baseline characteristics of both the groups were comparable [Table/Fig-1]. Overall, the mean time taken to improve from NYHA functional class IV to class II was four days with a minimum of two days and a maximum of 16 days. The mean time taken to improve from NYHA functional class IV to class II were 146 h for FENa<0.2% and 60 h for FENa≥0.2%, which was highly statistically significant [Table/Fig-2].
[Table/Fig-1]:
Baseline characters of both groups
| PARAMETERS | FeNa <0.2(n=65) | FeNa ≥ 0.2(n=105) | p-value |
|---|---|---|---|
| AGE (YRS) | 54.55(±15.27) | 57.6(±13.87) | 0.171 |
| MALE | 51 (78%) | 79 (75 %) | 0.768 |
| DM | 11 (17%) | 16 (15 %) | 0.939 |
| HTN | 14 (21.5 %) | 21 (20 %) | 0.963 |
| SMOKING | 33 ( 50.7%) | 55 (52 %) | 0.963 |
| CAD | 28 (43.07 %) | 45 ( 42.8%) | 0.896 |
| Serum Na+ (meq/l) | 136.9±8.1 | 138.1±5.9 | 0.28 |
| Serum Hb(g/dl) | 12.58±1.93 | 12.6±1.83 | 0.95 |
| Mean LVEF% | 22.6 ±5.51 | 24.36 ±6.00 | 0.0569 |
DM- Diabetes mellitus; HTN- Hypertension; CAD- Coronary artery disease
[Table/Fig-2]:
Comparison of time taken to improve from NYHA IV→II between groups
| PARAMETERS | FeNa <0.2(n=65) | FeNa ≥ 0.2(n=105) | p-value |
|---|---|---|---|
| Time taken to improve from NYHA IV to II (Hours) | 146.62±61.34 | 60.58±21.17 | <0.0001 |
Thirty days all cause mortality showed that there were two mortalities (1.9%) in Fena≥0.2 and 13 mortalities (20%) in Fena <0.2. The 30 days all cause mortality is significantly associated with level of FENA (p <0.001) and is inversely proportional [Table/Fig-3].
[Table/Fig-3]:
Association of 30 days mortality with FENa (p <0.001)
| FENa status | Mortality status | Total | |
|---|---|---|---|
| Death | Alive | ||
| <0.02 | 13 | 52 | 65 |
| >0.02 | 2 | 103 | 105 |
| Total | 15 | 155 | 170 |
Overall, FENa results came out with a mean value of 0.507. There is a fair negative correlation between FENa and time taken for improvement from NYHA functional class IV to class II [Table/Fig-4].
[Table/Fig-4]:
![[Table/Fig-4]:](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/9466/4437091/bc2e474df281/jcdr-9-OC01-g001.jpg)
Correlation between FeNa versus Time Taken to improve from NYHA IV→ II
As a way to identify the independent predictor(s) of time taken for improvement from NYHA functional class IV to class II, a multiple linear regression analysis was done. Using the enter method, a 2significant model (F5,164 =13.054, p< 0.001, Adjusted R2 =0.263 ) was obtained for prediction of time taken for improvement from NYHA functional class IV to class II using FENa, Hemoglobin (Hb), LVEF, Serum Sodium, pulse rate as predictors [Table/Fig-5,6,Table/Fig-7]. Significant factors were FENa (standardized “B” is -0.480, p<0.001) and LVEF (standardized “B” is -0.182, p=0.007). FENa contributed a negative 48% change and LVEF contributed a negative 18.2% change in time taken for improvement from NYHA functional class IV to class II. Serum sodium, Hb and Pulse rate were not significant predictors in this model.
