Abstract
Background
Patients in home health care (HHC), the fastest growing health care sector, are at risk for infection. The existing research on infection in HHC is often limited by small sample sizes, local scope of inquiry, and a lack of current data. There is no national study examining agency-level infection rates.
Methods
This secondary data analysis used a 20% random sample of the 2010 national Outcome and Assessment Information Set (OASIS) data. An infection case was identified when the HHC patient was hospitalized or received emergency care for respiratory infection, urinary tract infection, intravenous catheter-related infection, wound infection, or deterioration. Proportions of infection cases out of the total number of patients were calculated for the whole sample and for each HHC agency.
Results
The final analysis included 199,462 patients from 8,255 HHC agencies. Approximately 3.5% of patients developed infections during their HHC stay, leading to emergency care treatment or hospitalization. Seventeen percent of unplanned hospitalizations among HHC patients were caused by infections. The agency-level infection rate ranged from 0%–34%, with an average of 3.5%.
Conclusion
To our knowledge, this is the first study to examine the proportion of hospitalizations or emergency care treatment caused by infection in HHC and the agency-level infection rate at a national level by using OASIS data. These data demonstrate that infection is a serious problem in HHC, and infection rates varied between agencies. The variance in agency level rates may be caused by differences in infection control policies and practices. Better infection surveillance system in HHC is needed to benchmark quality of care.
Keywords: Infection, Home health care, Outcome and Assessment Information Set
There has been a dramatic change in American health care delivery since the 1970s, with many acutely ill patients moving out of hospitals to their communities1 because of the impetus for decreased length of hospital stay and the advancement of medical technologies.2–4 The ability to reduce health care costs and maintain patients’ dignity and independence by providing health care in their homes2–4 has made home health care (HHC) a booming business. In 2009, >$72.2 billion was spent in HHC.5 Approximately 12 million patients received health care services from HHC agencies nationwide in 2010, with more than two-thirds (69%) being ≥65 years,5 a statistic expected to increase as the American population ages.6
The increasing number of acutely ill patients with complex conditions now receiving medical care at home has brought many issues to light, including increased risk of infection. In the home environment with uncontrolled sanitation hazards,7 acutely ill patients with complex medical conditions self-manage or receive health care from family members or friends who have little or no formal health care training. This, along with the increased use of medical devices in the home, places these patients at high risk.1
In the 1990s, 3 infection outbreaks were reported in HHC patients and captured national attention; all were related to indwelling catheters.8–10 Since then, researchers have sporadically focused on infections in HHC patients and reported that infection was prevalent in HHC settings.11–16 A 2002 landmark article17 estimated that 1.2 million infections occur in HHC annually and suggested a need for national infection surveillance in HHC. To date, such a surveillance system has not been established.
In a recently published systematic review,18 25 research articles exploring infections and risk factors in HHC settings published since 1990 were examined. In this review, the authors found most researchers focused on patients with home parenteral nutrition treatment and reported a wide range of infection rates for this patient population from 0.48–10.04 infections per 1,000 device days (or 14%–80% using the definition of proportion of infected patients out of total HHC patients). Only a few researchers examined infection rates in general HHC patient populations, and they found that 4.5%–11.5% of HHC patients had at least 1 episode of infection during their HHC stay. In this review, the authors also reported that 82% of the studies used data collected before 2005,18 which limits the generalizability of the findings to current practice. Furthermore, most of the published studies examined infections in a single HHC agency with small sample sizes, which failed to provide a full picture of infection at a national level. None of the previous studies examined how many HHC patients were hospitalized or received emergency care treatment because of infection or studied infection rates at the agency level. Therefore, to address the knowledge gap, the objectives of this study were to describe the rates of hospitalization and emergency care use caused by infection among patients receiving HHC and compare reported infection rates between HHC agencies.
METHODS
This was a secondary data analysis of a 20% random sample of the 2010 national Outcome and Assessment Information Set (OASIS) data.
