Abstract
Racism and discrimination can have significant implications for health, through complex biopsychosocial interactions. Latino groups, and particularly Puerto Ricans, are an understudied population in the United States in terms of the prevalence of discrimination and its relevance to health. Participants in our study were 45-75- year- old (N=1122) Puerto Ricans. The measures were perceived discrimination, depressive symptomatology, (CES-D), perceived stress (PSS), self-rated health, medical conditions, blood pressure, smoking and drinking behaviours, demographics. Our findings show that 36.9 per cent of participants had experienced discrimination, with men, those with more years of education, currently employed and with higher incomes being more likely to report it. Experiences of discrimination were associated with increased levels of depressive symptoms and perceived stress. When controlling for covariates, perceived discrimination was predictive of the number of medical conditions, of ever having smoked and having been a drinker, higher values of diastolic pressure. Depressive symptoms are a mediator of the effect of perceived discrimination on medical conditions, confirmed by the Sobel test: z=3.57, p < 0.001. Mediating roles of perceived stress, smoking and drinking behaviours were not confirmed. Increased depressive symptoms might be the main pathway through which perceived discrimination is associated with a greater number of medical diagnoses.
Keywords: discrimination, depressive symptoms, medical conditions, Puerto Ricans
Introduction
Discrimination and health
A growing literature suggests that discrimination may be a core factor in explaining racial and ethnic disparities in health outcomes (Harris et al. 2006, Mays et al. 2007). Increased awareness of the importance of health disparities has stimulated interest in the role that discrimination may be playing in sustaining them (Williams et al. 2003). Racism and experiences and perceptions of discrimination impact on health through multiple pathways. Williams and Collins (1995) proposed at least three ways that racism affects health. First, structurally, racism transforms socio-economic status such that socio-economic indicators are not equivalent across racial/ethnic groups. Secondly, racism restricts access to services and goods which promote health. Finally, racism and discrimination increase psychological distress which adversely affects physical and mental health status, as well as health-related behaviors (Williams and Collins 1995).
Thus, the research on health outcomes of perceived racism and discrimination often employs an explicit or implicit biopsychosocial framework, aiming to take into account multiple pathways of interaction between social context, psychological and physiological resonance, as well as mediation of these linkages by demographic, behavioural or personal characteristics, such as coping (Clark et al. 1999). In the case of discrimination, the social context includes attitudinal or behavioural phenomena which denigrate, exclude or deny equality to people because of their ethnicity. Perceived racism or discrimination is the subjective assessment and experience of this negative social context, and the subjective dimension is very important in terms of how these contexts will be responded to and will impact health (Schnittker and McLeod 2005). Perceived discrimination on the one hand might be less encompassing of structural forms of discrimination (Brondolo et al. 2003), but on the other hand might be attuned to subtler symbolic dimensions of discrimination (Clark et al. 1999). Thus, the focus on perceived discrimination is consistent with the stress and coping frameworks as applied to discrimination. Within this framework, the subjective appraisal of the extent to which the social context and events are threatening is of importance. This appraisal of threat is followed by relevant coping approaches, including behaviours which aim to solve the problem or to mitigate the experience of stress—it also elicits physiological stress responses (Dougall and Baum 2001). Social rejection and exclusion (MacDonald and Leary 2005), and threats to social relationships are phenomena to which individuals are particularly sensitive, and can have serious immediate and long-term health consequences (Miller et al. 2009, Uchino 2006). A context of social threats in the past (such as an accumulation of experiences of discrimination) can have on-going consequences for physiological and biological processes, and is an important issue to address (Miller et al. 2009).
Perhaps the most studied pathways between perceived discrimination and health are those related to mental health, as discrimination serves as a stressor, but the internalisation of discrimination can also impact on self-esteem and identity (Karlsen and Nazroo 2002, Krieger and Sidney 1996). Some of the constructs which have been used as indicators of mental health status include psychological distress, life satisfaction, depressive symptoms, major depression, anxiety and unhappiness (Williams et al. 2003). In most of these studies, experiences of discrimination are associated with poorer mental health outcomes, and higher levels of psychological distress (Araujo and Borrell 2006, David and Williams-Morris 2000 Williams et al. 2003). This association has been shown to be moderated by education, acculturation, coping, social support and religious involvement (Bierman 2006, Cardarelli et al. 2007 Noh et al. 1999, Noh and Kaspar 2003, Prelow et al. 2006).
A number of indicators of physical health have been examined in relation to discrimination; however, these findings are mixed in that there is not a consistent pattern of significant associations. These indicators include self-rated health (Finch et al. 2001, Karlsen and Nazroo 2002), chronic health conditions (Borrell et al. 2006, Finch et al. 2001, Gee et al. 2007a, Ryan et al. 2006), systolic (SBP) and diastolic blood pressure (DBP) or cardiovascular reactivity (CVR) as outcome measures (Borrell et al. 2006, Brondolo et al. 2003, Clark 2000, Din-Dzietham et al. 2004, Finch et al. 2001, Gee et al. 2007a, Guyll et al. 2001, Krieger and Sidney 1996, Ryan et al. 2006). A review of existing studies concluded that the findings are ‘quite robust’ in pointing to poorer self-rated health, and in some cases greater self-reported incidence of chronic medical conditions, among those who have experienced discrimination (Williams et al. 2003) - yet as mentioned, some studies do not find such an association (Stuber et al. 2003). As Stuber et al (2003) point out, the relationship between experiences of discrimination and physical health outcomes could have many other contributing factors and thus clear pathways are not easily identified.
Negative social experiences, including social conflict, exclusion and, specifically, discrimination, have been shown to be related to the development of and mortality from cardiovascular disease (Everson-Rose and Lewis 2005, Mays et al. 2007). There is a growing literature that addresses the importance of racism and discrimination for hypertension. This research has been, to some extent, motivated by the very high incidence of hypertension in the African-American population in the United States, some of which could be attributable to the persistence of prejudice against this group (Guyll et al. 2001, Krieger and Sidney 1996, Mays et al. 2007). Attempts to understand the relationship between discrimination and blood pressure illustrate the complexity of the mechanisms, as they show the importance of potential mediators and moderators of these relationships, such as coping style, gender, socioeconomic status and others (Brondolo et al. 2003).
Discrimination could also be a stressor that contributes to an increase in health risk behaviours such as smoking, alcohol consumption, and eating or sleeping patterns that, in turn, can have negative health consequences. These behaviours could be a way of coping with the stress, frustration and anger provoked by discriminatory experiences (Broman 2007, Chae et al. 2008, Guthrie et al. 2002, Zucker and Landry 2007).
An important gap in the literature is the limited number of studies that evaluate or compare the effects of perceived discrimination on physical and on mental health concurrently (Pavalko et al. 2003) or that delineate the mechanisms through which they can be connected (Finch et al. 2001). This paper makes such a contribution, by following several pathways which may link, in different ways, perceived discrimination to psychological distress, to health risk behaviours, to medical conditions, and to physiological indicators (blood pressure).
