Abstract
Objective
Cervical cancer screening uptake may be influenced by inadequate knowledge in resource-limited settings. This randomized trial evaluated a health talk’s impact on cervical cancer knowledge, attitudes, and screening rates in rural Kenya.
Methods
419 women attending government clinics were randomized to an intervention (n=207) or control (n=212) group. The intervention was a brief health talk on cervical cancer. Participants completed surveys at enrollment (all), immediately after the talk (intervention arm), and at three-months follow-up (all). The primary outcomes were the change in knowledge scores and the final screening rates at three-months follow-up. Secondary outcomes were changes in awareness about cervical cancer screening, perception of personal cervical cancer risk, cervical cancer and HIV stigma, and screening acceptability.
Results
Knowledge Scores increased by 26.4% (8.7 to 11.0 points) in the intervention arm compared to only 17.6% (8.5 to 10.0 points) in the control arm (p<0.01). Screening uptake was moderate in both the intervention (58.9%; N=122) and control (60.9%; N=129) arms, with no difference between the groups (p=0.60).
Conclusion
A brief health talk increased cervical cancer knowledge, although it did not increase screening over simply informing women about free screening.
Practice Implications
Screening programs can increase patient understanding with just a brief educational intervention.
Keywords: cervical cancer screening, knowledge, risk perception, behavior, health education, Sub-Saharan Africa
1. Introduction
Cervical cancer is a leading cause of cancer in Sub-Saharan Africa [1]. Screening coverage in Africa is estimated to be only 2–20% in urban areas and 0.4–14% in rural areas; in Kenya, screening rates are approximately 4% in urban areas and only 2.6% in rural areas [2]. Low screening rates are due not only to limited availability of screening services, but also to barriers to screening uptake such as inadequate knowledge, not feeling at risk for cervical cancer, and stigma [3–6].
Alongside improving access, achieving maximal screening uptake will depend on understanding patient knowledge and attitudes. In South Africa, where women are legally entitled to free cervical cancer screening, screening is estimated at less than 10–20% [2]. Although this low rate is partially attributable to limited access, surveys also indicate that one to two thirds of women are unaware of screening availability [3]. Similarly, women in Botswana reported that the main barrier to screening was “inadequate knowledge about the test” (46.7%), ranking even above “limited access to doctors” (33.3%) [5]. Women in Limuru, Kenya also cited “lack of knowledge” and “lack of concern” as barriers to screening uptake and suggested cervical cancer education at the health facility would increase screening [7].
In addition to inadequate knowledge, another barrier to screening is not feeling at risk for cervical cancer. At two large hospitals in Kenya, 35–69% of women did not perceive themselves to be at risk for cervical cancer [8, 9]. Additionally, in the Limuru study, women frequently had misconceptions about cervical cancer risk factors and said that they did not feel the need for screening because they felt healthy [7]. Perceptions of risk are formed by information, emotional experiences, and cultural frameworks within a community; and studies have suggested that perception of personal risk for developing cancer can affect cancer screening behaviors [10].
Stigma is another potential barrier to screening. Due to cervical cancer’s sexual risk factors and association with HIV, stigma is being increasingly recognized as a potential deterrent to screening acceptance [6]. A study exploring the acceptability of different approaches to cervical cancer education in South Africa also highlighted the importance of providing a clear, non-stigmatizing message to increase screening uptake [11].
The Information Motivation and Behavior model purports that several factors influence motivation and behavior but that having information is an essential component of behavior change; this model has been used by HIV and family planning health education programs around the world, including programs in Kenya [12]. However, there are currently no widely used, reproducible educational interventions to promote cervical cancer screening in rural Africa. In 2012, the Family AIDS Care and Education Services (FACES) began supporting a Cervical Cancer Screening and Prevention (CCSP) program in rural FACES-supported government health facilities in the Nyanza Province of western Kenya. As part of this program, screening and treatment for precancerous lesions were offered free of charge to all women (regardless of HIV status). The program developed a clinic-based health talk following principles of culturally-sensitive health education [13], including creating an educational design that is familiar to participants, training community members to deliver the health message in the local language, and tailoring the health information to the local context. In order to evaluate the effectiveness of this educational intervention, we conducted a randomized control trial among women who had not yet been screened. The primary outcomes measured were the change in knowledge scores and the final screening rates at follow-up. Secondary outcomes were changes in cervical cancer awareness, perception of personal risk for cervical cancer, stigma, and screening acceptability.
