Abstract
Aims
Controversy exists regarding the inclusion of cannabis withdrawal as an indicator of dependence in the next revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Classification of Diseases (ICD). This study contrasted the concurrent and predictive validity of three operational definitions of cannabis withdrawal in a sample of treated adolescents.
Design
Prospective study of treated adolescents with 1-year follow-up.
Setting and participants
Adolescents (n = 214) were recruited from intensive out-patient treatment programs for substance abuse, and followed at 1 year (92% retention). Youth who were included in the analyses reported regular cannabis use.
Measurements
The number of DSM-IV cannabis abuse and dependence symptoms at baseline and 1-year follow-up, past year frequency of cannabis use at baseline and follow-up, and periods of abstinence at 1-year follow-up. Cannabis withdrawal was defined based on (i) the presence of two or more cannabis withdrawal symptoms; (ii) a definition proposed by Budney and colleagues (2006) that requires four or more withdrawal symptoms (four-symptom definition); and (iii) the use of latent class analysis to identify subgroups with similar cannabis withdrawal symptom profiles.
Findings and conclusions
All three definitions of cannabis withdrawal demonstrated some concurrent validity. Only the four-symptom and latent class-derived definitions of withdrawal predicted severity of cannabis-related problems at 1-year follow-up. No cannabis withdrawal definition predicted frequency of use at follow-up. Further research is needed to determine the clinical utility and validity of the four-symptom definition, as well as alternative definitions of cannabis withdrawal, to inform revisions leading to DSM-V and ICD-11.
Keywords: Adolescent, cannabis, DSM, ICD, withdrawal
INTRODUCTION
Controversy exists regarding whether a cannabis withdrawal syndrome should be included in the next revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM) [1]. If included in DSM-V, an operational definition of a cannabis withdrawal syndrome would facilitate recognition of an acute syndrome that warrants treatment (similar to criteria used to identify withdrawal syndromes for substances such as alcohol and cocaine), and would also provide a means of determining the presence of the ‘withdrawal’ criterion when evaluating an individual for a diagnosis of cannabis dependence. In contrast to DSM-IV, the International Classification of Diseases (ICD) recognizes a cannabis withdrawal syndrome, but states that its diagnostic criteria remain to be determined [2].
Critics who oppose including cannabis withdrawal in DSM and ICD have cited the need for a clear operational definition of the syndrome with regard to time–course, symptom profile and clinical significance [3]. Proponents of including cannabis withdrawal emphasize research on its neurobiological basis [4], delineation of the typical time–course and symptoms of a cannabis abstinence syndrome [5–7] and reports of functional impairment due to cannabis withdrawal [8,9]. Questions remain as to the type and number of symptoms that optimally identify cannabis withdrawal, and the extent to which withdrawal plays a role in maintaining the compulsive pattern of drug use that is the hallmark of dependence.
Among adult heavy cannabis users, abstinence from cannabis typically precipitates withdrawal symptoms that emerge within 24–48 hours of abstinence [10]. The symptoms usually peak within a week, and last roughly 1–2 weeks [6,11]. Re-administration of cannabis relieves the symptoms associated with abstinence from the drug [6,12,13], and provides another way (i.e. withdrawal relief) in which cannabis withdrawal as a possible dependence criterion may manifest. Cannabis withdrawal symptoms generally represent physical and psychological dimensions based on results of principal components analysis [7]. Affective and behavioral, rather than physical (e.g. tremor, sweating) cannabis withdrawal symptoms are reported most often, and include irritability, decreased appetite, restlessness and sleep problems [7,10]. Among adults seeking treatment for cannabis use, 85% reported four or more cannabis withdrawal symptoms of at least mild severity during the most recent episode of abstinence [6]. Cannabis withdrawal is associated with greater severity of cannabis involvement both cross-sectionally and prospectively in adults [14]. Cannabis withdrawal also appears to play a role in maintaining dependence (e.g. use to relieve withdrawal) and impacting negatively attempts to quit or cut down on use [7,15], although the number and type of symptoms to use in defining a cannabis withdrawal syndrome, which would also function as a criterion used to diagnose cannabis dependence, remain to be specified in DSM and ICD.
Less is known about the prevalence and symptom profile of cannabis withdrawal among adolescents, although cannabis is the illicit substance most commonly used by youth [16]. In a community sample, among adolescents with a cannabis use disorder 15% endorsed cannabis withdrawal (the operational definition used to identify withdrawal was not specified); withdrawal was the least prevalent dependence symptom [17]. Higher rates of cannabis withdrawal, ranging from 40 to 67%, have been reported among adolescents in addictions treatment ([18,19]; these studies also did not specify the operational definition of withdrawal used). In a sample of treated youth, 15% reported use to relieve withdrawal [19]. The most commonly reported cannabis withdrawal symptoms among adolescents include craving, depression, irritability, difficulty sleeping, restlessness and decreased appetite [18–21]. Among treated adolescents, one-third reported four or more withdrawal symptoms of at least moderate severity [20]. As an indication of the clinical significance of cannabis withdrawal, withdrawal symptoms in a sample of out-patient adolescents were found to interfere with completion of school work and the ability to maintain abstinence from cannabis [21]. Importantly, commonly reported cannabis withdrawal symptoms were similar for adults and adolescents, although withdrawal prevalence and severity were typically lower in youth [10].
In a comprehensive literature review, Budney and colleagues [10,22] proposed criteria for a cannabis withdrawal syndrome to be considered for inclusion in the next revision of the DSM. The proposed criteria include the following six symptoms: anger or aggression, irritability, decreased appetite, nervousness/anxiety, restlessness and insomnia (including strange dreams) [10,22]. Because most treated adult cannabis users generally reported four or more of these six commonly reported symptoms occurring with substantial severity, and because a four-symptom threshold has been used to define withdrawal syndromes for other substances in DSM-IV, report of four or more of the six more commonly reported symptoms, in combination with impairment in functioning or subjective distress, was proposed as an operational definition of a cannabis withdrawal syndrome [22,23]. Details on the method of selecting the six symptoms and the four-symptom threshold, however, were not provided. Research is needed to determine systematically the type and number of symptoms that defines optimally a cannabis withdrawal criterion, and the extent to which withdrawal predicts a relatively chronic course.
To determine empirically the optimal number and type of symptoms that define a cannabis withdrawal syndrome, we used latent class analysis (LCA [24]). LCA identifies subtypes based on the symptom profiles reported by individuals in the sample, and has been used to evaluate the validity of distinctions between existing diagnostic categories [25]. A particular advantage of the LCA approach is that it identifies a small number of mutually exclusive subgroups that may differ in the number and type of symptom endorsed. Thus, LCA can provide information efficiently to guide the evaluation of which symptoms are most useful to include in an operational definition of cannabis withdrawal, and what symptom thresholds distinguish the subgroups—two types of information that are essential to developing an empirically based operational definition of cannabis withdrawal.
This prospective study of adolescents recruited from addictions treatment, and followed over 1 year, examined the number and type of cannabis withdrawal symptoms that defines optimally the withdrawal syndrome in youth. Three definitions of cannabis withdrawal were examined: episodes involving two or more withdrawal symptoms (i.e. two-symptom threshold used in previous research [14,26]), criteria for withdrawal proposed by Budney and colleagues [10,22] (i.e. four-symptom definition) and a definition based on results from latent class analysis of cannabis withdrawal symptoms (i.e. latent class definition, a new empirically determined definition of cannabis withdrawal). All three definitions of cannabis withdrawal required the recurrence of withdrawal episodes (i.e. three or more withdrawal episodes within a 1-year period) and report of subjective distress or impairment in functioning due to withdrawal symptoms (i.e. clinical significance). The three definitions of cannabis withdrawal were contrasted with regard to concurrent and predictive validity. We predicted that more stringent definitions of cannabis withdrawal (e.g. four-symptom definition) would be more likely to demonstrate concurrent and predictive validity compared to a milder definition of withdrawal (e.g. two-symptom definition).