Latinos and perceived discrimination
In the United States, the majority of studies on racism focus on racism against African-American groups (Mays et al. 2007). There are fewer studies with other groups, such as Somali (Ellis et al. 2008), Asian refugees (Noh et al. 1999), and Asian-Americans (Gee et al. 2007b). Latino groups are an understudied population when it comes to understanding the prevalence and consequences of discrimination and particularly, its relevance to health (Gee et al. 2006). The importance of understanding the psychological and somatic impact of perceived discrimination on the Puerto Rican population stems from the unique historical, geographical and political context of Puerto Rican migration and citizenship in the United States. Specific studies about the Puerto Rican experience of discrimination are few, but those available report high incidences of discrimination. For example, a study of Puerto Rican adolescents reported that as high as 50 per cent of the participants had experienced discrimination (Araujo and Borrell 2006, Szalacha et al. 2003). These studies then conclude that the extent of discrimination faced by Latinos may be lower than for African-Americans (Araujo and Borrell 2006). However, these authors also agree that the discrimination experiences of Latinos might be underreported because of the research methods used and that because of the higher proportion of members with darker skin colour, Puerto Ricans may be exposed to discrimination experiences at a higher rate than other Latinos.
While many findings about the association between discrimination and health might be similar across minority groups, there are important associations that tend to be group specific. For example, the association between discrimination and a measure of physical health was found to be similar in direction for African Americans, African immigrants, and for Latino immigrants, but it was much weaker for the Latino immigrants (Ryan et al. 2006). Gee et al. (2006) found a similar weaker relationship between discrimination and mental health for Latinos as compared to African-Americans. These studies also find that the length of residency in the United States is an important moderating factor between experiences of discrimination and mental health among immigrants. This finding, it is argued, is largely due to the immigrant character of the Latino population. Latino groups tend to have a significant proportion of recent arrivals among them. A shorter time of exposure to the United States context implies fewer opportunities to understand and experience racial dynamics and to understand and separate racist behaviour from, for example, class distinctions. In addition, recent immigrants tend to be more likely to be located within ethnically based communities where more community resources exist, racial distinctions are not pronounced, and the opportunity to experience discrimination is more limited. While co-ethnic communities can be protective in one sense, in another sense, however, they can be segregated and disadvantaged with negative implications for health (Ahmad and Bradby 2007).
A recent publication identified 14 papers examining discrimination against the Latino population (Araujo and Borrell 2006), concluding that most of the research had addressed the issue for Mexican-American groups—only four studies included Puerto Ricans. Most of the publications examined the relevance of discrimination experienced by Latinos in the United States in relation to life chances (Araujo and Borrell 2006). Further, only a few of these publications focused on physical health or psychological symptoms (Araujo and Borrell 2006, Finch et al. 2001, Finch et al. 2000, Stuber et al. 2003).
One study by Szalacha et al. (2003) focused on discrimination and health exclusively in Puerto Rican respondents – children and adolescents - in the Boston area. They found that the prevalence of perceived discrimination was 12 per cent in the group of children, but 49 per cent for the adolescents. In both groups, discrimination (and anxiety about being faced with discrimination) was associated with depression and stress, but not with other measures of psychological wellbeing.
A longitudinal study of the consequences, among Latino adolescents, of perceiving discrimination from adults and peers found that Puerto Ricans reported significantly less discrimination (by peers) than the other Latino groups and that the psychological health of the Puerto Rican group was not as strongly negatively affected over time as it was for the other groups (Greene et al. 2006).
Stuber et al. (2003) found a relationship between perceived discrimination and the mental health of Latino respondents (Puerto Ricans, Dominican, Mexicans and others) but did not find an association between discrimination and their measure of physical health. Based on their findings, they argue that the effects of discrimination on mental health are intensified when other domains of racial and non-racially based discrimination, such as sexual orientation, gender, appearance, religion, and age, are taken into account. For example, those participants who reported experiencing discrimination in one additional domain (i.e. gender, religion) besides race, had a 23 per cent greater probability of reporting lower mental health (Stuber et al. 2003).
A study of the physical consequences of perceived discrimination for Mexicans in California (Finch et al. 2001), found a relationship with both self-rated health and chronic conditions and confirmed that depression was a crucial mediator of the pathway between perceived discrimination and health problems.
In summary, the cumulative impact of lifetime experiences of discrimination on older adults, particularly older Hispanic adults, remains inadequately examined. While interest in the role of racial and ethnic discrimination in explaining disparities in health has grown steadily, very few studies have addressed this question for the Puerto Rican population in the United States. When compared to other Latino groups in the United States, middle aged and older Puerto Ricans have a high prevalence of depressive symptoms and perceived stress, as well as chronic medical conditions, such as hypertension, diabetes, obesity, arthritis and others, (Tucker et al. 2007, Tucker et al. 2000). Thus, it is important to ascertain whether these health disparities experienced by Puerto Ricans are to some extent related to experiences of discrimination.
In accordance with the biopsychosocial framework informing our design, we hypothesise that the accumulation of lifetime experiences of discrimination could be associated with psychological distress and poorer physical health. Further, perceived discrimination may be relevant for physical health (medical conditions and hypertension) through the effects of the psychological distress it elicits, or through eliciting coping behaviours that are a health risk, such as smoking and drinking. Thus, we ask the following research questions: (1) What is the prevalence of lifetime perceived discrimination among a middle-aged and older sample of Puerto Ricans living in the Boston area? (2) What are the patterns of perceived discrimination and how do these vary by demographic indicators? (3) What is the role of perceived discrimination for their mental and physical health-- current psychological distress, chronic diseases, and health risk behaviours, such as tobacco and alcohol consumption? (4) Is the impact of perceived discrimination on physical health mediated through psychological distress and/or health risk behaviours? To clarify the last research question we tested several mediation models:
-
a)
Is the effect of lifetime perceived discrimination on medical conditions mediated through psychological distress? Is the effect of lifetime perceived discrimination on medical conditions mediated through health risk behaviours?
-
b)
Is the effect of lifetime perceived discrimination on blood pressure mediated through psychological distress? And, finally, is the effect of lifetime perceived discrimination on blood pressure mediated through health risk behaviours?
Design, recruiting and sample
Data for the analysis come from the Boston Puerto Rican Health Study (BPRHS) -- a two-wave cohort study funded by The National Institutes of Health (NIH) and being conducted by the Boston Puerto Rican Center on Health and Health Disparities. The BPRHS study, a collaboration between Tufts and Northeastern University, examines how psychosocial stress impacts on health outcomes (i.e. depression, disability, cognitive impairment) through physiological processes. Eligibility to participate in the study was limited to those who self-identified as being of Puerto Rican descent, were able to answer questions in either Spanish or English, were between the ages of 45 and 75 years, and were residents of the Boston, Massachusetts metropolitan area. We focused on the 45-to-75-year-old cohort because of interest in the timing of a series of life events and the development of a number of health outcomes over the lifecourse. Our previous research indicated a relatively high prevalence of type 2 diabetes, depression and other conditions and impairments for this age group (Tucker et al. 2000). Identified eligible individuals were only excluded if they had a serious health condition that prevented them from being able to answer questions or scored 10 or less in the Mini Mental State Examination (MMSE) indicating severe cognitive impairment.