2. Materials and Methods
Setting & Sampling
This study took place in eleven CCSP-supported rural health facilities in Suba and Mbita, two of the poorest districts in rural Kenya with an estimated HIV-prevalence of 25% [14, 15]. The health facilities included two district hospitals (highest level facility in a district offering inpatient, outpatient, and surgical services), five sub-district hospitals (middle level facility with inpatient and outpatient services), and four local dispensaries (local outpatient facility). Women attending these health facilities were directly approached while waiting for health services and invited to participate. Women qualified if they were eligible for cervical cancer screening according to FACES guidelines (i.e. non-pregnant women at least 23 years of age), had not previously been screened, could speak Kiswahili, Dholuo, or English, and were able and willing to provide informed consent. Participants were randomized to the control or intervention arm. Randomization was done in computer-generated blocks of eight.
Study Design
All participants completed a baseline survey on the day of enrollment. Participants in the intervention arm then participated in the health talk, followed by a post-education survey on the same day. All participants were invited to return to the health facility three months later to complete a follow-up survey; cell phone reminders were sent a few days prior to scheduled follow-up times. Participants who did not follow-up were called and those without functioning cell phone numbers were followed-up at their homes using the standard method of patient tracing used by the clinic’s community health workers based on locating information (ie nearby landmarks, local nicknames, etc) obtained at baseline. All participants were invited to seek free cervical cancer screening at the health facility either on a study day or another clinic day at their convenience. Screening verification was done through interview and clinic records.
Educational Intervention
The intervention consisted of a 30-minute interactive talk about cervical cancer. The talk reviewed basic health facts about cervical cancer, risk factors, how screening is performed, what screening results mean, and treatment options. The talk also included a guided discussion about barriers to screening and fears or stigma associated with screening. For standardization, each session was guided by a flip-chart and corresponding script, with content derived from WHO guidelines and other studies of common misconceptions about cervical cancer [3, 5, 16]. Community health workers who administered the talk attended a one-day training to learn and practice the teaching materials. In order to minimize contamination between the intervention and control arms, the health talk was given to the group of women in the intervention arm (typically 4–6 women) in a private area of each health facility and sessions typically concluded after all participants had completed the baseline survey and most women in the control arm had left clinic.
Survey Tool / Measurements
The orally administered surveys lasted approximately 20 minutes. Questions were adapted from previously validated questionnaires [3, 11, 17] and piloted prior to administration. Surveys collected demographic data and included yes/no and true/false questions regarding cervical cancer awareness, knowledge, perception of personal risk, stigma, and screening acceptability. All survey tools were written in English and translated into Kiswahili and Dholuo. Trained interviewers administered the surveys in the participant’s preferred language and recorded responses at the time of the interview into tablets using the Open Data Kit database program.
Analysis
Awareness of cervical cancer was assessed by five yes/no questions asking participants if they had ever heard of cervical cancer, screening, Pap smears, visual inspection with acetic acid (VIA), and human papilloma virus (HPV). An Awareness Score (AS) was generated out of five possible points with one point given for a “yes” response. The Knowledge section consisted of 15 true/false statements that included both facts and common myths about cervical cancer, risk factors, and HPV. A Knowledge Score (KS) was then generated, with one point given for each correct answer and no points given for incorrect answers and “I don’t know.” Perception of Risk was assessed by asking participants to respond “yes,” “no,” or “I don’t know” to the statement “I think I am at risk for cervical cancer.” Stigma was evaluated in two steps. First, participants answered an HIV stigma questionnaire that had been previously validated in this region to measure HIV stigma [17]. Next, participants were asked these same stigma questions in relation to cervical cancer. A Cervical Cancer Stigma Score and an HIV Stigma Score were both created out of 9 possible points, with one point given for each “yes” response. Based on previous studies, a score > 1.8 points would suggest the presence of disease-related stigma [17, 18]. Finally, Screening Acceptability was measured by asking whether the participant would accept screening. Participants were offered screening and uptake was recorded. Women who did not get screened were asked their reasons for declining.