OASIS data
OASIS, developed in 1999 by the Health Care Financing Administration in collaboration with the Center for Health Sciences and Policy Research to monitor the quality of HHC with a standardized, comprehensive, reproducible assessment instrument, serves the purpose of outcome-based quality improvement. OASIS assessment is required for all Medicare-certified HHC agencies as part of a comprehensive assessment for all patients ≥18 years who are receiving skilled care and are reimbursed by Medicare or Medicaid, with an exception of pre- or postnatal patients.19 HHC patients are assessed using OASIS at different time points: admission or readmission to HHC (start of care or resumption of care after inpatient stay); when there is any change of health status indicated by transfer to inpatient facility, death, or discharge from home care; or when a patient’s HHC stay reaches a 60-day time point. The OASIS data are collected by registered nurses or therapists with a variety of strategies being used to obtain a comprehensive assessment. These strategies include observation, interview, review of pertinent documentation (eg, hospital discharge summaries to obtain information on inpatient facility procedures and diagnoses), discussions with other care team members where relevant (eg, phone calls to the physician to verify diagnoses), and measurement (eg, wound length and width, intensity of pain).19 Detailed instructions for data collection are specified in OASIS User Manuals.19 Web-based OASIS training is also provided to assist HHC in accurately completing OASIS assessment.20 OASIS data have been used to examine HHC patient outcomes other than infection21–23 and has a high level of interrater reliability.24
Variables
We used 2 OASIS items to identify infections: (1) M2310, which describes the reasons why a HHC patient received emergency care (with or without hospitalization) and is collected whenever the patient transfers to an inpatient facility or is discharged from HHC; and (2) M2430, which describes the reason why a HHC patient is hospitalized. Both items include 18 medical conditions, 4 of which are related to infections: respiratory infection (eg, pneumonia, bronchitis), urinary tract infection, intravenous (IV) catheter-related infection, and wound infection or deterioration. In this analysis, an infection case is identified if OASIS indicates that a patient received emergency care or was transferred to hospital for any of the 4 types of infection. No microbiologic information was used in infection diagnosis in OASIS. Given the nature of the OASIS data collection, the infection case reported throughout this article is the infection reported by nurses or therapists as the reason for hospitalization or emergency care treatment.
Statistical analysis
After institutional review board approval from Columbia University Medical Center was received, deidentified 2010 OASIS data were obtained from the Centers for Medicare and Medicaid. For this analysis, we used a 20% random national sample. If patients had multiple HHC admissions, only the first HHC stay was included. Using Stata 12.1 software (StataCorp, College Station, TX), proportions of infection cases were calculated for the whole sample and for each HHC agency. A comparison of the demographic and clinical characteristics (ie, age, sex, past inpatient admission, diagnosis at HHC admission) of those with and without infection were conducted using t tests and χ2 tests.
RESULTS
Study population characteristics
The sample included 199,462 HHC patients from 8,255 HHC agencies. As summarized in Table 1, the average age was 75 years, with 82.8% patients being ≥65 years. More than 60% of the patients were women. Most were Caucasian (75.6%) and were insured by the Medicare fee-for-service (70.4%). About half had had an inpatient facility stay, primarily in an acute care hospital, within 14 days prior to the HHC admission. The top 5 diagnoses for the HHC admission were unspecified congestive heart failure, hypertension, after care after joint replacement or circulatory system surgery, and diabetes mellitus without complications. Approximately 1.7% (n = 3,388) of the patients had an infection when they were admitted to HHC. A small number of patients had cancer (6.7%) or renal disease (13.9%) when entering HHC.
Table 1.