Because of limitations in the availability of an appropriate sampling frame to identify the study population and where it resided, multiple recruitment methods were used. About 80 per cent of the sample was recruited through random selection using tract and block data from the 2000 US Census and door-to-door enumeration methods. US Census data on the distribution of Hispanics in Massachusetts allowed the identification of tracts (population for tracts ranges from 1,500 to 8,000) with at least 25 Puerto Rican adults, ages 45-75 years. Within the identified tracts, Census-defined street blocks with 10 or more Hispanics (identification of Puerto Ricans is not available at block level) were randomly selected and enumerated (through a household composition survey) door by door, for the presence of Puerto Rican adults who met the study criteria. Selected blocks were visited at least three times (in some cases up to six times) on different days of the week and time of the day with more than 17,000 doors approached. Households with at least one eligible adult were identified and the eligible adult invited to participate. Random selection was used to invite one participant in households with more than one eligible member.
In addition to random selection at the block level, a smaller subset of the sample (20.9 %) was identified through community activities in collaboration with La Alianza Hispana -- a large community agency serving the Puerto Rican and Hispanic Community and a partner in our grant application to NIH. These methods included community fairs and events (8.9 %), referrals from participants (6.1%) and calls placed by interested individuals to the study office (4.6%) as a result of having seen publicity regarding the research project. Using two types of recruitment methods allowed us not only to increase the size of the sample but to also to capture a segment of the Puerto Rican population more likely to be engaged in community events and less sedentary than those found at home.
Comparisons between those recruited through door-to-door enumeration and those recruited through community activities suggests that the latter are younger, more likely to be men, to have better education, be more acculturated, and more likely to be employed (Tucker et al. 2009). However, there were no differences by poverty status, the Body Mass Index (BMI) or the prevalence of type 2 diabetes. In all, Census tract areas from which five or more of our participants were recruited accounted for 95.8 per cent of the Puerto Rican population identified by the 2000 Census as living in the Greater Boston area. Our response rate from eligible individuals invited to participate in the study was 86.4 per cent.
The number of people in our sample was 1122 adults; the characteristics are presented in Table 1. The participants were given the choice to take the interview in English or Spanish, and the interviewers were bilingual. Two per cent of the respondents conducted the interview in English, 11 per cent in both languages, and the rest in Spanish. The interviews lasted three to four hours total and were conducted in one or two visits at the participants’ homes. Nine participants were excluded due to a low MMSE.
Table 1.
Demographic characteristics of people who have experienced discrimination based on Chi2 for the categorical variables
| Sample Characteristics | % Perceived Discrimination | Chi2 | |
|---|---|---|---|
| Sample | N = 1122 | 36.9% | |
| Gender | 4.07* | ||
| Men | 331 (29.5%) | 41.4% | |
| Women | 791 (70.5%) | 35.0% | |
| Age | 2.9 (n.s.) | ||
| 44-55 | 543 (48.5%) | 39.4% | |
| 56-65 | 386 (39.3%) | 34.5% | |
| 66-75 | 191 (18.2%) | 34.6% | |
| Education | 47.99*** | ||
| No school | 39 (3.5%) | 20.5% | |
| Up to 8th | 490 (43.8%) | 30.0% | |
| Up to 12th | 425 (38.0%) | 38.8% | |
| Some college | 122 (10.9%) | 52.5% | |
| Bachelor's | 24 (2.1%) | 66.7% | |
| Some grad | 19 (1.7%) | 73.7% | |
| Marital Status | 12.41** | ||
| Married | 357(32.0%) | 42.9% | |
| Divorced | 441 (39.5%) | 35.8% | |
| Widowed | 153 (13.7%) | 26.8% | |
| Never married | 166 (14.9%) | 36.1% | |
| Income per member of household (SES) | 13.45** | ||
| $0-5000 | 291 (27.5%) | 32.0% | |
| $5001-10,000 | 527 (49.7%) | 34.5% | |
| Over $10,000 | 242 (22.8%) | 46.3% | |
| Currently employed | 8.70** | ||
| no | 768 (77.7%) | 36.7% | |
| yes | 220 (22.3%) | 47.7% | |
| Language use | 44.10*** | ||
| Only Spanish | 398 (35.9%) | 26.9% | |
| Mostly Spanish | 437 (39.4%) | 36.6% | |
| Both the same | 203 (18.3%) | 51.7% | |
| English | 72 (6.5%) | 52.8% | |
| Years in the US | 1.02 (n.s.) | ||
| 0-10 | 61 (8.1%) | 41.0% | |
| 11-20 | 93 (12.3%) | 36.6% | |
| 21-30 | 143 (19%) | 34.3% | |
| 31-40 | 272 (36.1%) | 37.1% | |
| 41-50 | 150 (19.9%) | 36.7% | |
| Over 51 | 35 (4.6%) | 40.0% | |
p< 0.001
p < 0.01
p < 0.05
Measures
Perceived discrimination
This was assessed through four items, such as ‘Have you ever experienced discrimination as a result of your race, ethnicity or language?’ The possible responses were ‘yes’ or ‘no’. The following questions asked whether they had experienced discrimination in healthcare settings in general (without specifying the type of setting). If the response was affirmative, the respondents were then asked to clarify how often this had happened and whether it had interfered with their ability to access healthcare.
Psychological health
As the measure of depressive symptomatology we used the Centre for Epidemiological Studies Depression Scale (CES-D) (Radloff 1977). This instrument has shown good validity in older adults (Radloff 1986), as well as in Hispanics (Moscicki et al. 1987). It consists of 20 items, which ask the respondents about their mood during the past week, and includes questions about negative affect, positive affect, psychosomatic complaints and interpersonal relationships. Participants rate to what extent each item has been true for them, using a four-point Likert scale. Scores of 16-21 indicate moderate levels of depressive symptoms and scores of 22 and higher indicate possible clinically relevant depressive symptoms. The internal consistency based on the coefficient alpha for this scale was 0.91.
We also used the 14-item Spanish version of the Perceived Stress Scale (PSS) (Cohen and Williamson 1988). It is developed based on the definition of stress as a perception that events in one's life are threatening and one's resources are not adequate to cope with them. The PSS measures the extent to which respondents perceived stress in their lives over the past month.
Health status
We used several indicators of health status to delineate the potential impact of perceived discrimination. Self-rated health (SRH) was assessed through one item in a five-point Likert scale. This measure has been shown to be a reliable predictor of morbidity and mortality for the general population and for Latinos (Finch et al. 2002, Idler and Benyamini 1997).
The number of medical conditions was identified through a list of 14 diagnoses. The respondents were asked, ‘Has a doctor ever told you that you had any of the following illnesses or conditions?’ Thus, while it is a self-report measure, it asks not about symptoms, but about diagnosis confirmed by a healthcare provider. These include diabetes, hypertension, being overweight, arthritis, osteoporosis, heart attack, heart disease, stroke, respiratory disease, liver/ gallbladder, kidney, gastrointestinal, Parkinson's disease, and cancer. Diabetes and hypertension are not self-report, but based on lab and clinical measurements, as well as medications taken. Diabetes status is defined using guidelines from the American Diabetes Association (2006). Hypertension is assessed following the guidelines of the Joint National Committee on Prevention (Joint National Committee on Prevention Detection Evaluation and Treatment of High Blood Pressure 2003).We calculated the sum of the number of medical conditions diagnosed.