[Table/Fig-5]:
Model Summary
| Model | R | R Square | Adjusted R Square | Std. Error of the Estimate |
|---|---|---|---|---|
| 1 | .534a | .285 | .263 | 49.97523 |
a. Predictors: (Constant), pulse rate, FENA, Hemoglobin, LVEF%, S. Sodium
[Table/Fig-6]:
ANOVAb
| Model | Sum of Squares | Df | Mean Square | F | Sig. | |
|---|---|---|---|---|---|---|
| 1 | Regression | 163017.279 | 5 | 32603.456 | 13.054 | <0.001a |
| Residual | 409593.874 | 164 | 2497.524 | |||
| Total | 572611.153 | 169 |
a.Predictors: (Constant), pulse rate, FENA, Hemoglobin, LVEF %, S. sodium
b.b. Dependent Variable: Time taken to improvement from NYHA functional class IV to class II
[Table/Fig-7]:
Coefficientsa
| Model | Sum of Squares | Df | Mean Square | T | Sig. | |
|---|---|---|---|---|---|---|
| B | Std. Error | Beta | ||||
| 1 | (Constant) | 234.046 | 84.368 | 2.774 | .006 | |
| FENA | -52.492 | 7.240 | -.480 | -7.251 | <0.001 | |
| S. sodium | -.731 | .560 | -.087 | -1.305 | .194 | |
| LVEF % | -1.808 | .657 | -.182 | -2.755 | .007 | |
| Hemoglobin | -.278 | 2.063 | -.009 | -.135 | .893 | |
| pulse rate | .329 | .263 | .083 | 1.253 | .212 | |
Discussion
FENa has been used to assess the effectiveness of diuresis in heart failure in various studies. Significantly higher time taken for improvement from NYHA functional class IV to class II in CHF patients with FENa <0.2% could be due to impaired kidney function, increased sodium reabsorption by a nephron segment other than the loop of Henle, Hyponatremia, poor LVEF, Chronic and severe anemia in CHF.
Studies have shown that baseline FENa in heart failure patients before starting diuretic therapy is approximately less than 1% indicating pre-renal azotemia due to renal hypoperfusion and decreased GFR [5.7]. Decreased GFR causes decreased delivery of diuretic to its urinary site of action. This possibility was ruled out in our patient as we included only those patients whose GFR was in the normal range or only slightly reduced.
Hyponatremia is frequently associated with reduced diuretic efficacy due to diminished distal tubular sodium delivery and secondary hyperaldosteronism [3]. Callahan et al., [8], found that admissions with hyponatremia had significantly longer hospital length of stay than those admitted without hyponatremia. In our study the effect of hyponatremia on differences in mean time to improve has been ruled out as the serum sodium was comparable in both the groups.
Chronic and severe anaemia is associated with an increased likelihood of hospitalisations and an increased length of stay when hospitalised [9]. This has been ruled out in our study as haemoglobin in both groups was comparable. The most probable and possible explanation for the decreased diuretic response in our patients is that the substrate (i.e. sodium chloride) is increasingly reabsorbed by a nephron segment other than the loop of Henle. Congestive heart failure patients have reduced effective blood volume which leads to activation of at least four pathways: the sympathetic system, the renin-angiotensin-aldosterone system, the nonosmotic release of antidiuretic hormone (ADH), and the renal prostaglandin production [5]. So, even if glomerular filtration rate is normal, excretion of sodium chloride is reduced; this results in low FENa.
As regard to time taken to improve from NYHA functional class IV to II, there was a fair negative correlation with FENa with correaltion coefficeint being -0.4842.
The mean time taken to improve from NYHA IV to NYHA II was four days with a minimum of two days and a maximum of 16 d. A multiple linear regression for prediction of this time taken for improvement was done with variables that might have an influence on this time including, hemoglobin level, serum sodium level, low ejection fraction, FENa and heart rate. Significant factors were FENA (standardized “B” is -0.480, p<0.001) and LVEF (standardized “B” is -0.182, p=0.007). FENA has a negative 48% change in NYHA and LVEF has a negative 18.2% change in NYHA. S.sodium, Hb, Pulse rate was not significant predictors in this model.