The differences between mean survey scores from the initial survey to the three-month follow-up survey for the two study arms were compared using chi-square or t-tests where appropriate. The screening rates at three-month follow-up for the two arms were compared using a chi-square test. Outcome measures for the initial survey and the immediate post-education survey were also compared using chi-square or t-tests to measure the immediate impact of the health talk for all women enrolled in the intervention group. Stigma Scores, which had a skewed distribution, were analyzed with the Wilcoxon-Mann-Whitney test. Randomization and data analysis were done using STATA version 12.0 (College Station, TX).
Ethics
All study participants were informed about the study design, objectives, and follow-up protocol and they signed a written consent in their preferred language. Ethical approval was obtained from the Kenya Medical Research Institute Ethical Review Committee and the University of California, San Francisco Committee on Human Research.
3. Results
Demographic Characteristics
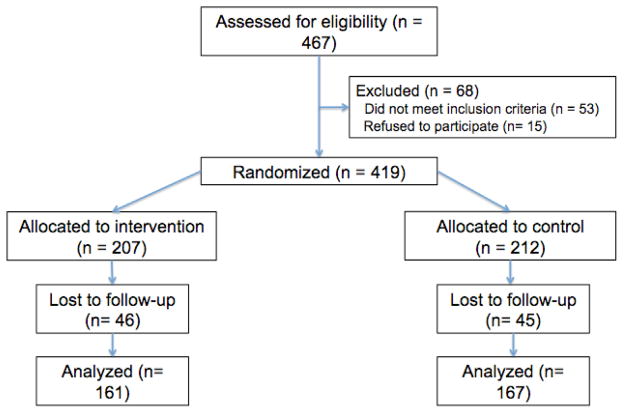
Between March and April 2013, women were recruited from eleven facilities to participate in the study. 419 women met study criteria, consented, and were individually randomized to the intervention (N=207) or control (N=212) arm. (Figure 1) Demographic characteristics did not differ significantly between the intervention and control groups, with the exception that women in the control group had higher parity (p=0.02) and gravidity (p=0.03). (Table 1)
Figure 1.
Participant Flow Chart
Table 1.
Demographic Characteristics
| Intervention (n=207) | Control (n=212) | p-value | |
|---|---|---|---|
| Age (mean +/− sd)a | 32.6 +/− 8.9 | 34.0 +/− 9.6 | 0.13 |
|
| |||
| Relationship Status | 0.42 | ||
| Single | 24 (11.6%) | 16 (7.6%) | |
| Married | 134 (64.7%) | 148 (69.8%) | |
| Widowed | 46 (22.2%) | 43 (20.3%) | |
| Separated/Divorced | 3 (1.5%) | 5 (2.4%) | |
|
| |||
| Highest Educational Level | 0.68 | ||
| Primary school incomplete or none | 99 (47.8%) | 101 (47.6%) | |
| Primary school complete | 57 (27.5%) | 52 (24.5%) | |
| Some secondary school or beyond | 51 (24.6%) | 59 (27.8%) | |
|
| |||
| Occupation | 0.32 | ||
| Professional/technical/managerial | 13 (6.3%) | 20 (9.4%) | |
| Housewife/farming | 81 (39.1%) | 89 (42.0%) | |
| Non-professional work outside the home | 113 (54.6%) | 103 (48.6%) | |
|
| |||
| Facility Typea | 0.35 | ||
| District Hospital (Level 1 Facility) | 56 (27.1%) | 52 (24.5%) | |
| Sub-district Hospital (Level 2 Facility) | 92 (44.4%) | 97 (45.8%) | |
| Dispensary (Level 3 Facility) | 59 (28.5%) | 63 (29.7%) | |
|
| |||
| Transportation to clinic | 0.23 | ||
| Walking | 112 (54.1%) | 132 (62.3%) | |
| Motorcycle | 89 (43.0%) | 74 (34.9%) | |
| Other (bicycle, boat, bus) | 6 (2.9%) | 6 (2.8%) | |