Questions regarding the health behaviours of smoking and alcohol consumption were adapted from the National Health and Nutrition Examination Survey. Respondents were asked whether they had ever smoked, and whether they currently smoked. They were considered as never having smoked if they had consumed fewer than 100 cigarettes in their lifetime. Respondents who had had had fewer than 12 drinks in their lifetime were considered as never having consumed alcohol. They were considered past drinkers if they had had more than 12 drinks, but had stopped drinking. For those who currently consumed alcohol, the frequency of use was assessed as moderate (1 drink per day for women and 2 drinks for men) and heavy drinking (more than 1 drink per day for women and more than 2 drinks for men).
Respondents’ blood pressure was taken six times during the interviews, twice at each of three intervals. Interviewers were trained to calibrate the automated sphygmomanometer daily and to conduct and register the blood pressure readings, which were taken on the left arm, after the respondent had been sitting for at least 15 minutes. We use the average value from the last two intervals recorded during the interview as a continuous variable.
Covariates
We collected information about the respondents’ gender, age, education, and length of residency in the United States, and employment status. We also collected information on total household income, as well as the number of people in the household. We calculated socioeconomic status (SES), defined as the total household income divided by the number of people in the household.
We used the Social and Community Support and Assistance Questionnaire, developed for the Massachusetts Hispanic Elderly Study (MAHES) (Falcon and Tucker 2000) and particularly the subscale for participation in hobbies and other such leisure activities during the past two weeks. The number of social activities was used as a covariate in most of the subsequent models.
The scale used to assess language use was adopted for use with the Puerto Rican population in the Massachusetts Hispanic Elderly Study (MAHES) (Falcon and Tucker 2000), and is based on Marin and Gamba (1996). We also use an item (with 7 sub-items) which indicates the language they use during different daily activities (watching television, reading, speaking with neighbours, etc), using a five-point scale. From these seven questions we calculated the percentage of English language use in daily activities – this variable is the `Language acculturation’ and is used as a continuous variable and covariate.
Statistical analysis
We use the SPSS statistical package and present descriptive statistics for the main variables. For bivariate analyses, we use the Chi-square test to assess the prevalence and patterns of perceived discrimination among demographic groups, as well as according to language use, years in the United States, smoking and alcohol consumption. We have also conducted analysis of the differences between respondents who report discrimination and those who do not, using the t-test. We use linear regression analysis, controlling for the covariates listed below, to estimate the association of perceived discrimination and the outcomes of depressive symptoms, perceived stress, self-rated health, number of medical conditions, systolic and diastolic blood pressure. The covariates used are gender, age, education, SES, language acculturation, and social activities. We use logistic regression analysis to estimate the association of perceived discrimination and separate medical conditions, as well as smoking and alcohol consumption.
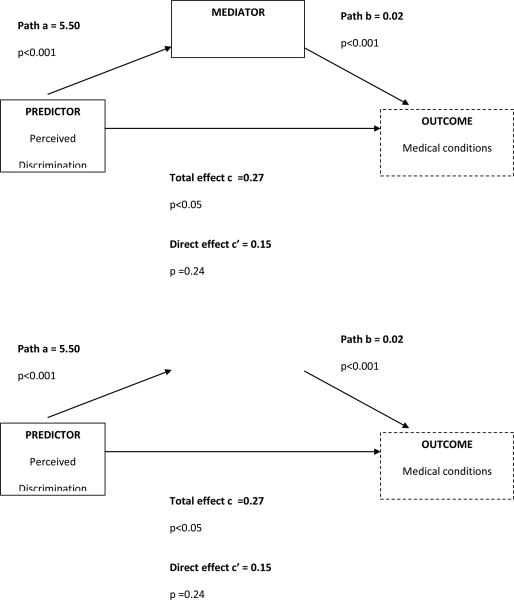
To test for mediating effects, we used the framework proposed by (Barron and Kenny 1986), and we also supplemented it with the Sobel test i(Preacher and Hayes 2004). We used the SAS macro developed by Jasti et al. (2008) as it allows for tests of mediation with both continuous and binary mediators. We ascertain whether the effect of the independent variable (perceived discrimination) on the dependent variable (physical health) is being mediated through psychological distress (depressive symptoms and perceived stress) or through health risk behaviours (smoking and alcohol consumption). The test was structured as follows: The independent variable is associated with the dependent variable through the total effect (path c), the independent variable is associated with the mediator (path a), and the mediator is associated with the dependent variable when controlling for the independent variable (path b) (Barron and Kenny 1986). Mediation is assumed if the effect of the independent variable is significantly reduced or eliminated, when including the mediator in the model (path c’) – in other words if the direct effect is less than the total effect of the independent variable on the dependent variable (c’ < c) (Figure1). All regression models controlled for the covariates listed earlier.
Figure 1.
Mediation model with perceived discrimination as predictor, medical conditions as outcome and CES-D as mediator, controlling for covariates. The B coefficients are presented, the Sobel test for this model is: z=3.57, p < 0.001.
Results
Patterns of perception of discrimination according to demographic groups
Of our sample of 1122 Puerto Rican adults, 36.9 per cent stated that they had experienced discrimination because of their ethnicity, race or language (Table 1). Data not shown indicate that one-third of those had also experienced discrimination in healthcare settings. Those who were significantly more likely to report having perceived discrimination were men, had more years of education, were currently employed and had higher incomes. Younger people were more likely to report such experiences; however, the relationship did not reach statistical significance. The percentage of people experiencing discrimination was independent of length of residency in the United States.
Respondents in our sample tended to be more ingrained in the Puerto Rican Spanish-based language culture rather than the American culture. Increased English language use in daily activities was associated with greater probability of experiencing discrimination) (Table 2). Having perceived discrimination was associated with engagement in a higher number of social activities. This suggests the possibility that increased exposure to social interaction and non-Spanish language use may bring this group into situations outside the social context of their ethnic community where experiences of discrimination may be more common (Table 2). Perceived discrimination and its association with psychological distress and physical health The average CES-D score for our sample was quite high at 19.7 (Table 2). Based on the criteria described by the authors (Radloff 1986), 41.6 per cent of the sample had no depressive symptoms, 16.1 per cent had moderate level symptoms, and 41.5 per cent had scores that placed them at risk for clinical depression. Women had higher scores on the CES-D than men (t=6.18, p <0.001). Similarly, the level of perceived stress score for our sample was also high, compared to published norms for this scale (Cohen and Williamson 1988). Women had a higher mean of perceived stress of 22.2, as compared to men, who had a mean score of 24.2 (t=3.34, p = 0.001). Experiences of discrimination were associated with increased levels of depressive symptoms and perceived stress (Table 2). In a linear regression model with the covariates, perceived discrimination preserved its independent effect on depressive symptoms and on perceived stress (Table 3).
Table 2.