Characteristics of home health care patients (n = 199,462)*
| Patient characteristics | Total (N = 199,462) | Patients with infection (n = 7,018) | Patients without infection (n = 192,444) | P value |
|---|---|---|---|---|
| Mean age ± SD (y) | 75.1 ± 13.4 | 73.7 ± 14.6 | 75.1 ± 13.4 | .00 |
| Age ≥65 y | 82.8 | 78.1 | 83 | .00 |
| Female | 63 | 57.8 | 63.2 | .00 |
| Ethnicity | .00 | |||
| White | 75.6 | 78.8 | 75.5 | |
| Black | 14.0 | 12.5 | 14.0 | |
| Hispanic | 8.0 | 6.5 | 8.1 | |
| Asian | 1.7 | 1.2 | 1.8 | |
| Other | 0.7 | 0.9 | 0.7 | |
| Payer | .00 | |||
| Medicare (fee-for-service) | 70.4 | 69.2 | 70.4 | |
| Medicare (health maintenance organization-managed care) | 16.0 | 15.2 | 16.0 | |
| Medicaid | 10.0 | 11.7 | 9.8 | |
| Private insurance | 3.8 | 4.0 | 3.8 | |
| Past inpatient facility discharge in prior 14 d | .00 | |||
| None | 34.6 | 25.9 | 35.0 | |
| Short-stay acute hospital | 44.6 | 50.0 | 44.4 | |
| Inpatient rehabilitation hospital or unit | 6.4 | 6.8 | 6.4 | |
| Skilled nursing facility | 14.1 | 15.8 | 14.0 | |
| Long-term care facility | 2.8 | 3.9 | 2.8 | |
| Admission diagnosis | ||||
| Infection | 1.7 | 1.5 | 1.7 | .13 |
| Cancer | 6.7 | 8.6 | 6.6 | .00 |
| Renal disease | 13.9 | 18.9 | 13.7 | .00 |
| Receiving intravenous therapy or parenteral nutrition | 3.0 | 5.5 | 2.9 | .00 |
NOTE. Values are percentages unless otherwise indicated.
t tests or χ2 tests were used to test the group comparison.
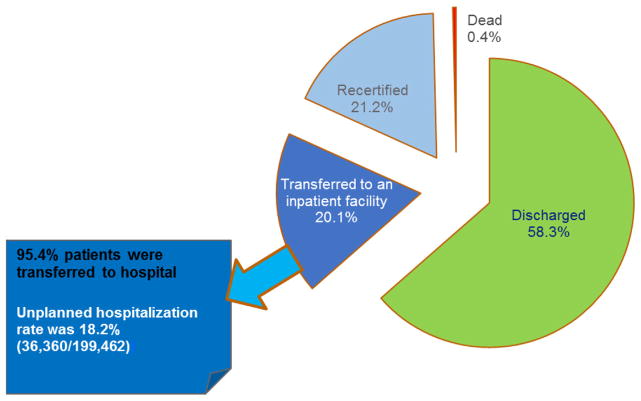
In total, 11,476 (6%) patients received emergency care during their HHC stay, with most (n = 9,790) leading to hospital admission. Figure 1 demonstrates the dispositions of the 199,462 HHC patients within their 60-day HHC stay. Most (58.3%) were discharged from HHC, 20.7% continued in HHC, and 20.1% were transferred to an inpatient facility, with 95.6% of these to acute care hospitals. Approximately 5% of the hospitalizations were planned for scheduled treatment or procedures. In total, 36,360 (18.2%) HHC patients had unplanned hospitalizations. Seventeen percent of these unplanned hospitalizations were caused by infections; 2,787 (7.7%) were caused by respiratory infections; 1,702 (4.7%) were for wound infection or deterioration; 1,587 (4.4%) were because of urinary tract infections; and 105 (0.3%) were caused by IV catheter-related infection (Table 2). Three of the 6 top reasons for unplanned hospitalization were related to infections.
Fig 1.
Patient disposition after the initial 60-day home health care stay.
Table 2.