| Travel time to clinic (mean minutes +/− sd) | 45.2 +/− 37.3 | 49.7 +/− 42.7 | 0.25 |
|
| |||
| Primary source of health information | 0.14 | ||
| Health facility or healthcare worker | 171 (82.6%) | 186 (87.7%) | |
| Outside Source (radio, church, school, etc) | 36 (17.4%) | 26 (12.3%) | |
|
| |||
| Knows someone with cervical cancer | 62 (30.1%) | 59 (28.0%) | 0.63 |
|
| |||
| Prior Health seeking behavior | |||
| History of STD testing | 36 (17.5%) | 45 (21.2%) | 0.33 |
| History of breast exam | 15 (7.3%) | 10 (4.7%) | 0.27 |
| History of Mammogram | 9 (4.4%) | 8 (3.8%) | 0.77 |
| History of HIV testing* | 192 (92.8%) | 198 (93.4%) | 0.80 |
|
| |||
| Reproductive History | |||
| Gravida (mean +/− sd) | 3.2 +/− 2.3 | 3.7 +/−2.5 | 0.03 |
| Parity (mean +/− sd) | 2.9 +/− 2.1 | 3.4 +/− 2.3 | 0.02 |
| Age of sexual debut (mean +/− sd) (n=105) | 16.5 +/− 2.6 | 16.5 +/− 2.6 | 0.72 |
| # of current sexual partners (mean +/− sd) | 0.9 +/− 0.4 | 0.9 +/− 0.5 | 0.50 |
| # of lifetime sexual partners (mean +/− sd) | 2.2 +/− 1.3 | 2.3 +/− 1.2 | 0.30 |
| Sex workera | 3 (1.5%) | 5 (2.4%) | 0.50 |
|
| |||
| Family Planning | |||
| None | 122 (58.9%) | 105 (49.5%) | 0.08 |
| Type of Family Planning (% of those using FP) | 0.97 | ||
| Depo-provera | 40 (48.2%) | 53 (49.5%) | |
| Long-term (IUCD or Implant) | 21 (25.3%) | 23 (21.5%) | |
| Condom | 9 (10.8%) | 12 (11.2%) | |
| Permanent (Tubal Ligation or Vasectomy) | 7 (8.4%) | 9 (8.4%) | |
| Other (patch, OCP’s, natural, multiple) | 6 (7.2%) | 10 (9.4%) | |
|
| |||
| HIV Statusa | 0.73 | ||
| Positive | 115 (55.6%) | 118 (55.7%) | |
| Negative | 59 (28.5%) | 55 (25.9%) | |
| Unknownb | 33 (15.9%) | 39 (18.4%) | |
| Average duration since tested positive (years) | 3.4 +/− 2.8 | 3.1 +/− 2.7 | 0.46 |
| Average duration since last negative HIV test | 0.7 +/− 0.8 | 1.0 +/− 1.7 | 0.24 |
Characteristics that differed significantly (p<0.05) between participants who followed-up and those who did not follow-up. Women who did NOT follow-up were more likely to be younger, attend a district hospital, be a sex worker, have no history of HIV testing, and have an unknown HIV status.
”Unknown” = never screened for HIV or no negative test within the last year
Three hundred and twenty-eight (78%) women completed the three-month follow-up survey, 161 (78%) from the intervention and 167 (79%) from the control (p=0.81). Compared to women who did follow-up, women who did not follow-up were younger (31.6 yrs vs. 33.8 yrs; p<0.05), more likely to be interviewed at a district hospital (36.3% vs 22.9%; p=0.04), and more likely to have never been tested for HIV (13.2% vs 5.2%; p<0.01). Of those who followed-up, there were no demographic differences between the intervention and control arm. Of those who followed-up, baseline scores across all outcome measures did not significantly differ between the two study arms.