Comparison (t –test) between people who have experienced discrimination and those who have not, according to psychological distress, indicators of physical health and social activities
| Sample Mean | Discrimination Mean | No Discrimination Mean | t | |
|---|---|---|---|---|
| Language acculturation | 24.25 ± 22.52 | 31.35 ± 23.45 | 20.08 ± 20.88 | 8.08*** |
| Depressive symptoms (CES-D) | 19.71 ± 12.95 | 22.03 ± 13.39 | 18.35 ± 12.50 | 4.62*** |
| Perceived stress (PSS) | 23.58 ± 9.37 | 25.18 ± 8.93 | 22.65 ± 9.50 | 4.39*** |
| Self-rated health | 2.35 ± 0.95 | 2.40 ± 0.99 | 2.32 ± 0.93 | 1.41 (n.s.) |
| Medical conditions | 3.33 ± 1.97 | 3.35 ± 1.98 | 3.32 ± 1.96 | 0.31 (n.s.) |
| Systolic BP | 135.29 ± 19.09 | 134.32 ± 18.55 | 135.86 ± 19.39 | 1.29 (n.s.) |
| Diastolic BP | 80.89 ± 10.64 | 82.04 ± 11.19 | 80.20 ± 10.25 | 2.77** |
| Number of social activities engaged | 5.82 ± 2.30 | 6.37 ± 2.37 | 5.51 ± 2.19 | 6.03*** |
p< 0.001
p < 0.01
* p < 0.05
Table 3.
Linear regression analysis with perceived discrimination as the independent variable, and depressive symptoms, perceived stress and medical conditions as dependent variables, controlling for covariates.
| Depressive symptoms CES-D | Perceived Stress PSS | Medical Conditions | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B | 95% C.I. for B | p | B | 95% C.I. for B | p | B | 95% C.I. for B | p | |
| Age | −0.09 | (−0.186 – 0.006) | 0.066 | −0.12 | (−0.187 – −0.046) | 0.001 | 0.02 | (0.009 – 0.040) | 0.002 |
| Gender | 5.22 | (3.565 – 6.869) | 0.000 | 2.48 | (1.274 – 3.692) | 0.000 | 0.79 | (0.523 – 1.051) | 0.000 |
| Education | −0.83 | (−1.802 – 0.149) | 0.097 | −0.26 | (−0.969 – 0.456) | 0.480 | −0.16 | (−0.313 – −0.002) | 0.047 |
| SES | −0.00 | (0.000 – 0.000) | 0.001 | −0.00 | (0.000 – 0.000) | 0.035 | −0.00 | (0.000 – 0.000) | 0.259 |
| Language acculturation | 0.01 | (−0.028 – 0.051) | 0.566 | 0.01 | (−0.020 – 0.037) | 0.558 | −0.01 | (−0.014 – −0.001) | 0.015 |
| Social activities | −1.19 | (−1.541 – −0.845) | 0.000 | −0.81 | (−1.063 – −0.553) | 0.000 | −0.02 | (−0.077 – 0.035) | 0.459 |
| Perceived discrimination | 5.79 | (4.199 – 7.388) | 0.000 | 3.59 | (2.421 – 4.758) | 0.000 | 0.27 | (0.018 – 0.525) | 0.036 |
Only 5.4 per cent (N=60) of respondents rated their health as excellent, 5.7 (N=64) per cent as very good, and 19.6 per cent (N=220) as good. The majority of respondents, 56.9 per cent (N=637), chose to rate their health as fair and 12.4 per cent (N=139) as poor. The mean of the self-rated health variable was 2.35 and women rated their health as being much poorer than men did (t=4.93 p < 0.001). The respondents’ self-rated health was not related to their experience of discrimination in the bivariate analysis (Table 2), nor in the linear regression model when controlling for covariates.
The number of reported medical conditions ranged from zero to 13 with a mean of 3.33 conditions. Women reported more medical conditions than men did (t= 6.82, p < 0.001). The total number of medical conditions was not related to their experience of discrimination in the bivariate analysis (Table 2). In the linear regression model, however, when controlling for the covariates, perceived discrimination was predictive of the number of medical conditions (Table 3). Of the conditions identified, 38.1 per cent of the sample had diabetes, 67.3 per cent hypertension, 38.3 per cent were overweight, 48.5 per cent arthritis, 12.3 per cent osteoporosis, 8.6 per cent heart attacks, 12.4 per cent heart disease, 3.5 per cent stroke, 37.4 per cent respiratory disease, 15.7 per cent liver/gall bladder, 10.8 per cent kidney, 29.9 per cent gastrointestinal, 0.4 per cent Parkinson's and 5.9 per cent cancer. When testing the relevance of perceived discrimination for each of the 14 medical conditions separately using binary logistic regression and the same covariates, we found that perceived discrimination is predictive of being overweight, having arthritis, respiratory disease and gastrointestinal disease.
Blood pressure readings conducted during the interviews gave mean values for the whole sample of 135 mm Hg systolic and 81 mm Hg diastolic blood pressure. There was no difference in the systolic blood pressure values for the people who had experienced discrimination compared to those who had not. However, the group that had experienced discrimination had higher values of diastolic pressure. After controlling for covariates, we found that perceived discrimination was not a significant predictor of systolic or diastolic blood pressure.
Of our sample, 44.6 per cent (N=469) had never smoked, 29.9 per cent (N=333) had smoked in the past and 25.4 per cent (N=283) were current smokers. Those who were past smokers were most likely to report experiencing discrimination (p < 0.05). Smoking behaviour was not associated with systolic or diastolic blood pressure, but past smokers reported the highest rates of medical conditions (p < 0.001), suggesting that they may reduce smoking when their health deteriorates. A binary variable of smoking (ever having smoked/ never having smoked) was constructed in order to be able to test for mediation (Jasti et al. 2008). In logistic regression analysis, controlling for covariates, perceived discrimination was associated with a higher probability of ever having smoked (Exp (B) = 1.32, p = 0.05). To explore the role of smoking behaviour further, we also tested the binary variable past smoker/ current smoker. Logistic regression analyses did not show a relationship between perceived discrimination and current smoking behaviour.
Of the sample, 28.7 per cent (N = 320) had never consumed alcohol, 29.9 per cent (N = 334) had consumed in the past and 41.4 per cent (N = 462) were current consumers. Those who were current drinkers were most likely to report experiencing discrimination (p < 0.001). Current drinkers had higher diastolic blood pressure (p < 0.001). On the other hand, those who were past drinkers reported significantly more medical conditions, and current drinkers had the fewest number of medical conditions (p < 0.001). Similar to the pattern with smoking, people may have given up alcohol when medical problems arose, yet the impact of alcohol consumption on blood pressure continued to be relevant. A binary variable for alcohol consumption (ever been a drinker/ never been a drinker) was constructed in order to be able to test for mediation (Jasti et al. 2008). In logistic regression analysis, when controlling for covariates, perceived discrimination was associated with a higher probability of ever having been a drinker (Exp (B)=1.43, p < 0.05).
Mediators of perceived discrimination on health
We tested several mediation models, first ascertaining that each model fits the criteria (Barron and Kenny 1986, Preacher and Hayes 2004). Our first hypothesis was that the effect of lifetime perceived discrimination on medical conditions could be mediated through depressive symptoms and perceived stress. The model for depressive symptoms as a mediator was confirmed. We found a reduction of the total effect of perceived discrimination on medical conditions, for which the Sobel test confirmed that this reduction is significant and conclusive of mediation (Sobel test: z=3.57, p < 0.001) (Figure 1). However, the model for perceived stress was not confirmed, as it did not meet the criteria for mediation. We also tested whether the effect of lifetime perceived discrimination on medical conditions could be mediated through smoking and drinking behaviour, and neither model was confirmed.