Reasons for unplanned hospitalization (n = 36,360)
| Hospital reason | n | % |
|---|---|---|
| Other respiratory problem | 3,520 | 9.7 |
| Respiratory infection | 2,878 | 7.7 |
| Heart failure | 2,659 | 7.3 |
| Dehydration, malnutrition | 1,761 | 4.8 |
| Wound infection/deterioration | 1,702 | 4.7 |
| Urinary tract infection | 1,587 | 4.4 |
| Uncontrolled pain | 1,487 | 4.1 |
| Myocardial infarction | 1,319 | 3.6 |
| Gastrointestinal issues | 1,167 | 3.2 |
| Acute mental-behavioral | 1,044 | 2.9 |
| Cardiac dysrhythmia | 997 | 2.7 |
| Stroke (CVA) or TIA | 818 | 2.3 |
| Hypoglycemic-hyperglycemic | 734 | 2.0 |
| Other heart disease | 672 | 1.9 |
| DVT pulmonary embolus | 539 | 1.5 |
| Improper medication administration | 394 | 1.1 |
| IV catheter infection or complication | 105 | 0.3 |
NOTE. Outcome and Assessment Information Set indicates that 34% of unplanned hospitalizations were related to some other reasons not listed here, and 11% unplanned hospitalizations were marked as reasons unknown.
CVA, cerebrovascular accident; DVT, deep venous thrombosis; IV, intravenous; TIA, transient ischemic attack.
Individual-level infection rate
Approximately 3.52% (7,018/199,462) of the patients received emergency care or were hospitalized because of infection based on assessment by registered nurses or therapists. Excluding patients who were admitted to HHC with infection, 3.46% (6,915/199,462) of patients developed infection that led to hospitalization or emergency care treatment sometime while receiving HHC. The average time to developing infection while receiving HHC was 23.8 ± 17.1 days. Because IV catheter-related infection can only occur in patients with IV catheter, we pulled out a subsample and found that 5,958 HHC patients received IV therapy or parenteral nutrition treatment at home, and approximately 3% of these patients developed IV catheter-related infection during the HHC period.
Compared with their counterparts, HHC patients who were hospitalized or received emergency care because of infection were significantly younger, were more likely to be men, were more likely to be white, have had acute hospital stays 14 days prior to HHC admission, have cancer or renal diseases when admitted to HHC, and were more likely to be receiving IV therapy or parenteral nutrition during HHC (Table 1). The common diagnoses for patients who developed infections during HHC were unspecified congestive heart failure, obstructive chronic bronchitis with exacerbation, after care after circulatory system surgery or joint placement surgery, and diabetes without complication.
Agency-level infection rate
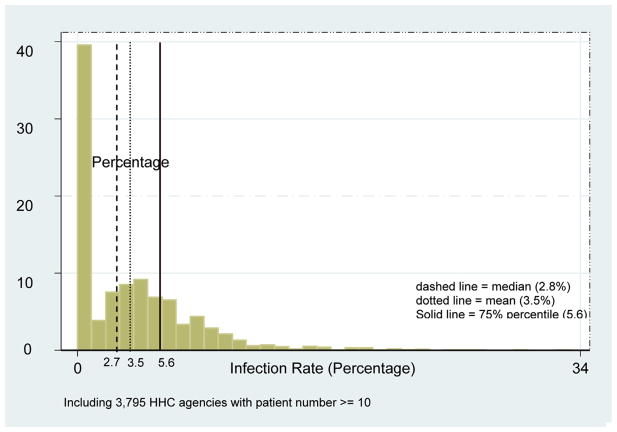
The agency-level infection rates varied dramatically from 0%–100%, with an average of 3.3% ± 8.8%. This sample included a number of agencies with a very small number of patients; 34% (n = 2,810) of the agencies had <5 patients, and 20% (n = 1,650) had 5–10 patients. The outcomes of the HHC agencies with small patient numbers were likely to be influenced by some extreme cases. Therefore, to reduce potential bias, we used a subgroup of HHC agencies with >10 patients (n = 3,975, 46% of 8,255 HHC agencies) and calculated their agency-level infection rates. As shown in Figure 2, the agency-level infection rates for these HHC agencies varied from 0%–33.3%, with a mean of 3.5% ± 4.1% and a median of 2.8%. Approximately 25% of these HHC agencies had 0 infections, and another 25% had infection rates >5.6%.
Fig 2.