METHOD
Participants
Adolescents, aged 14–18 years, were recruited from intensive out-patient addictions treatment programs for youth in Western Pennsylvania. The treatment programs provided similar program content, and at all sites the typical course of intensive out-patient treatment lasted 6–8 weeks. Shortly after treatment admission, adolescents were provided with a brief description of a research study on the course of alcohol and drug problems to determine their interest in study participation. Most (77%) youth who were approached by project staff agreed to study participation. Youth enrolled in the study are broadly comparable on demographic and substance use characteristics to the population of youth in addictions treatment [16]. Adolescents included in these analyses (n = 214) reported, at minimum, life-time cannabis use at least once per month for at least 6 months. This is a sample of relatively heavy cannabis users: 45% of adolescents reported daily cannabis use in the year prior to treatment, and 21% reported use four to six times per week (Table 1).
Table 1.
Descriptive statistics on frequency of cannabis use and cannabis symptom prevalence at baseline (n = 214) and 1-year follow-up (n = 197).
| Baseline | 1-year follow-up | |
|---|---|---|
| Past year frequency of cannabis use (%) | ||
| No use in past year | 0.0 | 16.6 |
| < Once per month | 7.5 | 17.6 |
| Once per month | 1.9 | 2.1 |
| 2–3 times per month | 6.6 | 6.7 |
| Once per week | 5.2 | 6.7 |
| 2–3 times per week | 12.7 | 7.8 |
| 4–6 times per week | 20.8 | 21.2 |
| Daily | 45.3 | 21.2 |
| Past year DSM-IV cannabis abuse and dependence symptoms (%) | ||
| Abuse 1: role obligation | 64.5 | 26.4 |
| Abuse 2: hazardous use | 51.4 | 39.1 |
| Abuse 3: legal problems | 3.7 | 2.0 |
| Abuse 4: interpersonal problems | 65.9 | 28.9 |
| Dependence 1: tolerance | 73.4 | 53.8 |
| Dependence 2: use more/longer | 22.4 | 5.6 |
| Dependence 3: quit/cut down | 62.6 | 39.1 |
| Dependence 4: much time | 77.6 | 47.7 |
| Dependence 5: reduce activities | 32.7 | 5.1 |
| Dependence 6: psychological/physical | 13.1 | 12.7 |
| Mean DSM-IV cannabis abuse and dependence symptom count (SD) | 4.7 (2.4) | 2.4 (2.3) |
| Observed range of values | 0–9 | 0–9 |
| Cannabis withdrawal (past year) definitions (%) | ||
| Two-symptom recurrent cannabis withdrawal | 37.4 | 21.3 |
| Four-symptom recurrent cannabis withdrawal | 17.8 | 11.2 |
| LCA high severity recurrent cannabis withdrawal | 17.3 | 10.6 |
Cannabis withdrawal is not included in the list of DSM-IV dependence symptoms in this table because DSM-IV does not specify how ‘cannabis withdrawal’ is to be identified. The total possible number of DSM-IV cannabis abuse and dependence symptoms is 10 (four abuse and six dependence symptoms). ‘LCA high severity’: latent class analysis-based definition of cannabis withdrawal that distinguishes youth in the LCA ‘high severity’ withdrawal class who reported recurrent episodes of withdrawal from all other participants. SD: standard deviation.
At baseline, the majority of participants were male (67%) and Caucasian (90%). African Americans represented 5% of the sample; Hispanics, Asians and ‘other’ ethnicity (i.e. individuals who reported a bi-racial ethnicity) accounted for 5% of the total sample. Participants had a mean age of 16.8 years [standard deviation (SD) = 1.1], and represented a broad range of socioeconomic status (SES; mean = 2.5, SD = 1.0; range = 1–5; [27]). Most adolescents were receiving treatment for a cannabis use disorder. At baseline, the majority (88.7%) of participants met criteria for a past year DSM-IV cannabis abuse (28.0%) or dependence (60.7%) diagnosis. At baseline, 68.2% of youth also met criteria for a past year alcohol diagnosis. The life-time mean number of other drugs used (excluding alcohol and cannabis, of a possible total of six drugs) was 3.2 (SD = 2.2); the most common drugs tried were opiates, sedatives and hallucinogens. Regarding other commonly reported psychopathology (past year) at baseline, 37.4% met criteria for conduct disorder, 27.6% for a depressive disorder (major depression or dysthymia), 17.3% for attention deficit hyperactivity disorder and 10.3% for an anxiety disorder (specific phobia, social phobia, generalized anxiety disorder or panic disorder).
Participants were followed for 1 year after completion of the baseline assessment (n = 197; 92% retention). Comparison of retained participants and dropouts (197 versus 17 adolescents, respectively) indicated that dropouts at 1-year follow-up had higher SES (3.1 versus 2.5; t = 2.5, d.f. = 203, P < 0.05), reported more past year DSM-IV cannabis dependence symptoms at baseline (2.7 versus 3.8; t = 2.6, d.f. = 212, P < 0.05), more past year DSM-IV cannabis abuse and dependence symptoms at baseline (4.6 versus 5.9; t = 2.3, d.f. = 212, P < 0.05) and greater baseline frequency of past year cannabis use (measured on an ordinal scale: 7.5 versus 6.5; t = 2.1, d.f. = 210, P < 0.05). No differences were observed for retained youth and dropouts on other variables that were included in the analyses, P > 0.05 (e.g. gender, age, ethnicity, baseline past year diagnoses of alcohol use disorder, conduct disorder, other psychopathology and life-time other substance use).
Procedure
Adolescents completed baseline and 1-year follow-up assessment protocols that were administered by highly trained bachelor’s or master’s level interviewers. In this repeated-measures study, interview and questionnaire measures that were administered at baseline were also administered at 1-year follow-up. The time-frame for all measures at each time-point was ‘past year’, with the exception of ‘life-time’ other substance use assessed at baseline. Interviewers received intensive training over 3 months to obtain >80% agreement on symptom and diagnostic ratings with a doctoral level supervisor on at least three consecutive interviews. Interviewer drift in ratings was minimized through weekly supervision led by doctoral level clinicians with substantial experience in the assessment of psychiatric and substance use disorders in youth.
After description of study procedures and prior to data collection, written informed consent or assent was obtained from the adolescent and his/her guardian. Baseline interviews were completed within 6 weeks of treatment entry. Each assessment lasted 2–3 hours, and collected data on the adolescent’s substance use, DSM-IV substance use disorders (SUDs) and co-occurring psychopathology. Youth completed a urine drug screen at each assessment; drug screen results that were discrepant with self-reported substance use were discussed with the adolescent to ensure high-quality data. Participants were compensated upon completion of each assessment. The university’s institutional review board approved the study protocol.
Measures
The Structured Clinical Interview for DSM-IV (SCID) [28], modified for use with youth [29], was used to determine the presence of DSM-IV SUD criteria and diagnoses at baseline and 1-year follow-up. The SCID was adapted to include developmentally appropriate queries of DSM-IV SUD symptoms (e.g. cannabis-related suspensions or expulsion from school). The modified SCID included probes to determine the presence of cannabis withdrawal, which could be met either by repeated episodes of cannabis withdrawal (based on a two-symptom threshold used in other studies [14,26]) or ‘withdrawal relief’ (i.e. use of cannabis to relieve or to prevent withdrawal based on the two-symptom threshold). If the adolescent reported symptoms that resulted from a sharp reduction or cessation in cannabis use, 22 withdrawal symptoms [8] were rated as present or absent. For a cannabis withdrawal symptom to be rated as ‘present’, subjective distress or impairment in functioning due to the symptom needed to be reported as an indication of the clinical significance of the symptom. Therefore, all definitions of withdrawal tested in this study included evidence of subjective distress or impairment in functioning, because this evaluation was built-in at the symptom level. If the adolescent reported two or more withdrawal symptoms [14,26], the adolescent was asked further if the symptoms occurred together three or more times in the past year (i.e. recurrence was defined as three or more episodes within a 12-month period for all definitions tested) following reduction or cessation of heavy use. Interviewers probed whether withdrawal symptoms were due specifically to cannabis or some other drug, or due to exacerbation of a co-occurring psychiatric condition.
