Abstract
In this study we tested the hypothesis that participants higher in dispositional self-compassion would show lower stress-induced reactivity of salivary alpha-amylase (sAA), a marker of sympathetic nervous system activation. Thirty-three healthy participants (18–34 years old) were exposed to a standardized laboratory stressor on two consecutive days. Self-compassion, self-esteem, and demographic factors were assessed by questionnaire and sAA was assessed at baseline and at 1, 10, 30, and 60 minutes following each stressor. Self-compassion was a significant negative predictor of sAA responses on both days. This relationship remained significant when controlling for self-esteem, subjective distress, age, gender, ethnicity, and Body Mass Index (BMI). These results suggest that self-compassion may serve as a protective factor against stress-induced physiological changes that have implications for health.
Keywords: self-compassion, self-esteem, psychosocial stress, Trier Social Stress Test, salivary alpha-amylase
Acute psychosocial stress activates a biological fight-or-flight response that includes the activation of the sympathetic nervous system and the release of epinephrine and norepinephrine, which increase heart rate and blood pressure and induce other physiological changes (Frankenhaeuser et al., 1978). These changes help to increase energy and alertness to help the organism cope more effectively with threats in the environment, but repeated activation of the stress response can contribute to the wear-and-tear of critical organ systems (McEwen, 1998) and increase disease risk (e.g., Cohen, Janicki-Deverts, & Miller, 2007; Grassi, Arenare, Pieruzzi, Brambilla, & Mancia, 2009; Piazza, Charles, Sliwinski, Mogle, & Almeida, 2013; Charles, Piazza, Mogle, Sliwinski, & Almeida, 2013).
The magnitude of biological stress responses is determined in part by the extent to which stressors are appraised as threatening to the self (Dickerson & Kemeny, 2004; Lazarus & Folkman, 1984). Recent research suggests that self-compassion, which involves treating the self with kindness and understanding rather than self-criticism (Neff, 2003a), may counteract perceived threat and therefore reduce biological responses to repeated stress. Compared to individuals low in self-compassion, self-compassionate individuals exhibit less emotional reactivity in stressful situations (Leary, Tate, Adams, Allen, & Hancock, 2007), and show lower elevations in the pro-inflammatory cytokine interleukin-6 in response to acute psychosocial stress (Breines, Thoma, Gianferante, Hanlin, Chen, & Rohleder, 2014). Self-compassion interventions have been shown to reduce stress, anxiety, and depression (Neff & Germer, 2013), to attenuate feelings of shame and self-criticism (Gilbert & Procter, 2006), and to increase cortisol habituation (Breines & Rohleder, under review).
To date, only one study (Arch, Brown, Dean, Landy, Brown, & Laudenslager, 2014) has examined the relationship between self-compassion and a marker of sympathetic nervous system activation. In that study, salivary alpha-amylase (sAA) concentration was used as a surrogate marker of sympathetic nervous system activity. Multiple prior studies have found support for the link between sAA and other sympathetic markers, such as norepinephrine (e.g., Rohleder, Nater, Wolf, Ehlert, & Kirschbaum, 2004; Thoma, Kirschbaum, Wolf, & Rohleder, 2012), making it a reliable alternative to more invasive and costly measurement techniques. Arch et al. (2014) found that sAA reactivity to stress was lowest among participants who were randomly assigned to a pre-stress self-compassion intervention, compared to those assigned to two control conditions. Participants in the self-compassion condition also showed lower subjective anxiety and greater heart rate variability, a marker of cardiovascular parasympathetic activity (Thayer & Lane, 2000).
Although this study (Arch et al., 2014) provides strong initial evidence for the role of self-compassion in attenuating stress-induced sympathetic activation, several questions remain. First, the sample was comprised only of females, so it is unknown whether self-compassion is related to reduced sAA activation among males as well. Second, the relationship between self-compassion and sAA responses across repeated stressors is unknown. Because individuals are likely to encounter repeated stressors in everyday life, and because negative affective responses to everyday stressors are predictors of mental and biomedical disease (Piazza, Charles, Sliwinski, Mogle, & Almeida, 2013; Charles, Piazza, Mogle, Sliwinski, & Almeida, 2013), assessing responses to repeated in addition to novel stressors can provide a window into how individuals might respond to naturalistic stressors that recur in their daily lives. Third, it is unknown whether individuals high in the dispositional tendency to be self-compassionate will show lower sAA stress reactivity even in the absence of explicit reminders to be self-compassionate. Finally, it is unclear whether the benefits of self-compassion are independent of self-esteem, a related construct.
The present study sought to address these questions by examining the relationship between dispositional self-compassion and sAA responses to an initial and repeated stressor in a mixed gender sample. After an initial assessment of self-compassion, self-esteem, and demographic factors, participants were exposed to a standardized laboratory stressor, the Trier Social Stress Test (TSST; Kirschbaum, Pirke, & Hellhammer, 1993) at the same time on two consecutive days, and sAA was assessed in saliva samples taken at baseline and at 1, 10, 30 and 60 minutes post-stress. Subjective distress was assessed immediately following each stressor.