Distribution of infection rates across HHC agencies. HHC, home health care.
DISCUSSION
To our knowledge, this is the first study to use OASIS data to examine the rate of hospitalizations or emergency care usage because of infection among patients receiving HHC at a national level. We found that based on the assessment from HHC nurses and therapists, 3.5% of patients were hospitalized or received emergency care because of infection developed in HHC, and the IV catheter-related infection rate was 3.0%. These 2 numbers are lower than previously reported infection rates (4.5% to 11.5%) among the general HHC patient population,18 which is for several possible reasons. First, to be conservative, we only used the patients’ first HHC episode. Second, and importantly, in our study, an infection case was identified only when a patient received emergency care or was transferred to acute care hospitals. Other studies may have included infections developed at HHC that did not lead to hospitalization or emergency care treatment. For example, HHC patients may develop infections during HHC stay and receive outpatient treatment. These infections were not captured using OASIS data. Our estimate of infection using hospitalization and emergency care data most likely underestimates the actual infection rate and represents only the tip of the iceberg.
Nevertheless, the estimate of infection rates using OASIS data has significant clinical implications. One of the goals of HHC is to reduce health care costs; when a patient is referred to an HHC agency, the idea is that the patient can continue treatment and recovery in the comfort of their own home at a lower cost. Any infection developed during HHC incurs additional costs. However, infection that leads to acute care hospital admission and emergency room treatment adds major financial burdens to both patients and the health care system because the direct hospital costs of treating infections were $28–$33 billion.25 Hence, it is important that infection prevention and control practices be followed in the home to minimize the risk of infection and the need for additional acute care interventions.
Using data regarding hospitalization or receiving emergency care as the method to identify infection is also relevant to the Affordable Care Act because one of its important aims is to reduce costly and preventable rehospitalizations.26 There is no information regarding the exact number of hospital discharged patients being sent to HHC. However, our data showed that over half of the HHC patients had had inpatient stays within 14 days prior to HHC admission, suggesting that HHC has become a major postacute care provider in the current health care system. We found that 18.2% of HHC patients were admitted to acute care hospitals for medical conditions after an average of 23 days in HHC, and 17% of these unplanned hospitalizations were caused by infections. This indicates the importance of focusing on infection control and prevention in HHC in national efforts to reduce rehospitalization.
Infection control and prevention has always been a focus for health care policymakers. National efforts guided by the Department of Health and Human Services’ action plan to prevent health care–associated infections27 have made great strides in the hospital setting, demonstrated by a reduction of bloodstream infections in intensive care units by 58% from 2001–2009.28 Although such national efforts have demonstrated success in reducing health care–associated infections in hospital settings, challenges remain in HHC settings. Researchers have recognized the challenges and identified barriers for effective and efficient infection control in HHC. One of these barriers is the lack of a national dataset for measuring infection.17 As demonstrated in a previous systematic review,18 different studies used different approaches to define and measure infection rates, making it difficult to compare infections between HHC agencies. To overcome the barriers, thought leaders have called for a simple and practical approach to study infection and proposed 3 potential databases, which are OASIS, Missouri Alliance for Homecare Infection Surveillance Project, and Outpatient Parenteral Antimicrobial Therapy registry.17 Compared with the other 2 databases, OASIS has the broader scale and has been adopted by most HHC agencies nationwide and may be the most appropriate. Because the nation is committed to enhancing electronic health records utilization, using OASIS can avoid the cost of developing a new system, therefore improving evaluation of health services and ultimately improving quality of care at a cost-effective manner.