Because a stereotyped pattern of substance use and rapid reinstatement of dependence symptoms after a period of abstinence have been linked to the presence of withdrawal for other substances (e.g. alcohol [30]), the modified SCID also included probes for these symptoms. To determine the presence of a stereotyped pattern of use, probes such as ‘did smoking marijuana put you on a schedule, where you smoked every few hours because you felt that you needed to?’ were used. To evaluate rapid reinstatement of dependence, probes such as ‘after stopping smoking for at least 1 month, when you started smoking again, how long did it take for (list dependence symptoms that were rated as present in the assessment) to re-emerge?’ were used. At least two dependence symptoms needed to re-emerge within a month after resumption of daily or near-daily use (or 2 months if use was resumed at a lower level) for this symptom to be assigned. For both these additional symptoms, recurrence (as defined above) and clinical significance (i.e. report of subjective distress or impairment due to the symptom) needed to be reported in order for the symptoms to be rated as ‘present’ by the interviewer.
Two-week test–retest showed high levels of agreement for life-time cannabis diagnoses in this study: cannabis abuse (kappa = 0.80) and dependence (kappa = 0.85). Two-week test–retest also showed high agreement at the symptom level for cannabis and other substances. For example, intraclass correlations (ICCs) for life-time count of the total number of abuse and dependence symptoms were high: alcohol = 0.78 and cannabis = 0.96 [31].
To assess life-time substance use at baseline, adolescents were asked ‘Have you ever tried … ?’ (yes or no) substances that were grouped into eight drug classes: alcohol, cannabis, cocaine, opiates, sedatives, stimulants, hallucinogens and other drug (e.g. ecstasy). The number of drug classes endorsed at baseline, excluding alcohol and cannabis, was used as a proxy measure of the extent of other substance use. A questionnaire item was used to determine the frequency of cannabis use in the past year (‘How often did you use marijuana in the past year?’) according to response categories listed in Table 1 at baseline and 1-year follow-up. The Lifetime Drug Use History [32] interview collected data on the number of 30-day periods of abstinence that occurred over 1-year follow-up. Two-week test–retest for these types of substance use scores and data were comparable to retest ICCs reported above [32].
A modified version of the Schedule for Affective Disorders and Schizophrenia (K-SADS) [33] was used to assess Axis I psychopathology other than substance use disorders at baseline. Conduct disorder was considered for inclusion as a covariate in predictive validity analyses because it is a relatively robust predictor of adolescent treatment outcome [25,34], and other common psychiatric disorders were also included as covariates (e.g. attention deficit hyperactivity disorder). The modified K-SADS has good reliability and concurrent validity [35].
Data analysis
In addition to the two- and four-symptom definitions of cannabis withdrawal, we used latent class analysis (LCA) [24] to determine the type and number of cannabis withdrawal symptoms that best defines the syndrome in treated adolescents. Using Latent Gold 4.0 [36], latent class models specifying 1–6 classes were applied to the 22 baseline cannabis withdrawal symptoms. Because this study examined the predictive validity of different definitions of cannabis withdrawal, results of LCA on withdrawal symptoms at 1-year follow-up are not detailed here (note, however, that LCA results were similar at both time-points, with the number rather than type of withdrawal symptom endorsed distinguishing the classes). In LCA, each latent class represents a distinct profile of symptom endorsement probabilities (SEPs; i.e. the likelihood of having a symptom given membership in a certain class) that is the same for all members of the class, taking stochastic factors into account [24]. LCA produces class membership probabilities and SEPs for each class in a model. Identification of the best-fitting model was based on the lowest Bayesian information criterion (BIC) [37]. Individuals were assigned to the class with the highest posterior probability.
Agreement between the three definitions of cannabis withdrawal was computed using kappa, where 0.40–0.75 indicates fair to good agreement and kappa >0.75 indicates excellent agreement [38]. Concurrent validity of the different definitions of cannabis withdrawal was then examined using SPSS version 14.0 based on t-tests (two-tailed) and χ2 tests, as appropriate. Concurrent validators at baseline and 1 year included the number of past year cannabis abuse and dependence symptoms, past year cannabis dependence symptoms, past year frequency of cannabis use, duration of regular cannabis use (at baseline only), past year presence of the cannabis tolerance symptom (because tolerance tends to be associated with withdrawal; [30]), past year presence of a stereotyped pattern of cannabis use and rapid reinstatement of dependence after at least 1 month of abstinence from cannabis use.
Predictive validity of the different definitions of cannabis withdrawal was examined using regression analyses (SPSS version 14.0), controlling for gender, age, ethnicity, SES, frequency of cannabis use at baseline (using response categories described in Table 1), life-time number of substances used (other than alcohol and cannabis), past year alcohol diagnosis (yes/no) and other past year psychopathology at baseline (yes/no diagnosis): conduct disorder, depressive disorder (major depression or dysthymia), attention deficit hyperactivity disorder and anxiety disorder (social phobia, panic disorder, agoraphobia). Simultaneous linear regression (all predictors entered together) was used to predict the following 1-year outcomes: past year DSM-IV cannabis abuse and dependence symptom count, past year DSM-IV cannabis dependence symptom count, past year frequency of cannabis use (using response categories described in Table 1), number of periods of 30-day abstinence over 1-year follow-up and maximum consecutive abstinent days over 1-year follow-up. The rationale for examining the number of 30-day periods of abstinence that were reported over 1-year follow-up (in addition to other variables related to ability to maintain abstinence) is based on the minimum level of use that needed to be reported (i.e. use at least once per month) to be included in these analyses. Simultaneous logistic regression was used to predict the following 1-year outcomes: 7-day and 30-day point prevalence abstinence at 1 year. Critical alpha was set at 0.05 for all statistical tests.
RESULTS
Prevalence of cannabis withdrawal symptoms
Craving and irritability were the cannabis withdrawal symptoms reported most often at both time-points (Table 2). Seizure was not reported at either time-point. The average number of withdrawal symptoms was 4.4 (SD = 4.4) at baseline and 2.0 (SD = 3.2) at follow-up; this reduction over follow-up was statistically significant (paired t = 7.9, d.f. = 196, P < 0.01).
Table 2.
Prevalence of cannabis withdrawal symptoms at baseline (n = 214) and 1-year follow-up (n = 197).