For our second hypothesis, we tested whether the effect of lifetime perceived discrimination on diastolic blood pressure could be mediated through depressive symptoms or perceived stress, and neither of the models was confirmed, as they did not meet criteria for mediation. We also tested whether the effect of lifetime perceived discrimination on diastolic blood pressure could be mediated through smoking and drinking behaviours, and again, neither was confirmed.
Discussion
Our study has further confirmed the relevance of discrimination for existing minority health inequalities (Ahmad and Bradby 2007). Puerto Ricans in the United States live in a context which leads to experiences of racism and discrimination for many, with implications for their health. More than one third of the Puerto Rican adults reported that they had been exposed to discrimination associated with their ethnicity or language, and one third of these had experienced discrimination in healthcare settings. Participants who reported experiences of discrimination tended to be men, more educated, have higher incomes, were more likely to be employed, and more likely to use the English language. The greater extent of involvement in social and community activities was associated with a greater likelihood of reporting discrimination. These findings support the idea that greater social integration, mobility and thus contact with the surrounding environment increase one's chances of being exposed to unfair treatment and prejudice, and may increase one's sensitivity to such interactions. People who are less likely to leave their cultural niche or home environment due to functional limitations, advanced age or language limitations, are also less likely to face the prejudices of the mainstream society (Lauderdale et al. 2006). Similar findings have been reported by others (Borrell et al. 2006) .
Our findings confirm those from previous studies, which indicate a strong relevance of perceived discrimination for psychological health. Current levels of both depressive symptoms and of perceived stress were associated with lifetime experiences of discrimination. This suggests that at least some of the high depressive symptomatology in the Puerto Rican population in the Boston area (Falcon and Tucker 2000) may be attributed to lifetime exposure to discrimination.
Our findings also confirm existing literature, which shows that perceived discrimination may be associated with poorer physical health status. Unlike some authors (Finch and Vega 2003), we did not find a relationship with self-rated health. When controlling for demographic variables, however, we did find a relationship with the number of medical conditions. Importantly, similarly to Finch and Vega (2003), we also found that the effect of perceived discrimination on physical health, as operationalised by the number of existing medical conditions, and is mediated through depressive symptoms. It is important to note that in our analysis, the effect of perceived discrimination on chronic disease was not mediated by stress, but by depressive symptomatology. This finding speaks to the fact that lifetime accumulation of discrimination, while being associated with higher levels of perceived stress, ultimately promotes sustained depressive mood which resonates with poorer health status. As far as the physiological measure of blood pressure is concerned, we did not find an association between perceived discrimination and systolic blood pressure, but we did find an association with diastolic blood pressure.
The literature shows increased smoking and alcohol consumption as a result of perceived discrimination, which could be ways of coping with the evoked stress (Guthrie et al. 2002). Most of these studies are conducted with younger populations, such as adolescents and college students. In this older sample, with compromised health, many appear to have given up smoking and alcohol consumption when health problems appeared. We found that having experienced discrimination is associated with a higher probability of ever having smoked or ever having consumed alcohol. Discrimination may be leading to coping which includes health risk behaviours, but an alternative explanation is also possible – that smoking and (moderate) alcohol consumption are indicative of more active social involvement, which in turn increases one's exposure to perceived discrimination. However, unlike some other authors (Guthrie et al. 2002, Zucker and Landry 2007), we cannot state that perceived discrimination influences health through increasing these health risk behaviours, as potential mediating models of risk behaviours did not fit all the criteria for mediation.
Limitations
Our study was designed to address the psychosocial and physiological pathways through which perceived discrimination is related to health, using mainly self-report data and individual-level experiences. Thus, a clear limitation is that in this paper we have not examined structural discrimination and its impact on health, and we therefore have probably under-estimated the pact of discrimination and racism on health. In general, similarly to Pierret (2003) who stresses the importance of future research on the structural dimension of discrimination and stigma in relation to the subjective experience of illness, we underscore the need to expand research at the structural level of analysis and the interrelations between structural sources and conditions of discrimination more generally, interpersonal contexts of discrimination, personal experiences and responses, as well as the psychological and physical consequences. When focusing on perceived discrimination, we are not only addressing part of the potential discrimination that exists, but also only part of the potential health effects, since some of them, such as poorer housing, might be related to discrimination that is not perceived as such (Brondolo et al. 2003). In the development of the biopsychosocial model, it is still rare to find papers which connect all relevant levels of analyses (Suls and Rothman 2004); our on-going longitudinal study is however collecting data also at the neighborhood and community level (as well as the biological one) which will allow further exploration of this question in its more complicated form.
Additionally, while we hypothesise and test several pathways through which discrimination affects health, we are cognizant of the fact that we are working with cross-sectional data and that what we report are associations and not causal relationships. These pathways can be further illuminated through the analyses of longitudinal analyses which we are now in the process of collecting
A limitation of our study was that the measure we used was a one-item indicator of lifetime discrimination, and it has been suggested that such measures may underestimate the extent of these experiences (Ryan et al. 2006). While more expanded measures of perceived discrimination are available and can be used to further clarify the context of discrimination, single item measures have also been widely used (Araujo and Borrell 2006, David and Williams-Morris 2000) and much of the literature is built on the findings from such studies.
Another limitation is that our observations about perceived discrimination in relation to blood pressure are difficult to interpret clearly. Our findings regarding blood pressure could be confounded by the high prevalence of hypertension in this population (67.3%) and consequently the use of hypertension medications. Current understanding about the importance of SPB and DBP point to the stronger predictive value of SBP for cardiovascular morbidity and mortality (Beevers 2004, Black 2004, Kannel 1999). Interpretation of elevated SBP is more straightforward, as SBP linearly increases with age, and its relationship with mortality is generally linear. Interpretation of DBP is more complicated, as DBP tends to decrease with age (Black 2004), and lower DBP has been associated with greater heart disease risk (Beevers 2004). Existing literature on the relevance of discrimination to blood pressure shows varying results - associations with SBP, with DBP or both (Din-Dzietham et al. 2004, Krieger and Sidney 1996) More recently, laboratory investigations of cardiovascular reactivity (CVR) often indicate that DBP shows greater reactivity under the influence of racial stressors (Brondolo et al. 2003). Thus, DPB seems to be particularly sensitive to effects of racism and discrimination, with increased DBP for people experiencing such stresses. Additionally, our study of the physiological responses to discrimination might be limited by the statistical analyses which test linear associations. For example Krieger and Sidney (1996), have found that the relationship between the experience of discrimination and elevated blood pressure is not linear in African Americans. In other words, higher readings of systolic blood pressure were observed both for people who reported no discrimination, as well as for those who reported the highest levels of discrimination (in three or more settings), indicating the possible role of internalised anger. A non-linear association, or a U-shaped curve, has also been confirmed (Ryan et al. 2006).
Conclusion
It is clear that racism and discrimination are relevant for the health of Puerto Rican adults in the United States. Considering that this group experiences limited access to socioeconomic resources, poorer housing conditions, and limited access to healthcare (Rodriguez-Galan and Falcon 2009) as well as other interpersonal sources of stress such as language barriers, family separations and limited social networks, it is notable that having ever experienced discrimination is still so evidently related to their current health status. There are many intersecting factors which influence their health, yet the relevance of experiences of discrimination to indicators of both mental and physical health are evident and remain so even after taking into account other factors. Further longitudinal studies are needed to clarify the complexity of these associations.