We hypothesized that participants higher in self-compassion would show lower sAA responses to both the initial and repeated stressors, and potentially also show greater habituation of sAA across the two stressors. Self-compassion should reduce the extent to which a stressor is perceived as self-threatening, thereby attenuating the magnitude of the corresponding stress response. We also hypothesized that the relationship between self-compassion and sAA responses would be independent of self-esteem, a related construct that has also been shown to buffer stress reactivity (Ford & Collins, 2010; Rector & Roger, 1997; Taylor, Lerner, Sherman, Sage, & McDowell, 2003). Given that self-compassion has been shown to have several psychological advantages over self-esteem, such as lower defensiveness (Leary et al., 2007), greater self-worth stability (Neff & Vonk, 2009), and lower narcissism (Neff, 2003b), we also expected that self-compassion might be a stronger predictor of lower sAA responses compared to self-esteem. Furthermore, we hypothesized that the relationship between self-compassion and sAA responses would be independent of subjective distress in response to each stressor. Because the tendency to experience subjective distress could be lower among participants high in self-compassion—and higher among participants with greater sAA responses—we wanted to address this potential confound.
Method
Participants
The data reported in this manuscript were collected as part of a larger research study conducted over three years in which both young and older adults were recruited. In the current report we focused on the young adult participant group only. Participants were recruited from the Greater Boston area and the Brandeis University campus via print and social media advertisements. Participants were paid for their participation.
All participants underwent a brief medical and psychological phone screening prior to testing and were invited to participate only if they met a specific selection criteria: a) body mass index (BMI) within the reference range of 18–30 kg/m2; b) luteal phase of menstrual cycle at time of participation, if female (luteal phase estimation was based on self-reported cycle length); c) absence of psychiatric, endocrine, cardiovascular, or other specific chronic diseases; d) no intake of psychoactive drugs, beta-blockers, gonadal steroids (hormonal contraceptives), or glucocorticoids; e) non-smokers, and f) no previous experience with the stress protocol. Participants who reported, in the pretest questionnaire, health conditions or substance intake that met the exclusion criteria (i.e., asthma, N = 4; anxiety/depression, N = 3; active allergies/medication, N = 3; psychostimulants, N = 1) were excluded from analyses. One participant was missing sAA data for both stressors and was also excluded. Another participant was missing sAA data only for the repeated stressor, so this participant’s data was included in analyses of the initial stressor only.
Participants in the final sample (N = 33) were 48% female. Forty-nine percent of participants identified as White or Caucasian American, 36% as Asian or Asian American, 6% as Black or African American, and 9% as Other. Age ranged from 18 to 34 years (M = 21.12, SD = 3.94).
According to the guidelines for determining sample size set forth by Cohen (1992), our sample size was determined to be sufficient to detect large effect sizes in regression analyses with up to three predictors. We anticipated large effect sizes based on prior research examining the relationship between self-compassion and biological stress responses (Breines et al., 2014).
Procedure Overview
Eligible participants were scheduled for laboratory sessions on two consecutive days. All laboratory sessions were scheduled in the afternoon to control for circadian variation of stress hormones (Rohleder & Nater, 2009). Participants were instructed to refrain from eating or drinking anything but water for one hour before the laboratory sessions. Written informed consent was obtained prior to participation and ethical approval was granted by the Brandeis University Institutional Review Board.
Each laboratory session lasted approximately three hours and included a resting period followed by exposure to the Trier Social Stress Test (TSST). Saliva samples were taken at baseline and at 1, 10, 30, and 60 minutes following the TSST. At the beginning of day 1, self-compassion, self-esteem, and demographic factors were assessed using self-report paper-and-pencil questionnaires. Subjective distress was assessed immediately after each TSST. Details about these procedures are described below. Other measures not germane to the present investigation were also assessed.
Measures
Self-Compassion
The 26-item Self-Compassion Scale (SCS; Neff, 2003b) includes five items assessing self-kindness (e.g., “I try to be understanding and patient toward aspects of my personality I don’t like”), five reverse-scored items assessing self-judgment (e.g., “I’m disapproving and judgmental about my own flaws and inadequacies”), four items assessing perceptions of common humanity (e.g., “I try to see my failings as part of the human condition”), four reverse-scored items assessing perceived isolation (e.g., “When I think about my inadequacies it tends to make me feel more separate and cut off from the rest of the world”), four items assessing mindfulness (e.g., “When something painful happens I try to take a balanced view of the situation”), and four reverse-scored items assessing over-identification with emotional reactions (e.g., “When I’m feeling down I tend to obsess and fixate on everything that’s wrong”). Responses to the SCS were given on a 5-point scale (1 = Almost never; 5 = Almost always). The SCS has demonstrated concurrent, convergent, and discriminant validity, and test–retest reliability (Neff, 2003b; Neff, Kirkpatrick, & Rude, 2007). In the present study, the SCS was internally consistent (α = 0.92). On average, participants reported moderate levels of self-compassion (M = 3.14; SD = 0.67).