Primary Outcomes: Effect of Educational Intervention on Knowledge and Screening
Knowledge Scores increased significantly after the educational intervention. At three months follow-up, Knowledge Scores in the intervention arm increased 26.4% (8.7 to 11.0 points) compared to only a 17.6% increase (8.5 to 10.0 points) in the control arm, t(326)=2.64, p<0.01. (Table 2) Over half of all participants in both the intervention arm (N=122/207; 58.9%) and the control arm (N=129/212; 60.9%) got screened during the study period, with no significant difference in screening rates between the two groups,
Table 2.
Changes in Knowledge & Attitudes in Intervention Versus Control Arm
| Initial Survey | Follow-Up Survey | Change | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Intervention (n=161) | Control (n=167) | p-value | Intervention (n=161) | Control (n=167) | p-value | Intervention | Control | p-value | |
| Knowledge Scorea (0–15 points) | 8.7 (8.3–9.0) | 8.5 (8.1–8.9) | 0.17 | 11.0 (10.7–11.3) | 10.0 (9.6–10.3) | <0.001 | 2.3 (1.9–2.7) | 1.5 (1.0–2.0) | <0.01c |
| Awareness Scorea (0–5 points) | 2.6 (2.4–2.8) | 2.4 (2.2–2.6) | 0.44 | 4.0 (3.8–4.1) | 3.3 (3.1–3.4) | <0.001 | 1.4 (1.1–1.6) | 0.9 (0.7–1.1) | <0.01d |
| Perception of Personal Cervical Cancer Riskb | 115 (71.4%) | 116 (69.5%) | 0.15 | 135 (83.9%) | 143 (85.6%) | 0.65 | 12.5% | 16.1% | 0.69d |
| Cervical Cancer Stigma Scorea (0–9 points) | 0.8 (0.5–1.1) | 0.6 (0.4–0.9) | 0.49 | 0.2 (0.1–0.3) | 0.2 (0.0–0.3) | 0.49 | 0.6 (0.3–0.9) | 0.5 (0.2–0.7) | 0.62d |
| HIV Stigma Scorea (0–9 points) | 1.2 (0.8–1.5) | 0.7 (0.5–0.9) | 0.13 | 0.4 (0.2–0.6) | 0.4 (0.2–0.5) | 0.63 | 0.8 (0.4–1.1) | 0.3 (0.1–0.6) | 0.05d |
| Screening Acceptabilityb | 127 (78.9%) | 133 (79.6%) | 0.87 | 145 (90.1%) | 155 (92.8%) | 0.37 | 11.2% | 13.2% | 0.55d |
reported mean (95% CI)
reported N (%)
Primary outcome: At 3-month follow-up, Knowledge Score increased significantly more in the intervention arm compared the control arm.
Secondary outcomes: At 3-month follow-up, Awareness Score increased significantly more in the intervention arm compared to the control arm. The HIV Stigma Score also decreased significantly more in the intervention arm, although the final HIV Stigma Score at follow-up did not differ between arms. There was no difference in the change in perception of personal cervical cancer risk, cervical cancer stigma, or screening acceptability between the two arms.
χ2 (1, N=419) = 0.16, p=0.69. Screening rates were significantly higher amongst women who followed-up (N=228/328; 69.5%) compared to women who did not follow-up (N=23/91; 25.3%), χ2 (1, N=419) = 58.04, p=<0.001). However, amongst only those women who followed-up, there was again no significant difference in screening rates between the intervention (N=109/161; 67.7%) and control (N=119/167; 71.2%) arms (p=0.49), χ2 (1, N=328) = 0.49, p=0.48.