To our knowledge, our study is the first to examine agency-level infection rates on a national scale. We found that infection rates varied widely across different HHC agencies, perhaps because of diverse patient populations in different agencies, their small samples size, and agencies’ adherence to OASIS data collection guidelines; variations are also likely to be caused by different infection control practices adopted by HHC agencies. Although studies conducted in hospitals have found that facilities’ infection control policy and adherence to infection control practice guidelines can influence infection rates,29,30 the evidence of infection control policy and practice in HHC is sparse. In one study, Felembam et al31 observed hand hygiene practice among 40 HHC patient care episodes in Australia and reported low adherence. Kenneley32 surveyed HHC nurses and found great variation in infection control policies and procedures across organizations. However, these 2 studies were limited by either focusing only on a single infection control practice31 or including small sample sizes.31,32 A study using a national representative sample will help HHC policymakers to better understand the infection control policy and practice adherence at a national level, empowering them to make recommendations to improve the practice and prevent and control infection, further to improve the quality of HHC.
Limitations
This study has several limitations. First, the data items used in our study to define infections were based on the assessment by nurses or therapists without laboratory data confirmation, meaning that the infection may not be a confirmed diagnosis. However, as described previously, multiple data sources and strategies were used to ensure data accuracy, and detailed instructions from the OASIS user manuals and Web training were given to HHC agencies to improve the quality of data collection. Historically, nurses are reliable and accurate informants.33–35 Second, the reasons for hospitalization and emergency care use are not mutually exclusive; therefore, an infection might be one of a number of reasons why a nurse thinks the patient was hospitalized or received emergency care. However, our analysis revealed that only a very small proportion of unplanned hospitalizations had >2 reasons marked. Third, there were 34% of unplanned hospitalizations with reasons not listed in OASIS, and 11% marked with reason unknown. The former does not affect our estimate of infection rates, and the latter can be treated as random missing.
Despite the data collection nature of OASIS, OASIS is the only readily available comprehensive assessment of HHC patients adopted nationwide and has potential to be used for the development of a national infection surveillance system in HHC. Future investigators comparing the OASIS infection measurement with confirmative data sources, such as the Medicare Provider Analysis and Review files from the Centers for Medicare and Medicaid, to confirm the accuracy of the OASIS outcome measurement would be helpful. With the national effort to enhance electronic health record systems and health information technology, linking OASIS to the National Healthcare Safety Network and using the National Healthcare Safety Network as the surveillance system with consistent infection definitions being used across agencies would be an alternative solution with great improvement.
CONCLUSIONS
Using the national OASIS data, we are the first to examine the proportion of hospitalizations or emergency care treatments caused by infection in HHC and agency-level infection rate at a national level. Our study suggests that infection is a serious problem in HHC, and there is likely considerable variation in infection control policies and practices across agencies. OASIS may be used to develop an infection surveillance system in HHC so that HHC agencies can benchmark quality of care.
Acknowledgments
Funding/Support: This study is funded by the National Institute of Nursing Research (grant no. R03NR013966-01).
We thank Kristine Kulage and the Columbia University School of Nursing writing workshop for their assistance with review of the manuscript.
Footnotes
Conflicts of interest: None to report.
References
- 1.Jarvis WR. Infection control and changing health-care delivery systems. Emerg Infect Dis. 2001;7:170–3. doi: 10.3201/eid0702.010202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clark P. Emergence of infection control surveillance in alternative health care settings. J Infus Nurs. 2010;33:363–70. doi: 10.1097/NAN.0b013e3181f85a5e. [DOI] [PubMed] [Google Scholar]
- 3.Klevens RM, Edwards JR, Richards CL, Jr, Horan TC, Gaynes RP, Pollock DA, et al. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122:160–6. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheldon P, Bender M. High-technology in home care. An overview of intravenous therapy. Nurs Clin North Am. 1994;29:507–19. [PubMed] [Google Scholar]
- 5.National Association for Home Care & Hospice. [Accessed January 21st, 2015];Basic statistics about home care. 2010 Available from: http://www.nahc.org/assets/1/7/10HC_Stats.pdf.