Self-esteem
Self-esteem was assessed using the 10-item Rosenberg Self-Esteem Scale (RSE; Rosenberg, 1965). Participants were asked to rate their agreement or disagreement with ten statements (e.g., “I take a positive attitude toward myself”) on a 4-point response scale (0 = Strongly disagree; 3 = Strongly agree). Final scores were computed by summing scores on all items after reverse scoring five items. The RSE has demonstrated reliability and validity (Blascovich & Tomaka, 1991). In the present study, the RSE was internally consistent (α = 0.85), and participants reported moderate levels of self-esteem on average (M = 23.11; SD = 5.52).
Subjective distress
Immediately following each TSST, participants rated the extent to which they felt “distressed” by the task on a 5-point scale (1 = Very slightly or not at all; 5 = Extremely). On average, participants reported feeling moderate psychological distress (day 1 M = 2.97, SD = 1.13; day 2 M = 2.56, SD = 1.16). Subjective distress significantly habituated across the two stressors: day 1 responses were significantly greater than day 2 responses, F (1, 31) = 4.53, p = 0.041
Body mass index (BMI)
Height and weight measurements were taken using a tape measure and a Supra Plus 720 column scale (Seca, Hamburg, Germany), and BMI was computed as kg/m2.
Stress Induction Paradigm
Acute psychosocial stress was induced using the Trier Social Stress Test (TSST; Kirschbaum et al., 1993), a widely used standardized laboratory stress paradigm. The TSST used in the present study consisted of a three minute preparation period, a five minute public speech, and a five minute mental arithmetic task in front of an audience of two judges wearing lab coats and maintaining a neutral evaluative facial expression. The public speech involved describing how one’s personality makes one qualified for a dream job and the mental arithmetic ask involved counting backwards from 2043 by increments of 17 on the first study day and from 2011 by 13 on the second study day. Participants were informed that these judges were trained in analyzing verbal and non-verbal behavior and that their performance would be videotaped. The TSST has demonstrated reliability and validity and has been shown to produce strong biological responses to stress (Dickerson & Kemeny, 2004).
Saliva Collection and Measurement of Salivary Alpha-Amylase
On both study days, saliva was collected at baseline, and at 1, 10, 30, and 60 minutes following each TSST using Salivette collection devices (Sarstedt, Newton, NC). Salivettes were stored at −30°C until batch analysis of sAA at the end of data collection. Before assaying saliva was centrifuged at 2000g for 5 min. Salivary alpha-amylase measurement was completed using an enzyme kinetic method as described previously (Bosch et al., 2003; Rohlder & Nater, 2009). Saliva was diluted at 1:625 with ultrapure water, and diluted saliva was incubated with substrate reagent (α-amylase EPS Sys; Indianapolis, IN) at 37C for 3 min before a first absorbance reading was taken at 405 nm with a Tecan Sunrise ELISA reader (Tecan, Morrisville, NC). A second reading was taken after 5 min incubation at 37C and increase in absorbance was transformed to sAA concentration (U/ml) using “Calibrator f.a.s.” solution (Roche Diagnostics) as standard. Inter- and intra-assay coefficients of variation were below 10%.
Statistical Analyses
All statistical analyses were performed using SPSS for Mac OS X 22 software package (IBM, Chicago, IL, USA). Kolmogorov–Smirnov tests were computed prior to statistical analyses to test for normal distribution as well as homogeneity of variance of all dependent variables. Pearson correlations were used in preliminary analyses to examine relationships between self-compassion and other continuous variables (i.e., age, BMI, self-esteem, subjective distress); analyses of variance (ANOVA) were used to examine relationships between self-compassion and categorical variables (i.e., gender and ethnicity). Repeated measures ANOVA were used to examine stress-induced changes in sAA from baseline to peak on each study day and across days. Linear regression was used to examine the relationship between self-compassion and stress-induced changes in sAA on each study day and across study days. Because sAA levels showed significant violations of normality, log-10 transformations were conducted to correct positive skews. sAA responses on both days were computed as delta scores (i.e., peak sAA at 1 or 10 minutes post-TSST minus sAA levels at pre-TSST baseline). All reported results were considered to be significant at the p < 0.05 level.
Results
Preliminary Analyses
We first examined the relationships between self-compassion, demographic variables, and Body Mass Index (BMI). Self-compassion was not significantly correlated with age (r = 0.17, p = 0.36) or BMI (r = 0.01, p = 0.94). The two largest ethnic groups represented, White (M = 3.13, SD = 0.56, N = 16) and Asian (M = 3.24, SD = 0.87, N = 12), did not differ significantly in self-compassion, F (1, 31) = 0.15, p = 0.70, and the omnibus test of differences across all ethnic groups was also non-significant, F (1, 31) = 0.16, p = 0.96. Female (M = 3.02, SD = 0.67, N = 17) and male (M = 3.27, SD = 0.67, N = 16) participants did not differ significantly in self-compassion, F (1, 31) = 1.17, p = 0.29. There were no significant interactions between self-compassion and demographic variables predicting sAA responses on either study day.