| Cannabis withdrawal symptom | Baseline | 1-year follow-up |
|---|---|---|
| 1 Crave the drug | 66.4 | 34.0 |
| 2 Irritable | 46.3 | 27.9 |
| 3 Trouble concentrating | 38.3 | 15.2 |
| 4 Trouble sleeping | 34.1 | 17.8 |
| 5 Restless | 32.7 | 19.8 |
| 6 Anger, violent outburst | 28.0 | 10.2 |
| 7 Change in appetite | 27.6 | 12.7 |
| 8 Anxious | 25.7 | 12.2 |
| 9 Headache | 25.7 | 7.6 |
| 10 Depressed | 25.2 | 9.1 |
| 11 Tired, sleepy, weak | 22.9 | 7.6 |
| 12 Yawn a lot | 21.0 | 6.1 |
| 13 Vivid, unpleasant dreams | 14.5 | 7.1 |
| 14 Tremble, twitch | 8.4 | 1.5 |
| 15 Fast heartbeat | 5.6 | 1.0 |
| 16 Teary, runny nose | 4.7 | 1.5 |
| 17 Sweat, fever | 2.8 | 1.0 |
| 18 Nauseated, vomit | 2.8 | 0.5 |
| 19 Muscle pains | 2.8 | 2.0 |
| 20 Hallucinations | 1.9 | 0.5 |
| 21 Diarrhea, stomachache | 0.9 | 2.0 |
| 22 Seizures | 0.0 | 0.0 |
| Mean cannabis symptom count (SD) | 4.4 (4.4) | 2.0 (3.2) |
Two-symptom definition of cannabis withdrawal: prevalence
In DSM-IV, the withdrawal criterion for a substance may be met either by recurrent episodes of withdrawal or recurrent withdrawal relief. Based on previous studies [26], the modified SCID used a two-symptom threshold to identify cannabis withdrawal (i.e. two or more of 22 possible withdrawal symptoms) and to determine the occurrence of cannabis use to relieve withdrawal. Both the two-symptom definition of withdrawal and withdrawal relief, based on a two-symptom definition, required report of ‘recurrent’ episodes and distress or impairment in functioning due to the withdrawal symptoms. At baseline and 1 year, cannabis withdrawal, defined using a two-symptom threshold or withdrawal relief (based on a two-symptom definition), was the fourth most prevalent among the dependence symptoms (Table 1, baseline: 37.4%, 1 year: 21.3%). Based on a two-symptom threshold to define withdrawal, at baseline 23.4% had both cannabis withdrawal and withdrawal relief, 11.7% had withdrawal only and 2.3% reported withdrawal relief only. At 1 year, the relative proportions of these symptom components were similar, but lower compared to baseline: 11.7% had both cannabis withdrawal and withdrawal relief, 7.6% had withdrawal only and 2.0% reported withdrawal relief only.
Four-symptom definition of cannabis withdrawal: prevalence
Using the criteria and threshold for cannabis withdrawal proposed by Budney and colleagues (i.e. report of four or more of six specific symptoms) [10,22], along with report of recurrent episodes and distress or impairment, an estimated 17.8% had past year cannabis withdrawal at baseline and 11.2% had past year cannabis withdrawal over 1-year follow-up. We were not able to determine the presence of recurrent episodes of ‘withdrawal relief’ in the context of the four-symptom definition in this data set. Based on the four-symptom definition, withdrawal was among the least prevalent dependence symptoms at both time-points.
Latent class analysis (LCA) definition of cannabis withdrawal
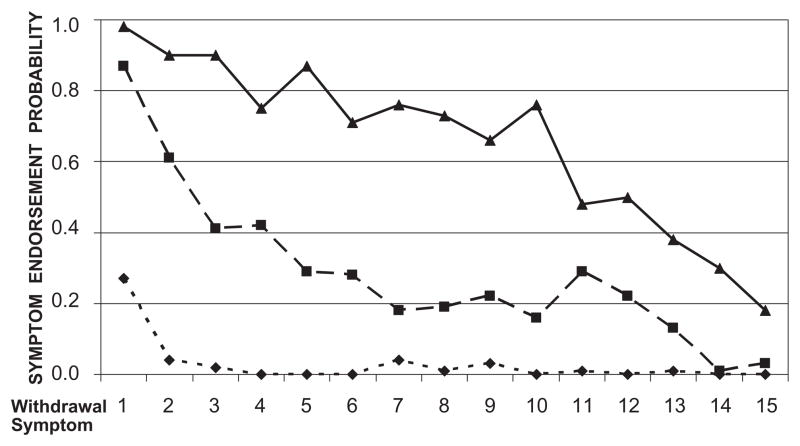
We applied LCA to 21 cannabis withdrawal symptoms (seizure was not included because it was not endorsed by any participant) assessed at baseline to determine the type and number of symptoms that distinguished subgroups of cannabis users. Results indicated that a three-class model provided the best fit to the data (BIC for the three-class model: 3113.61; four-class: 3161.56 and two-class: 3186.24). Six withdrawal symptoms were not statistically significant indicators of class membership in the three-class model (i.e. sweating, nausea, diarrhea/stomach ache, hallucinations, teary eyes/runny nose and muscle pains) and were therefore dropped. The three-class model remained the best-fitting solution among six models that were tested, even when these six symptoms were trimmed, and had high classification quality (average posterior probability of assignment to the most likely class ranged from 0.93–0.97). The three latent classes represented severity-based symptom profiles (Fig. 1) in which the number, rather than type of symptom, distinguished the classes. The average number of withdrawal symptoms in the low severity class (39.3% of the baseline sample) was 0.4 (SD = 0.6, range 0–2), for the moderate severity class (34.1%) was 4.2 (SD = 1.4, range 2–7) and for the highest severity class (26.6%) was 10.4 (SD = 2.8, range 7–17) symptoms. The latent classes provide some support for a two-symptom threshold to define withdrawal, but also suggest the utility of a higher threshold (i.e. >7 symptoms) to identify the most affected cases, if a broad range of symptoms (i.e. 15 symptoms) is queried.
Figure 1.
Symptom endorsement probabilities of cannabis withdrawal symptoms for the 3-class model. Withdrawal symptom numbers correspond to the numbering of cannabis withdrawal symptoms in Table 2. The solid line represents symptom endorsement probabilities for the severe class. The dashed lines represent the moderate and low severity classes. At baseline, the proportion in the low severity class was 39%, in the moderate severity class was 34%, and in the high severity class was 27%
After identifying severity-based classes of cannabis withdrawal using LCA, recurrence of withdrawal episodes was applied as an additional component of the LCA-based definition (note that subjective distress or impairment in functioning was determined at the symptom level). Requiring the recurrence of withdrawal episodes (i.e. three or more episodes within a 12-month period) resulted in a moderate severity class with recurrence (n = 43, 20.1% of the baseline sample) and a high severity class with recurrence (n = 37, 17.3%). No cases in the LCA low severity class reported recurrent episodes of withdrawal. Using LCA results, two possible definitions of withdrawal result: cases in the moderate or high severity classes with recurrence (‘LCA moderate to high severity’ definition: 37.4% of the baseline sample) versus all other cases, and cases in the high severity class with recurrence (‘LCA high severity’ definition: 17.3% of the baseline sample) versus all other cases. At 1 year, 20.8% of the follow-up sample had withdrawal according to the ‘LCA moderate to high severity’ definition, and 10.6% had withdrawal according to the ‘LCA high severity’ definition. Similar to the four-symptom definition of cannabis withdrawal, we were not able to determine post hoc the occurrence of ‘withdrawal relief’ according to LCA-based definitions in this data set.
Agreement between definitions of cannabis withdrawal
Computing agreement using kappa requires dichotomous variables. For LCA-derived subgroups, two dichotomous definitions of withdrawal were examined: ‘LCA moderate to high severity’ and ‘LCA high severity’ (described above). At baseline, there was perfect agreement (kappa = 1.00) between the two-symptom and the ‘LCA moderate to high severity definition’ (i.e. both definitions were based on a two-symptom threshold), and moderate agreement between the four-symptom and two-symptom definitions (kappa = 0.53; kappa is the same for agreement between the four-symptom and ‘LCA moderate to high severity’ definitions). For the LCA high severity definition, agreement with the two-symptom definition was moderate (kappa = 0.51), but agreement was high with the four-symptom definition (kappa = 0.91). A similar pattern of agreement was found using 1-year follow-up data. Because the two-symptom definition was completely redundant with the ‘LCA moderate to high severity’ definition, we focus on the LCA high severity definition in the concurrent and predictive validity analyses.
Concurrent validity of the three cannabis withdrawal definitions
The two-symptom, four-symptom and LCA high severity definitions of withdrawal all demonstrated concurrent validity in that those identified as having ‘withdrawal’ had, on average, more DSM-IV cannabis dependence symptoms and greater frequency of cannabis use at baseline (Table 3) and at 1-year follow-up (Table 4). Those with and without withdrawal did not differ on duration of cannabis use at baseline according to any withdrawal definition (P > 0.05). In addition, those with withdrawal according to any of the three definitions were more likely to endorse tolerance to cannabis and a stereotyped pattern of cannabis use at baseline and at 1-year follow-up (Tables 3 and 4). Of note, those who had withdrawal according to the two-symptom definition were more likely to report rapid reinstatement of dependence symptoms at baseline, although there was no statistically significant difference between those with and without withdrawal for the four-symptom and LCA high severity definitions on rapid reinstatement of dependence symptoms at baseline. At 1 year, however, those with withdrawal according to any of the three withdrawal definitions were more likely to report rapid reinstatement of dependence symptoms than those without withdrawal. In sum, all three definitions of withdrawal provided some demonstration of concurrent validity at baseline and at 1-year follow-up.