- 6.Administration on Aging. A profile of older Americans: 2010. Department of Health and Human Services; 2011. [Accessed January 21, 2015]. Available from: http://www.aoa.acl.gov/Aging_Statistics/Profile/2010/2.aspx. [Google Scholar]
- 7.Markkanen P, Quinn M, Galligan C, Chalupka S, Davis L, Laramie A. There’s no place like home: a qualitative study of the working conditions of home health care providers. J Occup Environ Med. 2007;49:327–37. doi: 10.1097/JOM.0b013e3180326552. [DOI] [PubMed] [Google Scholar]
- 8.Danzig LE, Short LJ, Collins K, Mahoney M, Sepe S, Bland L, et al. Bloodstream infections associated with a needleless intravenous infusion system in patients receiving home infusion therapy. J Am Med Assoc. 1995;273:1862–4. [PubMed] [Google Scholar]
- 9.Do AN, Ray BJ, Banerjee SN, Illian AF, Barnett BJ, Pham MH, et al. Bloodstream infection associated with needleless device use and the importance of infection-control practices in the home health care setting. J Infect Dis. 1999;179:442–8. doi: 10.1086/314592. [DOI] [PubMed] [Google Scholar]
- 10.Kellerman S, Shay DK, Howard J, Goes C, Feusner J, Rosenberg J, et al. Bloodstream infections in home infusion patients: the influence of race and needleless intravascular access devices. J Pediatr. 1996;129:711–7. doi: 10.1016/s0022-3476(96)70154-3. [DOI] [PubMed] [Google Scholar]
- 11.Dwyer LL, Harris-Kojetin LD, Valverde RH, Frazier JM, Simon AE, Stone ND, et al. Infections in long-term care populations in the United States. J Am Geriatr Soc. 2013;61:342–9. doi: 10.1111/jgs.12153. [DOI] [PubMed] [Google Scholar]
- 12.John BK, Khan MA, Speerhas R, Rhoda K, Hamilton C, Dechicco R, et al. Ethanol lock therapy in reducing catheter-related bloodstream infections in adult home parenteral nutrition patients: results of a retrospective study. JPEN J Parenter Enteral Nutr. 2012;36:603–10. doi: 10.1177/0148607111428452. [DOI] [PubMed] [Google Scholar]
- 13.Wilde MH, Brasch J, Getliffe K, Brown KA, McMahon JM, Smith JA, et al. Study on the use of long-term urinary catheters in community-dwelling individuals. J Wound Ostomy Continence Nurs. 2010;37:301–10. doi: 10.1097/WON.0b013e3181d73ac4. [DOI] [PubMed] [Google Scholar]
- 14.DeLegge MH, Borak G, Moore N. Central venous access in the home parenteral nutrition population-you PICC. JPEN J Parenter Enteral Nutr. 2005;29:425–8. doi: 10.1177/0148607105029006425. [DOI] [PubMed] [Google Scholar]
- 15.Tokars JI, Cookson ST, McArthur MA, Boyer CL, McGeer AJ, Jarvis WR. Prospective evaluation of risk factors for bloodstream infection in patients receiving home infusion therapy. Ann Intern Med. 1999;131:340–7. doi: 10.7326/0003-4819-131-5-199909070-00004. [DOI] [PubMed] [Google Scholar]
- 16.Weber DJ, Brown V, Huslage K, Sickbert-Bennett E, Rutala WA. Device-related infections in home health care and hospice: infection rates, 1998–2008. Infect Control Hosp Epidemiol. 2009;30:1022–4. doi: 10.1086/605641. [DOI] [PubMed] [Google Scholar]
- 17.Manangan LP, Pearson ML, Tokars JI, Miller E, Jarvis WR. Feasibility of national surveillance of health-care-associated infections in home-care settings. Emerg Infect Dis. 2002;8:233–6. doi: 10.3201/eid0803.010098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shang J, Ma C, Poghosyan L, Dowding D, Stone P. The prevalence of infections and patient risk factors in home health care: a systematic review. Am J Infect Control. 2014;42:479–84. doi: 10.1016/j.ajic.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Medicare and Medicaid Services. [Accessed November 21, 2014];OASIS user manuals. Available from: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/HHQIOASISUserManual.html.