We then examined correlations between self-compassion, self-esteem, and subjective distress on each study day. Self-compassion and self-esteem were significantly positively correlated (r = 0.65, p < 0.001). Self-compassion was not significantly correlated with subjective distress on day 1 (r = −0.16, p = 0.37) or day 2 (r = −0.03, p = 0.89). Zero-order correlations for all continuous variables are presented in Table 1.
Table 1.
Zero-Order Correlations Between All Continuous Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | |
|---|---|---|---|---|---|---|---|---|
| 1. Self-compassion | --- | |||||||
| 2. Self-esteem | 0.65** | --- | ||||||
| 3. Distress d1 | −0.16 | −0.22 | --- | |||||
| 4. Distress d2 | −0.03 | −0.04 | 0.48** | --- | ||||
| 5. sAA response d1 | −0.46** | −0.20 | −0.01 | −0.11 | --- | |||
| 6. sAA response d2 | −0.38* | −0.01 | −0.07 | 0.03 | 0.38* | --- | ||
| 7. Age | 0.17 | −0.12 | 0.01 | 0.07 | −0.27 | −0.29 | --- | |
| 8. BMI | 0.01 | −0.05 | −0.08 | −0.15 | 0.18 | 0.08 | −0.08 | --- |
p < 0.05,
p < 0.01
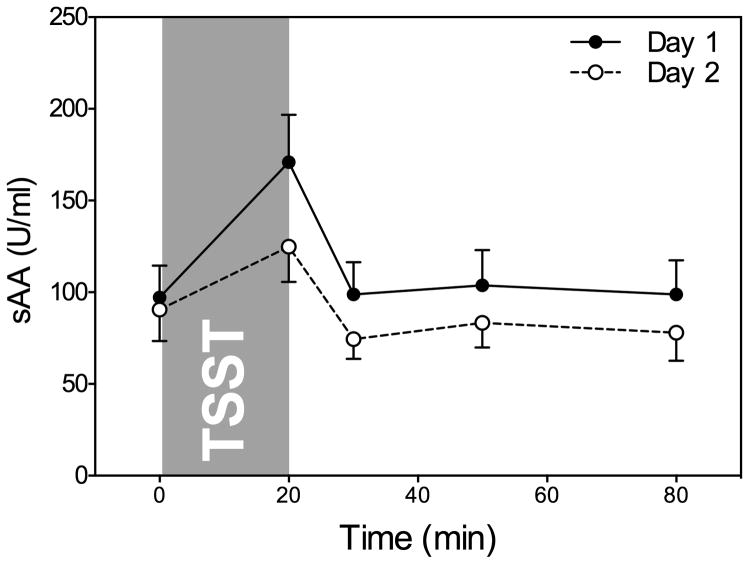
Salivary Alpha-Amylase Response
We next examined whether exposure to the TSST induced increases in salivary alpha-amylase (sAA). Repeated measures ANOVA indicated that there was a significant effect of time on sAA for both TSST1 and TSST2, indicating that sAA levels increased significantly from baseline to immediately post-stress following the TSST on both days: day 1 F (1, 31) = 24.01, p < 0.001; day 2 F (1, 31) = 49.01, p < 0.001. However, sAA responses did habituate across the two TSSTs: TSST1 responses were significantly greater than TSST2 responses, F (1, 31) = 4.23, p = 0.048. sAA levels recovered below baseline levels by 60 minutes post-stress (see Figure 1).
Figure 1.
Mean sAA levels at baseline and 1, 10, 30, and 60 min post-TSST on days 1 and 2.
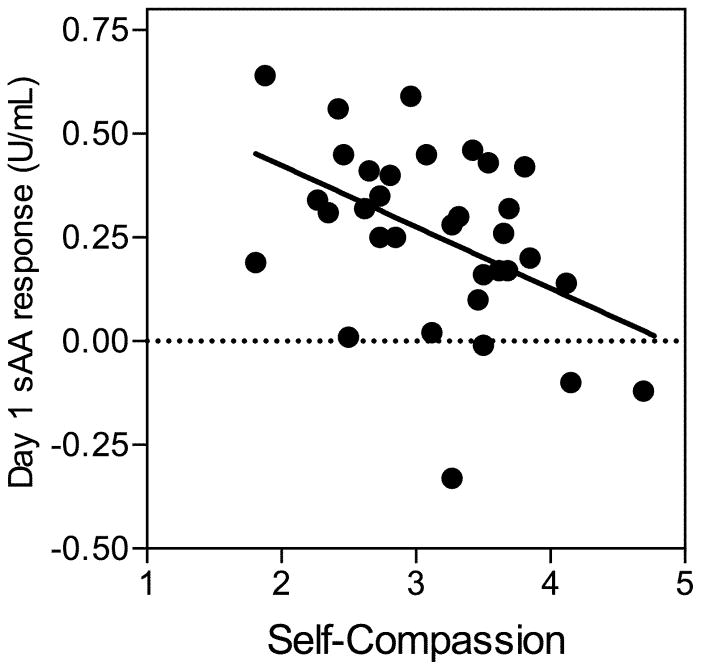
Self-Compassion and Day 1 Salivary Alpha-Amylase Response
We next performed a series of linear regression analyses to examine whether self-compassion predicted sAA response to the initial stressor. Self-compassion was not related to sAA at baseline on day 1, β = 0.09, t(1, 31) = 0.52, p = 0.61.