Table 3.
Concurrent validity of cannabis withdrawal definitions at baseline.
| Baseline | Two-symptom
|
Four-symptom
|
LCA high severity
|
|||
|---|---|---|---|---|---|---|
| Present mean (SD) | Absent mean (SD) | Present mean (SD) | Absent mean (SD) | Present mean (SD) | Absent mean (SD) | |
| DSM-IV cannabis abuse and dependence total symptom count (past year) | 6.1 (1.8) | 3.8 (2.2) | 6.7 (1.5) | 4.2 (2.3) | 6.8 (1.6) | 4.2 (2.3) |
| t(197) = −8.5, P = 0.00 | t(76) = −8.0, P= 0.00 | t(71) = −8.1, P = 0.00 | ||||
| DSM-IV cannabis dependence symptom count (past year) | 3.8 (1.2) | 2.2 (1.5) | 4.2 (1.1) | 2.5 (1.5) | 4.3 (1.1) | 2.5 (1.5) |
| t(193) = −8.5, P = 0.00 | t(212) = −6.5, P = 0.00 | t(212) = −6.7, P = 0.00 | ||||
| Frequency of cannabis use (past year) | 7.3 (1.3) | 6.2 (2.0) | 7.5 (1.4) | 6.4 (1.9) | 7.5 (1.4) | 6.4 (1.9) |
| t(209) = −5.1, P = 0.00 | t(67) = −4.1, P= 0.00 | t(63) = −4.1, P = 0.00 | ||||
| Duration of regular cannabis use (number of years of use) | 3.1 (1.6) | 2.9 (1.5) | 3.4 (1.7) | 2.9 (1.5) | 3.4 (1.6) | 2.9 (1.5) |
| t(157) = −0.9, P = 0.34 | t(212) = −1.8, P = 0.07 | t(212) = −1.9, P = 0.06 | ||||
| Baseline (past year) | Two-symptom
|
Four-symptom
|
LCA high severity
|
|||
|---|---|---|---|---|---|---|
| Present % | Absent % | Present % | Absent % | Present % | Absent % | |
| DSM-IV cannabis tolerance | 90.0 | 63.4 | 89.5 | 69.9 | 91.9 | 69.5 |
| χ2 (1) = 18.1, P = 0.00 | χ2 (1) = 6.1, P= 0.01 | χ2 (1) = 7.8, P = 0.01 | ||||
| Stereotyped pattern of use | 50.0 | 20.1 | 68.4 | 23.3 | 67.6 | 23.7 |
| χ2 (1) = 20.8, P = 0.00 | χ2 (1) = 29.6, P = 0.00 | χ2 (1) = 27.3, P = 0.00 | ||||
| Rapid reinstatement of symptoms | 22.5 | 11.2 | 23.7 | 13.6 | 21.6 | 14.1 |
| χ2 (1) = 4.9, P= 0.03 | χ2 (1) = 2.4, P= 0.12 | χ2 (1) = 1.3, P = 0.25 | ||||
‘LCA high severity’ definition distinguishes between two groups: youth in the ‘high severity’ cannabis withdrawal class versus youth in ‘moderate’ and ‘low’ severity cannabis withdrawal classes. LCA: latent class analysis; SD: standard deviation.
Table 4.
Concurrent validity of cannabis withdrawal definitions at 1-year follow-up.
| 1-year follow-up (past year) | Two-symptom
|
Four-symptom
|
LCA high severity
|
|||
|---|---|---|---|---|---|---|
| Present mean (SD) | Absent mean (SD) | Present mean (SD) | Absent mean (SD) | Present mean (SD) | Absent mean (SD) | |
| DSM-IV cannabis abuse and dependence total symptom count | 4.7 (1.8) | 2.0 (2.0) | 5.4 (1.9) | 2.2 (2.1) | 5.3 (1.9) | 2.3 (2.1) |
| t(195) = −7.5, P = 0.00 | t(195) = −6.7, P = 0.00 | t(195) = −6.2, P = 0.00 | ||||
| DSM-IV cannabis dependence symptom count | 3.0 (1.2) | 1.3 (1.2) | 3.4 (1.2) | 1.4 (1.3) | 3.4 (1.2) | 1.4 (1.3) |
| t(195) = −8.2, P = 0.00 | t(195) = −6.9, P = 0.00 | t(195) = −6.7, P = 0.00 | ||||
| Frequency of cannabis use | 7.0 (1.5) | 4.5 (2.7) | 6.8 (1.8) | 4.8 (2.7) | 6.8 (1.9) | 4.8 (2.7) |
| t(115) = −7.9, P = 0.00 | t(34) = −4.6, P= 0.00 | t(31) = −4.4, P = 0.00 | ||||
| 1-year follow-up (past year) | Two-symptom
|
Four-symptom
|
LCA high severity
|
|||
|---|---|---|---|---|---|---|
| Present % | Absent % | Present % | Absent % | Present % | Absent % | |
| DSM-IV cannabis tolerance | 88.1 | 44.5 | 90.9 | 49.1 | 90.5 | 49.4 |
| χ2 (1) = 25.2, P = 0.00 | χ2 (1) = 13.7, P = 0.00 | χ2 (1) = 13.0, P = 0.00 | ||||
| Stereotyped pattern of use | 42.9 | 4.5 | 54.5 | 7.4 | 57.1 | 7.4 |
| χ2 (1) = 43.8, P = 0.00 | χ2 (1) = 39.2, P = 0.00 | χ2 (1) = 41.9, P = 0.00 | ||||
| Rapid reinstatement of symptoms | 35.7 | 11.6 | 40.9 | 13.7 | 38.1 | 14.2 |
| χ2 (1) = 13.8, P = 0.00 | χ2 (1) = 10.4, P = 0.00 | χ2 (1) = 7.7, P = 0.01 | ||||
‘LCA high severity’ definition distinguishes between two groups: youth in the ‘high severity’ cannabis withdrawal class versus youth in ‘moderate’ and ‘low’ severity cannabis withdrawal classes. LCA: latent class analysis; SD: standard deviation.
Predictive validity of the three cannabis withdrawal definitions
To test the predictive validity of the three definitions of withdrawal (i.e. two-symptom, four-symptom and LCA high severity definitions), a series of simultaneous multiple regression analyses were conducted, using each definition as a predictor of the following 1-year outcomes: past year DSM-IV cannabis abuse and dependence symptom count, past year DSM-IV cannabis dependence symptom count, past year frequency of cannabis use, number of 30-day periods of abstinence over follow-up, maximum consecutive days of abstinence over follow-up and 7- and 30-day point prevalence abstinence at 1 year. The only outcomes predicted by baseline cannabis withdrawal (P < 0.05) were past year DSM-IV cannabis dependence symptom count (Table 5) [39] and past year DSM-IV cannabis abuse and dependence symptom count. Among the three withdrawal definitions tested, only the four-symptom [β = 0.18 (standardized beta weight), P = 0.006] and high severity LCA definitions (β = 0.24, P = 0.002) predicted DSM-IV cannabis dependence symptoms at 1 year (and DSM-IV cannabis abuse and dependence symptoms at 1 year). Post-hoc analyses to probe the absence of an association between the different baseline definitions of cannabis withdrawal and frequency of cannabis use over follow-up generally indicated a bi-modal distribution in which those with baseline cannabis withdrawal (by any of the three definitions) reported either relatively low or high levels of cannabis use over follow-up, resulting in predictive associations at 1 year that were not statistically significant.