- 20.CMS Survey and Certification Group. [Accessed November 21, 2014];Outcome and Assessment Information Set (OASIS) training – course menu. Available from: http://surveyortraining.cms.hhs.gov/pubs/CourseMenu.aspx?cid=0CMSOASISCWBT.
- 21.Bergquist-Beringer S, Gajewski BJ. Outcome and assessment information set data that predict pressure ulcer development in older adult home health patients. Adv Skin Wound Care. 2011;24:404–14. doi: 10.1097/01.ASW.0000405215.49921.a9. [DOI] [PubMed] [Google Scholar]
- 22.Scharpf TP, Madigan EA. Functional status outcome measures in home health care patients with heart failure. Home Health Care Serv Q. 2010;29:155–70. doi: 10.1080/01621424.2010.534044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Westra BL, Savik K, Oancea C, Choromanski L, Holmes JH, Bliss D. Predicting improvement in urinary and bowel incontinence for home health patients using electronic health record data. J Wound Ostomy Continence Nurs. 2011;38:77–87. doi: 10.1097/won.0b013e318202e4a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Madigan EA, Fortinsky RH. Interrater reliability of the outcomes and assessment information set: results from the field. Gerontologist. 2004;44:689–92. doi: 10.1093/geront/44.5.689. [DOI] [PubMed] [Google Scholar]
- 25.Scott RD., II [Accessed November 21, 2014];The direct medical cost of healthcare-associated infections in US hospitals and the benefits of prevention. 2009 Available from: http://www.cdc.gov/HAI/pdfs/hai/Scott_CostPaper.pdf.
- 26.Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. J Am Med Assoc. 2011;306:1794–5. doi: 10.1001/jama.2011.1561. [DOI] [PubMed] [Google Scholar]
- 27.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. [Accessed November 21, 2014];HHS action plan to prevent healthcare-associated infections. Available from: http://www.hhs.gov/ash/initiatives/hai/actionplan/index.html.
- 28.Centers for Disease Control and Prevention (CDC) Vital signs: central line-associated blood stream infections–United States, 2001, 2008, and 2009. MMWR Morb Mortal Wkly Rep. 2011;60:243–8. [PubMed] [Google Scholar]
- 29.Furuya EY, Dick A, Perencevich EN, Pogorzelska M, Goldmann D, Stone PW. Central line bundle implementation in US intensive care units and impact on bloodstream infections. PLoS One. 2011;6:e15452. doi: 10.1371/journal.pone.0015452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zachariah P, Furuya EY, Edwards J, Dick A, Liu H, Herzig CT, et al. Compliance with prevention practices and their association with central line-associated bloodstream infections in neonatal intensive care units. Am J Infect Control. 2014;42:847–51. doi: 10.1016/j.ajic.2014.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Felembam O, John W, Shaban R. Hand hygiene practices of home visiting community nurses: perceptions, compliance, techniques, and contextual factors of practice using the World Health Organization’s “five moments for hand hygiene”. Home Healthc Nurse. 2012;30:152–60. doi: 10.1097/NHH.0b013e318246d5f4. [DOI] [PubMed] [Google Scholar]
- 32.Kenneley I. Infection control in home healthcare: an exploratory study of issues for patients and providers. Home Healthc Nurse. 2012;30:1418–28. doi: 10.1097/NHH.0b013e31824adb52. [DOI] [PubMed] [Google Scholar]
- 33.Aiken LH, Sochalski J, Lake ET. Studying outcomes of organizational change in health services. Med Care. 1997;35(11 Suppl):NS6–18. doi: 10.1097/00005650-199711001-00002. [DOI] [PubMed] [Google Scholar]
- 34.Justice AC, Aiken LH, Smith HL, Turner BJ. The role of functional status in predicting inpatient mortality with AIDS: a comparison with current predictors. J Clin Epidemiol. 1996;49:193–201. doi: 10.1016/0895-4356(95)00546-3. [DOI] [PubMed] [Google Scholar]
- 35.Pearlin LI. Alienation from work: a study of nursing personnel. Am Sociol Rev. 1962;27:314–26. [Google Scholar]