Consistent with hypotheses, self-compassion was a significant negative predictor of day 1 sAA response, β = −0.46, t(1, 31) = −2.88, p = 0.007, accounting for approximately 21% of the variance in sAA response, R2 = 0.21, F(1, 31) = 8.27, p = 0.007 (see Figure 2). Cohen’s f 2 = 0.27, indicating that the effect size for the relationship between self-compassion and day 1 sAA response was between medium and large.
Figure 2.
Self-compassion predicting day 1 sAA response.
When self-esteem was entered as a predictor along with self-compassion, self-compassion remained a significant predictor of day 1 sAA response, β = −0.58, t(2, 30) = −2.73, p = 0.011, whereas self-esteem was not a significant predictor, β = 0.18, t(2, 30) = 0.85, p = 0.40. The change in R2 resulting from the addition of self-esteem to the model was non-significant, ΔR2 = 0.02, F(1, 30) = 0.72, p = 0.40.
When day 1 subjective distress was entered as a predictor along with self-compassion, self-compassion remained a significant predictor of day 1 sAA response β = −0.47, t(2, 30) = −2.89, p = 0.007, whereas subjective distress was not a significant predictor, β = −0.09, t(2, 30) = −0.55, p = 0.59. The change in R2 resulting from the addition of subjective distress to the model was non-significant, ΔR2 = 0.01, F(1, 30) = 0.30, p = 0.59.
When demographic factors (i.e., age, gender, and ethnicity) and BMI were entered as predictors along with self-compassion, self-compassion again remained a significant predictor of day 1 sAA response (all ps < 0.05). None of these variables significantly predicted day 1 sAA response.
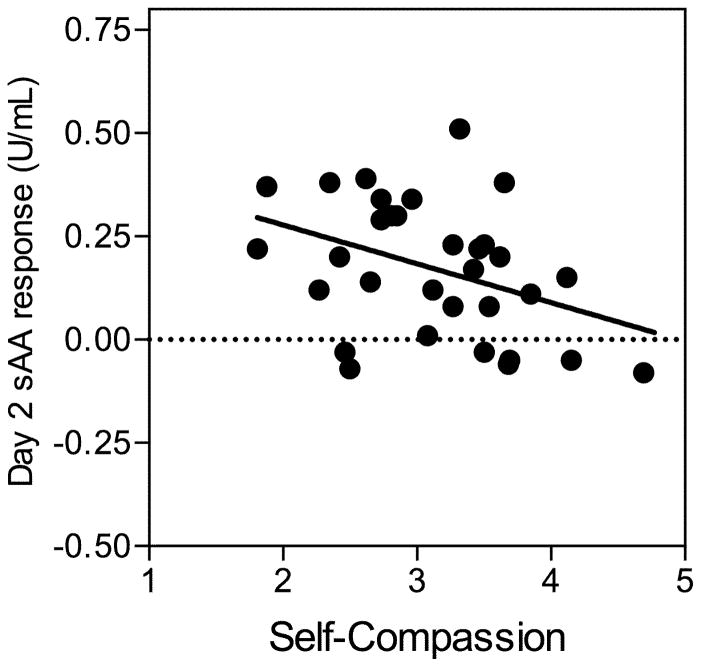
Self-Compassion and Day 2 Alpha-Amylase Response
We next examined whether self-compassion predicted sAA response to the repeated stressor. Self-compassion was not related to sAA at baseline on day 2, β = 0.18, t(1, 30) = 0.98, p = 0.34.
Consistent with hypotheses, self-compassion was a significant negative predictor of day 2 sAA response, β = −0.38, t(1, 30) = −2.28, p = 0.03, accounting for approximately 15% of the variance in sAA response, R2 = 0.15, F(1, 30) = 5.19, p = 0.03 (see Figure 3). Cohen’s f 2 = 0.18, indicating that the effect size for the relationship between self-compassion and day 2 sAA response was between medium and large.
Figure 3.
Self-compassion predicting day 2 sAA response.
When self-esteem was entered as a predictor along with self-compassion, self-compassion remained a significant predictor of day 2 sAA response, β = −0.64, t(2, 29) = −3.05, p = 0.005, whereas self-esteem remained a non-significant predictor, β = 0.40, t(2, 29) = 1.91, p = 0.066. The change in R2 resulting from the addition of self-esteem to the model was non-significant, ΔR2 = 0.10, F(1, 29) = 3.66, p = 0.066.
When day 2 subjective distress was entered as a predictor along with self-compassion, self-compassion remained a significant predictor of day 2 sAA response β = −0.38, t(2, 29) = −2.24, p = 0.033, whereas subjective distress was not a significant predictor, β = 0.02, t(2, 29) = −0.11, p = 0.92. The change in R2 resulting from the addition of subjective distress to the model was non-significant, ΔR2 = 0.000, F(1, 29) = 0.002, p = 0.97.