Table 5.
Three definitions of cannabis withdrawal as predictors of DSM-IV cannabis dependence symptom count at 1-year follow-up (n = 197).
| Baseline predictor | B | SE B | β |
|---|---|---|---|
| Sex | 0.53 | 0.23 | 0.17* |
| Age | 0.04 | 0.10 | 0.03 |
| Ethnicity | 0.94 | 0.35 | 0.20** |
| SES | −0.19 | 0.10 | −0.14 |
| Past year alcohol diagnosis (yes/no) | −0.06 | 0.14 | −0.03 |
| Past year conduct disorder symptom count | 0.06 | 0.06 | 0.08 |
| Life-time number of other drugs used | 0.06 | 0.06 | 0.08 |
| Past year depression diagnosis (yes/no) | −0.10 | 0.23 | −0.03 |
| Past year anxiety diagnosis (yes/no) | 0.13 | 0.34 | 0.03 |
| Past year ADHD diagnosis (yes/no) | 0.30 | 0.27 | 0.08 |
| Past year frequency of cannabis use | 0.08 | 0.06 | 0.10 |
| Two-symptom withdrawal | 0.31 | 0.22 | 0.10 |
| Sex | 0.54 | 0.22 | 0.17* |
| Age | 0.03 | 0.09 | 0.03 |
| Ethnicity | 0.93 | 0.34 | 0.20** |
| SES | −0.18 | 0.10 | −0.14 |
| Past year alcohol diagnosis (yes/no) | −0.12 | 0.14 | −0.03 |
| Past year conduct disorder symptom count | 0.04 | 0.06 | 0.08 |
| Life-time number of other drugs used | 0.04 | 0.06 | 0.08 |
| Past year depression diagnosis (yes/no) | −0.12 | 0.23 | −0.03 |
| Past year anxiety diagnosis (yes/no) | 0.18 | 0.34 | 0.03 |
| Past year ADHD diagnosis (yes/no) | 0.24 | 0.27 | 0.08 |
| Past year frequency of cannabis use | 0.07 | 0.06 | 0.10 |
| Four-symptom withdrawal | 0.79 | 0.29 | 0.18** |
| Sex | 0.56 | 0.22 | 0.18* |
| Age | 0.03 | 0.09 | 0.02 |
| Ethnicity | 0.92 | 0.34 | 0.20** |
| SES | −0.17 | 0.10 | −0.12 |
| Past year alcohol diagnosis (yes/no) | −0.11 | 0.13 | −0.06 |
| Past year conduct disorder symptom count | 0.04 | 0.06 | 0.06 |
| Life-time number of other drugs used | 0.04 | 0.06 | 0.05 |
| Past year depression diagnosis (yes/no) | −0.16 | 0.23 | −0.05 |
| Past year anxiety diagnosis (yes/no) | 0.21 | 0.34 | 0.04 |
| Past year ADHD diagnosis (yes/no) | 0.18 | 0.27 | 0.05 |
| Past year frequency of cannabis use | 0.07 | 0.06 | 0.09 |
| LCA high severity withdrawal | 0.90 | 0.29 | 0.24** |
Predictors were entered simultaneously in all regression analyses. SES: socio-economic status; ADHD: attention deficit hyperactivity disorder; LCA: latent class analysis. ‘LCA high severity’ definition distinguishes between two groups: youth in the ‘high severity’ cannabis withdrawal class versus youth in ‘moderate’ and ‘low’ severity cannabis withdrawal classes; B: unstandardized beta weight; SE B: standard error of the unstandardized beta weight; β: standardized beta weight (indication of effect size).
P < 0.05;
P < 0.01.
Effect sizes for the four-symptom and LCA high severity withdrawal definition are generally considered ‘small effects’ [39]. Results using the number of cannabis abuse and dependence symptoms at 1 year generated similar results (i.e. only the four-symptom and LCA high severity definitions predicted the number of cannabis abuse and dependence symptoms at 1-year follow-up).
DISCUSSION
This study contrasted three operational definitions of cannabis withdrawal in a sample of treated adolescents followed over 1 year, and is the first to examine the predictive validity of cannabis withdrawal in adolescents. A two-symptom definition had relatively high prevalence, and showed some concurrent validity in that those with withdrawal reported more DSM-IV cannabis dependence symptoms than those without withdrawal, at baseline and at 1 year. This relatively mild definition, however, did not demonstrate predictive validity at 1 year. In contrast, the four-symptom definition of cannabis withdrawal proposed by Budney and colleagues [10,22] had relatively low prevalence but, as hypothesized, did predict number of cannabis dependence symptoms at 1-year follow-up (as well as total number of cannabis abuse and dependence symptoms at follow-up). LCA, which was used to derive empirically a definition of cannabis withdrawal that would specify the number and type of symptoms that best distinguished groups of users, coincidentally derived groupings that were wholly redundant with (i.e. two-symptom definition) or very similar to (i.e. four-symptom definition) two definitions of cannabis withdrawal that have been described in the literature. Among possible LCA-based definitions of cannabis withdrawal, only the LCA high severity definition (which identified a group of users that was similar to the four-symptom definition) demonstrated predictive validity at 1 year. Demonstration of the predictive validity of relatively severe definitions of cannabis withdrawal supports its inclusion as a ‘course specifier’ of cannabis dependence [1], and argues for the specification of a cannabis withdrawal syndrome in DSM-V and ICD-11.
The cannabis withdrawal symptoms reported most frequently by adolescents in this study were similar to findings reported in other studies of adolescents (e.g. [17–21]), as well as adults [10], in that the most common symptoms were primarily psychological (e.g. irritable) rather than physical (e.g. nausea). The comparability of commonly reported cannabis withdrawal symptoms across studies provides some additional support for the validity of a cannabis withdrawal syndrome in both adolescents and adults. In addition, the similarity of prevalence estimates of cannabis withdrawal among treated adolescents [18] to this study’s two-symptom definition of withdrawal, and of withdrawal relief, suggest that some previous reports (e.g. [18]) used a relatively low threshold to determine the presence of cannabis withdrawal. Although use of a low threshold to determine cannabis withdrawal (i.e. two-symptom threshold) demonstrated some concurrent validity, withdrawal definitions that used a relatively low threshold had limited predictive validity at 1-year follow-up.
Those who argue against the inclusion of cannabis withdrawal as a criterion to be used in diagnosing cannabis dependence have cited the need for a clear operational definition of the syndrome, particularly with regard to a clinically significant profile of cannabis withdrawal symptoms. In this study, clinical significance was determined at the symptom level; that is, each cannabis withdrawal symptom that was rated as present needed to result in subjective distress or impairment in functioning. The application of LCA to a broad array of potential cannabis withdrawal symptoms indicated that the number, rather than type of withdrawal symptom, best distinguished subgroups of users based on individual reports of cannabis withdrawal symptom profiles. Concurrent and predictive validity analyses of the LCA high severity definition of cannabis withdrawal support further investigation of this LCA-based definition with regard to implications for treatment (e.g. development of interventions to help manage withdrawal) and refining diagnostic algorithms.
Given the high level of agreement between the LCA high severity and four-symptom definitions of cannabis withdrawal, the four-symptom definition may be preferred based on parsimony and efficiency of assessment. Specifically, whereas the LCA high severity definition used a higher threshold (i.e. >7 symptoms) and broader range of symptoms (i.e. 15 symptoms) to identify withdrawal, the four-symptom definition specified a smaller pool of six specific withdrawal symptoms, of which four or more needed to be met (note that all definitions tested in this study required recurrent episodes of withdrawal and evidence of the clinical significance of symptoms). Based on similar prevalence and performance with regard to concurrent and predictive validity, as well as efficiency in assessment (need to query 15 symptoms for LCA high severity definition versus six symptoms for the four-symptom definition), the four-symptom definition of withdrawal has distinct advantages over the empirically derived LCA high severity definition.