Secondary Outcomes: Effect of Educational Intervention on Awareness, Risk Perception, Stigma, and Screening Acceptability
Awareness Scores did increase significantly more in the intervention versus control arm at three months follow-up. Awareness Scores increased by 53.8% (2.6 to 4.0 points) in the intervention arm compared to only 37.5% (2.4 to 3.3 points) in the control arm, t(326)=2.6, p<0.01. (Table 2)
Perceived cervical cancer risk increased in both groups after three months with no significant difference between women who received education and those who did not, χ2 (2, N=328) = 0.73, p=0.69. Cervical Cancer Stigma Scores decreased in both groups with no difference between the intervention and control groups (Z = 0.49, p = 0.62). HIV Stigma Scores also decreased overall, and the decrease was significantly larger in the intervention group (Z = 2.0, p=0.05). Screening acceptability increased overall at follow-up but the change in acceptability did not differ significantly between women in the intervention and control arms, χ2 (2, N=328) = 1.19, p=0.55. Additionally, screening rates were not significantly associated with final measures of cervical cancer awareness, knowledge, risk, or stigma. (Table 2)
Immediately following the health talk, women in the intervention arm (n=207) had significantly increased cervical cancer knowledge (p<0.001), awareness (p<0.001), perception of personal risk (p=0.001), and had decreased cervical cancer stigma (p<0.001) and HIV stigma (p<0.001). Screening acceptability also increased but was not significantly different than the initial survey (p=0.26). These post-education measures were comparable to those seen at three-month follow-up and therefore are not reported.
Reported Reasons for Declining Screening
On the day of enrollment, the most common reasons for declining screening were “busy today/no time to wait” (N=92/168; 54.8%), “currently menstruating” (N=36/168; 21.4%), and “undecided/want more time to think about it” (N=34/168; 20.2%). At follow-up, in addition to “busy today/no time to wait” (N=15/79; 19.0%) and “currently menstruating” (N=14/79; 17.7%), two other reasons frequently given at this point were “do not understand enough about screening” (N=15/79; 19.0%) and “fear of pain with the speculum exam” (N=13/79; 16.5%). There was no significant difference between reasons given by women in the different study arms.
4. Discussion and Conclusion
4.1 Discussion
Our single brief health talk significantly increased cervical cancer knowledge and awareness at three months. Screening uptake was moderate at three-months follow-up in both groups and screening rates were no different between women who received the health talk and women who were simply informed that screening was available. Cervical cancer risk perception, stigma, and screening acceptability also improved at follow-up. However, the intervention did not have a significant effect on these measures when compared to the control group.
Despite widespread recognition that cervical cancer knowledge is low in Sub-Saharan Africa, there are few prospective controlled studies evaluating educational interventions. Trials of cervical cancer education programs in Turkey and Nigeria have shown increased knowledge post-intervention [19, 20], but knowledge and attitudes are highly contextual and educational programs may not be readily transferable. Our study shows the positive impact of an educational intervention on knowledge in Eastern Africa, the region with the highest incidence of cervical cancer worldwide [1].
Data on how increased knowledge affects screening rates is even more limited. A retrospective study in East Africa showed a positive association between screening history and cervical cancer knowledge, raising the question of whether education can increase screening [21]. However, in our study, screening rates did not differ between women who attended the health talk and those who were simply informed that they were eligible for free screening. It is possible that information about screening availability may be just as effective as more in-depth education. A shorter message may in fact leave more time for screening, addressing the long wait times cited by many participants as their reason for declining screening.
This study is unique in creating and validating a cervical cancer educational intervention in this setting through a randomized trial. However, it has some limitations. Sampling was limited to clinic attendees and may not be representative of the wider community. Additionally, social desirability bias may have influenced responses to questions about general awareness, risk perception, and stigma. However, the fact-based cervical cancer knowledge questions should not have been subject to this type of bias.
Interestingly, all outcome measures improved significantly from baseline to follow-up in both arms. The changes in the control group could be attributed to several things including: 1) contamination bias through peer to peer education after the educational intervention, 2) increased overall community awareness during the follow-up period from ongoing community health campaigns, and 3) an increased awareness and interest in cervical cancer as a result of simply being informed about screening availability. A strength of this study is that it compares the outcome measures to a control group, thereby minimizing the potential overestimation of the intervention’s impact.