When demographic factors (i.e., age, gender, ethnicity) and BMI were entered as predictors along with self-compassion, self-compassion again remained a significant predictor of day 2 sAA response (all ps < 0.05). None of these variables significantly predicted day 2 sAA response.
Self-Compassion and Alpha-Amylase Habituation
Finally, we examined whether self-compassion predicted greater habituation of sAA across the two stressors. Habituation was operationalized as day 1 sAA response minus day 2 sAA response. Self-compassion was not a significant predictor of sAA habituation, β = −0.21, t(1, 30) = −1.16, p = 0.26.
Discussion
In this study we examined the hypothesis that individuals higher in dispositional self-compassion would show lower salivary alpha-amylase (sAA) responses to a repeated laboratory-based psychosocial stressor. Consistent with this hypothesis, self-compassion was negatively related to the magnitude of the sAA response to both a novel and a repeated psychosocial stressor. These relationships remained significant when controlling for self-esteem, subjective distress, age, gender, ethnicity, and Body Mass Index (BMI). The inclusion of these covariates allowed us to address the alternative hypothesis that self-compassion may relate to sAA only indirectly, through its relationship with other potential correlates of sAA. We did not find evidence to support this alternative hypothesis.
Self-compassion was not a significant predictor of sAA habituation, operationalized as day 1 minus day 2 sAA response. This null finding may be related to the significant negative correlation between self-compassion and day 1 sAA response; because self-compassionate participants showed lower sAA responses to the initial stressor, there was less room for attenuation in response magnitude following the repeated stressor. These results suggest that self-compassionate individuals may show lower sAA responses across the board, rather than showing greater habituation per se, but future research is needed to examine this question further.
The relationship between self-compassion and sAA responses to repeated stress is consistent with research on social self-preservation theory (Dickerson, Gruenewald, & Kemeny, 2004), which has shown that negative self-evaluative states such as shame are associated with stronger biological stress responses (e.g., Rohleder, Chen, Wolf, & Miller, 2008). Self-compassionate individuals may be less likely to appraise a potential stressor as self-threatening, which may in turn reduce signals from the central nervous system responsible for initiating the biological stress response. Prior research suggests that self-compassionate individuals tend to use more adaptive coping strategies, such as positive cognitive restructuring, when faced with stress (Allen & Leary, 2010); engaging in these strategies may help prepare them to cope more effectively with repeated stressors. In contrast, individuals low in self-compassion are more likely to ruminate on stressful events (Raes, 2010) and experience increased fear of failure (Neff, Kirkpatrick, & Rude, 2007), making them potentially more vulnerable to overreact when faced with repeated stressors.
Several unexpected findings emerged in this study. First, although sAA increased in response to both the novel and repeated stressors, sAA responses decreased significantly across the two study days, with lower responses on day 2. This finding may seem at odds with prior research showing that catecholamine response, a key marker of sympathetic activation, tends not to habituate across repeated stressors (Schommer, Hellhammer, & Kirschbaum, 2003). However, heart rate—another sympathetic indicator—does show habituation, suggesting that different subsystems may show different habituation patterns. In addition, Strahler, Rohleder, and Wolf (in press) also found habituation of sAA responses across two days, indicating that, in contrast to catecholamines, sAA may show a small degree of habituation across stressors.
Also unexpected was the non-significant relationship between self-esteem and sAA response on both days. Although prior research suggests that self-esteem should buffer stress reactivity (e.g., Rector & Roger, 1997), it is possible that this is not always the case. Some correlates of self-esteem, such as social comparison, defensive self-enhancement, and narcissism (Neff, 2003a), may be less effective than self-compassion when it comes to attenuating biological stress responses. For example, prior research shows that narcissists exhibit heightened cortisol reactivity to stress (Edelstein, Yim, & Kwas, 2010). By contrast, individuals who are able to treat themselves with kindness and compassion when faced with stress may show attenuated biological stress response patterns, regardless of their level of self-esteem. This pattern is consistent with prior research showing that self-compassion has independent benefits for psychological (Leary et al., 2007) and immunological (Breines et al., 2014) responses to acute stress, but it remains to be seen whether the same pattern would emerge for other components of the stress response system, or in response to other types of stressors.
Although repeated stress is pervasive in daily life, from work-related pressure to marital conflict, individuals who are able to take a self-compassionate approach may experience reductions in sympathetic activation that, while seemingly small on their own, may have a sizable cumulative impact on the body over time, reducing allostatic load and therefore disease risk (McEwen, 1998). This study adds to the small body of research suggesting that self-compassion may represent a protective factor in the context of biological stress responses (Arch et al., 2014; Breines et al., 2014; Breines & Rohleder, under review). The potential link between self-compassion and longer-term health outcomes cannot be established from the present study, but this question represents an important direction for future research.