Findings for some concurrent validity analyses did not appear to support the more severe definitions of cannabis withdrawal. In particular, the more stringent withdrawal definitions (i.e. four-symptom and LCA high severity definitions) were not associated with rapid reinstatement of dependence symptoms at baseline, whereas the two-symptom definition was associated with the rapid reinstatement symptom at baseline. This result may have occurred due to the use of a treated sample of adolescents who may not attempt to limit cannabis use until there is a clear need to do so (e.g. treatment), particularly among more heavy users, who may have greater withdrawal severity. Thus, prior to baseline, heavier users with greater withdrawal severity tend to have fewer periods of reduced cannabis use prior to baseline, and less opportunity for dependence symptoms to be reinstated because there has not been a significant reduction in use. In partial support of this explanation, at 1-year follow-up all three definitions of cannabis withdrawal were associated with rapid reinstatement of dependence symptoms.
Cannabis withdrawal at baseline, variously defined, did not predict frequency of cannabis use over 1-year follow-up, although it did predict number of cannabis dependence symptoms at 1 year, and number of cannabis abuse and dependence symptoms at follow-up. Post-hoc analyses indicated that among adolescents with cannabis withdrawal at baseline (according to any of the three definitions tested) there was generally a bi-modal distribution in the frequency of cannabis use over follow-up. Although some youth with baseline cannabis withdrawal reported relatively low frequency of use over follow-up, others continued to engage in a relatively heavy pattern of use. By contrast, baseline cannabis withdrawal (i.e. four-symptom and LCA high severity definition) did predict DSM-IV cannabis abuse and dependence symptoms over follow-up. These results suggest that DSM-IV abuse and dependence symptoms capture aspects of use (e.g. difficulty reducing use, prioritizing cannabis use over other activities) that are not well indexed by frequency of cannabis use alone. Similarly, outcome variables representing periods of abstinence have similar limitations with regard to capturing cannabis-related symptoms that are not represented directly by periods of abstinence. In addition, the absence of a difference in number of years of regular cannabis use at baseline between those with and without cannabis withdrawal, variously defined, may be due to the use of a treatment seeking sample of adolescents who have generally short use histories.
Research suggests that DSM-IV defined withdrawal generally performs favorably as an indicator of dependence severity and more chronic course across a range of substances. For example, DSM-IV alcohol withdrawal has been associated cross-sectionally and prospectively with greater severity of alcohol-related problems [e.g. 40–42]. For other substances, such as cannabis, cocaine, amphetamines and opiates, report of withdrawal predicted greater substance-related problems cross-sectionally, as well as more chronic course in adults [14]. Few studies, however, have used empirically based methods to determine the number and type of withdrawal symptoms that would optimize concurrent and predictive validity for a given substance. This study is among the first to apply an empirically based method (i.e. LCA) to determine the number and type of cannabis withdrawal symptoms that would maximize validity, and provides support for more stringent or ‘narrow’ definitions of cannabis withdrawal (i.e. four-symptom and LCA high severity definitions) compared to definitions using a lower threshold (e.g. two-symptom), particularly with regard to predictive validity at 1 year in treated adolescents.
Certain study limitations warrant comment. Data on the occurrence of cannabis withdrawal symptoms, frequency of substance use and substance-related problems were based on retrospective self-report, and may be subject to recall bias or minimization. However, efforts to optimize valid reporting of substance use data were made (e.g. biochemical verification of cannabis use). Retention over follow-up was high; however, greater loss of youth who reported relatively high frequency of use and more severe cannabis-related problems, as well as those of higher SES, suggest some possible bias in the sample followed at 1 year that may affect the generalizability of results. In addition, the relatively low number of ethnic minority youth included in the sample raises another caveat regarding the generalizability of study results. The validity analyses focused on the presence of DSM-IV substance use disorder criteria, and did not examine specifically the validity of the definitions against ICD-10 cannabis dependence criteria, although concordance is generally high across the two systems (e.g. [43]).
The determination of whether to include cannabis withdrawal as an indicator of dependence in the next iterations of DSM and ICD needs to consider the operational definition of the symptom that will maximize clinical utility and validity across a wide range of ages, cultural influences, and for males and females. The criteria for defining cannabis withdrawal proposed by Budney and colleagues [10,22] holds promise as an indicator of cannabis-related problems over follow-up. However, further research on the prevalence and performance characteristics of this, and alternative definitions of cannabis withdrawal, are needed urgently to inform revisions to cannabis use disorder criteria leading to DSM-V and ICD-11.
Acknowledgments
This research and the preparation of this manuscript were supported by National Institute on Alcohol Abuse and Alcoholism K01 AA00324 and R01 AA014357.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) 4. Washington, DC: American Psychiatric Association; 2000. text revision. [Google Scholar]
- 2.World Health Organization. International Classification of Diseases. [accessed 18 June 2007];Mental and Behavioural Disorders Due to Substance Use. (10). 2007 :F10–F19. Available at: http://www.who.int/substance_abuse/terminology/ICD10ResearchDiagnosis.pdf.
- 3.Smith NT. A review of the published literature into cannabis withdrawal symptoms in human users. Addiction. 2002;97:621–32. doi: 10.1046/j.1360-0443.2002.00026.x. [DOI] [PubMed] [Google Scholar]
- 4.Lichtman AH, Martin BR. Marijuana withdrawal syndrome in the animal model. J Clin Pharmacol. 2002;42:20S–27S. doi: 10.1002/j.1552-4604.2002.tb05999.x. [DOI] [PubMed] [Google Scholar]
- 5.Budney AJ, Hughes JR, Moore BA, Novy P. Marijuana abstinence effects in marijuana smokers maintained in their home environment. Arch Gen Psychiatry. 2001;58:917–24. doi: 10.1001/archpsyc.58.10.917. [DOI] [PubMed] [Google Scholar]
- 6.Budney AJ, Moore BA, Vandrey R, Hughes JR. The time course and significance of cannabis withdrawal. J Abnorm Psychol. 2003;3:393–402. doi: 10.1037/0021-843x.112.3.393. [DOI] [PubMed] [Google Scholar]
- 7.Copersino ML, Boyd SJ, Tashkin DP, Huestis MA, Heishman SJ, Dermand JC, et al. Cannabis withdrawal among non-treatment-seeking adult cannabis users. Am J Addict. 2006;15:8–14. doi: 10.1080/10550490500418997. [DOI] [PubMed] [Google Scholar]
- 8.Budney AJ, Novy PL, Hughes JR. Marijuana withdrawal among adults seeking treatment for marijuana dependence. Addiction. 1999;94:1311–21. doi: 10.1046/j.1360-0443.1999.94913114.x. [DOI] [PubMed] [Google Scholar]