4.2 Conclusion
The educational intervention increased knowledge and awareness about cervical cancer screening, but it did not result in higher screening rates. A minimum level of understanding may be necessary for a woman to accept screening but perhaps simply informing women about screening availability is sufficient. The lack of difference in screening rates between the two study arms also raises the question of what factors that remained unchanged by the health talk could still influence a woman’s screening behavior. Stigma and perception of personal risk, which did not differ between the study arms at follow-up, may still be important barriers to screening but may require more than a health talk to change. Other important factors may include shorter wait times, repeated screening opportunities, and addressing women’s fears of the exam, as supported by this study and in prior literature [22, 23].
4.3 Practice implications
This study validated the positive influence of an educational intervention on knowledge, a commonly cited barrier to screening. Increasing knowledge about cervical cancer and awareness about screening opportunities can be achieved with a brief clinic-based health talk, but this is just the first step to improving screening rates. Attitudes and motivations are shaped not only by individual knowledge but also cultural shifts within a community; and decisions are made based on these and other competing interests such as finances and time [24]. As health systems increase efforts to address the enormous burden of cervical cancer disease, educational programs will need to expand beyond the clinic and into the community and continue striving to provide services in a patient-centered manner.
Supplementary Material
Highlights.
Patient education is a key component of cervical cancer screening programs.
Even short messages about cervical cancer screening may improve screening uptake.
A brief health talk increased patient knowledge about cervical cancer in rural Kenya.
A health talk also increased perception of cervical cancer risk and decreased stigma.
Acknowledgments
Role of Funding: This work was supported by a grant from the Doris Duke Charitable Foundation to the University of California, San Francisco to fund Clinical Research Fellow Joelle Rosser. While working on this project, M.J.H. was supported through a National Institutes of Health career development award (KL2 RR024130-04).
Elina Serrano for flipchart picture design. Jane Adera for Kiswahili and Dholuo translations.
Footnotes
Patient Confidentiality:
I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Conflict of Interest:
The authors have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011 Mar-Apr;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Louie KS, de Sanjose S, Mayaud P. Epidemiology and prevention of human papillomavirus and cervical cancer in sub-Saharan Africa: a comprehensive review. Trop Med Int Health. 2009 Oct;14(10):1287–1302. doi: 10.1111/j.1365-3156.2009.02372.x. [DOI] [PubMed] [Google Scholar]
- 3.Francis SA, Nelson J, Liverpool J, Soogun S, Mofammere N, Thorpe RJ., Jr Examining attitudes and knowledge about HPV and cervical cancer risk among female clinic attendees in Johannesburg, South Africa. Vaccine. 2010 Nov 23;28(50):8026–8032. doi: 10.1016/j.vaccine.2010.08.090. [DOI] [PubMed] [Google Scholar]
- 4.Hoque M, Hoque E, Kader SB. Evaluation of cervical cancer screening program at a rural community of South Africa. East African journal of public health. 2008 Aug;5(2):111–116. [PubMed] [Google Scholar]
- 5.McFarland DM. Cervical cancer and Pap smear screening in Botswana: knowledge and perceptions. Int Nurs Rev. 2003 Sep;50(3):167–175. doi: 10.1046/j.1466-7657.2003.00195.x. [DOI] [PubMed] [Google Scholar]
- 6.White HL, Mulambia C, Sinkala M, et al. ‘Worse than HIV’ or ‘not as serious as other diseases’? Conceptualization of cervical cancer among newly screened women in Zambia. Soc Sci Med. 2012 May;74(10):1486–1493. doi: 10.1016/j.socscimed.2012.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gatune JW, Nyamongo IK. An ethnographic study of cervical cancer among women in rural Kenya: is there a folk causal model? Int J Gynecol Cancer. 2005 Nov-Dec;15(6):1049–1059. doi: 10.1111/j.1525-1438.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- 8.Gichangi P, De Vuyst H, Estambale B, Rogo K, Bwayo J, Temmerman M. HIV and cervical cancer in Kenya. Int J Gynaecol Obstet. 2002 Jan;76(1):55–63. doi: 10.1016/s0020-7292(01)00560-4. [DOI] [PubMed] [Google Scholar]