The conclusions that can be drawn from the present study are limited by several factors. First, participants were a sample of healthy young adults, so we cannot draw inferences about the relationship between self-compassion and sAA among children, older adults, or individuals with health problems. Second, although we found no significant gender differences in self-compassion, sAA, or the relationship between these variables, it is possible that our sample was not large enough to detect subtle interaction effects; future research is needed to more thoroughly examine the role of gender. Third, sAA responses observed in response to the standardized laboratory-based stress paradigm may not accurately reflect an individuals’ habitual response to naturalistic stressors encountered in everyday life. However, the standardized stressor was similar to the types of experiences that university students, who comprised our sample, regularly experience in academic contexts in the form of oral presentations and interviews for employment, giving it some degree of ecological validity. Fourth, as noted above, the presence of increased stress-induced sAA on just two days does not in itself represent a health risk, but rather a snapshot of an individual’s typical response to repeated stress. Fifth, the methods used in the present study were correlational and therefore cannot address causal questions. Finally, although sAA has been proposed as an indicator of sympathetic activation (Bosch et al., 1996; Rohleder et al., 2004; Nater & Rohleder, 2009), and sAA stress responses have been found to be moderately correlated with catecholamine stress responses (Rohleder et al., 2004; Nater & Rohleder, 2009; Thoma et al., 2012), sAA stress responses are not completely independent of parasympathetic stimulation of saliva flow rate, and differential effects of parasympathetic innervation of different salivary glands. Therefore, sAA stress responses are likely indicators of activation, or deactivation, of both arms of the autonomic nervous system (e.g., Bosch, Veerman, de Geus, & Proctor, 2011). Therefore, future research should examine whether self-compassion is also related to other sympathetic and parasympathetic markers.
In sum, the present research provides support for the hypothesis that self-compassionate individuals show reduced activation of a marker of the sympathetic nervous system in response to both novel and repeated stress. Given the pervasiveness of psychosocial stress in everyday life, and the potential for repeated stress to contribute to biological wear-and-tear, it is important to identify factors that reduce the physiological impact of stress, and self-compassion appears to be one such factor.
Acknowledgments
This work was supported by the American Federation for Aging Research (NR) and the National Institutes of Health under grants T32 MH 019929 (CM), T32-084907 (DG), and T32-AG000204 (JB).
We would like to thank the numerous research assistants in the Health Psychology Laboratory at Brandeis University who assisted with data collection.
Footnotes
The authors have no conflicts of interest to disclose.
References
- Allen A, Leary MR. Self-compassion, stress, and coping. Social and Personality Psychology Compass. 2010;4(2):107–118. doi: 10.1111/j.1751-9004.2009.00246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arch JJ, Brown KW, Dean DJ, Landy LN, Brown KD, Laudenslager ML. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology. 2014;42:49–58. doi: 10.1016/j.psyneuen.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blascovich J, Tomaka J. Measures of self-esteem. In: Robinson JP, Shaver PR, Wrightsman LS, editors. Measures of personality and social psychological attitudes. I. San Diego, CA: Academic Press; 1991. [Google Scholar]
- Bosch JA, Brand HS, Ligtenberg TJM, Bermond B, Hoogstraten J, Nieuw Amerongen AV. Psychological stress as a determinant of protein levels and salivary-induced aggregation of Streptococcus gordonii in human whole saliva. Psychosomatic Medicine. 1996;58(4):374–382. doi: 10.1097/00006842-199607000-00010. [DOI] [PubMed] [Google Scholar]
- Bosch JA, Veerman ECI, Turkenburg M, Hartog K, Bolscher JGM, Nieuw Amerongen AV. A rapid fluorimetric assay for determining bacterial adherence using DNA-binding stains. Journal of Microbiological Methods. 2003;53:51–56. doi: 10.1016/s0167-7012(02)00220-8. [DOI] [PubMed] [Google Scholar]
- Bosch JA, Veerman EC, de Geus EJ, Proctor GB. Alpha-Amylase as a Reliable and Convenient Measure of Sympathetic Activity: Don’t Start Salivating Just Yet! Psychoneuroendocrinology. 2011;36:449–453. doi: 10.1016/j.psyneuen.2010.12.019. [DOI] [PubMed] [Google Scholar]
- Breines JG, Thoma MV, Gianferante D, Hanlin L, Chen X, Rohleder N. Self-compassion as a predictor of interleukin-6 response to acute psychosocial stress. Brain, Behavior and Immunity. 2014;37:109–114. doi: 10.1016/j.bbi.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breines JG, Rohleder N. A brief self-compassion intervention reduces cortisol responses to repeated acute psychosocial stress. (under review) [Google Scholar]