Acknowledgements
We are grateful to the National Institutes of Aging, who have funded this project, under grant P01 AG023394.
Footnotes
References
- Ahmad WIU, Bradby H. Locating ethnicity and health: exploring concepts and contexts. Sociology of Health and Illness. 2007;29(6):795–810. doi: 10.1111/j.1467-9566.2007.01051.x. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2006;29(Supplement 1):S43–48. [PubMed] [Google Scholar]
- Araujo BY, Borrell LN. Understanding the link between discrimination, mental health outcomes and life chances among Latinos. Hispanic Journal of Behavioral Sciences. 2006;28(245-66) [Google Scholar]
- Barron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic and research considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beevers DG. Epidemiological, pathophysiological and clinical significance of systolic, diastolic and pulse pressure. Journal of Human Hypertension. 2004;18(8):531–33. doi: 10.1038/sj.jhh.1001702. [DOI] [PubMed] [Google Scholar]
- Bierman A. Does religion buffer the effects of discrimination on mental health? Differing effects by race. Journal for the Scientific Study of Religion. 2006;45(4):551–65. [Google Scholar]
- Black HR. The paradigm has shifted to systolic blood pressure. Journal Of Human Hypertension. 2004;18(Supplement 2):S3–7. doi: 10.1038/sj.jhh.1001795. [DOI] [PubMed] [Google Scholar]
- Borrell LN, Kiefe CI, Williams DR, Diez-Roux AV, Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Social Science and Medicine (1982) 2006;63(6):1415–27. doi: 10.1016/j.socscimed.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Broman CL. Perceived discrimination and alcohol use among Black and White college students. Journal of Alcohol and Drug Education. 2007;51(1):8–16. [Google Scholar]
- Brondolo E, Rieppi R, Kelly K, Gerin W. Perceived racism and blood pressure: a review of the literature and conceptual and methodological critique. Annals of Behavioral Medicine. 2003;25(1):55. doi: 10.1207/S15324796ABM2501_08. [DOI] [PubMed] [Google Scholar]
- Cardarelli R, Cardarelli KM, Chiapa AL. Brief report: the modifying effects of education and income on Hispanics reporting perceived discrimination. Hispanic Journal of Behavioral Sciences. 2007;29(3):401–07. [Google Scholar]
- Chae DH, Takeuchi DT, Barbeau EM, Bennett GG, Lindsey J, Krieger N. Unfair treatment, racial/ethnic discrimination, ethnic identification, and smoking among Asian Americans in the National Latino and Asian American Study. American Journal of Public Health. 2008;98(3):485–92. doi: 10.2105/AJPH.2006.102012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R. Perceptions of interethnic group racism predict increased vascular reactivity to a laboratory challenge in college women. Annals of Behavioral Medicine: A Publication of The Society of Behavioral Medicine. 2000;22(3):214–22. doi: 10.1007/BF02895116. [DOI] [PubMed] [Google Scholar]
- Clark R, Anderson N, Clark V, Williams D. Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist. 1999;54(10):805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Sage; Newbury Park, CA: 1988. [Google Scholar]
- David RW, Williams-Morris R. Racism and mental health: the African American experience. Ethnicity and Health. 2000;5(3-4):243–68. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- Din-Dzietham R, Nembhard WN, Collins R, Davis SK. Perceived stress following race-based discrimination at work is associated with hypertension in African-Americans. The metro Atlanta heart disease study, 1999-2001. Social Science and Medicine (1982) 2004;58(3):449–61. doi: 10.1016/s0277-9536(03)00211-9. [DOI] [PubMed] [Google Scholar]
- Dougall AL, Baum A. Stress, health and illness. In: Baum A, Revenson TA, Singer JE, editors. Handbook of Health Psychology. Lawrence Erlbaum; Mahwah, NJ: 2001. [Google Scholar]
- Ellis BH, MacDonald HZ, Lincoln AK, Cabral HJ. Mental health of Somali adolescent refugees: the role of trauma, stress, and perceived discrimination. Journal of Consulting and Clinical Psychology. 2008;76(2):184–93. doi: 10.1037/0022-006X.76.2.184. [DOI] [PubMed] [Google Scholar]
- Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular disease. Annual Review of Public Health. 2005;26(469-500) doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- Falcon LM, Tucker KL. Prevalence and correlates of depressive symptoms among Hispanic elders in Massachusetts. Journal of Gerontology. 2000;55B(2):5108–16. doi: 10.1093/geronb/55.2.s108. [DOI] [PubMed] [Google Scholar]
- Finch BK, Hummer RA, Kolody B, Vega WA. The role of discrimination and acculturative stress in the physical health of Mexican-origin adults. Hispanic Journal of Behavioral Sciences. 2001;23(4):399–429. [Google Scholar]
- Finch BK, Hummer RA, Reindl M, Vega WA. Validity of self-rated health among Latino(a)s. American Journal of Epidemiology. 2002;155(8):755–59. doi: 10.1093/aje/155.8.755. [DOI] [PubMed] [Google Scholar]
- Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. Journal of Health and Social Behavior. 2000;41(3):295–313. [PubMed] [Google Scholar]
- Finch BK, Vega WA. Acculturation stress, social support and self-rated health among Latinos in California. Journal of Immigrant Health. 2003;5(109-17) doi: 10.1023/a:1023987717921. [DOI] [PubMed] [Google Scholar]
- Gee GC, Ryan A, Laflamme DJ, Holt J. Self-reported discrimination and mental health status among African descendants, Mexican Americans, and other Latinos in the New Hampshire REACH 2010 Initiative: the added dimension of immigration. American Journal of Public Health. 2006;96(10):1821–8. doi: 10.2105/AJPH.2005.080085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Spencer M, Chen J, Yip T, Takeuchi DT. The association between self-reported racial discrimination and 12-month DSM-IV mental disorders among Asian Americans nationwide. Social Science and Medicine (1982) 2007a;64(10):1984–96. doi: 10.1016/j.socscimed.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Spencer MS, Chen J, Takeuchi D. A nationwide study of discrimination and chronic health conditions among Asian Americans. American Journal of Public Health. 2007b;97(7):1275–82. doi: 10.2105/AJPH.2006.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene ML, Way N, Pahl K. Trajectories of perceived adult and peer discrimination among Black, Latino, and Asian American adolescents: patterns and psychological correlates. Developmental Psychology. 2006;42(2):218–36. doi: 10.1037/0012-1649.42.2.218. [DOI] [PubMed] [Google Scholar]
- Guthrie BJ, Young AM, Williams DR, Boyd CJ, Kintner EK. African American girls' smoking habits and day-to-day experiences with racial discrimination. Nursing Research. 2002;51(3):183–90. doi: 10.1097/00006199-200205000-00007. [DOI] [PubMed] [Google Scholar]
- Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: relationship to cardiovascular reactivity among African American and European American women. Health Psychology. 2001;20(5):315–25. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- Harris R, Tobias M, Jeffreys M, Waldegrave K, Karlsen S, Nazroo J. Racism and health: the relationship between experience of racial discrimination and health in New Zealand. Social Science and Medicine. 2006;63(1428-41) doi: 10.1016/j.socscimed.2006.04.009. [DOI] [PubMed] [Google Scholar]