- 9.Were E, Nyaberi Z, Buziba N. Perceptions of risk and barriers to cervical cancer screening at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya. Afr Health Sci. 2011 Mar;11(1):58–64. [PMC free article] [PubMed] [Google Scholar]
- 10.Lee SJ. Uncertain Futures: Individual Risk and Social Context in Decision-Making in Cancer Screening. Health, risk & society. 2010 Apr;12(2):101–117. doi: 10.1080/13698571003637048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maree JE, Wright SC. Cervical cancer: does our message promote screening? A pilot study in a South African context. Eur J Oncol Nurs. 2011 Apr;15(2):118–123. doi: 10.1016/j.ejon.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Onono M, Blat C, Miles S, et al. Impact of family planning health talks by lay health workers on contraceptive knowledge and attitudes among HIV-infected patients in rural Kenya. Patient education and counseling. 2014 Mar;94(3):438–441. doi: 10.1016/j.pec.2013.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health education & behavior : the official publication of the Society for Public Health Education. 2003 Apr;30(2):133–146. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 14.Camlin CS, Kwena ZA, Dworkin SL. Jaboya vs. jakambi: Status, negotiation, and HIV risks among female migrants in the “sex for fish” economy in Nyanza Province, Kenya. AIDS Educ Prev. 2013 Jun;25(3):216–231. doi: 10.1521/aeap.2013.25.3.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cohen CR, Montandon M, Carrico AW, et al. Association of attitudes and beliefs towards antiretroviral therapy with HIV-seroprevalence in the general population of Kisumu, Kenya. PLoS One. 2009;4(3):e4573. doi: 10.1371/journal.pone.0004573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO. Cervical cancer screening in developing countries: report of a WHO consultation 2002. http://whqlibdoc.who.int/publications/2002/9241545720.pdf.
- 17.Turan JM, Bukusi EA, Onono M, Holzemer WL, Miller S, Cohen CR. HIV/AIDS stigma and refusal of HIV testing among pregnant women in rural Kenya: results from the MAMAS Study. AIDS Behav. 2011 Aug;15(6):1111–1120. doi: 10.1007/s10461-010-9798-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weiser SD, Heisler M, Leiter K, et al. Routine HIV testing in Botswana: a population-based study on attitudes, practices, and human rights concerns. PLoS Med. 2006 Jul;3(7):e261. doi: 10.1371/journal.pmed.0030261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bebis H, Reis N, Yavan T, Bayrak D, Unal A, Bodur S. Effect of health education about cervical cancer and papanicolaou testing on the behavior, knowledge, and beliefs of Turkish women. Int J Gynecol Cancer. 2012 Oct;22(8):1407–1412. doi: 10.1097/IGC.0b013e318263f04c. [DOI] [PubMed] [Google Scholar]
- 20.Wright KO, Kuyinu YA, Faduyile FA. Community education on cervical cancer amongst market women in an urban area of Lagos, Nigeria. Asian Pac J Cancer Prev. 2010;11(1):137–140. [PubMed] [Google Scholar]
- 21.Lyimo FS, Beran TN. Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: three public policy implications. BMC Public Health. 2012;12:22. doi: 10.1186/1471-2458-12-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Busingye P, Nakimuli A, Nabunya E, Mutyaba T. Acceptability of cervical cancer screening via visual inspection with acetic acid or Lugol’s iodine at Mulago Hospital, Uganda. Int J Gynaecol Obstet. 2012 Dec;119(3):262–265. doi: 10.1016/j.ijgo.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 23.Stormo AR, Altamirano VC, Perez-Castells M, et al. Bolivian health providers’ attitudes toward alternative technologies for cervical cancer prevention: a focus on visual inspection with acetic acid and cryotherapy. J Womens Health (Larchmt) 2012 Aug;21(8):801–808. doi: 10.1089/jwh.2012.3796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sanders Thompson VL. Cultural context and modification of behavior change theory. Health education & behavior : the official publication of the Society for Public Health Education. 2009 Oct;36(5 Suppl):156S–160S. doi: 10.1177/1090198109340511. discussion 167S–171S. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.