- Charles ST, Piazza JR, Mogle J, Sliwinski MJ, Almeida DM. The wear-and-tear of daily stressors on mental health. Psychological Science. 2013;24(5):733–741. doi: 10.1177/0956797612462222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Gruenewald TL, Kemeny ME. When the social self is threatened: Shame, physiology, and health. Journal of Personality. 2004;72(6):1192–1216. doi: 10.1111/j.1467-6494.2004.00295.x. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130(3):355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- Edelstein RS, Yim IS, Quas JA. Narcissism predicts heightened cortisol reactivity to a psychosocial stressor in men. Journal of Research in Personality. 2010;44:565–572. doi: 10.1016/j.jrp.2010.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford MB, Collins NL. Self-esteem moderates neuroendocrine and psychological responses to interpersonal rejection. Journal of Personality and Social Psychology. 2010;98:405–419. doi: 10.1037/a0017345. [DOI] [PubMed] [Google Scholar]
- Frankenhaeuser M, von Wright MR, Collins A, von Wright J, Sedvall G, Swahn CG. Sex differences in psychoneuroendocrine reactions to examination stress. Psychosomatic Medicine. 1978;40:334–343. doi: 10.1097/00006842-197806000-00006. [DOI] [PubMed] [Google Scholar]
- Gilbert P, Procter S. Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy. 2006;13:353–379. [Google Scholar]
- Grassi G, Arenare F, Pieruzzi F, Brambilla G, Mancia G. Sympathetic activation in cardiovascular and renal disease. Journal of Nephrology. 2009;22(2):190–5. [PubMed] [Google Scholar]
- Kirschbaum C, Pirke KM, Hellhammer DH. The “Trier Social Stress Test” – a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28:76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Leary MR, Tate EB, Adams CE, Allen AB, Hancock J. Self-compassion and reactions to unpleasant self-relevant events: The implications of treating oneself kindly. Journal of Personality and Social Psychology. 2007;92(5):887–904. doi: 10.1037/0022-3514.92.5.887. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Neff KD. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity. 2003a;2(2):85–102. [Google Scholar]
- Neff KD. Development and validation of a scale to measure self-compassion. Self and Identity. 2003b;2:223–250. [Google Scholar]
- Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology. 2013;69(1):28–44. doi: 10.1002/jclp.21923. [DOI] [PubMed] [Google Scholar]
- Neff KD, Kirkpatrick K, Rude SS. Self-compassion and its link to adaptive psychological functioning. Journal of Research in Personality. 2007;41:139–154. [Google Scholar]
- Neff KD, Vonk R. Self-compassion versus global self-esteem: Two different ways of relating to oneself. Journal of Personality. 2009;77(1):23–50. doi: 10.1111/j.1467-6494.2008.00537.x. [DOI] [PubMed] [Google Scholar]
- Piazza JR, Charles ST, Sliwinski M, Mogle J, Almeida DM. Affective reactivity to daily stressors and long-term risk of reporting a chronic physical health condition. Annals of Behavioral Medicine. 2013;45:110–120. doi: 10.1007/s12160-012-9423-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raes F. Rumination and worry as mediators of the relationship between self-compassion and depression and anxiety. Personality and Individual Differences. 2010;48:757–761. [Google Scholar]
- Rector NA, Roger D. The stress buffering effects of self-esteem. Personality and Individual Differences. 1997;23:799–808. [Google Scholar]
- Rohleder N, Chen E, Wolf JM, Miller GE. The psychobiology of trait shame in young women: extending the social self preservation theory. Health Psychology. 2008;27(5):523–32. doi: 10.1037/0278-6133.27.5.523. [DOI] [PubMed] [Google Scholar]
- Rohleder N, Nater UM. Determinants of Salivary Alpha-Amylase in Humans and Methodological Considerations. Psychoneuroendocrinology. 2009;34:469–485. doi: 10.1016/j.psyneuen.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Rohleder N, Nater UM, Wolf JM, Ehlert U, Kirschbaum C. Psychosocial stress induced activation of salivary alpha-amylase: An indicator of sympathetic activity? Annals of the New York Academy of Sciences. 2004;1032:258–63. doi: 10.1196/annals.1314.033. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. NJ: Princeton. University Press; 1965. [Google Scholar]
- Schommer NC, Hellhammer DH, Kirschbaum C. Dissociation between reactivity of the hypothalamus-pituitary-adrenal axis and the sympathetic-adrenal-medullary system to repeated psychosocial stress. Psychosomatic Medicine. 2003;65:450–460. doi: 10.1097/01.psy.0000035721.12441.17. [DOI] [PubMed] [Google Scholar]
- Strahler J, Rohleder N, Wolf JM. Acute psychosocial stress induces differential short-term changes in catecholamine sensitivity of stimulated inflammatory cytokine production. Brain, Behavior, and Immunity. doi: 10.1016/j.bbi.2014.07.014. (in press) [DOI] [PubMed] [Google Scholar]
- Taylor SE, Lerner JS, Sherman DK, Sage RM, McDowell NK. Are self enhancing cognitions associated with healthy or unhealthy biological profiles? Journal of Personality and Social Psychology. 2003;85:605–615. doi: 10.1037/0022-3514.85.4.605. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders. 2000;61:201–216. doi: 10.1016/s0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- Thoma MV, Kirschbaum C, Wolf JM, Rohleder N. Acute stress responses in salivary alpha-amylase predict increases of plasma norepinephrine. Biological Psychology. 2012;91:342–348. doi: 10.1016/j.biopsycho.2012.07.008. [DOI] [PubMed] [Google Scholar]