Harjai et al., [10] found a significant inverse correlation between FENa and LVEF. Despite similar disease severity at admission, patients with ejection fraction <40% had significantly longer length of stay but similar in-hospital and 30-day mortality compared with patients with ejection fraction >40%. In our study overall there was a fair negative correlation with LVEF with time to recovery (correlation co-efficent being -0.182; p=0.007)but as both the group had insignificant difference in LVEF, so the contribution of decreased LVEF on prolonged time to recovery in FENa <0.2% group is ruled out. The significance of FENa level as a predictor of hospital stay was quite remarkable although it was not the only predictor of hospital stay but was certainly the most significant.
The 30 days all cause mortality was significantly associated with level of FENA (p=0.000) with mortality significantly higher in FENa <0.2% group.
Limitation
The limitation of the study was that larger number of patients is needed to detect accurate cut-off values for FENa to determine diuretic resistant patients. Also the exact cause of mortality was not known as it was enquired telephonically.
Conclusion
CHF patients with FENa <0.2% takes longer time to recover from NYHA functional class IV to class II. 30 days all cause mortality is also significantly higher among CHF patients with FENa <0.2%.
Measuring baseline FENa and regulating diuretic dose accordingly at admission to hospital may probably improve the prognosis of CHF patients.
Acknowledgement
We acknowledge the contribution of Dr Monika Rathore, Associate Professor, Department of Community Medicine, SMS Medical College, who did the statistics of this original article.
Financial or Other Competing Interests
None.
References
- [1].CW Yancy, M Jessup, B Bozkurt, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128:e240–327. doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- [2].RW Schrier. Pathogenesis of sodium and water retention in highoutput and lowoutput cardiac failure, nephrotic syndrome, cirrhosis, and pregnancy. N Engl J Med. 1988;319(16):1065–72. doi: 10.1056/NEJM198810203191606. [DOI] [PubMed] [Google Scholar]
- [3].BK Kramer, F Schweda, GA Riegger. Diuretic treatment and diuretic resistance in heart failure. Am J Med. 1999;106(1):90–96. doi: 10.1016/s0002-9343(98)00365-9. [DOI] [PubMed] [Google Scholar]
- [4].DC Brater. Diuretic resistance: mechanisms and therapeutic strategies. Cardiology. 1994;84(Suppl. 2):57–67. doi: 10.1159/000176458. [DOI] [PubMed] [Google Scholar]
- [5].H Knauf, E Mutschler. Sequential nephron blockade breaks resistance to diuretics in edematous states. J Cardiovasc Pharmacol. 1997;29(3):367–72. doi: 10.1097/00005344-199703000-00010. [DOI] [PubMed] [Google Scholar]
- [6].Brenner Barry M. 8th Edition. Philadelphia: Saunders Elsevier; 2008. Brenner and Rector’s The Kidney; Chapter 24. [Google Scholar]
- [7].MA Fifer, CR Molina, AC Quiroz, TD Giles, HC Herrmann, IR De Scheerder, et al. Hemodynamic and renal effects of atrial natriuretic peptide in congestive heart failure. Am J Cardiol. 1990;53(3):211–16. doi: 10.1016/0002-9149(90)90087-h. [DOI] [PubMed] [Google Scholar]
- [8].MA Callahan, HT Do, DW Caplan, K Yoon-Flannery. Economic impact of hyponatremia in hospitalized patients: a retrospective cohort study. J Postgrad Med. 2009;121(2):186–91. doi: 10.3810/pgm.2009.03.1991. [DOI] [PubMed] [Google Scholar]
- [9].TS Dharmarajan, A Pankratov, E Morris, S Qurashi, G Law, S Phillips, et al. Anemia: its impact on hospitalizations and length of hospital stay in nursing home and community older adults. J Am Med Dir Assoc. 2008;9(5):354–59. doi: 10.1016/j.jamda.2008.02.008. [DOI] [PubMed] [Google Scholar]
- [10].KishoreJ Harjai, Eduardo Nunez, Tansel Turgut, P Shah Mehul, J Stewart Humphrey, BS Jeff Newman, et al. The independent effects of left ventricular ejection fraction on short-term outcomes and resource utilization following hospitalization for heart failure. Clin Cardiol. 1999;22(3):184–90. doi: 10.1002/clc.4960220306. [DOI] [PMC free article] [PubMed] [Google Scholar]