- Idler I, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38(21-37) [PubMed] [Google Scholar]
- Jasti S, Dudley WN, Goldwater E. SAS Macros for testing statistical mediation in data with binary mediators or outcomes. Nursing Research. 2008;57(2):118–22. doi: 10.1097/01.NNR.0000313479.55002.74. [DOI] [PubMed] [Google Scholar]
- Joint National Committee on Prevention Detection Evaluation and Treatment of High Blood Pressure . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. U.S. Department of Health and Human Services; Bethesda, MD: 2003. NIH Publication No. 03-5233. [Google Scholar]
- Kannel WB. Historic perspectives on the relative contributions of diastolic and systolic blood pressure elevation to cardiovascular risk profile. American Heart Journal. 1999;138(3 Pt 2):205–10. doi: 10.1016/s0002-8703(99)70311-x. [DOI] [PubMed] [Google Scholar]
- Karlsen S, Nazroo J. Agency and structure: the impact of ethnic identity and racism on the health of ethnic minority people. Sociology of Health and Illness. 2002;24(1):1–20. [Google Scholar]
- Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young Black and White adults. American Journal of Public Health. 1996;86(10):1370–8. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Wen M, Jacobs EA, Kandula NR. Immigrant perceptions of discrimination in health care: the California Health Interview Survey. Medical Care. 2006;44(10):914–20. doi: 10.1097/01.mlr.0000220829.87073.f7. [DOI] [PubMed] [Google Scholar]
- MacDonald G, Leary MR. Why does social exclusion hurt? The realtionship between social exclusion and physical pain. Psychological Bulletin. 2005;131(2):202–23. doi: 10.1037/0033-2909.131.2.202. [DOI] [PubMed] [Google Scholar]
- Marin G, Gamba RJ. A new measurement of acculturation for Hispanics: the Bidimensional Acculturation Scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1996;18(3):297–316. [Google Scholar]
- Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annual Review of Psychology. 2007;58(201-25) doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller G, Chen E, Cole SW. Health psychology: developing biologically plausible models linking the social world and physical health. Annual Review of Psychology. 2009;60(501-24) doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
- Moscicki E, Rae DS, Reiger E, Locke B. Depression among Mexican Americans, Cubans and Puerto Ricans. In: Gaviria M, Arana J, editors. Health and behavior: Research agenda for Hispanics (Simon Bolivar Research Monograph Series I. University of Illinois Press; Chicago: 1987. [Google Scholar]
- Noh S, Beiser M, Kaspar V, Hou F, Rummens J. Perceived racial discrimination, depression, and coping: a study of Southeast Asian refugees in Canada. Journal of Health and Social Behavior. 1999;40(3):193–207. [PubMed] [Google Scholar]
- Noh S, Kaspar V. Perceived discrimination and depression: moderating effects of coping, acculturation, and ethnic support. American Journal of Public Health. 2003;93(2):232–8. doi: 10.2105/ajph.93.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavalko EK, Mossakowski KN, Hamilton VJ. Does perceived discrimination affect health? Longitudinal relationships between work discrimination and women's physical and emotional health. Journal of Health and Social Behavior. 2003;44(1):18–33. [PubMed] [Google Scholar]
- Pierret J. The illness experience: state of knowledge and perspectives for research. Sociology of Health and Illness. 2003;25(Silver Anniversary Issue):4–22. doi: 10.1111/1467-9566.t01-1-00337. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, and Computers. 2004;36(4):717–31. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Prelow HM, Mosher CE, Bowman MA. Perceived racial discrimination, social support, and psychological adjustment among African American college students. Journal of Black Psychology. 2006;32(4):442–54. [Google Scholar]
- Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(385-401) [Google Scholar]
- Radloff L. The use of the Center of Epidemiological Studies Depression Scale with older adults. Clinical Gerontology. 1986;5(119-36) [Google Scholar]
- Rodriguez-Galan MB, Falcon LM. Perceived problems with access to medical care and depression among older Puerto Ricans, Dominicans, Other Hispanics, and a comparison group of non-Hispanic whites. Journal of Aging and Health. 2009;21(3):501–18. doi: 10.1177/0898264308329015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan AM, Gee GC, Laflamme DF. The association between self-reported discrimination, physical health and blood pressure: findings from African Americans, Black immigrants, and Latino immigrants in New Hampshire. Journal of Health Care for the Poor and Underserved. 2006;17(2 Supplement):116–32. doi: 10.1353/hpu.2006.0092. [DOI] [PubMed] [Google Scholar]
- Schnittker J, McLeod JD. The social psychology of health disparities. Annual Review of Sociology. 2005;31(75-103) [Google Scholar]
- Stuber J, Galea S, Ahern J, Blaney S, Fuller C. The association between multiple domains of discrimination and self-assessed health: a multilevel analysis of Latinos and blacks in four low-income New York City neighborhoods. Health Services Research. 2003;38(6 Pt 2):1735–59. doi: 10.1111/j.1475-6773.2003.00200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suls J, Rothman A. Evolution of the biopsychosocial model: Prospects and challenges for health psychology. Health Psychology. 2004;23(2):119–25. doi: 10.1037/0278-6133.23.2.119. [DOI] [PubMed] [Google Scholar]
- Szalacha LA, Erkut S, Garcia Coll C, Alarcon O, Fields JP, Ceder I. Discrimination and Puerto Rican children's and adolescents' mental health. Cultural Diversity and Ethnic Minority Psychology. 2003;9(2):141–55. doi: 10.1037/1099-9809.9.2.141. [DOI] [PubMed] [Google Scholar]
- Tucker K, Bermudez O, Castaneda C. Type 2 diabetes is prevalent and poorly controlled among Hispanic elders of Caribbean origin. American Journal of Public Health. 2000;90(7):1288–1 93. doi: 10.2105/ajph.90.8.1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker K, Bermudez OI, Falcon LM, Ordovas J. Health Disparities among Older Latinos in Boston. NIH Center for Population Health and Health Disparities: Grantee Meeting; Boston, MA: 2007. [Google Scholar]
- Tucker K, Falcon LM, Bianchi LA, Cacho E, Bermudez OI. Self-reported prevalence and health correlates of functional limitation among Massachusetts elderly Puerto Ricans, Dominicans and a non-Hispanic white neighborhood comparison group. Journal of Gerontology. 2000;55A(2):M90–M97. doi: 10.1093/gerona/55.2.m90. [DOI] [PubMed] [Google Scholar]
- Uchino B. Social support and health: a review of physiological pathways potentially underlying link to disease outcomes. Journal of Behavioral Medicine. 2006;29(4):377–87. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. US Socioeconomic and racial differences in health: patterns and explanations. Annual Review of Sociology. 1995;21(349-86) [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. American Journal of Public Health. 2003;93(2):200–08. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker AN, Landry LJ. Embodied discrimination: the relation of sexism and distress to women's drinking and smoking behaviors. Sex Roles. 2007;56(3):193–203. [Google Scholar]