- 9.Vandrey RG, Budney AJ, Moore BA, Hughes JR. A cross-study comparison of cannabis and tobacco withdrawal. Am J Addict. 2005;14:54–63. doi: 10.1080/10550490590899853. [DOI] [PubMed] [Google Scholar]
- 10.Budney AJ, Hughes JR, Moore BA, Vandrey R. Review of the validity and significance of cannabis withdrawal syndrome. Am J Psychiatry. 2004;161:1967–77. doi: 10.1176/appi.ajp.161.11.1967. [DOI] [PubMed] [Google Scholar]
- 11.Kouri EM, Pope HG. Abstinence symptoms during withdrawal from chronic marijuana use. Exp Clin Psychopharmacol. 2000;8:483–92. doi: 10.1037//1064-1297.8.4.483. [DOI] [PubMed] [Google Scholar]
- 12.Jones RT, Benowitz N, Bachman J. Clinical studies of cannabis tolerance and dependence. Ann NY Acad Sci. 1976;282:221–39. doi: 10.1111/j.1749-6632.1976.tb49901.x. [DOI] [PubMed] [Google Scholar]
- 13.Haney M, Ward AS, Comer SD, Foltin RW, Fischman MW. Abstinence symptoms following smoked marijuana in humans. Psychopharmacology (Berl) 1999;14:395–404. doi: 10.1007/s002130050849. [DOI] [PubMed] [Google Scholar]
- 14.Schuckit MA, Daeppen JB, Danko GP, Tripp ML, Smith TL, Li T-K, et al. Clinical implications for four drugs of the DSM-IV distinction between substance dependence with and without a physiological component. Am J Psychiatry. 1999;156:41–9. doi: 10.1176/ajp.156.1.41. [DOI] [PubMed] [Google Scholar]
- 15.Cottler LB, Schuckit MA, Helzer JE, Crowley TJ, Woody G, Nathan P, et al. The DSM-IV field trial for substance use disorders: major results. Drug Alcohol Depend. 1995;38:59–69. doi: 10.1016/0376-8716(94)01091-x. [DOI] [PubMed] [Google Scholar]
- 16.Substance Abuse and Mental Health Services Administration (SAMHSA), Office of Applied Studies. National Admissions to Substance Abuse Treatment Services, DASIS Series: S-31, DHHS Publication no. (SMA) 06-4140. Rockville, MD: SAMHSA; 2006. Treatment Episode Data Set (TEDS). Highlights—2004. [Google Scholar]
- 17.Young SE, Corley RP, Stallings MC, Rhee SH, Crowley TJ, Hewitt JK. Substance use, abuse and dependence in adolescence: prevalence, symptom profiles and correlates. Drug Alcohol Depend. 2002;68:309–22. doi: 10.1016/s0376-8716(02)00225-9. [DOI] [PubMed] [Google Scholar]
- 18.Crowley TJ, Macdonald MJ, Whitmore EA, Mikulich SK. Cannabis dependence, withdrawal, and reinforcing effects among adolescents with conduct symptoms and substance use disorders. Drug Alcohol Depend. 1998;50:27–37. doi: 10.1016/s0376-8716(98)00003-9. [DOI] [PubMed] [Google Scholar]
- 19.Mikulich SK, Hall SK, Whitmore EA, Crowley TJ. Concordance between DSM-III-R and DSM-IV diagnoses of substance use disorders in adolescents. Drug Alcohol Depend. 2001;61:237–48. doi: 10.1016/s0376-8716(00)00143-5. [DOI] [PubMed] [Google Scholar]
- 20.Vandrey RG, Budney AJ, Kamon JL, Stanger C. Cannabis withdrawal in adolescent treatment seekers. Drug Alcohol Depend. 2005;78:205–10. doi: 10.1016/j.drugalcdep.2004.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dawes MA, Liguori A, Dougherty DM. Cannabis withdrawal among adolescent cannabis users in an outpatient research setting. Am J Addict. 2006;15:485–6. doi: 10.1080/10550490601000637. [DOI] [PubMed] [Google Scholar]
- 22.Budney AJ, Hughes JR. The cannabis withdrawal syndrome. Curr Opin Psychiatry. 2006;19:233–8. doi: 10.1097/01.yco.0000218592.00689.e5. [DOI] [PubMed] [Google Scholar]
- 23.Budney AJ. Are specific dependence criteria necessary for different substances: how can research on cannabis inform in press? Addiction. 2006;101:125–33. doi: 10.1111/j.1360-0443.2006.01582.x. [DOI] [PubMed] [Google Scholar]
- 24.McCutcheon AL. Latent Class Analysis. Beverly Hills: Sage Publications; 1987. [Google Scholar]
- 25.Chung T, Martin CS. Classification and short-term course of cannabis, hallucinogen, cocaine, and opioid disorders in treated adolescents. J Consult Clin Psychol. 2005;73:995–1004. doi: 10.1037/0022-006X.73.6.995. [DOI] [PubMed] [Google Scholar]
- 26.Wiesbeck GA, Schuckit MA, Kalmijn JA, Tipp JE, Bucholz KK, Smith TL. An evaluation of the history of a marijuana withdrawal syndrome in a large population. Addiction. 1996;91:1469–78. [PubMed] [Google Scholar]
- 27.Hollingshead A. Four-Factor Index of Social Status. New Haven: Author; 1975. [Google Scholar]
- 28.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 29.Martin CS, Kaczynski NA, Maisto SA, Bukstein OG, Moss HB. Patterns of DSM-IV alcohol abuse and dependence symptoms in adolescent drinkers. J Stud Alcohol. 1995;56:672–80. doi: 10.15288/jsa.1995.56.672. [DOI] [PubMed] [Google Scholar]
- 30.Edwards G, Gross M. Alcohol dependence: provisional description of a clinical syndrome. Br Med J. 1976;1:1058–61. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung T, Martin CS, San Pedro R, Shriberg RF, Cornelius JR. Retest reliability and discrepancy interview for DSM-IV alcohol, cannabis, and nicotine diagnoses in treated adolescents. Alcohol Clin Exp Res. 2004;28:111A. [Google Scholar]
- 32.Skinner H. Development and Validation of a Lifetime Alcohol Consumption Assessment Procedure. Toronto: Addiction Research Foundation; 1982. Substudy no. 1248. [Google Scholar]
- 33.Puig-Antich J, Orvaschel H, Tabrizi M, Chambers W. Adaptation of Schedule for Affective Disorders and Schizophrenia for School Age Children, Epidemiologic Version, Kiddie-SADS-E. New York: New York State. Psychiatric Institute, Department of Child and Adolescent Psychiatry; 1981. [Google Scholar]
- 34.Chung T, Maisto SA. Review and reconsideration of relapse as a change point in clinical course in treated adolescents. Clin Psychol Rev. 2006;26:149–61. doi: 10.1016/j.cpr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 35.Clark DB, Parker AM, Lynch KG. Psychopathology and substance-related problems during early adolescence: a survival analysis. J Clin Child Psychol. 1999;28:333–41. doi: 10.1207/S15374424jccp280305. [DOI] [PubMed] [Google Scholar]
- 36.Vermunt JK, Magidson J. Latent GOLD 4.0 User’s Guide. Belmont, MA: Statistical Innovations Inc; 2005. [Google Scholar]
- 37.Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6:461–4. [Google Scholar]
- 38.Fleiss JL. Statistical Methods for Rates and Proportions. 2. New York: John Wiley and Sons; 1981. [Google Scholar]
- 39.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. New Jersey: Lawrence Erlbaum; 1988. [Google Scholar]
- 40.Schuckit MA, Danko GP, Smith TL, Hesselbrock V, Kramer J, Bucholz K. A 5-year prospective evaluation of DSM-IV alcohol dependence with and without a physiological component. Alcohol Clin Exp Res. 2003;27:818–25. doi: 10.1097/01.ALC.0000067980.18461.33. [DOI] [PubMed] [Google Scholar]
- 41.Bucholz KK, Heath AC, Reich T, Hesselbrock VM, Kramer JR, Nurnberger JI, Jr, et al. Can we subtype alcoholism? A latent class analysis of data from relatives of alcoholics in a multi-center family study of alcoholism. Alcohol Clin Exp Res. 1996;20:1462–71. doi: 10.1111/j.1530-0277.1996.tb01150.x. [DOI] [PubMed] [Google Scholar]
- 42.Langenbucher J, Martin C, Labouvie E, Sanjuan P, Bavly L, Pollock N. Toward the DSM-V: the withdrawal-gate model versus the DSM-IV in the diagnosis of alcohol abuse and dependence. J Consult Clin Psychol. 2000;68:799–809. [PubMed] [Google Scholar]
- 43.Pollock NK, Martin CS, Langenbucher JW. Diagnostic concordance of DSM-III, DSM-III-R, DSM-IV and ICD-10 alcohol diagnoses in adolescents. J Stud Alcohol Drugs. 2000;61:439–46. doi: 10.15288/jsa.2000.61.439. [DOI] [PubMed] [Google Scholar]